Introduction
Chest Trauma Overview
Chest trauma represents a significant challenge in emergency medicine and trauma care, encompassing a broad spectrum of injuries ranging from minor rib fractures to life-threatening thoracic organ damage. Accidents, falls, assaults, and motor vehicle collisions are common chest trauma etiologies. Chest trauma is the second most frequently occurring unintentional traumatic injury and the third most common cause of death after abdominal injury and head trauma in patients with polytrauma.[1] Chest trauma results in the highest mortality, reaching up to 60%, according to some study results.[2] In patients with severe trauma, 25% of deaths are due to chest trauma.[3] Thus, this condition is a leading contributor to morbidity and mortality worldwide. Injury to any vital midthoracic organ can progress rapidly. Prompt recognition, assessment, and appropriate management of chest trauma are essential to mitigate associated complications and improve patient outcomes.
Anatomy of the Midthoracic Region
A thorough grasp of the pertinent anatomy is paramount to effectively managing chest trauma. The thoracic cage comprises the sternum, ribs, and thoracic vertebrae, providing crucial structural support and safeguarding vital organs within the chest cavity. The mediastinum is the thoracic cavity's central compartment, housing vital structures like the heart, great vessels, trachea, esophagus, and lymph nodes. The lungs are the primary respiratory organs, nestled within the pleural cavities and undertaking pivotal functions such as gas exchange, blood oxygenation, and carbon dioxide elimination. The heart is positioned centrally within the mediastinum, receiving deoxygenated blood from the venous system and ensuring the circulation of oxygenated blood throughout the body.
The great vessels facilitate systemic and pulmonary circulation. These vessels include the aorta, pulmonary artery, superior and inferior vena cavae, and pulmonary veins. The trachea and bronchial tree conduct air from the larynx to the bronchi, further branching into smaller bronchioles and alveoli within the lungs, facilitating vital air exchange. The diaphragm, a domed muscle separating the thoracic and abdominal cavities, aids respiration through its contraction and relaxation.
The esophagus lies adjacent to the trachea and conveys food and liquids from the mouth to the stomach through peristaltic contractions. The pleural space, the potential space between the visceral and parietal pleurae, normally contains a small quantity of lubricating fluid to facilitate smooth lung movement during respiration. The visceral pleura is a thin membrane covering the lungs' surface, closely adhering to their contours. The parietal pleura lines the thoracic cavity's inner surface and is attached to the chest wall, diaphragm, and mediastinum, providing structural support to the lungs and contributing to the maintenance of negative intrapleural pressure.
The intercostal nerves run along the intercostal spaces and provide sensory innervation to the thoracic wall and motor innervation to the intercostal muscles. Phrenic nerves originate from cervical spinal nerves C3 to C5, descending to innervate the diaphragm and regulate breathing. The vagus nerve supplies various thoracic structures, including the heart, lungs, esophagus, and abdominal viscera, contributing to regulating vital functions like cardiac contraction, respiration, and digestion.
The sympathetic chain lies alongside the vertebral column, contributing sympathetic innervation to thoracic organs, blood vessels, and muscles. Splanchnic nerves arise from the sympathetic chain and extend into the abdominal viscera, transmitting sensory and autonomic signals between the thoracic and abdominal regions. The recurrent laryngeal nerve branches from the vagus nerve and supplies sensory innervation to the laryngeal mucosa and motor innervation to the laryngeal muscles, which are crucial for airway protection and vocalization.
The lymphatic drainage of the thoracic region involves a complex network of vessels and nodes that facilitate the return of lymph to the circulatory system. Lymph from the lungs is collected by superficial (subpleural) and deep lymphatic plexuses, which drain into the bronchopulmonary (hilar) nodes. These, in turn, channel lymph to the tracheobronchial nodes around the tracheal bifurcation. The mediastinal lymph nodes, including the paratracheal, anterior, and posterior mediastinal nodes, receive lymph from various thoracic structures, such as the heart, thymus, and esophagus. The thoracic duct, originating from the cisterna chyli, ascends through the thoracic cavity and empties into the junction of the left subclavian and internal jugular veins, collecting lymph from the majority of the body except the right upper quadrant.
Conversely, the right lymphatic duct drains lymph from the right upper limb, right side of the thorax, and right side of the head and neck into the junction of the right subclavian and internal jugular veins. Intercostal lymph nodes, situated along the posterior intercostal spaces, drain the thoracic wall and parietal pleura, with their efferent vessels connecting to the thoracic duct or right lymphatic duct, depending on their location. The breast's lymphatic drainage primarily involves the axillary lymph nodes, which receive approximately 75% of the lymph, while the remaining drainage is directed to the parasternal (internal mammary) nodes. This organized system ensures efficient lymphatic drainage from thoracic structures, maintaining fluid balance and facilitating immune surveillance.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Chest trauma can result from penetrating or blunt trauma. Blunt trauma is a more common cause of traumatic injuries and may be life-threatening. The injury mechanism informs both primary and secondary surveys from the care team, especially what type of imaging modalities are indicated and when to involve a surgical consult.[4][5] Motor vehicle collisions (MVCs) are the leading cause of chest trauma. Most acute traumatic aortic injury cases also result from MVCs. Crushing or deceleration is the main cardiac injury mechanism. An open pneumothorax is associated with gunshot injuries.
Blast injuries mainly affect the chest and are increasingly recognized as a public health concern due to the rise in terrorist activities. These injuries occur in 5 stages. The primary blast injury results from the overpressure of the blast wave, causing barotrauma in gas-filled organs such as the lungs, gastrointestinal tract, and middle ear. Subsequently, clinical effects include pulmonary barotrauma, tympanic membrane rupture, and abdominal hemorrhage or perforation. This constellation of signs and symptoms is very useful in guiding management, and the presence of 1 should lead to the investigation of the others. Secondary blast injuries follow as shrapnel and debris propelled by the explosion cause penetrating or blunt trauma, often leading to lacerations, fractures, and penetrating wounds. Tertiary injuries occur when the force of the blast throws individuals against objects or the ground, leading to blunt force trauma, fractures, traumatic amputations, and brain injuries. Quaternary injuries arise from explosion-related factors like burns, inhalation of toxic gases, and crush injuries from structural collapse. Finally, quinary injuries involve systemic effects caused by exposure to hazardous materials, including chemical burns, radiation sickness, or infections.
While the primary, secondary, and tertiary stages result in direct tissue damage, quaternary and quinary injuries often lead to systemic complications, such as a massive cytokine surge that can precipitate acute respiratory distress syndrome (ARDS). In some cases, patients may exhibit no external injuries, with internal damage only detected through imaging studies, though external injuries are more commonly present. Treatment focuses on clinical symptoms rather than solely relying on radiographic findings. Survivors who reach medical facilities often succumb to complications unrelated to thoracic trauma. Surgical intervention is generally reserved for specific situations, with nonanatomic resection being the hallmark approach when required. The management of blast lung injury primarily involves intensive care, emphasizing lung-protective ventilatory strategies for ARDS.
Epidemiology
Chest trauma is one of the most common blunt injuries affecting patients of all ages. The 2016 Pediatric Report of the National Trauma Data Bank documented that chest injuries had the highest fatality rate by body region. MVC is the most common cause of these fatal conditions. Pulmonary contusion is more common in children compared to rib fractures.[6] Pneumothorax occurs in 30% of chest trauma. Recent data indicates that 36% of trauma deaths in the United States are potentially preventable. Among these, thoracic injuries account for 41%, with blunt trauma as the primary mechanism (80% to 92%).
Delayed treatment, inadequate management, and treatment errors are the primary causes of preventable deaths.[7] Older adults have a higher mortality rate than younger patients with similar injuries; a single rib fracture in an older patient doubles the mortality risk compared to a younger individual with the same injury. Mortality increases by 19% and the pneumonia risk by 27% for each additional rib fractured. Children are more prone to developing hypoxia when their functional reserve is depleted.
