Introduction
Trauma continues to be the predominant cause of death for individuals up to the age of 44 years old.[1] There were a reported 1.2 million deaths due to road traffic crashes in 2018 globally. It has been anticipated that global death rates from road traffic accidents will increase by 67% due to the effects of rapid population growth and industrialization.[2] Despite traumatic brain injury being the leading cause of death from trauma, exsanguination continues to play a significant role. Among patients who arrive at the emergency department with trauma, hemorrhage is the leading cause of death within the first hour. Within the first 24 hours of arrival to the emergency department, nearly 50% of deaths result from hemorrhage.[1]
Hemorrhage is the leading cause of both maternal mortality and preventable trauma death worldwide.[3] These deaths could be preventable if the hemorrhage is stopped and lost blood is replaced with blood transfusion. Blood transfusion is an essential part of efficient healthcare and prevents millions of deaths each year.
Trauma patients also require a large number of hospital resources and are responsible for using approximately 70% of all blood transfused at a trauma center.[4] Transfusions also place a high burden on the cost of treatment. One study in England found that nearly 12% of their total financial cost was due to transfusions in traumatic patients.[5][6]
Transfusion protocols from donated cross-matched blood remain the standard treatment for the hemorrhagic patient, although it is not without risk and has potential adverse side effects. Transfusion of donated blood carries the risk of disease transmission, citrate toxicity, hyperkalemia, hypothermia, hypomagnesemia, acidosis, sepsis, respiratory failure, and thrombotic complications.[7][8][9][10] For these reasons, autotransfusion has widely been known as an alternative or adjunct to cross-matched transfusion therapy with fewer risks.
Autotransfusion has not always been a safe procedure. The first known documented procedure of autotransfusion was performed in 1818 by Dr. James Blundell. Dr. Blundell became frustrated by the loss of a patient due to a uterine hemorrhage. Blood transfusions had been attempted for many years before Dr. Blundell, but he was the first to attempt autotransfusion from experimentation with canine specimens. Later he would try his procedure on humans but not without risk. The estimated mortality rate from his procedures was approximately 75%.[11] Due to modern advancements in filtration and sterile technique, autotransfusion is widely accepted as a relatively safe procedure.
Indications
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Indications
The indications for autotransfusion are relatively straightforward and merit consideration in every trauma patient with active extravasation. However, often the more important question is to consider the contraindications.
For autotransfusion to be a worthwhile procedure, there should be signs of significant blood loss, typically greater than 1000 mL.[12][13] Additional indications include the need for immediate blood, the inability to obtain or provide cross-matched blood, and if the patient is unwilling to receive cross-matched blood.[14]
Differences in autotransfusion systems and indications for their use are influenced by resource availability.[15] In high-resource facilities, advanced systems for autotransfusion are in place for non-urgent surgery, such as cardiac, vascular, and orthopedic surgery. The blood stays in a confined space in these systems and does not come into contact with the external environment. In contrast, autotransfusion in low-resource settings is generally reserved for emergency surgeries, such as in ruptured ectopic pregnancy surgery, where presentation to the hospital is often late and access to blood is critical. This low-resource autotransfusion is generally a very basic technique, meaning the blood gets exposed to the air at some point. The technique has been referred to as a life-saving procedure and the last resort when no other options are left.[16]
The following are some recorded indications of autotransfusion:
- Ruptured ectopic pregnancy (REP)
- Ectopic pregnancy
- Hemothorax
- Vaginal postpartum hemorrhage
- Abdominal trauma and REP
- Blood from the peritoneal cavity
- Ruptured uterus
- Maternal hemorrhage
- Thyroid surgery
Contraindications
Although the indications may be relatively straightforward, it is important to note that there are numerous contraindications that, if ignored, can result in serious consequences. The first question is whether or not the source of blood has sustained contamination. Contamination can present as an infectious vs. noninfectious source. Infectious contamination can occur in any penetrating chest wound that may have pierced the diaphragm and affected the gastrointestinal tract. Careful inspection of the wound site is necessary, if possible, before using collected blood. If there is any ambiguity about its sterility, cross-matched blood should be used instead. Another source of contamination can include noninfectious sources. The use of blood from a site where a sterile solution may have been mixed with the blood (e.g., iodine, sterile water, alcohol, irrigation solutions, or chlorhexidine) should be avoided.[17][18] It should also be worth noting that any form of cavity introduced to hemostatic agents, such as thrombin, should also not be used.[18]
If it has been determined that the source of autotransfusion is contamination-free, there should be careful consideration for underlying pathology. If there is evidence of coagulopathy or evidence of disseminated intravascular coagulopathy (DIC), this requires management with specific blood component therapy instead of autotransfusion.[19]
Some literature supports the avoidance of autotransfusion in sickle cell disease and cesarean delivery as a relative contraindication until the completion of further studies.[17][20][21][22]
The following is a concise list of contraindications to autotransfusion:
- Septicemia
- Malignant cells in the bloodshed
- Renal or hepatic insufficiency
- Coagulopathies
- Blood that has been in the collection system for longer than institutional standards allow
Any of these contraindications could be rescinded if the patient is exsanguinating and there is not a sufficient supply of banked blood available.
