Introduction
Cerebellar infarcts are acute ischemic stroke subtypes caused by the occlusion of 1 of the 3 main cerebellar branches of the vertebrobasilar arterial system or the posterior circulation, namely, the superior (SCA), anterior inferior (AICA), and posterior inferior (PICA) cerebellar arteries. Posterior circulation infarcts account for approximately 20% of all acute ischemic strokes. Cerebellar infarcts account for only 3% of all ischemic strokes in the United States.[1] Despite their relatively low frequency, cerebellar strokes carry significant morbidity and mortality, attributed to the challenges arising from their occasionally subtle initial presentation and the adverse effects of reactive swelling in the posterior fossa. Cerebellar infarcts demand attention due to their unique diagnostic and management challenges.[2]
Occlusion of 1 of the 3 named cerebellar arteries usually causes larger, symptomatic cortical and subcortical infarcts. However, the more widespread use of brain magnetic resonance imaging (MRI) has revealed many cases of small cerebellar infarcts, which are mainly cortical and may not correspond to cerebellar arterial territories. These small cerebellar infarcts, in isolation, may be completely asymptomatic, often detected as incidental MRI findings of ischemic cortical cavities.[3][4]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Cerebellar infarcts arise from obstructions to the PICA, AICA, or SCA. Similar to other vascular territory ischemic strokes, the underlying vascular etiologies include large artery atherosclerosis affecting the vertebral or basilar arteries, artery-to-artery embolism, cardioembolism, trauma affecting the neck arteries, arterial dissection, small vessel diseases, and other rare causes, such as vasculitis and fibromuscular dysplasia.[5][6] Vertebrobasilar atherosclerotic disease and cardioembolism are the most common etiologies, accounting for about 75% of all cases of acute cerebellar infarcts. Emboli originating from the heart often occur due to pump failure or irregular heart rhythms, disrupting smooth blood transit through the heart, as seen in conditions like atrial fibrillation and atrial flutter. The small (<2 cm), mostly asymptomatic cerebellar infarcts were believed to be border-zone infarcts between the known cerebellar vascular territories. Small vessel disease is also recognized as the etiology of these relatively common infarcts detected by MRI as ischemic cortical cavities.
Epidemiology
Cerebellar infarcts make up only about 2% of all strokes, yet they contribute significantly to the resulting morbidity and mortality. A study involving nearly 2000 consecutive patients with stroke revealed that cerebellar strokes had an alarming mortality rate of 23%, almost twice that of more common cerebral strokes (12.5%). Brainstem strokes fell in between, with a mortality rate of 17%.[7]
Pathophysiology
Neurological deficits arising from cerebellar infarcts are primarily determined by the physiologic function of the involved vascular territories (see Image. Cerebellar Arteries and Distribution). PICA occlusion, the most common vascular cause of cerebellar infarcts, leads to the acute onset of dizziness, vertigo, and an inability to walk or stand, sometimes resulting in classical Wallenberg syndrome.[8] Additional signs and symptoms may include hoarseness, dysarthria, Horner syndrome, and impaired pain and temperature sensation on the ipsilateral face and contralateral arm and leg.
Infarction in the AICA territory often causes dysmetria, unilateral hearing loss or tinnitus, and ipsilateral facial paralysis or anesthesia, with contralateral hemibody pain and temperature sensory loss. Obstruction of the more rostrally located SCA tends to produce more ataxia, dysarthria, and nystagmus, with less frequent occurrences of vertigo, headache, and vomiting.[9] However, presentations can overlap or have atypical features.
Acute cerebral or cerebellar infarcts cause cerebral edema, initially by cytotoxic mechanisms from energy failure and subsequent cell swelling, followed by more severe vasogenic edema from vascular endothelial damage and blood-brain barrier breakdown. Cerebral edema surrounding the territory of an infarct can pose significant challenges, particularly in the context of cerebellar strokes. The cerebellum is situated within the confined space of the posterior cranial fossa, enclosed by the tentorium cerebelli superiorly, occipital bone posterolaterally, foramen magnum inferiorly, and fourth ventricle and brainstem anteriorly. Swelling can lead to upward transtentorial herniation of the cerebellar vermis, a mechanism the brain employs to alleviate the increasing intracranial pressure.