Pathophysiology
Blunt or Penetrating Trauma
Thoracic injury is classified into blunt and penetrating. Blunt trauma imparts kinetic energy to the point of impact and causes direct damage to the chest and more distant sites. Penetrating trauma transfers kinetic energy into the tissues involved and is related to the square of the projectile velocity. Impairments at either the chest wall, musculature, or gas exchange influence breathing.
Pneumothorax
Pneumothorax is the accumulation of air in the pleural space from a breach in the visceral or parietal pleura, leading to lung collapse and symptoms such as chest pain and difficulty breathing. Tension pneumothorax occurs when a "flutter valve " forms, facilitating unidirectional airflow into the pleural space and increasing pleural gas volume and pressure. An open pneumothorax may occur when chest trauma creates communication between the chest cavity and the external environment.
Hemothorax
Hemothorax is the accumulation of blood within the pleural cavity, most commonly resulting from traumatic chest injuries. Clinically, this condition presents with signs such as diminished breath sounds, dullness to percussion, and varying degrees of respiratory distress. In severe cases, hemothorax can lead to hypovolemic shock if not addressed promptly. The condition arises from various mechanisms, including blunt trauma, where rib fractures may damage intrathoracic vasculature, and penetrating trauma, often caused by stab or gunshot wounds that injure intercostal vessels, internal mammary arteries, or pulmonary vasculature.
Complications can arise if hemothorax is not adequately managed. Retained blood within the pleural cavity may lead to infection, resulting in empyema or fibrothorax, where pleural fibrosis restricts lung expansion. Prompt diagnosis and treatment are essential for improving outcomes, as delays can significantly increase morbidity and mortality. The prognosis largely depends on the injury's severity and the intervention's timeliness.
Chylothorax
Chylothorax is characterized by the accumulation of chyle—a lipid-rich lymphatic fluid—in the pleural cavity. This condition arises when the thoracic duct, the primary conduit for lymphatic drainage from the gastrointestinal tract and lower body, is compromised. Such compromise can result from traumatic events, including surgical interventions, or from nontraumatic causes like malignancies or congenital lymphatic anomalies. The disruption leads to chyle leakage into the pleural space, which can cause respiratory distress, nutritional deficiencies, and immunosuppression due to the loss of lymphocytes and immunoglobulins. Management strategies depend on the underlying cause and may involve dietary modifications, drainage procedures, and, in persistent cases, surgical interventions to repair the thoracic duct or redirect lymphatic flow.
Pediatric Considerations
Greater kinetic energy transfer occurs in children as their chest wall is more pliant and compressible. The pediatric mediastinum's increased mobility allows it to readily shift to the contralateral side, facilitating robust compensation until tension physiology ensues and shock manifests. Cardiac output is relatively fixed during early life. Therefore, younger patients can remain normotensive despite significant blood volume loss. In the early phases, hypotension develops when all physiological compensatory mechanisms are exhausted. Children have an increased hypoxia risk due to this cohort's lower functional residual capacity and higher tissue oxygen consumption.
History and Physical
Individuals with chest trauma may present with various signs and symptoms, ranging from alarming apnea, unresponsiveness, and inaudible cardiac tone to innocuous skin discoloration. The primary survey must be quick, assessing the airway, breathing, circulation, disability, and exposure, according to the Advanced Trauma Life Support guidelines.[8] Resuscitation must be immediately started, simultaneously addressing significant injuries such as hemorrhage sites. A more detailed secondary survey may be completed after stabilizing the patient.
History
Conscious patients with chest trauma may complain of chest pain, dyspnea, hemoptysis, palpitations, or sensations of pressure or tightness in the chest. Associated symptoms such as dizziness, nausea, and diaphoresis may be reported if significant bleeding or cardiac injury occurs. Pain, deformity, and loss of function in other sites may be present in polytrauma cases. Flank or abdominal pain may be elicited in patients with a concomitant abdominal injury. Individuals with esophageal injuries often present with odynophagia, dysphagia, and hematemesis. Chest or back pain may also suggest esophageal injuries. Loss of consciousness may be a sign of significant blood loss, hypoxia, or concomitant brain injury. The injury mechanism must be explored.
Chest trauma most commonly arises from MVCs, falls, assaults, and penetrating injuries. The event's circumstances, including the force direction and impact, must be noted. Extensive vehicle damage, passenger space intrusion, prolonged extrication, airbag deployment, and steering wheel damage are all risk factors for significant injury in MVCs and must be assessed during history-taking. The patient's past medical history helps guide overall management.
Medical conditions that often impact trauma interventional approaches include diabetes mellitus, cardiovascular disease, coagulopathies, chronic lung disease, immunosuppression, and renal impairment. Exploring the patient's social history, including factors like tobacco use, alcohol consumption, drug use, and occupational or recreational activities, may provide additional clues relevant to injury management. A review of systems allows for the identification of any injuries that may have occurred concurrently with the chest trauma.
Physical Examination
Physical examination findings increase suspicion of chest trauma. Early recognition of life-threatening injuries is a priority. The following conditions should be quickly identified and addressed:
- Airway obstruction or rupture
- Tension pneumothorax
- Cardiac tamponade
- Massive hemothorax
- Flail chest
When the initial exam is complete and adjunct imaging is complete, a secondary survey is indicated that may reveal the following:
- Rib fractures
- Small hemothorax
- Small pneumothorax
- Pulmonary contusion
- Chest wall contusion
Potentially serious hidden injuries requiring a higher level of suspicion include the following:
- Tracheobronchial injury
- Aortic injury
- Myocardial contusion
- Pulmonary contusion
- Diaphragmatic rupture
- Esophageal rupture
Patients with significant hemorrhage, prolonged hypoxia, or severe brain injury may be unconscious. Findings suspicious of hemodynamic instability in a conscious individual include tachycardia, tachypnea, hypotension, and hypoxemia. Tachyarrhythmias may also be noted on the cardiac monitor, either from blood loss or myocardial trauma. An aortic root disruption may lead to rapid death due to blood loss, pericardial bleeding, and tamponade. Inspection should include evaluation for bruising, abrasions (for example, the "seat belt sign"), and penetrating wounds. Agitated or uncooperative individuals may have alcoholic breath. On auscultation, diminished breath sounds may suggest hemothorax or pneumothorax, and percussion can help differentiate between them. Chest wall contusions with a seatbelt pattern may produce point tenderness over the ribs. Crepitus and point tenderness on palpation signify pneumothorax or pneumomediastinum.
The diagnosis of tension pneumothorax is clinical—patients with tension pneumothorax present with respiratory distress, tachypnea, and hypoxia. Decreased or absent breath sounds occur on the affected side. The trachea is deviated away from the affected side. Neck veins may be distended. In patients with hypovolemia, the neck veins may not be distended. Pulmonary contusion should be suspected in patients with chest wall injury, especially if presenting with hypoxia. The degree of hypoxia often correlates with contusion size.[9][10] The physical examination must also assess for concomitant injuries. A detailed vascular examination is warranted, including bilateral pulse and upper extremity blood pressure. Patients who present unconscious but are resuscitated and stabilized require a complete neurologic examination.
Evaluation
The diagnostic process for chest trauma involves performing imaging, laboratory, and physiologic studies, aiding in timely diagnosis, risk stratification, and appropriate management to optimize patient outcomes. The choice of diagnostic tests must be clinically guided. The roles of the most important modalities are explained below.