Equipment
There are three types of autotransfusion systems in-line, self-filling, and continuous. In-line involves using a blood bag that collects the fluid for later use. The self-filling bag utilizes a vacuum to help improve the flow of fluid into the bag. Finally, the continuous autotransfusion uses an infusion pump and filter to directly place the blood into the patient's venous access. The advantage of a continuous system is that it is faster to transfuse, requires less staffing involvement after initial setup, and poses less risk of contamination. Continuous autotransfusion is often the method in the operating room, but many emergency departments do not have this type available and are more likely to utilize an in-line technique. There are various manufacturers of autotransfusion systems. Facilities should contact their supplier to see which system is available in their hospital as each may require additional, product-specific training.
The following equipment will be required to perform in-line autotransfusion.
- Sterile gown and gloves
- Face mask with a shield
- Hairnet or cap
- Sterile prep for patient's exposed skin (e.g., iodine or chlorhexidine)
- Blood collecting bag
- Microaggregate filter (typically 40 microns)
- 1 Liter sterile normal saline
- IV start kit with extension tubing.
- Pressure bag
- Citrate or heparin for anticoagulation
- Chest tube drainage kit with water seal
- Tube thoracostomy kit
A generalized list of equipment required is as follows:
- Personal protection equipment (i.e., gloves, mask, eyeshield)
- Chest-drainage unit
- Autotransfusion collection system
- Blood administration set
- 40- μ m microemboli filter
- Normal saline
- Wall suction and regulator
Preparation
Autotransfusion is most commonly used in the emergency department in trauma patients with evidence of a significant hemothorax. If the patient’s signs and symptoms display evidence of hemothorax, the preparation of autotransfusion should begin immediately before chest tube placement. If a chest tube is placed without the autotransfusion collecting bag in place, much of the blood will be lost during chest tube placement and may no longer be a viable option.
Preparation for a chest tube is common in other literature, but it is vital to maintain a strict sterile technique, including sterile gloves, a face mask with an eye shield, and a cap. In addition, the area of the skin should undergo prepping with iodine or chlorhexidine solution, and a sterile drape should be in place. A sterile setup is an essential factor in avoiding complications of infection.
The first step should be attaching the autotransfusion bag to the chest drain. An anticoagulant solution should be used to prime the system, and a steady drip of the anticoagulant solution should be mixed with the collected blood. Two types of anticoagulation are options: heparin and citrate. Heparin requires mixing with normal saline before administration with blood, whereas citrate can be mixed directly with the collected blood. Heparin does have the added risk of causing heparin-induced thrombocytopenia, and thus citrate is preferred over the use of heparin by many providers.
Heparin anticoagulation: A heparin anticoagulant solution can be formulated by mixing 30000 units of heparin with 1000 mL of normal saline.[13][21] The collecting bag should initially be primed with at least 100 mL of the anticoagulant solution before collecting blood and re-primed each time. While collecting the blood, the anticoagulant solution should be running at 13 to 15 mL per 100 mL of collected blood.[13][21] When approximately 500 mL of blood has been collected, it is ready to be reinfused.
Citrate anticoagulation: Citrate phosphate dextrose (CPD) can be added directly to the collected blood at a ratio of 1 mL of CPD to every 7 mL of blood. Another common method is to mix 60 mL of CPD into the autotransfusion bag prior to collecting the blood and then stop collection once the bag reaches 500 mL.
A microfilter should be attached to the tubing, and air must be removed from the autotransfusion bag.[23] It is important to note that a new filter and tubing are necessary for each autotransfusion bag. The collected blood can be stored at room temperature for up to six hours as needed, provided that collection takes place under aseptic conditions.
Patient Preparation
Providers should ensure the patient (or their surrogate) understands the procedural education. In a non-urgent setting, all questions should be answered as they arise, and information should be reinforced as necessary.
