 Mohs Micrographic Surgery Design and Execution of Intermediate and Complex Closure
Mohs Micrographic Surgery Design and Execution of Intermediate and Complex Closure
Introduction
Mohs micrographic surgery (MMS) is a surgical technique designed for the precise removal of cutaneous cancers. MMS is characterized by en-face tissue processing, allowing complete peripheral and deep-margin assessment intraoperatively. This results in the highest possible cure rates for skin malignancies, including non-melanoma skin cancers and thin melanomas with immunohistochemical stains.[1] In addition, MMS is a tissue-sparing technique that confirms negative histologic margins before defect reconstruction.
MMS was originally developed by Dr. Frederick E. Mohs and coined as chemosurgery.[2] Formerly, tumors were fixed with zinc chloride in situ. After 1 day of fixation, the tumor was excised and histologically read for tumor clearance. If tumor burden was retained after initial excision, the process was repeated daily until pathologic clearance was attained.[3][4] This process was time-consuming, involved serial visits over multiple days, and created a necrotic eschar at the excision site that did not allow for reconstruction. Modern MMS, popularized in the 1970s, utilizes fresh frozen section histology. This allows the entire procedure to be completed on the same day and avoids tissue damage to the defect site. As a result, Mohs defects can be repaired with various techniques ranging from linear closures to skin grafts and flaps on the same day as the Mohs procedure.[5]
Mohs surgeons perform the majority of reconstructions at cosmetically and functionally sensitive sites.[6][7] For a Mohs defect, the reconstructive ladder includes secondary intention healing, intermediate and complex linear repairs, split- or full-thickness skin grafts, local flaps, and interpolated flaps. Linear repair types include intermediate and complex closures. Both repair types are denoted with specific Current Procedural Terminology (CPT) criteria, and their definitions were revised in 2020. This recent CPT revision has resulted in a shift toward more intermediate closures and less complex closures being performed.[8]
Indications
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Indications
There are published Appropriate Use Criteria (AUC) guidelines to help determine which skin cancers are best served by MMS. Appropriateness varies based on tumor type, histology, size, location, and patient factors such as immunosuppression and genetic tumor syndromes. The Mohs AUC guidelines are described thoroughly in the MMS article in StatPearls.[9][5]
Indications for Intermediate Repair
Intermediate repairs are linear repair variants coded by length and anatomic location.[10]
According to the American College of Mohs Surgery (ACMS), intermediate repairs are linear repairs that utilize layered closure of at least 1 deeper layer of subcutaneous tissue, dermal and epidermal closure. More specifically, intermediate repairs include undermining with a distance that does not exceed the maximum width of the defect. Defect width is a measurement perpendicular to the closure line (See Image. Intermediate versus Complex Closure).
Indications for Complex Repair
Complex repairs include all the classifications of intermediate repair with at least 1 of the following additional criteria.[10]
- Exposure of bone, cartilage, tendon, or a named neurovascular structure.
- Significant debridement of wound edges. This is typically reserved for traumatic lacerations.
- Undermining was performed equal to or greater than the maximum defect width perpendicular to the direction of closure attempted. This distance must be maintained along 1 entire edge of the defect (See Image. Intermediate versus Complex Closure).
- Free margins are involved, eg, helical rim, vermillion border, or alar rim.
- Retention sutures have been placed. Retention sutures are sutures of lower gauge material to remove tension from the traditional closure material. This is often performed with pulley stitches and can be assisted with commercially available products to protect tissue edges.[11][12]
Equipment
MMS requires procedure rooms, equipment, and materials for frozen section histologic analysis. These are discussed in detail within the MMS section of StatPearls.[5]
Common equipment includes the following:
- Scalpel Handles
- Most commonly used handles include the Bard-Parker and Beaver models.
- The Bard-Parker sports a flattened and sleek design that is slim.
- The Beaver blade handle has an ergonomic round design, which can help with finer rotational control.
- Blades
- The Number (No.) 15 and No. 10 are commonly used blades.
- The No. 10 has a larger arched blade, with the sharpest point being the belly of the blade.[10] The No. 15 blade has a smaller design where the cutting edge is displaced more toward the instrument's tip.[13] The No. 15 blade allows for finer control in sensitive anatomic regions
- Forceps (Adson, Jewler, DeBakey, and Curtis)
- Adson forceps have 1 set of interlocking teeth for delicate tissue manipulation.
- Jewler forceps are pointed at the edge without interlocking to better manipulate finer tissue, such as eyelid skin.[13]
- DeBakey forceps have serrations at the tip to enhance suture and tissue grasping, but there is an increased risk of traumatizing wound edges.