Chest Radiography
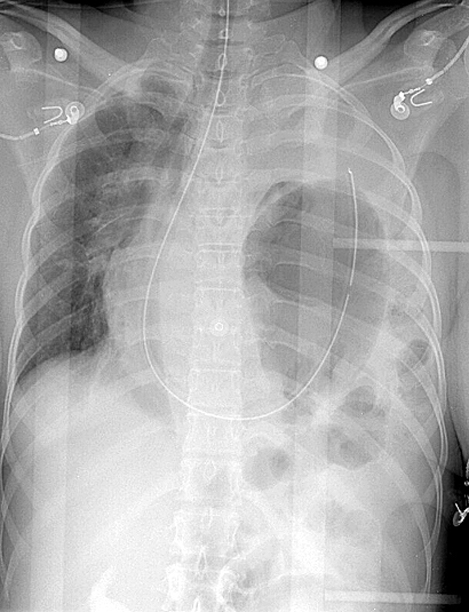
A portable chest radiograph is required in most trauma codes (see Image. X-Ray, Blunt Chest Trauma). However, the diagnosis of tension pneumothorax is clinical. If suspected, rapid decompression must be immediately performed. Radiographic confirmation is often not necessary for intervention. However, traditional physical examination indicators like tracheal deviation and distended neck veins exhibit low sensitivity when diagnosing tension pneumothorax. Point-of-care ultrasound provides accurate identification of tension pneumothorax.[11] In supine chest radiography, small- and medium-sized pneumothoraces and hemothoraces may be missed. An aortic injury should be suspected in the presence of a widened mediastinum, apical capping, aortic knob loss, or left mainstem bronchus deviation. A ratio of over 25% of the chest width is useful in determining mediastinal widening. An occult pneumothorax is suspected if a deep costophrenic sulcus, hemidiaphragm hyperlucency, and an abnormally well-defined mediastinal or cardiac border are evident.[12][13][14]
A chest trauma decision tool has been developed by the National Emergency X-Radiography Utilization Study (NEXUS) group as a potential strategy to minimize healthcare costs and unnecessary imaging burden on both the patient and the clinician. By employing 7 clinical criteria to assess the likelihood of thoracic injuries that are clinically significant on imaging and warrant further evaluation with computed tomography (CT), this instrument demonstrated a sensitivity of 99.7% and a negative predictive value of 99.9%. The NEXUS chest decision tool assigns a point for each of the following criteria: aged 60 years or older, a rapid deceleration mechanism such as a fall from over 20 feet or a motor vehicle collision exceeding 40 mph, the presence of chest pain, intoxication, altered mental status, a distracting painful injury, and tenderness upon palpation of the chest wall. For well-appearing individuals without signs of multiorgan injury who meet any of these criteria, a chest x-ray alone may be sufficient without the need for CT imaging. However, in patients who appear unwell or require further evaluation for significant injuries, the addition of a chest CT should be considered.[15][16][17][18]
Focused Assessment with Sonography in Trauma
Traditional Focused Assessment with Sonography in Trauma (FAST) has 4 views: the cardiac (subxiphoid) window, right upper quadrant (Morrison pouch), left upper quadrant, and suprapubic (bladder) window. In contrast, the extended FAST (eFAST) includes bilateral pulmonary views to evaluate for pneumothorax and hemothorax, besides traditional FASTS’s 4 views. This exam should be started in the area with the highest suspicion of injury. If the thorax is of concern, then eFAST should start in this area. A black collection outside an organ, viscera, or pericardia suggests the presence of free fluid in the area. Free fluid found on eFAST usually indicates the presence of blood.
The eFAST may evaluate the anterior chest wall between the ribs to search for pneumothorax. Bedside eFAST is more sensitive when evaluating pneumothorax than supine chest radiography. An ultrasound probe may be placed on the chest to assess lung sliding, but this absence suggests pneumothorax. The spinal stripe appears as a bright line parallel to the ribs and represents a reverberation artifact produced by the interface between the ribs and the air-filled lung tissue. Normal lung sliding on ultrasound appears as a "marching ants" pattern or "sandy beach" on ultrasound M-mode. The absence of pleural sliding, combined with a "stratosphere" or "barcode" sign on M-mode, is almost pathognomonic for pneumothorax with a specificity of 99%.[19][20] In acute trauma, finding the spinal stripe superior to the diaphragm in the right and left upper quadrant windows helps identify hemothorax.[21][22][23][24] The eFAST should be completed during the primary survey to direct definitive management, especially in unstable patients.
Computed Tomography
CT scan is more sensitive and specific for evaluating midthoracic structures than radiography or ultrasonography (see Image. Blunt Chest Trauma on Computed Tomography). This imaging modality is definitive in patients with chest trauma, helping to identify serious injuries more reliably. A CT scan may show pericardial effusion or hemopericardium in patients with cardiac injury. However, the patient should be hemodynamically stable throughout the test. Spiral chest CT angiography should be obtained in patients with high-energy injury mechanisms to evaluate for aortic injury. Findings suggestive of aortic injury include intimal flaps, pseudoaneurysm formation, abnormal aortic contour, and a sudden aortic caliber change. The following classification helps assess the severity of aortic injury:
- Grade I: Intimal disruption
- Grade II: Intramural hematoma
- Grade III: Pseudoaneurysm
- Grade IV: Aortic rupture
Most aortic injuries are located at the aortic isthmus, around 2 cm distal to the left subclavian artery’s origin. An occult intimal injury should be suspected if a hematoma is immediately adjacent to the aorta without evidence of another aortic injury.
Blood Tests
Blood tests that may be crucial in evaluating patients with chest trauma include a complete blood count, coagulation studies, blood typing, arterial blood gases, cardiac enzymes, and blood glucose. The complete blood count can help identify anemia, which may indicate acute blood loss. Leukocytosis suggests infection or inflammation. Thrombocytopenia may be observed in patients with significant bleeding or disseminated intravascular coagulation. Coagulation studies may reveal abnormalities in clotting function and guide appropriate management to minimize bleeding complications. Blood typing helps identify compatible blood products for potential transfusion in significant hemorrhage cases or if surgery is contemplated. Arterial blood gas analysis provides valuable insights into respiratory function and acid-base balance in patients with hypoxemia or shock. Cardiac biomarkers may be indicated if a myocardial injury is suspected, ie, based on clinical presentation and electrocardiography (ECG). Glucose levels should be monitored in patients who are unconscious or with a known history of diabetes mellitus.[25]
Electrocardiography
ECG assesses for potential cardiac involvement in acute trauma settings. This modality can help identify conduction abnormalities, myocardial ischemia, and signs of cardiac contusion. Specifically, findings such as ST-segment elevation or depression, T-wave abnormalities, new-onset bundle branch blocks, or dysrhythmias may indicate cardiac injury. However, a normal ECG does not rule out cardiac injury. Additional imaging studies, clinical evaluation, and cardiac biomarkers are often necessary to assess patients with blunt chest trauma and suspected cardiac or vascular injury comprehensively. The role of electrocardiography in chest thoracic trauma may grow in the coming years due to the implementation of artificial intelligence to interpret cardiac function.[26]
Imaging Adjuncts
Imaging adjuncts include endoscopy and bronchoscopy to assess for esophageal and pulmonary injuries, respectively.[27][28] A CT scan followed by an esophagogram should be obtained to determine esophageal injury if a chest wound is near the esophagus. Major thoracic trauma rarely occurs in isolation. Associated injuries are often present. Some injuries are challenging to diagnose and require increased suspicion, such as traumatic aortic injury, tracheobronchial disruption, and traumatic diaphragmatic tear.
Treatment / Management
Injury-specific interventions are required following the primary survey, prioritizing airway, breathing, and circulation stabilization.[29] Prompt interventions, such as emergent chest tube thoracostomy (CTT), are necessary for managing immediate life-threatening injuries, including large pneumothoraces and hemothoraces. Patients with pneumothorax should receive 100% oxygen via a nonrebreather mask, with needle decompression followed by CTT if tension pneumothorax is suspected.
