Introduction
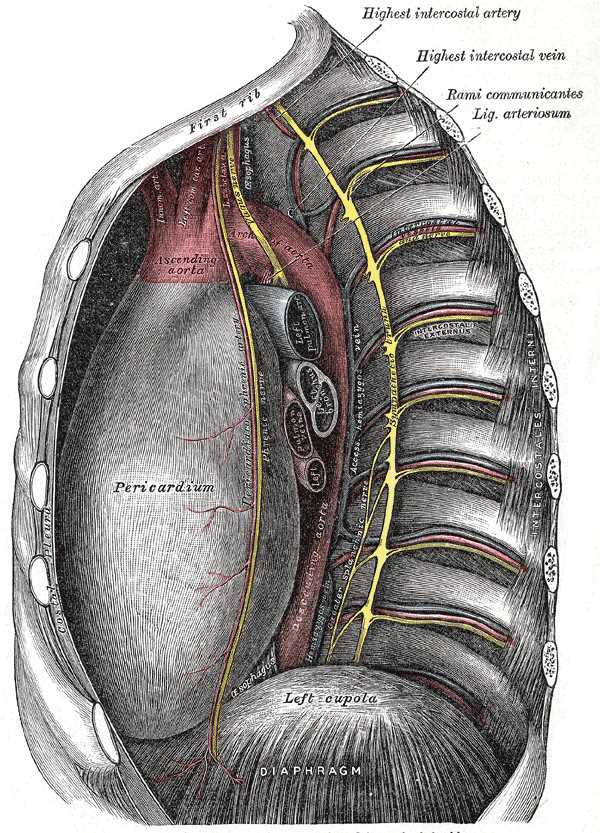
The pericardiacophrenic artery and vein make up, with the phrenic nerve, the pericardiacophrenic neurovascular bundle. The vessels pass through the superior thoracic aperture into the superior mediastinum and course along the pathway of the phrenic nerve anterior to the lung roots. The vessels are located between the fibrous pericardium and the parietal pleura in the middle mediastinum and extend inferiorly onto the dome of the diaphragm.[1]
The pericardiacophrenic artery supplies blood to the pericardium, diaphragm, and phrenic nerve. While the pericardiacophrenic arteries supply blood to these various tissues, they are also a non-coronary arterial collateral blood supply to the heart.[2][3] Their most important role clinically is to supply the phrenic nerve with blood when harvesting or surgically anastomosing the internal thoracic artery, as in CABG procedures, preserving blood flow in the pericardiacophrenic artery is important to prevent any ischemic damage to the phrenic nerve.
The pericardiacophrenic veins are variable tributaries of the right and left brachiocephalic veins (also formerly known as the innominate veins) or internal thoracic veins. The pericardiacophrenic veins are a minor portocaval anastomosis connecting splenic vein and superior vena cava and can become engorged in portal hypertension. Imaging the pericardiacophrenic veins (or arteries) is a reliable aid in clinical procedures that require locating the phrenic nerve.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The right pericardiacophrenic artery courses caudally between fibrous pericardium and pleura along the right margin of the heart as it accompanies the phrenic nerve anterior to the root of the lung to the diaphragm. The left pericardiacophrenic artery is displaced laterally by the developing heart and passes along the left (obtuse) margin of the heart to the diaphragm, also in the company of the phrenic nerve. The pericardiacophrenic artery arises from the internal thoracic artery, a branch of the first part of the subclavian artery.[4] It is the first and most superior segmental branch coming off the internal thoracic artery on its medial side. It exits the internal thoracic artery opposite the first anterior intercostal artery, which extends laterally under the first rib. The artery takes a sharp turn inferiorly into the thorax to accompany the phrenic nerve soon after the latter enters the superior thoracic aperture. It runs between the costal parietal pleura and the fibrous pericardium in the company of the phrenic nerve and the pericardiacophrenic vein. The neurovascular bundle so formed runs bilaterally along the obtuse margin of the heart on the left side and the right margin of the heart, anterior to the roots of the lung.