- Curtis forceps have both serrations and interlocking teeth, allowing for the advantages of delicate wound edge manipulation and enhanced suture grasping.
- Scissors
- Gradle scissors are often used in Mohs surgery. These scissors have sharp, fine tips.[13]
- Specialized dissecting Gradle scissors are easily identified by black handles and are considered sharp and delicate. These scissors should only be used to handle tissue, not suture cutting.
- Iris scissors are a type of tissue scissors that have sharp tips with shorter handles. These scissors are also available in a hyper-sharp patented formulation and can cut tissue easily.
- Metzenbaum scissors are often employed for undermining. They have longer handles with blunt tips. There are variations of Metzenbaum scissors based on size and sharpness.[13]
- More specialized scissors include Westcott and Castroviejo spring-loaded scissors, which are only used on thin skin such as eyelid tissue.[13]
- Gradle scissors are often used in Mohs surgery. These scissors have sharp, fine tips.[13]
- Sutures (absorbable, non-absorbable, or both)
- Tissue Adhesives
Personnel
For intermediate and complex reconstruction, the surgeon, surgical technologist, and at least 1 assistant are required in the operating room.
Technique or Treatment
After histologic clearance is achieved with MMS, planning for reconstruction is the next step.
Reconstruction
- First, draw out the planned closure with attention to anatomic location, underlying structures, proximity to free margins, and the relaxed skin tension lines. Determine tissue mobility and standing cone placement.
- Administer local anesthetic and prep and drape the site.
- The defect can be closed centrally first, followed by removal and suturing of standing cones, or the standing cones can be removed first before suturing. The closure and the standing cones should be oriented to avoid encroaching or placing tension on free margins and adjacent structures. They should also be oriented within relaxed skin tension lines when possible. Standing cone excision should create a fusiform defect with a length-to-width ratio of approximately 3:1.[14] Convex surfaces such as the nasal dorsum and tip may require an extended closure line in a 4:1 to 5:1 ratio. The closure can also be designed as a crescent or S-plasty for improved placement in relaxed skin tension lines or to help accommodate curved surfaces such as the forearm.
- Undermining is performed when needed. Undermining can be blunt or sharp. The plane of undermining varies based on anatomic location. Care should be taken to avoid damaging underlying neurovascular structures.
- Hemostasis is achieved with electrosurgery and ligation of vessels as needed.
Suturing is a fundamental component of both intermediate and complex linear closures. Both require the repair of multiple tissue layers, including deeper subcutaneous tissue as well as dermal and epidermal components. Deeper layers of tissue are closed with delayed absorbing sutures, either monofilament or braided, with buried vertical mattress and buried pulley techniques. Deep closure of a wound is fundamental in relieving wound tension, reducing the likelihood of dehiscence, and improving cosmesis. Suture material is often chosen based on characteristics such as knot security, ease of handling, rates of absorption, and tensile strength.
Regarding monofilament versus braided absorbable sutures, there is little evidence to show whether they vary in functional and cosmetic outcomes. Traditionally, monofilament sutures are considered to have lower knot security and ease of handling but lower tissue reaction rates. Comparatively, braided sutures generally have better knot security and handling but can potentially harbor microorganisms and increase tissue reactivity.[15] The theoretical increased risk of infection with braided sutures is largely unsupported by the literature. Regarding monofilament versus braided absorbable sutures, evidence is lacking as to whether they vary in functional and cosmetic outcomes.[15] An example of a braided suture for deep closure is polyglactin 910. Monofilament examples include poliglecaprone 25 and polydioxanone.
Absorbable sutures are then placed in the subcutis and deep dermis using either a buried vertical mattress or set-back sutures, both of which evert the wound edges. Placing fascial plication sutures, multiple stacked layers of deep sutures, and/or buried pulley sutures should be considered for high-tension wounds.[16] Slipknots are also very useful for tying surgical knots in high-tension areas. Buried sutures may be placed in a left-to-right fashion or according to the "rule of halves" method. The area of maximum tension in a fusiform defect is in the center.[14]
Closure Once defect approximation and wound eversion are achieved with buried sutures, epidermal closure commences. Materials utilized are absorbable sutures, non-absorbable sutures, staples, or tissue adhesives.
- Interrupted sutures allow for segmented wound reinforcement without complete suture line failure if one separates. Simple interrupted is the most common technique, but modifications can be made to increase hemostasis (horizontal mattress) and eversion (horizontal and vertical mattress).