In hemothorax cases, adequate drainage is imperative to prevent blood retention in the pleural space. Retained hemothorax can lead to empyema requiring video-assisted thoracoscopic surgery.[30] Most thoracic trauma cases can be managed nonoperatively. However, operative management should not be delayed when warranted. Operative thoracic injury exploration should be considered if initial (CTT) drainage exceeds 1000 to 1500 mL, approximately 200 mL per hour for 2 to 4 hours, or hypotension of unknown cause continues despite resuscitation by blood transfusion. Asymptomatic, stable individuals with an occult pneumothorax may not require a CTT. Patients with occult pneumothoraces rarely progress to tension physiology.[31](A1)
Admission
Patients with 3 or more rib fractures, a flail segment, and any number of rib fractures with pulmonary contusions, hemopneumothorax, hypoxia, or preexisting pulmonary disease should be hospitalized. These patients should be monitored at an advanced care level.
Pain Control
Pain management is critical in reducing respiratory complications.[32] Pain control significantly affects mortality and morbidity in patients with chest trauma.[33] Pain leads to splints—involuntary guarding due to pain—which worsen or prevent healing. In many cases, splints can lead to pneumonia. Early analgesia should be considered to decrease splinting. Push doses of short-acting narcotics may be given in the acute setting. Other pain control options include intrapleural nerve blocks, transdermal patches, intravenous analgesia, and epidural analgesia. Nonnarcotic transdermal patches are a safe option and should be considered when chest wall pain persists despite a lack of confirmed rib fractures, an adjunct pain control modality is required, or the patient is discharged.
Antibiotics
A study revealed that prophylactic antibiotics for CTT performed under sterile conditions in blunt thoracic trauma did not reduce the incidence of pneumonia or empyema. Such findings suggest that routine prophylactic antibiotic use may not be necessary in all chest trauma cases where CTT is performed, and their benefits must be evaluated alongside their potential risks, such as antibiotic resistance and adverse reactions.[34](B3)
Operative Management
A careful evaluation is required to identify patients who require surgical intervention. Open reduction and internal fixation have been shown to decrease mortality in patients with flail chest, shorten the duration of mechanical ventilation, reduce hospital stay, and reduce intensive care stay.[35] Most pulmonary contusions require supportive therapy until the contusion heals. Contusions can gradually evolve over the first 24 to 48 hours after trauma. Thus, close monitoring is needed. Treatment aims to prevent respiratory insufficiency, failure, and complications.[36]
Appropriate pain control helps avoid chest muscle splinting that may limit lung expansion. Supportive care like postural drainage, suctioning, chest physiotherapy, incentive spirometry, encouraging coughing, and deep breathing are attempted to prevent atelectasis. Bilevel or continuous positive airway pressure may be used for positive pressure ventilation.[37] Minimum positive end-expiratory pressure is necessary to keep the lungs open, recruit maximum alveoli, and prevent barotrauma.[38] Prone positioning of the patient with contusion reduces stress on the diaphragm, and positioning the contused lung in a nondependent position helps recruit alveoli.
Noninvasive ventilation can cause significant gastric distention and aspiration if consciousness is impaired. Invasive ventilation is required if positive pressure ventilation fails. Low tidal volumes are suggested, as large tidal volumes can have adverse effects. Patients with severe hypoxia and poor response to other therapies can benefit from nitric oxide. Diuretics reduce pulmonary venous resistance and capillary hydrostatic pressure, thus improving contusions. Measuring pulmonary artery pressure is recommended to maintain euvolemia while avoiding pulmonary edema when administering fluid therapy. Surgical stabilization of multiple rib fractures or flail chest corrects pulmonary mechanics. The extracorporeal gas exchange has been successfully used for pulmonary contusions refractory to all conventional therapies.[39] Surgical repair is required for aortic injuries with pseudoaneurysm formation.
Cardiac Injuries
Cardiac injury in the context of chest trauma presents significant diagnostic and management challenges, particularly in cases of blunt thoracic trauma. These injuries can range from minor myocardial contusions to life-threatening conditions such as cardiac rupture, valvular damage, or pericardial tamponade. Blunt cardiac injury often results from high-energy mechanisms such as motor vehicle collisions, falls from height, or direct impact to the chest. The injury is commonly caused by compression of the heart between the sternum and the thoracic spine, rapid deceleration forces, or increased venous return leading to chamber overdistension and rupture. While penetrating trauma, including stab wounds and gunshot injuries, is more likely to cause immediate cardiac tamponade or exsanguination, blunt trauma presents a broader spectrum of clinical severity.
The initial evaluation of cardiac injury relies heavily on clinical suspicion, particularly in patients presenting with chest pain, hypotension, arrhythmias, or signs of cardiac tamponade such as distended neck veins, muffled heart sounds, and pulsus paradoxus. ECG is a first-line diagnostic tool, with findings ranging from nonspecific ST-segment abnormalities to conduction disturbances and new-onset tachyarrhythmias. While an abnormal ECG raises suspicion of myocardial injury, a normal ECG does not completely exclude significant cardiac trauma.
Cardiac biomarkers, particularly troponin levels, may aid in diagnosing myocardial injury. However, the correlation between elevated cardiac enzymes and clinically significant outcomes remains controversial yet promising.[40] In patients with abnormal ECG findings or hemodynamic instability, transthoracic (TTE) or transesophageal echocardiography (TEE) is recommended to assess myocardial function, detect pericardial effusion, and identify structural damage such as septal defects or valvular injuries.
The management of blunt cardiac injury is largely supportive, with close hemodynamic monitoring and intervention guided by clinical severity. Cases of mild contusions and normal hemodynamics can be managed conservatively, whereas those with significant arrhythmias, hemodynamic compromise, or structural injuries may require advanced cardiac monitoring and intensive care admission. In the case of severe blunt cardiac injury, early diagnosis, with limited fluid resuscitation and rapid surgical intervention, proved effective in reducing mortality rates.[41] In cases of cardiac rupture or tamponade, emergency surgical intervention is necessary. Pericardiocentesis may provide temporary relief in tamponade, but definitive management typically requires surgical exploration and repair.[42](B3)
The prognosis of cardiac trauma varies depending on the severity and rapidity of intervention. While minor contusions often resolve without sequelae, major injuries involving chamber rupture, valvular disruption, or severe conduction disturbances carry a high risk of morbidity and mortality. The early identification of high-risk patients using a combination of clinical assessment, ECG, echocardiography, and biomarker evaluation is crucial in guiding appropriate management and improving outcomes in patients with cardiac trauma.
Aortic Injuries
Aortic injuries are managed based on severity. Conservative management is usually attempted for Grade I injuries. Grade II injuries are monitored closely for a few days using appropriate imaging modalities, such as CT aortography, magnetic resonance orthography, or transoesophageal ultrasound. Surgery is performed if the condition progresses. Grade III to IV injuries require emergent intervention, although most patients with Grade IV aortic injury do not survive before hospital arrival.[43]
Esophageal Injuries
Esophageal injuries should be managed early and aggressively. A torn esophagus can allow gastrointestinal contents to contaminate the mediastinum, leading to complications such as mediastinal abscess and sepsis.[44] Additionally, delayed management of esophageal injuries can lead to difficulties with swallowing and oral intake.(B3)
Tracheobronchial Injuries
Tracheobronchial injuries are rare but potentially life-threatening complications of chest trauma, most commonly resulting from high-energy blunt force mechanisms such as motor vehicle collisions, falls, or crush injuries. These injuries typically occur near the carina, mostly affecting the proximal mainstem bronchi within 2 cm of the bifurcation. The mechanism of injury often involves severe compression of the thoracic cage, rapid deceleration forces, or a sudden increase in intrathoracic pressure leading to disruption of the tracheobronchial structures.
Clinically, tracheobronchial injuries can present with significant respiratory distress, persistent air leaks, hemoptysis, subcutaneous emphysema, or tension pneumothorax that does not resolve with standard chest tube placement. Patients may exhibit hoarseness, dysphonia, or signs of airway obstruction, particularly when the injury is in the cervical portion of the trachea. Physical examination often reveals crepitus due to subcutaneous air, which may extend from the neck to the upper thorax, raising suspicion of underlying airway disruption.