Alternatively, edema can anteriorly obstruct the fourth ventricle and aqueducts, causing direct brainstem compression. Fourth ventricle obstruction can increase intracranial pressure, beginning from the choroid plexus where cerebrospinal fluid is produced. This pressure buildup may cause the cerebellar tonsils to herniate downward into the foramen magnum, resulting in a potentially catastrophic condition.
History and Physical
The most characteristic symptoms of an acute cerebellar infarct include the abrupt onset of vertigo, nausea, vomiting, and gait ataxia. In any person of advanced age with sudden vertigo and inability to walk, an acute cerebellar infarct should be suspected until proven otherwise. Similarly, someone of advanced age presenting with acute vertigo, headache, and inability to walk should be considered to have an acute cerebellar hemorrhage until ruled out. A high index of suspicion is most important in diagnosing acute cerebellar stroke and avoiding its associated complications.
Approximately 75% of patients with cerebellar infarcts report experiencing dizziness in various forms, often described as vertigo or feeling like falling toward the side of the infarct.[10] Many patients complain of difficulty walking, attributed to ataxia or focal or systemic weakness. More than 50% of patients report symptoms of nausea or vomiting. The severity of symptoms is frequently more significant than evident upon examination.
Neurological findings in cerebellar strokes may include truncal or limb ataxia, cranial nerve defects like diplopia or nystagmus, especially if direction-changing, gaze-evoked, vertical, or torsional, and dysarthria. Unlike cerebral strokes, these deficits are usually ipsilesional, occurring on the same side of the patient as the cerebellar stroke. In cases of larger strokes or features of elevated intracranial pressure or brainstem compression, patients may present with lethargy, frank coma, or cardiovascular collapse, all of which indicate a poor outcome.
In some cases, the diagnosis of a cerebellar stroke is missed due to the nonspecific nature of the symptoms. The presentation largely depends on the location and extent of the lesion. Therefore, a comprehensive history and neurological examination are crucial to diagnosing cerebellar lesions. The presence of vascular disease risk factors, including age, smoking, obesity, diabetes, hyperlipidemia, and hypertension, further amplifies the suspicion of cerebellar infarcts.
The presenting symptoms of a cerebellar infarction are frequently nonspecific and can overlap with other neurological, cardiovascular, gastrointestinal, and systemic conditions.[11] Attention must be given to thoracic, abdominal, and systemic complaints and findings to rule out other potentially life-threatening conditions, such as trauma, aortic dissection, acute coronary syndrome, pulmonary embolism, hypovolemia, or sepsis.
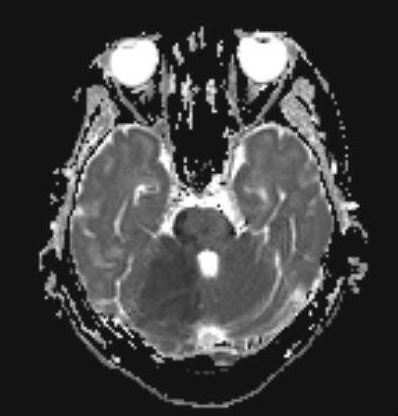
Evaluation
MRI with diffusion-weighted imaging of the brain is considered the gold standard test for diagnosing cerebellar infarction. MRI can visualize poor perfusion and signs of tissue injury, providing valuable information for accurate diagnosis (see Image. Cerebellar Infarction on Magnetic Resonance Imaging). Additionally, magnetic resonance angiography (MRA) can localize vascular obstructions and guide endovascular treatment, especially in cases of large vessel occlusion, which is particularly beneficial in basilar artery occlusion.