The pericardiacophrenic arteries travel between the pleura and pericardium and constitute a collateral blood supply to the coronary arteries to the heart.[2][3] These arterial anastomoses help supply oxygen during myocardial infarctions and cardiac ischemia, although their contribution alone is insufficient to meet the demands of myocardial tissue. The vessels continue to course along the pericardium and onto the diaphragm anastomosing with the musculophrenic, superior phrenic, and inferior phrenic arteries. This pathway also helps to provide oxygen to the diaphragm.[2][5]
The pericardiacophrenic veins, which are veni communicantes, each of which can be single or double, begin on the anterosuperior aspect of the diaphragm and drain superiorly into the brachiocephalic veins directly or via their internal thoracic venous tributaries.
Embryology
The long course of the pericardiacophrenic vessels through the thorax is mostly determined by the course of the accompanying phrenic nerve, which derives from cervical spinal nerves 3, 4, and 5 and then descends through the superior thoracic aperture traversing the thorax on its way to innervate the diaphragm. The phrenic nerve is pulled caudally during embryogenesis as the septum transversum, a major primordium of the diaphragm, descends from a location craniad to the developing brain by craniocaudal folding to its adult location separating the thorax and abdomen. The phrenic nerve receives its arterial supply from the pericardiacophrenic artery when the nerve passes through the superior thoracic aperture, or at vertebral levels T2-3, the point at which the artery branches off from the internal thoracic artery. The roots and superior-most portions of the phrenic nerve are supplied by the ascending cervical arteries.
The embryological origin of the internal thoracic artery, from which the pericardiacophrenic artery branches, is the eighth intersegmental somatic artery. This embryological artery is the dorsal "aortic arch" directly caudal to the seventh intersegmental somatic artery, which gives rise to the distal subclavian artery.[4] The proximal subclavian artery on the right side derives from aortic arch 4, which gives rise to the aortic arch and descending aorta on the left side.[6] The primordia of the internal thoracic and pericardiacophrenic arteries run roughly perpendicular to the intersegmental somatic arteries and develop from longitudinally oriented ventral somatic anastomoses that connect the ventral extensions of the intersegmental somatic arteries located dorsal (posterior) to the sternum (see Gray's Anatomy, 38th ed, Williams 1995:318). The ascending cervical arteries which supply the superior-most portions of the phrenic nerve are embryological derivatives of the longitudinal anastomoses extending cranially from the seventh dorsal intersegmental arteries.
The pericardiacophrenic veins develop from subcardinal veins draining cranially from the diaphragm and entering into the brachiocephalic veins to flow into the superior vena cava and the right atrium. Venous drainage of the superior-most portion of the phrenic nerve is via deep cervical veins, derived from pre-cardinal veins.
Blood Supply and Lymphatics
The pericardiacophrenic arteries supply blood to the anterior aspect of the fibrous pericardium, to the phrenic nerves along their common course, and to the anterosuperior aspect of the diaphragm, where the arteries terminate via anastomosis with the musculophrenic artery (also a branch of the internal thoracic artery), and superior phrenic and inferior phrenic arteries (somatic body wall arteries).
Nerves
The pericardiacophrenic vessels course along the pathway of the phrenic nerve, anterior to the lung hilum, and splay out at the pericardium to provide blood to the pericardial sac, diaphragm, and phrenic nerve. The pericardiacophrenic arteries are essential for blood supply for the phrenic nerve.[7] It is vital to keep intact during the harvesting of the internal thoracic artery during cardiac bypass, as injury or ligation can cause ischemic changes to the phrenic nerve. The phrenic nerve carries somatic efferent fibers to the diaphragm and visceral afferent fibers from its region of distribution.