Radiographic evaluation is essential in identifying tracheobronchial injuries. Chest radiographs may demonstrate pneumomediastinum, persistent pneumothorax despite chest tube placement, or a collapsed lung that remains retracted toward the hilum. However, definitive diagnosis requires bronchoscopy, which provides direct visualization of airway integrity and allows for precise localization of the injury. In some cases, computed tomography with 3-dimensional reconstruction can aid in assessment, particularly in hemodynamically stable patients.
The management of tracheobronchial injuries depends on the severity and location of the disruption. In stable individuals with partial airway tears, conservative management with close observation, supplemental oxygen, and endotracheal intubation may be sufficient, particularly when spontaneous healing is expected. However, significant disruptions, complete airway transections, or cases associated with massive air leaks and respiratory compromise require prompt surgical intervention. The surgical approach varies based on the injury site; cervical tracheal injuries can often be repaired through a low cervical incision, while intrathoracic injuries may necessitate a right thoracotomy for optimal exposure. Surgical repair typically involves meticulous debridement of devitalized tissue followed by primary anastomosis, ensuring tension-free closure and preservation of blood supply.
Postoperative care is crucial to prevent complications such as anastomotic dehiscence, tracheal stenosis, or secondary infections. Patients should undergo close respiratory monitoring, early mobilization, and aggressive pulmonary hygiene to reduce the risk of atelectasis and pneumonia. In cases where airway edema or anastomotic stress is a concern, temporary tracheostomy or chin-to-chest sutures may be employed to minimize movement and enhance healing. Long-term follow-up with bronchoscopy is often recommended to assess for late complications such as granulation tissue formation or stricture development.[29][45][46]
Traumatic Asphyxia
Traumatic asphyxia, also known as Perthes syndrome, is an uncommon but serious consequence of severe compressive thoracic trauma. This occurs when sudden, intense pressure is applied to the chest, typically in situations such as crush injuries, entrapment under heavy objects, or industrial accidents. The mechanism of injury involves a forceful increase in intrathoracic pressure against a closed glottis, leading to a retrograde surge of venous blood into the upper body, head, and neck. This results in characteristic clinical manifestations due to venous engorgement and capillary rupture.
Patients with traumatic asphyxia typically present with striking physical findings. One of the hallmark features is cervicofacial cyanosis, often accompanied by petechial hemorrhages affecting the conjunctiva, face, neck, and upper chest. The intense venous pressure may also cause subconjunctival hemorrhage, which can mimic ocular trauma. Additional signs include facial edema, distended neck veins, and mucosal hemorrhages in the oral or nasal cavities. Some patients may report transient vision disturbances or dizziness due to compromised cerebral perfusion.
Although the external appearance of traumatic asphyxia may be alarming, the underlying pathophysiology is largely self-limiting once the compressive force is relieved. The key priority in management is ensuring airway patency and adequate ventilation, particularly in cases where concurrent thoracic injuries, such as rib fractures or pulmonary contusions, are present. Oxygen supplementation and hemodynamic stabilization are essential supportive measures. In cases where traumatic asphyxia is associated with significant chest trauma, imaging studies such as chest radiography or CT scans are warranted to assess for potential pulmonary or cardiac injuries.
Neurologic complications, though uncommon, can occur if cerebral venous congestion is prolonged. Some patients may experience transient confusion, headaches, or even seizures due to increased intracranial pressure. Severe cases, particularly those involving prolonged compression, may lead to diffuse cerebral hypoxia, requiring close neurological monitoring.
While the prognosis for traumatic asphyxia is generally favorable with prompt decompression and supportive care, long-term sequelae are possible in cases where there has been significant ischemic insult to the brain or ocular structures. Follow-up ophthalmologic and neurologic evaluations may be necessary to assess for any persistent deficits. Preventative measures, such as improved workplace safety protocols and protective restraints in high-risk environments, are crucial in reducing the incidence of this rare but potentially serious condition.[47][48]
Differential Diagnosis
The following differential diagnosis should be considered in patients presenting with chest trauma:
- Acute coronary syndrome
- Chest pain or pressure often radiates to the left arm or jaw and is associated with dyspnea, diaphoresis, and nausea. Susceptible individuals may develop this condition in acute traumatic settings, as it may be precipitated by significant bleeding or emotional stress.[49]
- Pneumonia
- Chest pain is exacerbated by coughing or deep breathing and is associated with fever, productive cough, and signs of respiratory distress.
- Pulmonary embolism
- This condition presents with sudden-onset pleuritic chest pain worsened by deep breathing and accompanied by dyspnea, tachypnea, and signs of hemodynamic instability. Risk factors include prolonged immobility and coagulopathies.
- Aortic dissection
- This condition presents with severe, sudden-onset chest pain radiating to the back. Dyspnea, hypotension, and signs of aortic regurgitation or peripheral ischemia may be present.
- Tension gastrothorax
- Chest pain and difficulty breathing arise from gastric herniation into the thoracic cavity, leading to lung tissue compression and mediastinal shift.
- Pericarditis
- Deep breathing or lying flat exacerbates chest pain, which is associated with dyspnea, fever, and a pericardial friction rub.
- Anxiety or panic attack
- Chest pain, palpitations, and hyperventilation may develop after chest trauma.
- Musculoskeletal pain
- Chest pain is exacerbated by movement or palpation and is not associated with dyspnea or other respiratory symptoms.
A thorough clinical assessment and diagnostic testing can help distinguish chest trauma from these conditions.
Prognosis
The outcomes of chest trauma vary depending on the extent of injury. This type of trauma is the second most common form of unintentional traumatic injury and ranks third in terms of mortality among patients with polytrauma.[50][51] Study results indicate that up to 60% of chest trauma cases are fatal, emphasizing the urgency for prompt evaluation and intervention and elucidating the injury mechanisms, whether penetrating or blunt, is crucial for effective management.[27]
The prognosis for isolated rib fractures is good. However, lung or cardiac injury often leads to prolonged recovery. Thoracic aortic injuries are life-threatening and generally associated with poor outcomes. These injuries are independent predictors of mortality. Most patients may die before reaching an emergency department, and many patients who reach the hospital die within 24 hours. The highest morbidity following chest trauma is seen in younger and older patients.[52] Chest trauma is one of the leading causes of pediatric mortality.
Complications
Complications of chest trauma include pneumonia, acute respiratory distress syndrome, acute lung injury, mediastinitis, arteriovenous fistula, and bronchopleural fistula. These conditions may be due to direct damage or secondary to critical injuries.
Consultations
Consider a lower threshold for trauma activation, especially in cases of penetrating chest injuries. Stable individuals with chest trauma should be examined by the surgeon on duty. Thoracic surgeons should be involved early to consider surgical management of specific injuries. Immediate thoracic surgical intervention is required in the following situations:
- Initial blood loss of at least 1500 mL or greater than 200 mL/hour over 2 to 4 hours
- Massive contusion with significant ventilatory impairment
- Tracheobronchial tree injury
- Vascular injury, including the heart or large vessels
The collaborative involvement of the interprofessional team, comprising healthcare professionals such as surgeons, emergency physicians, and critical care specialists, facilitates comprehensive evaluation and timely intervention. This approach ensures effective care coordination and optimized treatment strategies for patients with chest trauma.
Deterrence and Patient Education
Chest trauma prevention involves a multifaceted approach addressing primary and secondary prevention strategies. Primary prevention focuses on mitigating risk factors and promoting safety measures to prevent traumatic events, such as implementing strict seatbelt and helmet use laws, promoting safe driving practices, enforcing speed limits, and reducing exposure to violence and physical altercations.
Additionally, workplace safety protocols, including proper personal protective equipment use in high-risk occupations, can help prevent occupation-related chest trauma. Secondary prevention strategies aim to minimize the severity of injuries when traumatic events occur. Preventive measures include prompt access to emergency medical services, effective prehospital care, and public education on first aid techniques. Chest trauma severity and incidence can be significantly reduced by prioritizing injury prevention measures at individual, community, and societal levels.