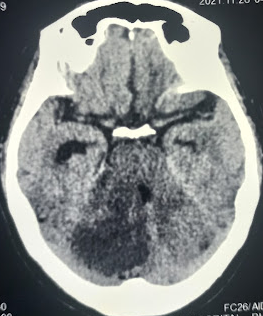
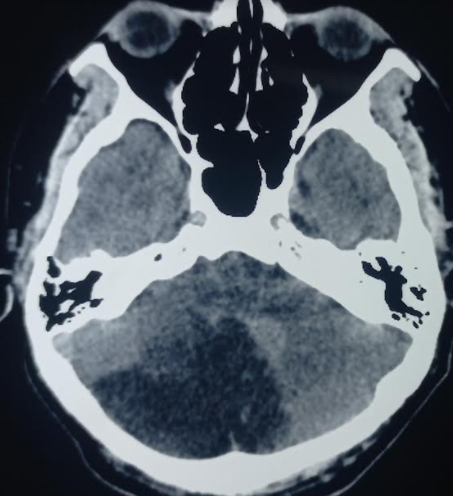
Unenhanced computed tomography (CT) can assist in assessing hemorrhagic lesions and occasionally demonstrate findings suggestive of infarction (see Image. Acute Cerebellar Infarction on Noncontrast Computed Tomography). However, the utility of this test is limited by the radiopaque temporal and occipital bones surrounding the cerebellum, reducing resolution, sensitivity, and specificity compared with other brain areas. Nonetheless, unenhanced CT is usually the initial choice, partly to assess for other causes but also because it is often more readily available than MRI or MRA (see Image. Acute Cerebellar Infarction on Computed Tomography).
Enhanced CT angiogram and perfusion imaging can be viable alternatives if MRI is unavailable. In addition to a standard bedside neurological examination, the oculomotor Head Impulse, Nystagmus, and Test of Skew (HINTS) examination can be valuable for differentiating peripheral vertigo and suggesting cerebellar infarction, especially if the "alternate eye cover test" reveals skew deviation.[12][13] Laboratory tests and electrocardiographic, echocardiographic, and electroencephalographic assessments may be conducted to evaluate for other systemic conditions. These tests are valuable in determining concurrent medical or surgical management.
Treatment / Management
Cerebellar infarcts are treated similarly to other acute ischemic stroke types initially. Patients who experience acute events with a precise onset time within 4.5 hours may be candidates for thrombolysis with recombinant tissue plasminogen activator (rtPA).[14] The criteria for thrombolysis are mentioned later. However, diagnosing posterior circulation infarcts can be challenging, making timely intervention difficult. Thrombectomy, similar to other strokes, remains an option. Structures in the posterior circulation, having higher white matter content and collateral flow, are believed to possess a stronger tolerance to ischemia and hypoxia than those in the anterior circulation.[15](A1)
In the case of larger basilar artery occlusion, thrombectomy is often considered beyond the typical 6-hour time window, and even delayed reperfusion therapy is deemed feasible for posterior infarcts.[16] Brain imaging revealing a substantial “mismatch” between the brain infarct volume and the area of decreased perfusion or a high degree of collateral circulation might prompt a more urgent thrombectomy. When reperfusion is not possible, aspirin therapy and the potential addition of another antiplatelet agent, such as clopidogrel, are indicated. Anticoagulation therapy may also be considered in patients with embolic events.
Reactive vasogenic cerebral edema typically intensifies over 3 to 4 days after the initial infarct. Admission to a neurologic intensive care unit (ICU) becomes essential if the neurological symptoms worsen, ensuring thorough and careful monitoring. Underlying preventable causes of the infarct are usually investigated during admission. Cardiac monitoring may uncover atrial fibrillation or other arrhythmias. Echocardiography may show a patent foramen ovale or ventricular dysfunction. Blood testing may reveal diabetes or hyperlipidemia.
Cerebellar strokes, especially after the first day, tend to develop progressive edema and potential subsequent herniation. Therefore, admitting these patients to the ICU is critical for close monitoring. Early symptoms often include severe headache, altered mental status, vomiting, and drowsiness. The important neurological signs for these patients are impaired level of consciousness, new or worsened cranial nerve deficits, gaze paresis, and downward gaze conjugation.