Surgical Considerations
During ablation surgery for atrial fibrillation, CTA imaging of the pericardiacophrenic artery can accurately locate the phrenic nerve within the pericardiacophrenic neurovascular bundle, thus avoiding damage to the nerve.[8]
During the placement of a central venous line, the pericardiacophrenic vein can be accidentally catheterized, instead of the superior vena cava, using the internal jugular approach.[9]
In a transradial approach for percutaneous coronary artery intervention, there is a risk of perforating the pericardiacophrenic artery during wire advancement intended for the aorta because the aorta and the pericardiacophrenic artery can appear to have similar parallel courses.[10]
Clinical Significance
Hemoptysis resulting from anterior lung lesions that have eroded the pleural linings can involve the pericardiophrenic arteries.[11] While this is an infrequent occurrence, it is possible that evolving lung tumors can erode into the neighboring structures and result in blood loss and hemoptysis. Additionally, during internal thoracic artery harvesting, it is possible that ligation of the pericardiacophrenic artery can result in ischemia of the neighboring phrenic nerve. As previously established, the vessel is important in helping supply blood to the cardiac segment of the phrenic nerve.[11]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Stoddard N, Heil JR, Lowery DR. Anatomy, Thorax, Mediastinum. StatPearls. 2023 Jan:(): [PubMed PMID: 30969641]
Picichè M. Noncoronary Collateral Myocardial Blood Flow: The Human Heart's Forgotten Blood Supply. The open cardiovascular medicine journal. 2015:9():105-13. doi: 10.2174/1874192401509010105. Epub 2015 Dec 21 [PubMed PMID: 27006713]
Shahoud JS, Kerndt CC, Burns B. Anatomy, Thorax, Internal Mammary (Internal Thoracic) Arteries. StatPearls. 2023 Jan:(): [PubMed PMID: 30726022]
Rahimi O, Geiger Z. Anatomy, Thorax, Subclavian Arteries. StatPearls. 2023 Jan:(): [PubMed PMID: 30969558]
Oliver KA, Ashurst JV. Anatomy, Thorax, Phrenic Nerves. StatPearls. 2023 Jan:(): [PubMed PMID: 30020697]
Kau T, Sinzig M, Gasser J, Lesnik G, Rabitsch E, Celedin S, Eicher W, Illiasch H, Hausegger KA. Aortic development and anomalies. Seminars in interventional radiology. 2007 Jun:24(2):141-52. doi: 10.1055/s-2007-980040. Epub [PubMed PMID: 21326792]
Jiang S, Xu WD, Shen YD, Xu JG, Gu YD. An anatomical study of the full-length phrenic nerve and its blood supply: clinical implications for endoscopic dissection. Anatomical science international. 2011 Dec:86(4):225-31. doi: 10.1007/s12565-011-0114-x. Epub 2011 Oct 13 [PubMed PMID: 21993978]
Horton R, Di Biase L, Reddy V, Neuzil P, Mohanty P, Sanchez J, Nguyen T, Mohanty S, Gallinghouse GJ, Bailey SM, Zagrodzky JD, Burkhardt JD, Natale A. Locating the right phrenic nerve by imaging the right pericardiophrenic artery with computerized tomographic angiography: implications for balloon-based procedures. Heart rhythm. 2010 Jul:7(7):937-41. doi: 10.1016/j.hrthm.2010.03.027. Epub 2010 Mar 25 [PubMed PMID: 20348030]
Belda FJ, Frasquet FJ, Maruenda A, Almenar L, Rufino A, Company R, Chulia V. [Malpositioning of central venous catheters using the internal jugular vein approach. Accidental catheterization of the internal thoracic and pericardiacophrenic veins]. Revista espanola de anestesiologia y reanimacion. 1981 Nov:28(6):306-10 [PubMed PMID: 7330378]
Arsanjani R, Echeverri J, Movahed MR. Successful coil embolization of pericardiacophrenic artery perforation occurring during transradial cardiac catheterization via right radial artery. The Journal of invasive cardiology. 2012 Dec:24(12):671-4 [PubMed PMID: 23220984]
Level 3 (low-level) evidenceBhasin A, Venkatesh SK, Caleb MG. Pericardiophrenic artery embolisation for control of massive haemoptysis. Singapore medical journal. 2011 May:52(5):e104-7 [PubMed PMID: 21633756]
Level 3 (low-level) evidence