Pearls and Other Issues
The key points when evaluating and managing chest trauma are as follows:
- Patients should be stabilized first before performing definitive surgical intervention. Airway, breathing, and circulation must be examined and addressed according to Advanced Trauma Life Support guidelines.
- Injuries likely to arise from a chest trauma mechanism must be identified or anticipated. Blunt and penetrating chest injuries present with different symptom patterns.
- Thoracic trauma rarely occurs in isolation. Other body areas must be investigated for associated injuries. Life-threatening injuries must be rapidly recognized and addressed.
- The presence of a flail chest signifies severe thoracic injury. Significant chest trauma can occur without rib fractures.
- High-velocity chest injuries are associated with lung contusion, pneumothorax, hemothorax, and intrathoracic blood vessel damage.
- Rib fractures may suggest that significant force has been applied. The underlying structures must be evaluated. Lower rib fractures may be associated with intraabdominal injuries.
- Pneumothorax can occur in both blunt and penetrating thoracic trauma. A simple pneumothorax can progress to a tension pneumothorax.
- Pulmonary contusion often occurs in patients with chest wall injury. During the initial evaluation, the contusion may be silent. Hypoxia is the most important clinical sign of pulmonary contusion.
- Plain chest radiography may reveal vascular injury, including hemothorax, wide mediastinum, and loss of aortic knob contour.
- The trauma team must be activated promptly in the presence of hemodynamic instability. Stable individuals with thoracic injuries warrant a surgical consultation.
- Aortic injuries are managed based on severity.
- Esophageal and cardiac injuries must be treated promptly and aggressively.
Improving safety on the road, at work, and at home prevents traumatic injuries. However, trauma prevention efforts must come from different sectors of society to be truly effective.
Enhancing Healthcare Team Outcomes
Chest trauma is best managed by an interprofessional team comprising emergency clinicians, trauma surgeons, anesthesiologists, thoracic surgeons, intensive care clinicians, cardiac surgeons, nurses, respiratory therapists, and pharmacists. The emergency clinician initially assesses and stabilizes patients with chest trauma and coordinates the subsequent care pathway. Trauma surgeons offer their expertise in surgical interventions for severe thoracic injuries and oversee the overall management of trauma patients. Anesthesiologists ensure optimal pain management and airway control, particularly during surgical procedures or in critically ill patients requiring mechanical ventilation.
Thoracic surgeons bring specialized skills in the surgical management of complex chest injuries, including chest wall reconstruction, lung resection, and repair of thoracic vascular injuries. Intensive care clinicians provide comprehensive critical care management for severely injured patients, including hemodynamic stabilization, ventilatory support, and monitoring for potential complications. Cardiac surgeons may be involved in cases of cardiac trauma, providing surgical management of cardiac injuries or complications arising from thoracic trauma.
Nurses are essential in chest trauma management, providing initial assessments, interventions, and ongoing monitoring to stabilize patients. Respiratory therapists provide respiratory support interventions such as oxygen therapy, airway management, and mechanical ventilation to ensure adequate oxygenation and ventilation in patients with chest injuries. Pharmacists collaborate with healthcare teams to optimize medication regimens and provide valuable patient education on medication use and potential side effects.[53] Through coordinated efforts and expertise from each team member, the interprofessional team ensures comprehensive and effective management of chest trauma, leading to improved patient outcomes.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
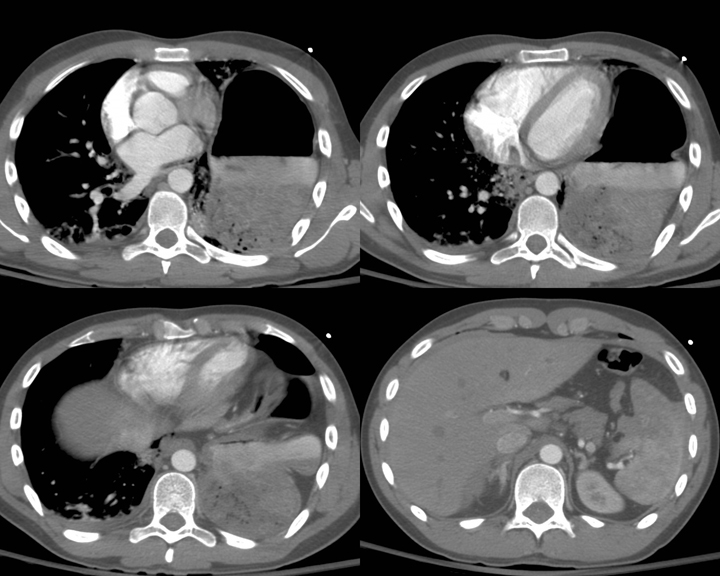
Blunt Chest Trauma on Computed Tomography. Blunt chest trauma caused organ rupture within the thoracic cavity. CT imaging shows bowel herniation into the left hemithorax with mediastinal shift to the right. A small amount of hyperattenuating fluid is seen adjacent to the liver and spleen, consistent with hemoperitoneum. Findings are compatible with a traumatic diaphragmatic rupture.
Contributed by H Shulman, MD
References
Chrysou K, Halat G, Hoksch B, Schmid RA, Kocher GJ. Lessons from a large trauma center: impact of blunt chest trauma in polytrauma patients-still a relevant problem? Scandinavian journal of trauma, resuscitation and emergency medicine. 2017 Apr 20:25(1):42. doi: 10.1186/s13049-017-0384-y. Epub 2017 Apr 20 [PubMed PMID: 28427480]
Clark GC, Schecter WP, Trunkey DD. Variables affecting outcome in blunt chest trauma: flail chest vs. pulmonary contusion. The Journal of trauma. 1988 Mar:28(3):298-304 [PubMed PMID: 3351988]
Khandhar SJ, Johnson SB, Calhoon JH. Overview of thoracic trauma in the United States. Thoracic surgery clinics. 2007 Feb:17(1):1-9 [PubMed PMID: 17650692]
Level 3 (low-level) evidenceZiegler DW, Agarwal NN. The morbidity and mortality of rib fractures. The Journal of trauma. 1994 Dec:37(6):975-9 [PubMed PMID: 7996614]
Veysi VT, Nikolaou VS, Paliobeis C, Efstathopoulos N, Giannoudis PV. Prevalence of chest trauma, associated injuries and mortality: a level I trauma centre experience. International orthopaedics. 2009 Oct:33(5):1425-33. doi: 10.1007/s00264-009-0746-9. Epub 2009 Mar 6 [PubMed PMID: 19266199]
Sweet AAR, de Bruin IGJ, Peek J, IJpma FFA, van Baal MCPM, Leenen LPH, Houwert RM. Epidemiology and outcomes of traumatic chest injuries in children: a nationwide study in the Netherlands. European journal of pediatrics. 2023 Apr:182(4):1887-1896. doi: 10.1007/s00431-023-04828-1. Epub 2023 Feb 18 [PubMed PMID: 36807757]
Helsloot D, Fitzgerald MC, Lefering R, Verelst S, Missant C, TraumaRegister DGU®. The first hour of trauma reception is critical for patients with major thoracic trauma: A retrospective analysis from the TraumaRegister DGU. European journal of anaesthesiology. 2023 Nov 1:40(11):865-873. doi: 10.1097/EJA.0000000000001834. Epub 2023 May 3 [PubMed PMID: 37139941]
