Mohs Micrographic Surgery Interpretation of Positive Versus Negative Specimens
Mohs Micrographic Surgery Interpretation of Positive Versus Negative Specimens
Summary / Explanation
Overview
The accurate interpretation of positive and negative margins in Mohs micrographic surgery depends on specialized training in histological evaluation. This process involves the histological interpretation of tangentially processed frozen sections—a method that differs from the traditional vertical sectioning used in general pathology. When interpreting a slide, the initial step of a Mohs surgeon is to identify the tumor. This initial information is usually obtained from a biopsy performed before the surgical procedure. However, the biopsy results may not always be accurate or complete. For instance, a superficial basal cell carcinoma could have an undetected nodular component not identified during the initial histological evaluation.
Certain skin cancers are easier to identify due to their prevalence and recognizable features in patients. In contrast, rare tumors can be more challenging to diagnose and may require special histological stains for accurate margin assessment. Many recurrences of skin cancer are attributed to errors in slide preparation or interpretation.[1]
Tissue Processing
Correct tissue mapping is the initial step in interpreting margins during Mohs surgery. The Mohs surgeon must ensure that the score marks on the tissue align accurately with the map while mapping the tumor and that the specimens are properly stained. Additionally, the surgeon should verify that the histological features of the specimen correspond to the correct anatomical area from which it was taken.
Finally, the surgeon must also evaluate the quality of the staining and overall laboratory processes. Common issues include poor or incomplete staining, air bubbles, improper coverslip placement, folded specimens, chatter artifacts, and specimens that are either too thick or too thin.[2]
Pearls and Pitfalls
Although many tumors are treated with Mohs surgery, this summary will focus on basal cell carcinoma, highlighting common pearls and pitfalls associated with the procedure.
Inflammation: Dense lymphocytic aggregates are characteristic of inflammation surrounding skin cancers in histological specimens. However, inflammation can also occur from causes unrelated to skin cancer, making it challenging to determine whether the tumor margin is positive or negative. Some surgeons may opt to take an additional layer in the presence of inflammation, as it can potentially obscure small foci of malignancy.[3]