- Running suture allows for quicker placement and less strangulation of tissue in a focal area. However, suture breakage can create a critical failure of the entire superficial suture line.
- Running subcuticular suturing is another option that allows for buried intradermal placement of suture creating a superficial closure without suture penetration through the epidermis. This technique avoids suture track marks on the surface of the skin and is cosmetically appealing.[15] It is most useful in low-tension wounds.
- Absorbable and non-absorbable sutures both have utility in this setting.
- Non-absorbable sutures commonly used for epidermal approximation include polypropylene, nylon, and polyester.
- Absorbable sutures used for epidermal approximation include fast-absorbing gut, plain gut, and fast-absorbing polyglactin 910.
- Staples can also be used in select scenarios, such as on the scalp, as they are easier to use on terminal hair-bearing areas.
- If the wound is under low tension after deep sutures are placed, tissue adhesives such as 2-octyl cyanoacrylate or adhesive strips can be considered as a substitute for epidermal sutures.
Upon completion, a pressure bandage is placed on the closed suture line for 2 days, at which point the patient performs daily wound care with gentle washing, ointment, and a bandage until the incision is fully healed. If non-absorbable superficial sutures are placed, suture removal is performed at a later date. However, some studies suggest higher patient satisfaction with absorbable top sutures as they avoid the need for a return visit for suture removal.[17] The timeline for suture removal varies based on location.
Complications
Possible complications include poor wound healing, tissue necrosis, scarring, distortion of anatomy, nerve damage (most commonly manifested as loss of cutaneous sensation), excessive bleeding, hematoma formation, and infection.
Linear repair complications after MMS have a low incidence, reported at 0.5%.[18] Surgical site infection (SSI) rates for linear closures after Mohs are reported as <1%. SSI per body region in primary closure is 5% for the lower extremity, 2% for the upper extremity and trunk, and 1% for the head and neck.[19]
Closures near the eyelid may result in ectropion if not properly designed or if there are complications such as tissue necrosis. Poorly planned linear closures on the nose may compromise the nasal valve, causing functional issues.
Clinical Significance
MMS is the treatment of choice for qualifying skin malignancies due to optimal cure rates and tissue sparing. Linear repairs are commonly performed for the closure of Mohs defects. Literature suggests that dermatologists are the specialists using these repairs most often, and the definition change in 2020 has already influenced the reporting of closure types.[6][8]
Enhancing Healthcare Team Outcomes
The incorporation of MMS with intermediate and complex closure in the dermatologic surgical armamentarium has had a profound impact on healthcare outcomes. By minimizing tissue excision and optimizing wound closure, patient morbidity has been reduced with improved overall healthcare resource utilization. The emphasis on functional and cosmetic outcomes has enhanced patient satisfaction and improved psychological well-being and quality of life. Preservation of critical anatomical structures and minimizing functional impairments is paramount. This comprehensive approach exemplifies a paradigm shift in managing high-risk skin cancers, emphasizing tumor eradication and the preservation of patient quality of life and healthcare resources.
MMS requires a thorough understanding of technique, repair approach, complications, and wound management. The surgeon and team members are all critical to the success of the procedure and the postoperative healing course. Healthcare professionals in other specialties must be aware of Mohs surgery and closures to appropriately refer patients for the procedure and to help triage and manage any postoperative concerns or complications.