In cases of large strokes with significant cerebral edema, especially if the intracranial pressure is elevated, neurosurgical interventions such as extraventricular drains, ventriculostomy, or decompressive suboccipital craniotomy may be necessary.[17] Neurosurgical procedures like removal of infarcted tissue or hematoma are occasionally required. Additionally, in the acute setting, temporary reduction of intracranial pressure can be achieved using agents like mannitol, hypertonic saline, or hyperventilation.(A1)
Criteria for the Treatment of Acute Ischemic Stroke with Intravenous Thrombolysis
Intravenous thrombolysis with rtPA is a critical intervention for acute ischemic stroke. This treatment aims to restore blood flow and minimize neurological damage if administered within a specific time window from symptom onset. The inclusion and exclusion criteria for its use are given below.
Inclusion criteria
Treatment with rtPA is indicated for patients aged 18 years or older who have a clinical diagnosis of ischemic stroke resulting in a noticeable neurologic deficit. Treatment should begin within 4.5 hours of symptom onset, or if the exact time of onset is unknown, from when the patient was last known to be at their neurological baseline.
Exclusion criteria
Exclusion criteria ensure patient safety and the effectiveness of thrombolysis in acute ischemic stroke treatment. These criteria help identify conditions and factors that may contraindicate the use of intravenous rtPA, reducing the risk of adverse outcomes. The exclusion criteria for rtPA infusion are divided into several categories, as follows:
- Clinical exclusions: Patients should be excluded if they present with symptoms suggestive of subarachnoid hemorrhage, active internal bleeding, or infective endocarditis. Other exclusion criteria include suspected aortic arch dissection, acute bleeding diathesis, and persistent elevation of blood pressure (systolic pressure ≥185 mm Hg or diastolic pressure ≥110 mm Hg).
- Preclusive head CT findings: Head CT results showing evidence of hemorrhage or extensive hypodensity suggesting irreversible injury are also exclusionary.
- Disqualifying historical features: A history of severe head trauma or ischemic stroke within the last 3 months, prior intracranial hemorrhage, gastrointestinal malignancy, and intraaxial intracranial neoplasm are contraindications. Additionally, gastrointestinal hemorrhage within the last 3 weeks or recent intraspinal or intracranial surgery within the last 3 months warrants exclusion.
- Hematologic exclusions: Patients currently using anticoagulants with an international normalized ratio greater than 1.7, prothrombin time longer than 15 seconds, or activated partial thromboplastin time greater than 40 seconds should be excluded. A platelet count below 100,000/mm³ is also a contraindication. Recent therapeutic doses of low molecular weight heparin within 24 hours (such as for venous thromboembolism prevention) or the use of direct thrombin inhibitors or direct factor Xa inhibitors within the last 48 hours in patients with normal renal function also preclude rtPA treatment.
Evaluating these exclusion criteria is vital to ensure that thrombolysis is used only in appropriate situations. Every patient is different, and alternative treatments should be considered if rtPA's risks outweigh its benefits.
Differential Diagnosis
Cerebellar infarctions are often misdiagnosed as vestibular neuronitis, migraine, syncope (potentially due to orthostasis or arrhythmia), hypertensive emergency, renal failure, hypoglycemia, or ethanol or drug intoxication. Like other types of strokes, paying attention to historical features is crucial for risk stratification and treatment planning.
The timing of symptom onset and progression, coupled with provoking or alleviating factors, can be invaluable in diagnosing cerebellar strokes and distinguishing them from other conditions. Symptoms appearing within seconds to minutes are typically associated with benign paroxysmal positional vertigo, vasovagal syncope, or arrhythmia. Signs emerging over minutes to hours are often due to hypoglycemia, migraine, or psychological causes. Conversely, symptoms developing over hours to days are attributable to labyrinthitis or medication side effects but also raise suspicion for a cerebellar infarct.