Technique or Treatment
There are various methods of performing autotransfusion with different techniques within the operating room and emergency department. The goal of autotransfusion remains the same, to maintain a sterile field, prevent clotting of the collected blood, filtration of the blood, and administration to the patient. The procedure should not take more than a few minutes to prepare, and the typical intent is an alternative or interim to alternative treatments. It is essential to familiarize oneself with the equipment provided at the treating facility to minimize the risks of infection and other complications.
Following are the steps of the procedure:
- Assemble collection system.
- Add anticoagulant into the autotransfusion bag prior to collecting the blood (this could vary based on the institution's protocols).
- Connect the patient's drainage system to the collection bag either directly or through a water-seal system.
- Before removing the filled collection bag for infusion, get a new collection bag ready.
- Close clamp on the new collection bag.
- Close the clamp on the chest drainage system.
- Remove the filled bag from the patient system, ensuring sterility at all times.
- Attach the previously prepared new collection bag to the water-seal unit or the chest or drainage tube.
- Ensure all connections are secured and open clamps on the patient drainage tubing and the autotransfusion bag.
- Prime the blood-administration tubing system with normal saline.
- Add the microfilter to the blood portion of the tubing and connect the filled collection bag.
- Start the infusion of the shed blood.
- Repeat this process as needed based on a reassessment of the patient following the initial transfusion.
- Discard supplies and equipment and remove personal protective equipment.
Complications
The most common complication of autotransfusion is blood loss if not properly connected. A common finding is chest tube placement, in which blood is found to be expressed and then wasted. The more serious complication includes blood contamination resulting in infection.[12][13][21] This issue is avoidable by using a sterile procedure for chest tube placement and careful handling of the lines and equipment. A continuous autotransfusion system can also help reduce the risk of infection, although not readily available in most emergency departments.
Other less common complications that merit consideration include hemodilution, hemolysis due to suction or degradation, air embolism, contamination of activated leukocytes, and thrombocytopenia.[12][17] Overall complications are avoidable using sterile technique and if less than 3000 mL of blood is reinfused.
Clinical Significance
An autotransfusion is a tool that should be considered in every trauma patient while in the emergency department. It can also be used in patients undergoing surgery or with anticipated blood loss, provided there are no contraindications. It has the benefit of reduced risk to the patient for transfusion reactions as well as possible cost-saving benefits. Autotransfusion can be used in conjunction with cross-matched blood and can help provide a temporary measure while waiting for cross-matched blood to arrive. The setup is relatively straightforward and does not require significantly extra time or resources.
Enhancing Healthcare Team Outcomes