Media
(Click Image to Enlarge)
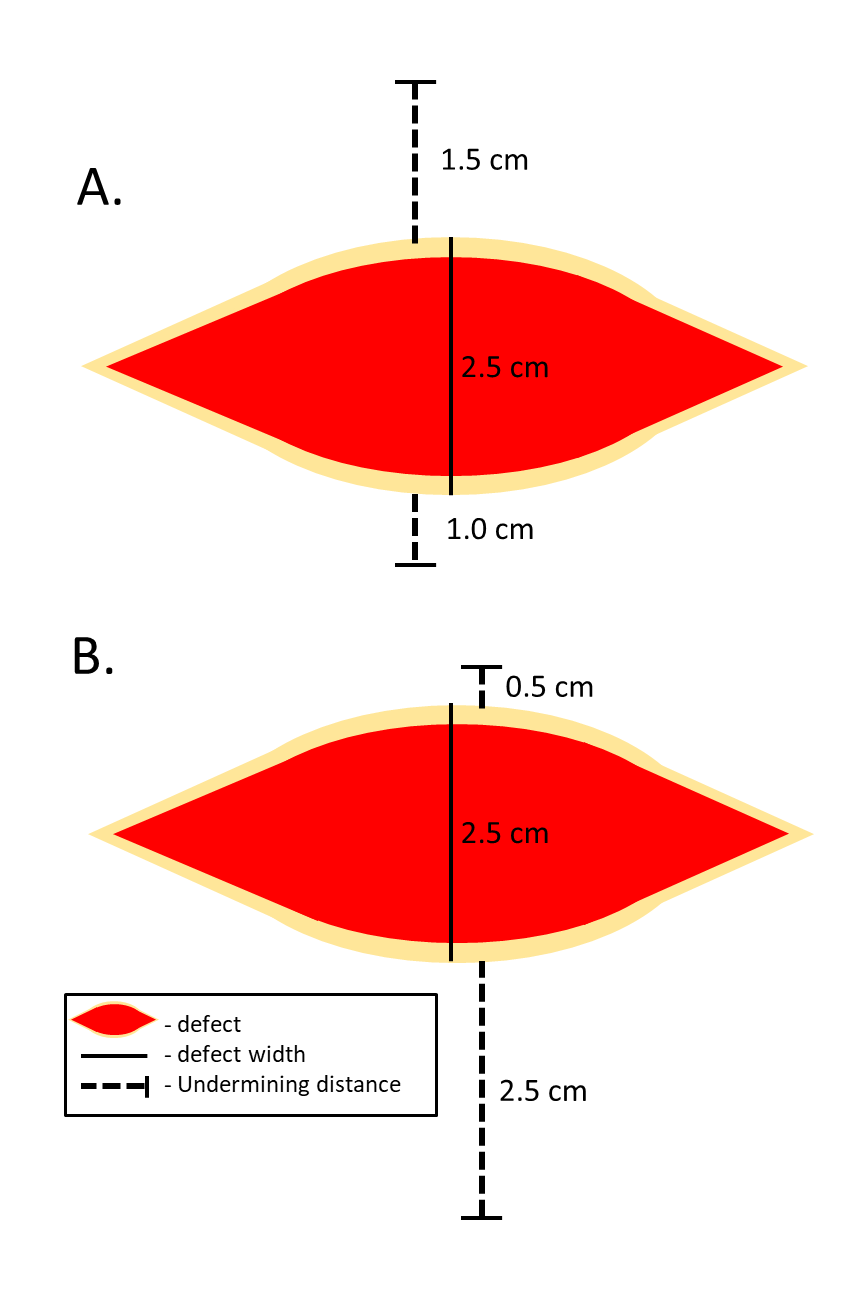
Intermediate versus Complex Closure. Intermediate repair is a multilayered repair type of cutaneous defects. Undermining can be performed in intermediate repairs but must not exceed the width of the defect on one side as show in part A. Complex repairs can include defects requiring undermining equal or greater to the defect width as shown in part B. Contributed by Austin Cusick, DO
References
Golda N, Hruza G. Mohs Micrographic Surgery. Dermatologic clinics. 2023 Jan:41(1):39-47. doi: 10.1016/j.det.2022.07.006. Epub 2022 Oct 28 [PubMed PMID: 36410982]
Mohs FE. Chemosurgery. Clinics in plastic surgery. 1980 Jul:7(3):349-60 [PubMed PMID: 7438703]
Mohs FE. Chemosurgery for skin cancer: fixed tissue and fresh tissue techniques. Archives of dermatology. 1976 Feb:112(2):211-5 [PubMed PMID: 60916]
Mohs FE. Chemosurgery for the microscopically controlled excision of cutaneous cancer. Head & neck surgery. 1978 Nov-Dec:1(2):150-66 [PubMed PMID: 755808]
Prickett KA, Ramsey ML. Mohs Micrographic Surgery. StatPearls. 2024 Jan:(): [PubMed PMID: 28722863]
Donaldson MR, Coldiron BM. Dermatologists perform the majority of cutaneous reconstructions in the Medicare population: numbers and trends from 2004 to 2009. Journal of the American Academy of Dermatology. 2013 May:68(5):803-8. doi: 10.1016/j.jaad.2013.01.026. Epub 2013 Feb 28 [PubMed PMID: 23453358]
Tan A, Castner NB, Slutsky JB. Mohs Surgeons Dominate Cutaneous Reconstructions in Cosmetically and Functionally Sensitive Sites: Medicare Trends From 2013 to 2019. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2023 Jun 1:49(6):539-543. doi: 10.1097/DSS.0000000000003787. Epub 2023 Mar 30 [PubMed PMID: 37000985]
Gronbeck C, Feng H. Distribution of intermediate and complex skin repairs performed by dermatologists following updated 2020 coding guidelines. Journal of the American Academy of Dermatology. 2023 Apr:88(4):954-956. doi: 10.1016/j.jaad.2022.11.032. Epub 2022 Nov 25 [PubMed PMID: 36436694]
Ad Hoc Task Force, Connolly SM, Baker DR, Coldiron BM, Fazio MJ, Storrs PA, Vidimos AT, Zalla MJ, Brewer JD, Smith Begolka W, Ratings Panel, Berger TG, Bigby M, Bolognia JL, Brodland DG, Collins S, Cronin TA Jr, Dahl MV, Grant-Kels JM, Hanke CW, Hruza GJ, James WD, Lober CW, McBurney EI, Norton SA, Roenigk RK, Wheeland RG, Wisco OJ. AAD/ACMS/ASDSA/ASMS 2012 appropriate use criteria for Mohs micrographic surgery: a report of the American Academy of Dermatology, American College of Mohs Surgery, American Society for Dermatologic Surgery Association, and the American Society for Mohs Surgery. Journal of the American Academy of Dermatology. 2012 Oct:67(4):531-50. doi: 10.1016/j.jaad.2012.06.009. Epub 2012 Sep 5 [PubMed PMID: 22959232]
