 Anatomy, Bony Pelvis and Lower Limb: Lateral Circumflex Femoral Artery
Anatomy, Bony Pelvis and Lower Limb: Lateral Circumflex Femoral Artery
Introduction
The femoral artery is the branch of the external iliac artery, passing inferiorly to the inguinal ligament. It serves as the lower limb's primary blood supply. The deep femoral artery (profunda femoris artery) is the main branch of the common femoral artery. Its largest branches are the medial and lateral femoral circumflex arteries (see Image. Branches of the Femoral Artery).
The medial femoral circumflex artery branches out posteromedially from the deep femoral artery, while the lateral femoral circumflex artery diverges posterolaterally from the same source.[1][2] The lateral femoral circumflex artery supplies blood to the femoral head and neck, greater trochanter, vastus lateralis, and knee.[2]
The lateral femoral circumflex artery is clinically significant because it can get injured during hip joint surgery. It is also useful as a vascular graft for coronary artery bypass graft surgery and similar procedures.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The lateral femoral circumflex artery supplies the soft tissues surrounding the hip joint.[3] After bifurcating from the deep femoral artery, it courses laterally between the divisions of the femoral nerve. It then travels inferiorly into the septum between the sartorius and rectus femoris muscles, where it further divides into the ascending, transverse, and descending lateral femoral circumflex arteries.[4][5][6]
Ascending Branch
The ascending branch of the lateral femoral circumflex artery bifurcates into muscular and capsular branches approximately 11 cm distal to the anterior superior iliac spine. These branches supply the femoral neck (at the intertrochanteric line), the anterior hip capsule, and the anterior portion of the femoral neck.[7]
The ascending branch of the lateral femoral circumflex artery supplies approximately 18% of the blood supply to the femoral head, mostly on its anterior aspect.[7] One anatomical study found that the medial femoral circumflex artery supplies about two-thirds of the femoral neck. The lateral femoral circumflex artery covers the remainder, specifically on the anteroinferior aspect.[7]
Descending Branch
Distal to its branch point, the descending branch of the lateral femoral circumflex artery courses inferiorly, medial to the vastus lateralis muscle.[4][5] Lateral branches from the descending lateral femoral circumflex artery take either of two possible paths. One group perforates the vastus lateralis. The other travels within the muscular septum until the terminal arteries reach the skin overlying the anterolateral thigh. Medial branches from the descending lateral femoral circumflex artery course medially, deep to the rectus femoris. They supply the rectus femoris muscle and the skin overlying the anteromedial thigh.[4]
Embryology
Ogden previously described how the circulation in the femoral head area develops.[8]
In the first few years of life, the lateral and medial femoral circumflex arteries cover areas of nearly equal sizes. The lateral femoral circumflex artery supplies the anterior aspect of the proximal femur and cartilaginous epiphysis. Its medial counterpart provides circulation to the posterior side.
Over time, the area supplied by the lateral femoral circumflex diminishes until only the junction between the anterior femoral neck and metaphysis remains. Meanwhile, the medial femoral circumflex expands to include the growing femoral neck and eventually becomes the dominant arterial source of the femoral head.
This arterial reorganization increases the risk of ischemic injury to the anterolateral capital femoral epiphysis as one matures.[7][8]
Physiologic Variants
Studies reveal variations in the branching patterns of the femoral vessels. In most people, the lateral femoral circumflex artery branches out from the deep femoral artery just superior to the origin of the medial femoral circumflex artery. Occasionally, the lateral and medial femoral circumflex arteries bifurcate from the deep femoral artery at the same level. The lateral femoral circumflex artery may also directly diverge from the femoral artery above or below the bifurcation of the deep femoral artery from the femoral artery.[1]
Tomaszewski and colleagues classified the lateral femoral circumflex artery branching patterns as follows:[9]
- Type 1 (most common): The lateral femoral circumflex artery branches out from the deep femoral artery superior to the medial femoral circumflex artery's origin.
- Type 2: The lateral femoral circumflex artery diverges from the common femoral artery above the origin of the deep femoral artery.
- Type 3: The lateral femoral circumflex artery bifurcates from the common femoral artery at the level of the deep femoral artery's origin.
- Type 4: The lateral femoral circumflex artery branches out from the superficial femoral artery.
- Type 5: The lateral ascending and lateral descending branches of the lateral femoral circumflex artery do not originate from a common branch. Instead, they diverge individually from the common femoral artery, deep femoral artery, or superficial femoral artery.