An interprofessional team approach can help achieve the best possible outcomes in some of the highest mortality scenarios. Hemorrhage is the number one cause of death in trauma patients within the first hour, and often cross-matched blood is either not available or painfully delayed. Autotransfusion can provide a segway towards stabilizing the patient and often presents with fewer risks and fewer delays than cross-matched blood. Autotransfusion requires a team approach to ensure the procedure is performed effectively, safely, and with as few complications as possible. This interprofessional team approach includes providers, nursing, and laboratory scientists both in the preparation and execution of the procedure. [Level 5]
Before autotransfusion, the following should be in place:
- Early recognition by providers of the presenting patient that autotransfusion should be utilized
- Quick preparation from nursing staff of equipment required
- The sterile technique achieved providing a minimal risk of systemic infection
- Peripheral access with a blood sample sent to the lab for cross-match and additional laboratory testing if autotransfusion is not possible or insufficient
- Consultation to surgery if there is an inability to achieve hemostasis
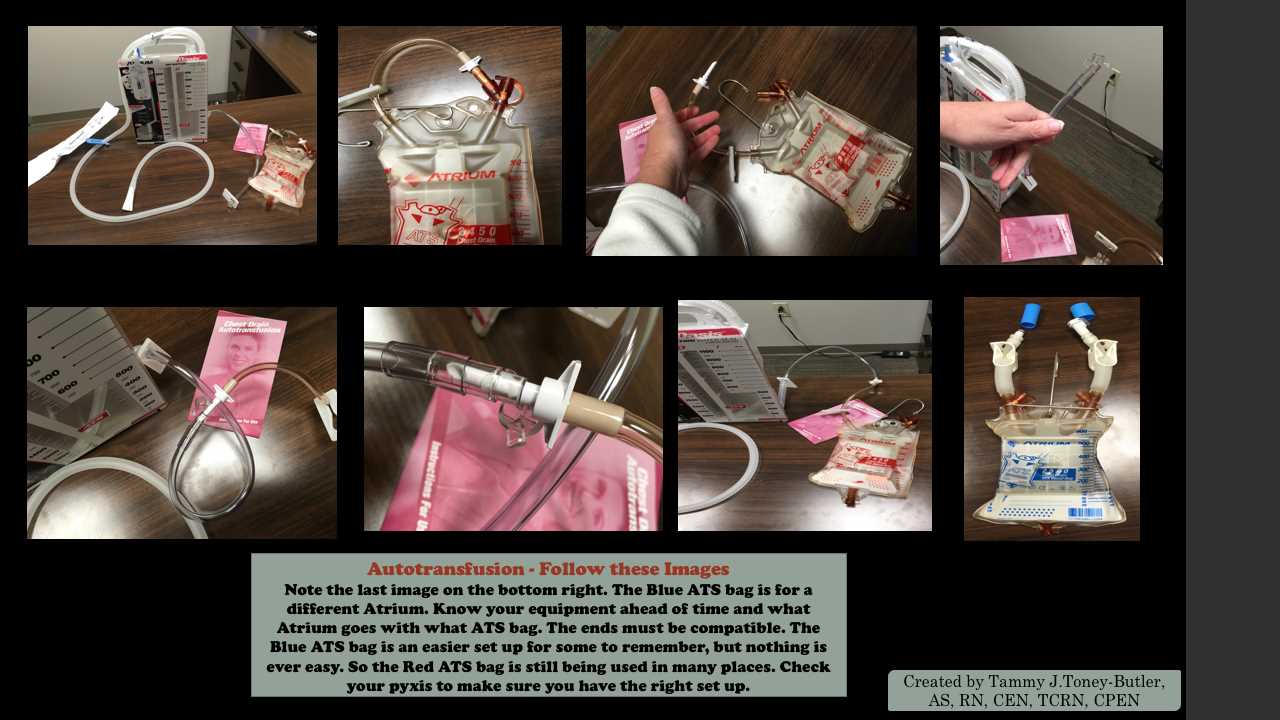
Media
(Click Image to Enlarge)
References
Moore K. Injury Prevention and Trauma Mortality. Journal of emergency nursing. 2016 Sep:42(5):457-8. doi: 10.1016/j.jen.2016.06.015. Epub [PubMed PMID: 27594080]
Pathak SM, Jindal AK, Verma AK, Mahen A. An epidemiological study of road traffic accident cases admitted in a tertiary care hospital. Medical journal, Armed Forces India. 2014 Jan:70(1):32-5. doi: 10.1016/j.mjafi.2013.04.012. Epub 2013 Aug 30 [PubMed PMID: 24623944]
Level 2 (mid-level) evidencePfeifer R,Tarkin IS,Rocos B,Pape HC, Patterns of mortality and causes of death in polytrauma patients--has anything changed? Injury. 2009 Sep; [PubMed PMID: 19540488]
Level 2 (mid-level) evidenceKauvar DS, Lefering R, Wade CE. Impact of hemorrhage on trauma outcome: an overview of epidemiology, clinical presentations, and therapeutic considerations. The Journal of trauma. 2006 Jun:60(6 Suppl):S3-11 [PubMed PMID: 16763478]
Level 3 (low-level) evidenceCampbell HE,Stokes EA,Bargo DN,Curry N,Lecky FE,Edwards A,Woodford M,Seeney F,Eaglestone S,Brohi K,Gray AM,Stanworth SJ, Quantifying the healthcare costs of treating severely bleeding major trauma patients: a national study for England. Critical care (London, England). 2015 Jul 6; [PubMed PMID: 26148506]
Duffy G,Tolley K, Cost analysis of autologous blood transfusion, using cell salvage, compared with allogeneic blood transfusion. Transfusion medicine (Oxford, England). 1997 Sep; [PubMed PMID: 9316218]
Perez P, Salmi LR, Folléa G, Schmit JL, de Barbeyrac B, Sudre P, Salamon R, BACTHEM Group, French Haemovigilance Network. Determinants of transfusion-associated bacterial contamination: results of the French BACTHEM Case-Control Study. Transfusion. 2001 Jul:41(7):862-72 [PubMed PMID: 11452153]
Level 2 (mid-level) evidenceWilliamson LM,Lowe S,Love EM,Cohen H,Soldan K,McClelland DB,Skacel P,Barbara JA, Serious hazards of transfusion (SHOT) initiative: analysis of the first two annual reports. BMJ (Clinical research ed.). 1999 Jul 3; [PubMed PMID: 10390452]
Kuehnert MJ,Roth VR,Haley NR,Gregory KR,Elder KV,Schreiber GB,Arduino MJ,Holt SC,Carson LA,Banerjee SN,Jarvis WR, Transfusion-transmitted bacterial infection in the United States, 1998 through 2000. Transfusion. 2001 Dec [PubMed PMID: 11778062]