Mazmudar RS, Sheth A, Tripathi R, Bordeaux JS, Scott JF. Inflation-Adjusted Trends in Medicare Reimbursement for Common Dermatologic Procedures, 2007-2021. JAMA dermatology. 2021 Nov 1:157(11):1355-1358. doi: 10.1001/jamadermatol.2021.3453. Epub [PubMed PMID: 34524396]
Feigenbaum L, Srivastava D, Nijhawan RI. Intraoperative retention sutures to facilitate closure. Journal of the American Academy of Dermatology. 2016 Dec:75(6):e229-e230. doi: 10.1016/j.jaad.2016.06.037. Epub [PubMed PMID: 27846971]
Ferrell K, Fancher W, Lear W. Use of a novel suture retention device to protect skin edges while using pulley suture technique for high-tension wound closure. Journal of the American Academy of Dermatology. 2020 Aug:83(2):e113-e115. doi: 10.1016/j.jaad.2019.04.030. Epub 2019 Apr 19 [PubMed PMID: 31009663]
Gandhi SA, Kampp JT. Dermatologic Surgical Instruments: A History and Review. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2017 Jan:43(1):11-22. doi: 10.1097/DSS.0000000000000911. Epub [PubMed PMID: 27749442]
Lear W, Roybal LL, Kruzic JJ. Forces on sutures when closing excisional wounds using the rule of halves. Clinical biomechanics (Bristol, Avon). 2020 Feb:72():161-163. doi: 10.1016/j.clinbiomech.2019.12.018. Epub 2019 Dec 23 [PubMed PMID: 31887483]
Butt E, Ashraf I, Veitch D, Wernham A. Dermatological surgery: an update on suture materials and techniques. Part 2. Clinical and experimental dermatology. 2021 Dec:46(8):1411-1419. doi: 10.1111/ced.14812. Epub 2021 Aug 26 [PubMed PMID: 34155674]
Lee CH, Wang T. A novel suture technique for high-tension wound closure: the tandem pulley stitch. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2015 Aug:41(8):975-7. doi: 10.1097/DSS.0000000000000422. Epub [PubMed PMID: 26177115]
Ashraf I, Butt E, Veitch D, Wernham A. Dermatological surgery: an update on suture materials and techniques. Part 1. Clinical and experimental dermatology. 2021 Dec:46(8):1400-1410. doi: 10.1111/ced.14770. Epub 2021 Jul 14 [PubMed PMID: 34056751]
Berens AM, Akkina SR, Patel SA. Complications in facial Mohs defect reconstruction. Current opinion in otolaryngology & head and neck surgery. 2017 Aug:25(4):258-264. doi: 10.1097/MOO.0000000000000375. Epub [PubMed PMID: 28509671]
Level 3 (low-level) evidenceChen A, Alsawas M, Tan KW, Prokop L, Murad MH, Powers JG. Surgical site infection rates following Mohs micrographic surgery by body site: A systematic review and meta-analysis. Journal of the American Academy of Dermatology. 2023 Oct:89(4):862-864. doi: 10.1016/j.jaad.2023.06.032. Epub 2023 Jun 24 [PubMed PMID: 37364613]
Level 1 (high-level) evidence