Other anatomic investigations have reported similar findings.[3] Another study revealed that femoral vessel diameter was greater in males than in females.[1]
Prakash and colleagues hypothesized that the anatomic variations of the femoral artery branches exist due to an evolutionary shift in the deep femoral artery's origin. The deep femoral artery used to be a branch of the internal iliac artery, but with evolution, it now branches out from the femoral artery.[10]
Surgical Considerations
Injuries to the lateral and medial femoral circumflex arteries may result in avascular necrosis of the femoral head. Hip joint surgery risks damage to these blood vessels. The lateral circumflex femoral artery and its branches are more vulnerable to injury during femoral neck surgery due to their anterior course. Knowledge of the branching pattern variations of these blood vessels can help reduce iatrogenic risk.[1][7]
Other procedures that risk injury to lateral femoral circumflex arteries are the following:[1][6][11][12][13]
- Vascular interventional procedures that use the femoral approach, such as catheterization, stenting, embolectomy, angiography, and angioplasty
- Using the artery for bypass grafting, for example, of the coronary arteries and posterior inferior cerebellar artery
- Using the artery in vascular reconstruction, for example, in the oropharyngeal area
- Intramuscular injections of the anterior thigh, including ultrasound-guided hip joint injections
Reconstructive surgeries sometimes make use of anterolateral thigh flaps. The lateral circumflex femoral artery, its septocutaneous branches, and the musculocutaneous perforators supply these soft-tissue flaps.[4][5]
Clinical Significance
Femoral neck fractures and procedures involving the lateral femoral circumflex artery risk ischemic damage to the femur and the surrounding areas.[7] Besides limited mobility, other complications may arise from such injuries. Pseudoaneurysms of the deep femoral artery and the left and right femoral circumflex arteries have also been reported in patients with a history of intertrochanteric hip fracture. These lesions may present as profuse bleeding or hematoma after the injury or its surgical treatment, which can be catastrophic to individuals with poor cardiac function.[14]
Media
(Click Image to Enlarge)
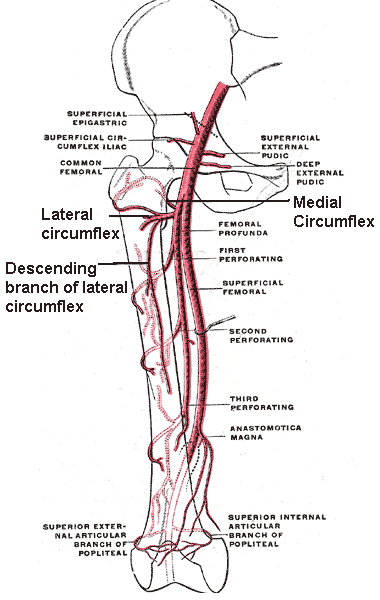
Branches of the Femoral Artery. This illustration shows the following structures: common femoral artery, deep femoral artery (femoral profunda), superficial femoral artery, perforating arteries, lateral circumflex artery, medial circumflex artery, descending branch of the lateral circumflex artery, anastomotica magna, and superior external and internal articular branches of the popliteal artery.