Level 2 (mid-level) evidencePolmear MM, Kakalecik J, Croft C, Hagen JE. Early Care of Polytraumatized Patients: A Framework for Orthopaedic Surgeons. The Journal of the American Academy of Orthopaedic Surgeons. 2024 Dec 31:():. doi: 10.5435/JAAOS-D-24-00990. Epub 2024 Dec 31 [PubMed PMID: 39739953]
Ekpe EE, Eyo C. Determinants of mortality in chest trauma patients. Nigerian journal of surgery : official publication of the Nigerian Surgical Research Society. 2014 Jan:20(1):30-4. doi: 10.4103/1117-6806.127107. Epub [PubMed PMID: 24665200]
Demetriades D, Kimbrell B, Salim A, Velmahos G, Rhee P, Preston C, Gruzinski G, Chan L. Trauma deaths in a mature urban trauma system: is "trimodal" distribution a valid concept? Journal of the American College of Surgeons. 2005 Sep:201(3):343-8 [PubMed PMID: 16125066]
Inocencio M, Childs J, Chilstrom ML, Berona K. Ultrasound Findings in Tension Pneumothorax: A Case Report. The Journal of emergency medicine. 2017 Jun:52(6):e217-e220. doi: 10.1016/j.jemermed.2017.02.008. Epub 2017 Mar 23 [PubMed PMID: 28342574]
Level 3 (low-level) evidenceEbrahimi A, Yousefifard M, Mohammad Kazemi H, Rasouli HR, Asady H, Moghadas Jafari A, Hosseini M. Diagnostic Accuracy of Chest Ultrasonography versus Chest Radiography for Identification of Pneumothorax: A Systematic Review and Meta-Analysis. Tanaffos. 2014:13(4):29-40 [PubMed PMID: 25852759]
Level 1 (high-level) evidenceNagarsheth K, Kurek S. Ultrasound detection of pneumothorax compared with chest X-ray and computed tomography scan. The American surgeon. 2011 Apr:77(4):480-4 [PubMed PMID: 21679560]
Alrajab S, Youssef AM, Akkus NI, Caldito G. Pleural ultrasonography versus chest radiography for the diagnosis of pneumothorax: review of the literature and meta-analysis. Critical care (London, England). 2013 Sep 23:17(5):R208. doi: 10.1186/cc13016. Epub 2013 Sep 23 [PubMed PMID: 24060427]
Level 1 (high-level) evidenceRodriguez RM, Hendey GW, Mower W, Kea B, Fortman J, Merchant G, Hoffman JR. Derivation of a decision instrument for selective chest radiography in blunt trauma. The Journal of trauma. 2011 Sep:71(3):549-53. doi: 10.1097/TA.0b013e3181f2ac9d. Epub [PubMed PMID: 21045745]
Rodriguez RM, Anglin D, Langdorf MI, Baumann BM, Hendey GW, Bradley RN, Medak AJ, Raja AS, Juhn P, Fortman J, Mulkerin W, Mower WR. NEXUS chest: validation of a decision instrument for selective chest imaging in blunt trauma. JAMA surgery. 2013 Oct:148(10):940-6. doi: 10.1001/jamasurg.2013.2757. Epub [PubMed PMID: 23925583]
Level 1 (high-level) evidenceRodriguez RM, Hendey GW, Mower WR. Selective chest imaging for blunt trauma patients: The national emergency X-ray utilization studies (NEXUS-chest algorithm). The American journal of emergency medicine. 2017 Jan:35(1):164-170. doi: 10.1016/j.ajem.2016.10.066. Epub 2016 Oct 29 [PubMed PMID: 27838036]
Dillon DG, Rodriguez RM. Screening performance of the chest X-ray in adult blunt trauma evaluation: Is it effective and what does it miss? The American journal of emergency medicine. 2021 Nov:49():310-314. doi: 10.1016/j.ajem.2021.06.034. Epub 2021 Jun 19 [PubMed PMID: 34182276]
Blaivas M, Lyon M, Duggal S. A prospective comparison of supine chest radiography and bedside ultrasound for the diagnosis of traumatic pneumothorax. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2005 Sep:12(9):844-9 [PubMed PMID: 16141018]
Husain LF, Hagopian L, Wayman D, Baker WE, Carmody KA. Sonographic diagnosis of pneumothorax. Journal of emergencies, trauma, and shock. 2012 Jan:5(1):76-81. doi: 10.4103/0974-2700.93116. Epub [PubMed PMID: 22416161]
Lichtenstein DA, Menu Y. A bedside ultrasound sign ruling out pneumothorax in the critically ill. Lung sliding. Chest. 1995 Nov:108(5):1345-8 [PubMed PMID: 7587439]
Ding W, Shen Y, Yang J, He X, Zhang M. Diagnosis of pneumothorax by radiography and ultrasonography: a meta-analysis. Chest. 2011 Oct:140(4):859-866. doi: 10.1378/chest.10-2946. Epub 2011 May 5 [PubMed PMID: 21546439]
Level 1 (high-level) evidenceHyacinthe AC, Broux C, Francony G, Genty C, Bouzat P, Jacquot C, Albaladejo P, Ferretti GR, Bosson JL, Payen JF. Diagnostic accuracy of ultrasonography in the acute assessment of common thoracic lesions after trauma. Chest. 2012 May:141(5):1177-1183. doi: 10.1378/chest.11-0208. Epub 2011 Oct 20 [PubMed PMID: 22016490]
Level 2 (mid-level) evidenceMumtaz U, Zahur Z, Raza MA, Mumtaz M. Ultrasound And Supine Chest Radiograph In Road Traffic Accident Patients: A Reliable And Convenient Way To Diagnose Pleural Effusion. Journal of Ayub Medical College, Abbottabad : JAMC. 2017 Oct-Dec:29(4):587-590 [PubMed PMID: 29330983]
Schwerin DL, Svancarek B. EMS Diabetic Protocols For Treat and Release. StatPearls. 2025 Jan:(): [PubMed PMID: 32809447]
Muse ED, Topol EJ. More than meets the eye: Using AI to identify reduced heart function by electrocardiograms. Med (New York, N.Y.). 2021 Jul 9:2(7):791-793. doi: 10.1016/j.medj.2021.06.003. Epub [PubMed PMID: 35590216]
Mowery NT, Gunter OL, Collier BR, Diaz JJ Jr, Haut E, Hildreth A, Holevar M, Mayberry J, Streib E. Practice management guidelines for management of hemothorax and occult pneumothorax. The Journal of trauma. 2011 Feb:70(2):510-8. doi: 10.1097/TA.0b013e31820b5c31. Epub [PubMed PMID: 21307755]
Casós SR, Richardson JD. Role of thoracoscopy in acute management of chest injury. Current opinion in critical care. 2006 Dec:12(6):584-9 [PubMed PMID: 17077691]
Level 3 (low-level) evidenceBoutros J, Marquette CH, Ichai C, Leroy S, Benzaquen J. Multidisciplinary management of tracheobronchial injury. European respiratory review : an official journal of the European Respiratory Society. 2022 Mar 31:31(163):. doi: 10.1183/16000617.0126-2021. Epub 2022 Jan 25 [PubMed PMID: 35082126]
Chou YP, Lin HL, Wu TC. Video-assisted thoracoscopic surgery for retained hemothorax in blunt chest trauma. Current opinion in pulmonary medicine. 2015 Jul:21(4):393-8. doi: 10.1097/MCP.0000000000000173. Epub [PubMed PMID: 25978625]
Level 3 (low-level) evidenceKirkpatrick AW, Rizoli S, Ouellet JF, Roberts DJ, Sirois M, Ball CG, Xiao ZJ, Tiruta C, Meade M, Trottier V, Zhu G, Chagnon F, Tien H, Canadian Trauma Trials Collaborative and the Research Committee of the Trauma Association of Canada. Occult pneumothoraces in critical care: a prospective multicenter randomized controlled trial of pleural drainage for mechanically ventilated trauma patients with occult pneumothoraces. The journal of trauma and acute care surgery. 2013 Mar:74(3):747-54; discussion 754-5. doi: 10.1097/TA.0b013e3182827158. Epub [PubMed PMID: 23425731]