Tumor floaters: During processing, tumor tissue or excised specimen fragments can occasionally become ectopically placed in other areas of the specimen. This phenomenon is referred to as a tumor floater.[2] Several factors can contribute to this occurrence of tumor floaters, and a trained Mohs surgeon must be able to recognize them as artifacts. However, differentiating them from genuine tumors may be challenging, necessitating the removal of a thin layer from the area where the potential tumor floater is located.
Common benign structures and proliferation: Another common pitfall is the failure to recognize benign neoplasms and normal structures within the tissue, leading to confusion with malignant tissue that requires excision. Common skin mimics include:
- Salivary glands that are located around the lip or within specimens adjacent to the parotid gland.[2]
- The folliculosebaceous unit consisting of the hair follicle and the attached sebaceous gland.[2]
- Benign adnexal neoplasms such as trichoepitheliomas and fibrofolliculomas.[4]
- Follicular basaloid proliferation, also known as benign follicular proliferation or benign follicular hamartoma.[4]
Example Cases
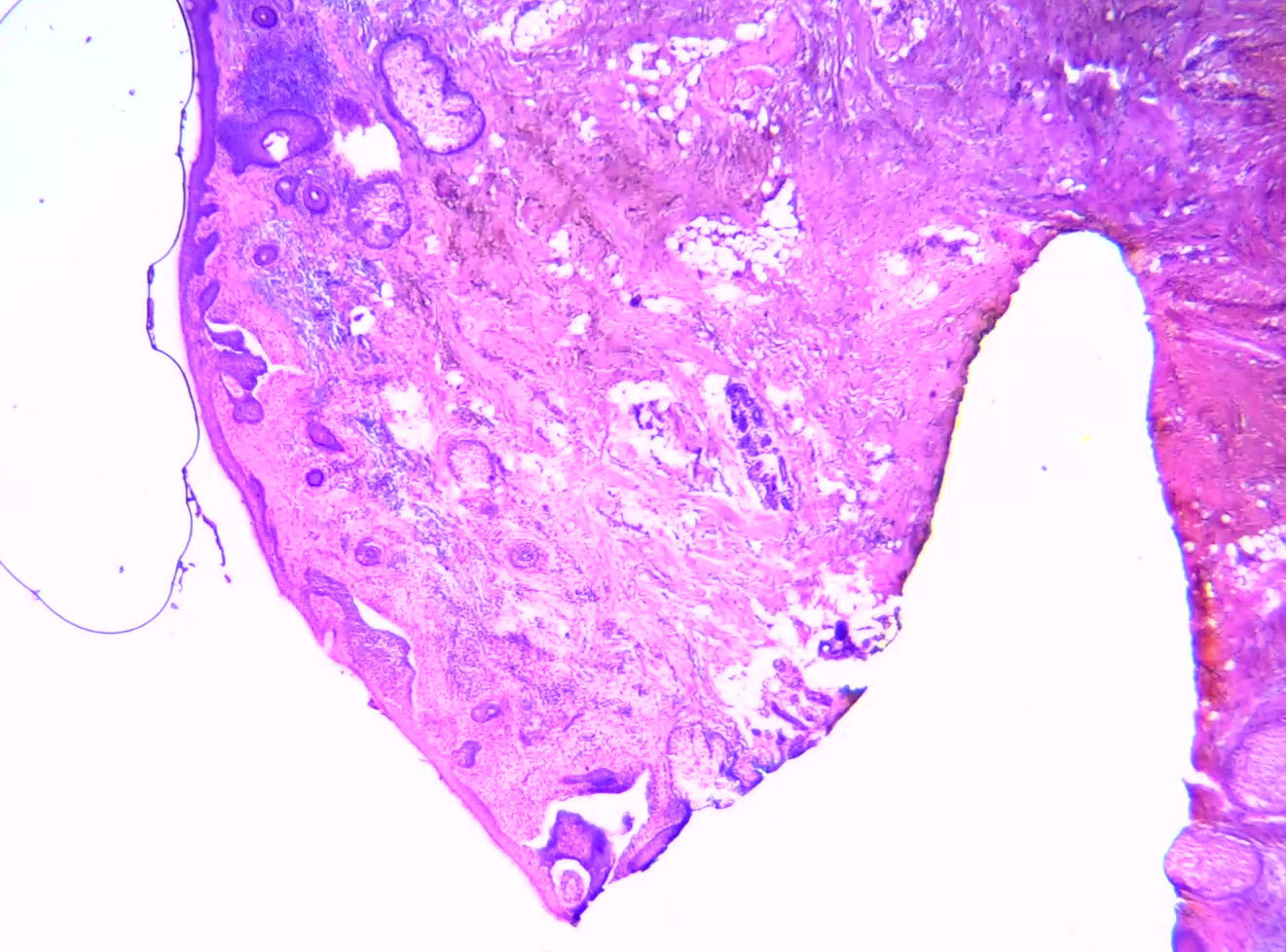
In the first stage of a Mohs procedure on the nasal sidewall, a superficial basal cell carcinoma is evident between the 3-o'clock and 6-o'clock margins. This is indicated by the purple buds protruding from the epidermis, which are accompanied by retraction artifacts. The 3-o'clock margin is stained orange. Near the 6-o'clock margin, a notable hair follicle and sebaceous gland are present, which may mimic basal cell carcinoma (see Image. Mohs Procedure Stage 1).
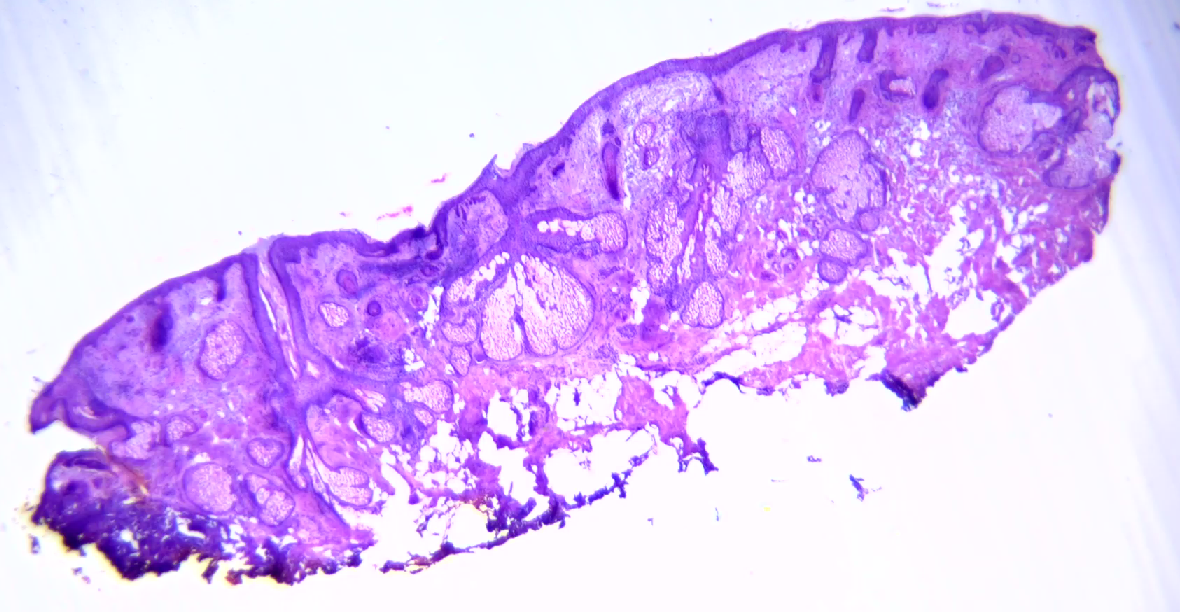
By the third stage of the same procedure, basal cell carcinoma is no longer visible. However, multiple benign hair follicles and normal sebaceous glands are observed, along with a regular epidermis and dermal-epidermal junction (see Image. Mohs Procedure Stage 3).
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Hruza GJ. Mohs micrographic surgery local recurrences. The Journal of dermatologic surgery and oncology. 1994 Sep:20(9):573-7 [PubMed PMID: 8089356]
Golda N, Hruza G. Mohs Micrographic Surgery. Dermatologic clinics. 2023 Jan:41(1):39-47. doi: 10.1016/j.det.2022.07.006. Epub 2022 Oct 28 [PubMed PMID: 36410982]
Macdonald J, Sneath JR, Cowan B, Zloty D. Tumor detection after inflammation or fibrosis on Mohs levels. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2013 Jan:39(1 Pt 1):64-6. doi: 10.1111/dsu.12012. Epub 2012 Nov 27 [PubMed PMID: 23190366]
Stanoszek LM, Wang GY, Harms PW. Histologic Mimics of Basal Cell Carcinoma. Archives of pathology & laboratory medicine. 2017 Nov:141(11):1490-1502. doi: 10.5858/arpa.2017-0222-RA. Epub [PubMed PMID: 29072946]