The differential diagnosis for cerebellar infarction is broad and includes the following:
- Intracranial hemorrhage, especially acute cerebellar infarction
- Multiple sclerosis
- Brainstem infarction [18]
- Lacunar stroke
- Middle cerebral artery stroke
- Hypertensive encephalopathy
- Migraine headache [19]
- Toxic-metabolic disturbance (eg, hypoglycemia, drug intoxication)
- Posterior reversible encephalopathy syndrome
- Seizure with postictal paresis (Todd paralysis)
Careful history-taking, physical examination, and diagnostic evaluation can help differentiate cerebellar infarcts from these other clinical entities and guide management.
Prognosis
The prognosis following a cerebellar infarction is typically comparable to that of other strokes, with larger ischemic territories being associated with higher morbidity and mortality.[20] Advances in early recognition and treatment have contributed to a decline in the overall morbidity associated with the condition over time. The functional status of patients after a small cerebellar infarction is generally better than that of individuals who have experienced a larger, symptomatic cerebellar infarct.
Complications
Delayed diagnosis and treatment of cerebellar infarction can lead to cerebral edema and, ultimately, the patient's death. However, with prompt and effective treatment and diagnosis, most patients experience positive outcomes, with functional debility being the primary complication. Cerebellar infarction is associated with acute complications during hospitalization, such as venous thromboembolism, pressure ulcers, urinary tract infections, and pneumonia, similar to other acute stroke patients.
Postoperative and Rehabilitation Care
Rehabilitation care for cerebellar stroke is a comprehensive and tailored approach aimed at optimizing recovery and restoring functional independence. Patients undergo intensive monitoring in an acute care setting following surgical interventions, such as decompressive surgeries. Early rehabilitation initiation, often beginning in the hospital and extending to rehabilitation facilities or homes, is critical for maximizing recovery potential. An interprofessional team, including physical, occupational, and speech therapists, must collaborate to address specific deficits associated with cerebellar stroke.
Balance and coordination training are integral components of the rehabilitation program, given the cerebellum's role in these functions. Cognitive rehabilitation may be necessary to address memory, attention, and problem-solving deficits. Assistive devices, such as canes, walkers, and orthotics, may be introduced to enhance mobility and safety. Home modifications are assessed and implemented to ensure a supportive environment for the patient.
Psychosocial support is an essential aspect of rehabilitation, addressing the emotional and psychological impact of the stroke on both the patient and their caregivers. Ongoing monitoring and follow-up appointments with neurologists and rehabilitation specialists allow adjustments to the care plan based on the patient's progress and emerging needs. Individualized and goal-oriented care plans, incorporating a range of rehabilitation modalities, are crucial for facilitating recovery and improving the overall quality of life for individuals who have experienced a cerebellar stroke.
Consultations
An interprofessional team typically sees and manages patients with a cerebellar infarct. The initial assessment and triage often occur in the emergency department, where a physician or advanced practitioner evaluates the patient. Depending on the extent of the patient's condition, the intensivist or internal medicine practitioner may oversee their care, with plans for consultation with neurology to assist in management and treatment. In cases requiring surgical intervention, neurosurgeons may be involved in procedures such as decompressive surgeries to relieve pressure on the brain. Coordination among these specialists ensures comprehensive and effective care for individuals with cerebellar infarcts.
Deterrence and Patient Education
Patient education plays a pivotal role in the secondary prevention of cerebellar stroke. Imparting information about lifestyle changes and interventions can minimize the risk of recurrent strokes. Key aspects of patient education include encouraging smoking cessation and emphasizing the importance of maintaining optimal control of underlying comorbid conditions like diabetes and hypertension.
Patients should also be educated on the significance of consistent medication compliance and empowered to adopt lifestyle modifications, such as a heart-healthy diet and regular exercise, to reduce the risk of future cerebellar strokes. Healthcare providers can significantly contribute to long-term preventive measures and enhance overall health outcomes by fostering patient understanding and engagement.