Mikael Häggström, Public Domain, via Wikimedia Commons
References
Łabętowicz P, Olewnik Ł, Podgórski M, Majos M, Stefańczyk L, Topol M, Polguj M. A morphological study of the medial and lateral femoral circumflex arteries: a proposed new classification. Folia morphologica. 2019:78(4):738-745. doi: 10.5603/FM.a2019.0033. Epub 2019 Mar 25 [PubMed PMID: 30906974]
Tomaszewski KA, Henry BM, Vikse J, Roy J, Pękala PA, Svensen M, Guay DL, Saganiak K, Walocha JA. The origin of the medial circumflex femoral artery: a meta-analysis and proposal of a new classification system. PeerJ. 2016:4():e1726. doi: 10.7717/peerj.1726. Epub 2016 Feb 29 [PubMed PMID: 26966661]
Level 1 (high-level) evidenceZlotorowicz M, Czubak-Wrzosek M, Wrzosek P, Czubak J. The origin of the medial femoral circumflex artery, lateral femoral circumflex artery and obturator artery. Surgical and radiologic anatomy : SRA. 2018 May:40(5):515-520. doi: 10.1007/s00276-018-2012-6. Epub 2018 Apr 12 [PubMed PMID: 29651567]
Artero GE, Ulla M, Neligan PC, Angrigiani CH. Bilateral Anatomic Variation of Anterolateral Thigh Flap in the Same Individual. Plastic and reconstructive surgery. Global open. 2018 May:6(5):e1677. doi: 10.1097/GOX.0000000000001677. Epub 2018 May 18 [PubMed PMID: 29922539]
Valdatta L, Tuinder S, Buoro M, Thione A, Faga A, Putz R. Lateral circumflex femoral arterial system and perforators of the anterolateral thigh flap: an anatomic study. Annals of plastic surgery. 2002 Aug:49(2):145-50 [PubMed PMID: 12187341]
Goel S, Arora J, Mehta V, Sharma M, Suri RK, Rath G. Unusual disposition of lateral circumflex femoral artery: Anatomical description and clinical implications. World journal of clinical cases. 2015 Jan 16:3(1):85-8. doi: 10.12998/wjcc.v3.i1.85. Epub [PubMed PMID: 25610855]
Level 3 (low-level) evidenceDewar DC, Lazaro LE, Klinger CE, Sculco PK, Dyke JP, Ni AY, Helfet DL, Lorich DG. The relative contribution of the medial and lateral femoral circumflex arteries to the vascularity of the head and neck of the femur: a quantitative MRI-based assessment. The bone & joint journal. 2016 Dec:98-B(12):1582-1588 [PubMed PMID: 27909118]
Ogden JA. Changing patterns of proximal femoral vascularity. The Journal of bone and joint surgery. American volume. 1974 Jul:56(5):941-50 [PubMed PMID: 4847241]
Tomaszewski KA, Vikse J, Henry BM, Roy J, Pękala PA, Svensen M, Guay D, Saganiak K, Walocha JA. The variable origin of the lateral circumflex femoral artery: a meta-analysis and proposal for a new classification system. Folia morphologica. 2017:76(2):157-167. doi: 10.5603/FM.a2016.0056. Epub 2016 Oct 7 [PubMed PMID: 27714726]
Level 1 (high-level) evidencePrakash, Kumari J, Kumar Bhardwaj A, Jose BA, Kumar Yadav S, Singh G. Variations in the origins of the profunda femoris, medial and lateral femoral circumflex arteries: a cadaver study in the Indian population. Romanian journal of morphology and embryology = Revue roumaine de morphologie et embryologie. 2010:51(1):167-70 [PubMed PMID: 20191139]
Level 2 (mid-level) evidenceNakajima Y, Fujii T, Mukai K, Ishida A, Kato M, Takahashi M, Tsuda M, Hashiba N, Mori N, Yamanaka A, Ozaki N, Nakatani T. Anatomically safe sites for intramuscular injections: a cross-sectional study on young adults and cadavers with a focus on the thigh. Human vaccines & immunotherapeutics. 2020:16(1):189-196. doi: 10.1080/21645515.2019.1646576. Epub 2019 Aug 23 [PubMed PMID: 31403356]
Level 2 (mid-level) evidenceZhang M, Pessina MA, Higgs JB, Kissin EY. A Vascular Obstacle in Ultrasound-Guided Hip Joint Injection. Journal of medical ultrasound. 2018 Apr-Jun:26(2):77-80. doi: 10.4103/JMU.JMU_8_17. Epub 2018 Jun 12 [PubMed PMID: 30065523]
Strickland BA, Bakhsheshian J, Rennert RC, Fredrickson VL, Lam J, Amar A, Mack W, Carey J, Russin JJ. Descending Branch of the Lateral Circumflex Femoral Artery Graft for Posterior Inferior Cerebellar Artery Revascularization. Operative neurosurgery (Hagerstown, Md.). 2018 Sep 1:15(3):285-291. doi: 10.1093/ons/opx241. Epub [PubMed PMID: 30125010]
Arbeloa-Gutierrez L, Arenas-Miquelez A, Muñoa L, Gordillo A, Eslava E, Insausti I, Martínez de Morentin J. Lateral circumflex femoral artery false aneurysm as a complication of intertrochanteric hip fracture with displaced lesser trochanter. Journal of surgical case reports. 2019 Jun:2019(6):rjz184. doi: 10.1093/jscr/rjz184. Epub 2019 Jun 18 [PubMed PMID: 31249660]
Level 3 (low-level) evidence