Menis M, Forshee RA, Anderson SA, McKean S, Gondalia R, Warnock R, Johnson C, Mintz PD, Worrall CM, Kelman JA, Izurieta HS. Febrile non-haemolytic transfusion reaction occurrence and potential risk factors among the U.S. elderly transfused in the inpatient setting, as recorded in Medicare databases during 2011-2012. Vox sanguinis. 2015 Apr:108(3):251-61. doi: 10.1111/vox.12215. Epub 2014 Dec 3 [PubMed PMID: 25470076]
Level 2 (mid-level) evidenceBlundell J, Experiments on the Transfusion of Blood by the Syringe. Medico-chirurgical transactions. 1818; [PubMed PMID: 20895353]
Carless PA,Henry DA,Moxey AJ,O'Connell D,Brown T,Fergusson DA, Cell salvage for minimising perioperative allogeneic blood transfusion. The Cochrane database of systematic reviews. 2010 Apr 14; [PubMed PMID: 20393932]
Level 1 (high-level) evidenceKlein AA, Bailey CR, Charlton AJ, Evans E, Guckian-Fisher M, McCrossan R, Nimmo AF, Payne S, Shreeve K, Smith J, Torella F. Association of Anaesthetists guidelines: cell salvage for peri-operative blood conservation 2018. Anaesthesia. 2018 Sep:73(9):1141-1150. doi: 10.1111/anae.14331. Epub 2018 Jul 10 [PubMed PMID: 29989144]
Garcia JH, Coelho GR, Feitosa Neto BA, Nogueira EA, Teixeira CC, Mesquita DF. Liver transplantation in Jehovah's Witnesses patients in a center of northeastern Brazil. Arquivos de gastroenterologia. 2013 Apr:50(2):138-40 [PubMed PMID: 23903624]
Level 2 (mid-level) evidenceSelo-Ojeme DO,Onwude JL,Onwudiegwu U, Autotransfusion for ruptured ectopic pregnancy. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics. 2003 Feb; [PubMed PMID: 12566181]
Sjöholm A, Älgå A, von Schreeb J. A Last Resort When There is No Blood: Experiences and Perceptions of Intraoperative Autotransfusion Among Medical Doctors Deployed to Resource-Limited Settings. World journal of surgery. 2020 Dec:44(12):4052-4059. doi: 10.1007/s00268-020-05749-y. Epub 2020 Aug 27 [PubMed PMID: 32856098]
Waters JH, Indications and contraindications of cell salvage. Transfusion. 2004 Dec; [PubMed PMID: 15585004]
Esper SA,Waters JH, Intra-operative cell salvage: a fresh look at the indications and contraindications. Blood transfusion = Trasfusione del sangue. 2011 Apr; [PubMed PMID: 21251468]
Spahn DR, Bouillon B, Cerny V, Coats TJ, Duranteau J, Fernández-Mondéjar E, Filipescu D, Hunt BJ, Komadina R, Nardi G, Neugebauer E, Ozier Y, Riddez L, Schultz A, Vincent JL, Rossaint R. Management of bleeding and coagulopathy following major trauma: an updated European guideline. Critical care (London, England). 2013 Apr 19:17(2):R76. doi: 10.1186/cc12685. Epub 2013 Apr 19 [PubMed PMID: 23601765]
Level 1 (high-level) evidenceLim G,Melnyk V,Facco FL,Waters JH,Smith KJ, Cost-effectiveness Analysis of Intraoperative Cell Salvage for Obstetric Hemorrhage. Anesthesiology. 2018 Feb; [PubMed PMID: 29194062]
Waters JH, Intraoperative blood recovery. ASAIO journal (American Society for Artificial Internal Organs : 1992). 2013 Jan-Feb; [PubMed PMID: 23232181]
Waters JH, Lukauskiene E, Anderson ME. Intraoperative blood salvage during cesarean delivery in a patient with beta thalassemia intermedia. Anesthesia and analgesia. 2003 Dec:97(6):1808-1809. doi: 10.1213/01.ANE.0000087046.91072.E8. Epub [PubMed PMID: 14633564]
Level 3 (low-level) evidenceCatling S, Williams S, Freites O, Rees M, Davies C, Hopkins L. Use of a leucocyte filter to remove tumour cells from intra-operative cell salvage blood. Anaesthesia. 2008 Dec:63(12):1332-8. doi: 10.1111/j.1365-2044.2008.05637.x. Epub [PubMed PMID: 19032302]