Enhancing Healthcare Team Outcomes
Patients with cerebellar infarction frequently present with nonspecific symptoms, and clinical presentations can overlap or have atypical characteristics, especially in the case of hemorrhagic infarcts. Diagnosing cerebellar infarction requires a high index of suspicion and proficient diagnostic skills to ensure timely and appropriate treatment. Engaging a specialized interprofessional team consisting of clinicians, specialists, nurses, and pharmacists is essential when the disease is suspected. This collaborative approach enables a comprehensive evaluation of the case, facilitating prompt decisions on emergent treatment and determining which specialists to involve. The interprofessional paradigm is instrumental in achieving the best patient outcomes by ensuring a well-coordinated and multidisciplinary approach to managing cerebellar infarction.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)

Cerebellar Arteries and Distribution. Illustration depicting the arteries of the cerebellum and their distribution in the brain. The accompanying table outlines the structures influenced by these arteries and details anticipated neurological deficits that could be observed.
Contributed by B. Petit, CC BY-SA 4.0
References
Datar S, Rabinstein AA. Cerebellar infarction. Neurologic clinics. 2014 Nov:32(4):979-91. doi: 10.1016/j.ncl.2014.07.007. Epub 2014 Sep 13 [PubMed PMID: 25439292]
Edlow JA, Newman-Toker DE, Savitz SI. Diagnosis and initial management of cerebellar infarction. The Lancet. Neurology. 2008 Oct:7(10):951-64. doi: 10.1016/S1474-4422(08)70216-3. Epub [PubMed PMID: 18848314]
Calic Z, Cappelen-Smith C, Cuganesan R, Anderson CS, Welgampola M, Cordato DJ. Frequency, Aetiology, and Outcome of Small Cerebellar Infarction. Cerebrovascular diseases extra. 2017:7(3):173-180. doi: 10.1159/000481459. Epub 2017 Nov 2 [PubMed PMID: 29130973]
De Cocker LJ, van Veluw SJ, Biessels GJ, Spliet WG, Thunnissen IE, Luijten PR, Hendrikse J, Zwanenburg JJ. Ischaemic cavities in the cerebellum: an ex vivo 7-tesla MRI study with pathological correlation. Cerebrovascular diseases (Basel, Switzerland). 2014:38(1):17-23. doi: 10.1159/000365411. Epub 2014 Aug 27 [PubMed PMID: 25171512]
Wada Y, Kitano T, Uemura J, Yagita Y. Isolated Posterior Inferior Cerebellar Artery Dissection. Internal medicine (Tokyo, Japan). 2017 Nov 1:56(21):2959-2960. doi: 10.2169/internalmedicine.8780-16. Epub 2017 Sep 15 [PubMed PMID: 28924125]
Ripa V, Urakov TM, Jernigan SC. Vertebral Artery Dissection in a Bouncy Castle Injury: Case Report and Literature Review. Pediatric neurosurgery. 2017:52(4):234-239. doi: 10.1159/000474944. Epub 2017 May 30 [PubMed PMID: 28554184]
Level 3 (low-level) evidenceMacdonell RA, Kalnins RM, Donnan GA. Cerebellar infarction: natural history, prognosis, and pathology. Stroke. 1987 Sep-Oct:18(5):849-55 [PubMed PMID: 3629642]
Lui F, Tadi P, Anilkumar AC. Wallenberg Syndrome. StatPearls. 2024 Jan:(): [PubMed PMID: 29262144]
Hewett KM, Lorenzetti B, Jackson BF. Ataxia and Headache in a Child: A Case of Acute Cerebellar Infarction. Pediatric emergency care. 2017 Aug:33(8):570-572. doi: 10.1097/PEC.0000000000001216. Epub [PubMed PMID: 28777266]