Level 1 (high-level) evidenceLodhia JV, Eyre L, Smith M, Toth L, Troxler M, Milton RS. Management of thoracic trauma. Anaesthesia. 2023 Feb:78(2):225-235. doi: 10.1111/anae.15934. Epub 2022 Dec 26 [PubMed PMID: 36572548]
Galvagno SM Jr, Smith CE, Varon AJ, Hasenboehler EA, Sultan S, Shaefer G, To KB, Fox AD, Alley DE, Ditillo M, Joseph BA, Robinson BR, Haut ER. Pain management for blunt thoracic trauma: A joint practice management guideline from the Eastern Association for the Surgery of Trauma and Trauma Anesthesiology Society. The journal of trauma and acute care surgery. 2016 Nov:81(5):936-951 [PubMed PMID: 27533913]
Heydari MB, Hessami MA, Setayeshi K, Sajadifar F. Use of prophylactic antibiotics following tube thoracostomy for blunt chest trauma in the prevention of empyema and pneumonia. Journal of injury & violence research. 2014 Jul:6(2):91-2. doi: 10.5249/jivr.v6i2.11. Epub 2013 Sep 17 [PubMed PMID: 24045157]
Level 3 (low-level) evidenceKasotakis G, Hasenboehler EA, Streib EW, Patel N, Patel MB, Alarcon L, Bosarge PL, Love J, Haut ER, Como JJ. Operative fixation of rib fractures after blunt trauma: A practice management guideline from the Eastern Association for the Surgery of Trauma. The journal of trauma and acute care surgery. 2017 Mar:82(3):618-626. doi: 10.1097/TA.0000000000001350. Epub [PubMed PMID: 28030502]
Rendeki S, Molnár TF. Pulmonary contusion. Journal of thoracic disease. 2019 Feb:11(Suppl 2):S141-S151. doi: 10.21037/jtd.2018.11.53. Epub [PubMed PMID: 30906578]
Ganie FA, Lone H, Lone GN, Wani ML, Singh S, Dar AM, Wani NU, Wani SN, Nazeer NU. Lung Contusion: A Clinico-Pathological Entity with Unpredictable Clinical Course. Bulletin of emergency and trauma. 2013 Jan:1(1):7-16 [PubMed PMID: 27162815]
Požgain Z, Kristek D, Lovrić I, Kondža G, Jelavić M, Kocur J, Danilović M. Pulmonary contusions after blunt chest trauma: clinical significance and evaluation of patient management. European journal of trauma and emergency surgery : official publication of the European Trauma Society. 2018 Oct:44(5):773-777. doi: 10.1007/s00068-017-0876-5. Epub 2017 Nov 22 [PubMed PMID: 29167928]
Paolone S. Extracorporeal Membrane Oxygenation (ECMO) for Lung Injury in Severe Acute Respiratory Distress Syndrome (ARDS): Review of the Literature. Clinical nursing research. 2017 Dec:26(6):747-762. doi: 10.1177/1054773816677808. Epub 2016 Nov 11 [PubMed PMID: 27836935]
Haller PM, Beer BN, Tonkin AM, Blankenberg S, Neumann JT. Role of Cardiac Biomarkers in Epidemiology and Risk Outcomes. Clinical chemistry. 2021 Jan 8:67(1):96-106. doi: 10.1093/clinchem/hvaa228. Epub [PubMed PMID: 33225348]
Gao JM, Du DY, Kong LW, Yang J, Li H, Wei GB, Li CH, Liu CP. Emergency Surgery for Blunt Cardiac Injury: Experience in 43 Cases. World journal of surgery. 2020 May:44(5):1666-1672. doi: 10.1007/s00268-020-05369-6. Epub [PubMed PMID: 31915978]
Level 3 (low-level) evidenceGupta B, Singh Y, Bagaria D, Nagarajappa A. Comprehensive Management of the Patient With Traumatic Cardiac Injury. Anesthesia and analgesia. 2023 May 1:136(5):877-893. doi: 10.1213/ANE.0000000000006380. Epub 2023 Apr 14 [PubMed PMID: 37058724]
Mouawad NJ, Paulisin J, Hofmeister S, Thomas MB. Blunt thoracic aortic injury - concepts and management. Journal of cardiothoracic surgery. 2020 Apr 19:15(1):62. doi: 10.1186/s13019-020-01101-6. Epub 2020 Apr 19 [PubMed PMID: 32307000]
Abila AW, Nditika ME, Kipkemoi RD, Ondigo S, Khwa-Otsyula BO. Primary repair of esophageal perforation: Case report. International journal of surgery case reports. 2020:71():159-162. doi: 10.1016/j.ijscr.2020.04.026. Epub 2020 May 11 [PubMed PMID: 32454452]
Level 3 (low-level) evidenceRieth A, Varga E, Kovács T, Ottlakán A, Németh T, Furák J. Contemporary management strategies of blunt tracheobronchial injuries. Injury. 2021 Mar:52 Suppl 1():S7-S14. doi: 10.1016/j.injury.2020.07.026. Epub 2020 Jul 10 [PubMed PMID: 32674886]
Grewal HS, Dangayach NS, Ahmad U, Ghosh S, Gildea T, Mehta AC. Treatment of Tracheobronchial Injuries: A Contemporary Review. Chest. 2019 Mar:155(3):595-604. doi: 10.1016/j.chest.2018.07.018. Epub 2018 Jul 27 [PubMed PMID: 30059680]
Byard RW, Wick R, Simpson E, Gilbert JD. The pathological features and circumstances of death of lethal crush/traumatic asphyxia in adults--a 25-year study. Forensic science international. 2006 Jun 2:159(2-3):200-5 [PubMed PMID: 16183229]
Colville-Ebeling B, Freeman M, Banner J, Lynnerup N. Autopsy practice in forensic pathology - evidence-based or experience-based? a review of autopsies performed on victims of traumatic asphyxia in a mass disaster. Journal of forensic and legal medicine. 2014 Feb:22():33-6. doi: 10.1016/j.jflm.2013.11.006. Epub 2013 Nov 28 [PubMed PMID: 24485418]
Culhane JT, Mangold MA, Freeman C. Analysis of Predictors of Myocardial Infarction in Trauma With Development of a Trauma Cardiac Risk Index. Cureus. 2021 Feb 5:13(2):e13153. doi: 10.7759/cureus.13153. Epub 2021 Feb 5 [PubMed PMID: 33692923]
Deng H, Tang TX, Yao Y, Zhang C, Wu H, Li ZW, Tang LS, Chen D, Chang TD, Yang JZ, Luo JL, Dong L, Yang XP, Tang ZH. The incidence, clinical characteristics, and outcome of polytrauma patients with the combination of pulmonary contusion, flail chest and upper thoracic spinal injury. Injury. 2022 Mar:53(3):1073-1080. doi: 10.1016/j.injury.2021.09.053. Epub 2021 Oct 1 [PubMed PMID: 34625240]
Beshay M, Mertzlufft F, Kottkamp HW, Reymond M, Schmid RA, Branscheid D, Vordemvenne T. Analysis of risk factors in thoracic trauma patients with a comparison of a modern trauma centre: a mono-centre study. World journal of emergency surgery : WJES. 2020 Jul 31:15(1):45. doi: 10.1186/s13017-020-00324-1. Epub 2020 Jul 31 [PubMed PMID: 32736642]
Vollrath JT, Schindler CR, Marzi I, Lefering R, Störmann P, TraumaRegister DGU. Lung failure after polytrauma with concomitant thoracic trauma in the elderly: an analysis from the TraumaRegister DGU®. World journal of emergency surgery : WJES. 2022 Feb 23:17(1):12. doi: 10.1186/s13017-022-00416-0. Epub 2022 Feb 23 [PubMed PMID: 35197078]
Kleinpell R, Grabenkort WR, Boyle WA 3rd, Vines DL, Olsen KM. The Society of Critical Care Medicine at 50 Years: Interprofessional Practice in Critical Care: Looking Back and Forging Ahead. Critical care medicine. 2021 Dec 1:49(12):2017-2032. doi: 10.1097/CCM.0000000000005276. Epub [PubMed PMID: 34387239]