Level 3 (low-level) evidenceWu B, Zhang W, Peng F, Zhang M, Shen B, Shi X, Zhang Y. Clinical Reasoning: A 37-Year-Old Man Presenting With Intermittent Dizziness and Brief Choreiform Movements. Neurology. 2023 Feb 21:100(8):389-396. doi: 10.1212/WNL.0000000000201653. Epub 2022 Dec 1 [PubMed PMID: 36456197]
Mehkri Y, Poe J, Nasrullah I, Hernandez J, Buchwald N, De Prey J, Albayram M, Shuhaiber H. Subacute Posterior Inferior Cerebellar Artery Stroke Radiographically Mimicking Lhermitte-Duclos Disease. Cureus. 2022 Nov:14(11):e31381. doi: 10.7759/cureus.31381. Epub 2022 Nov 11 [PubMed PMID: 36514563]
Level 3 (low-level) evidenceGuler A, Karbek Akarca F, Eraslan C, Tarhan C, Bilgen C, Kirazli T, Celebisoy N. Clinical and video head impulse test in the diagnosis of posterior circulation stroke presenting as acute vestibular syndrome in the emergency department. Journal of vestibular research : equilibrium & orientation. 2017:27(4):233-242. doi: 10.3233/VES-170620. Epub [PubMed PMID: 29081427]
Kattah JC, Talkad AV, Wang DZ, Hsieh YH, Newman-Toker DE. HINTS to diagnose stroke in the acute vestibular syndrome: three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke. 2009 Nov:40(11):3504-10. doi: 10.1161/STROKEAHA.109.551234. Epub 2009 Sep 17 [PubMed PMID: 19762709]
Level 2 (mid-level) evidenceKolahchi Z, Rahimian N, Momtazmanesh S, Hamidianjahromi A, Shahjouei S, Mowla A. Direct Mechanical Thrombectomy Versus Prior Bridging Intravenous Thrombolysis in Acute Ischemic Stroke: A Systematic Review and Meta-Analysis. Life (Basel, Switzerland). 2023 Jan 9:13(1):. doi: 10.3390/life13010185. Epub 2023 Jan 9 [PubMed PMID: 36676135]
Level 1 (high-level) evidenceMattle HP, Arnold M, Lindsberg PJ, Schonewille WJ, Schroth G. Basilar artery occlusion. The Lancet. Neurology. 2011 Nov:10(11):1002-14. doi: 10.1016/S1474-4422(11)70229-0. Epub [PubMed PMID: 22014435]
Vergouwen MD, Algra A, Pfefferkorn T, Weimar C, Rueckert CM, Thijs V, Kappelle LJ, Schonewille WJ, Basilar Artery International Cooperation Study (BASICS) Study Group. Time is brain(stem) in basilar artery occlusion. Stroke. 2012 Nov:43(11):3003-6. doi: 10.1161/STROKEAHA.112.666867. Epub 2012 Sep 18 [PubMed PMID: 22989501]
Ayling OGS, Alotaibi NM, Wang JZ, Fatehi M, Ibrahim GM, Benavente O, Field TS, Gooderham PA, Macdonald RL. Suboccipital Decompressive Craniectomy for Cerebellar Infarction: A Systematic Review and Meta-Analysis. World neurosurgery. 2018 Feb:110():450-459.e5. doi: 10.1016/j.wneu.2017.10.144. Epub 2017 Dec 2 [PubMed PMID: 29104155]
Level 1 (high-level) evidenceSun B, Jin Y, Ye Z, Xu H, Luo W, Liu S. Vertebral artery dissection induced lateral medullary syndrome characterized with severe bradycardia: a case report and review of the literature. Annals of palliative medicine. 2022 Oct:11(10):3330-3336. doi: 10.21037/apm-22-1098. Epub [PubMed PMID: 36367000]
Level 3 (low-level) evidencePescador Ruschel MA, De Jesus O. Migraine Headache. StatPearls. 2025 Jan:(): [PubMed PMID: 32809622]
Lee L, Loh D, Kam King NK. Posterior Fossa Surgery for Stroke: Differences in Outcomes Between Cerebellar Hemorrhage and Infarcts. World neurosurgery. 2020 Mar:135():e375-e381. doi: 10.1016/j.wneu.2019.11.177. Epub 2019 Dec 6 [PubMed PMID: 31816455]