Anatomy, Back, Posterior Longitudinal Ligament
Anatomy, Back, Posterior Longitudinal Ligament
Introduction
The posterior longitudinal ligament is one of the three more important ligaments that contribute to stability in the spine. This ligament passes along the posterior aspect of the vertebral body inside the vertebral canal from the body of the axis to the sacrum.[1] The ligament is composed of longitudinal fibers that are denser than the anterior longitudinal ligament. However, like the anterior longitudinal ligament, the denser fibers are deeper and span one vertebra, while the superficial fibers span three to four. The superficial layer is a continuation of the tectorial membrane at the axis, and the deep layer is a continuation of the cruciform ligament at the atlas.[2]
The fibers are wider at the intervertebral spaces and are more adherent to the annulus fibrosus of the intervertebral discs than at the vertebral body, where they are thinner. This phenomenon is more visible in the posterior ligament than in the anterior. Therefore, the posterior longitudinal ligament is much thinner than the anterior longitudinal ligament, which is significant for the pathophysiology of disc herniations occurring posterolaterally.[1]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The posterior longitudinal ligament (PLL) is composed of superficial and deep connective tissue layers, which can generally be distinguished by their morphology and fiber arrangement. The superficial layer is more posterior than the anterior. The distinction of the PLL from the dura mater is often difficult to determine.[1] The PLL consists of a central band of fibers 8 to 10 mm wide extending over several vertebral segments. Due to the PLL's broad attachment to the intervertebral disc, it has been described as "fanlike," giving it a denticulate appearance over each vertebral body. This denticulate appearance becomes more apparent in the lower thoracic and lumbar regions, where the superficial layer is more uniform in width.[3]
Nevertheless, there is considerable morphological variation even within the lumbar region, where both the central fibers and the "fanlike" portion appear to decrease in width between L1 and L5.[4] The deep layer, which adheres to the superficial layer in the midline, is of more uniform diameter throughout its length, being 2 to 3 mm wide at its narrowest point.[5] The PLL also has a denticulate appearance.
In the cervical region, the PLL is a wide bandlike structure similar in width over both the intervertebral disc and vertebral body. However, the ligament becomes increasingly denticulate more inferiorly, with its widest part being over the intervertebral disc (IVD). The separate fibers of the superficial and deep layers are difficult to identify at the level of the IVD, but their attachment to the margins of the vertebral bodies and intervening annulus fibrosus is clear.[6]
The fibers of each layer appear to merge, forming a common attachment. Both superficial and deep layers are attached to a midline bony septum on the posterior surface of the vertebral body between the superior and inferior margins. This attachment is not always continuous because of deficiencies in the septum in the central third of the vertebral body. The orientation of fibers within the PLL is consistent at all levels, with those in the central portion of the superficial layer being more vertical than those of the "fanlike" portion. Although the deep layer is visible through the superficial layer, its fiber orientation may not be established.[1]
The posterior longitudinal ligament has a more protective role than a supportive role. The observed pattern of migrations of foreign materials like masses and bony fragments following a vertebral fracture into the vertebral canal confirms that PLL protects the spinal cord from foreign objects and displaced disc material.[5]
Fibers of the superficial layer will limit forward flexion, while the oblique fibers of the deep layer will limit lateral flexion and rotation. However, research has suggested that fibers from both layers are involved in all movements, with an increasing number of fibers recruited with increasing load.[2] The more denticulate appearance of the PLL in the lower thoracic and lumbar regions may be due to the increased rotational and lateral flexion forces generated in the lower region compared with the upper regions of the vertebral column. The presence of elastin in the PLL supports the idea that the PLL has a role in the dynamic motion of the spine.[7] Observed patterns of disc fragment migration following vertebral burst fractures suggest that the PLL also protects the contents of the vertebral canal.[8]
Embryology
During the first six weeks of gestation, the vertebral column consists of a light zone and a dark zone. A hypocellular light zone represents the vertebral body, and a hypercellular dark zone represents the intervertebral disk.[9] At seven weeks, the light zone and dark zone become distinct, but the ligament is unclear. During the eighth week, the longitudinal arrangement of cells and collagen fibers appears at the location of the adult anterior longitudinal ligament.[10]
On the other hand, no longitudinal cell arrangement is identifiable at the location of the posterior longitudinal ligament. At ten weeks, the dark zone decreases in width, and the origin of the posterior longitudinal ligament appears. The structure is unclear at the level of the vertebral body but clear at the level of the disc.[9]
Blood Supply and Lymphatics
The primary source of blood supply to the spinal cord is from a single anterior spinal artery and the two posterior spinal arteries. These two arteries are the branches of the vertebral artery. Posterior arteries supply the posterior part of the spinal cord, and the anterior portion receives its blood supply from the anterior spinal artery.[11] Besides these arteries, there are other arteries at each spinal segment called radicular spinal arteries, which derive from the arteries of the body wall. The small penetrating arteries given off by both anterior and posterior spinal arteries anastomose in the spinal cord.
The radicular spinal arteries supply the dorsal and ventral parts of the spinal cord. The drainage of blood from the spinal cord takes place with the help of anterior and posterior spinal veins. These veins drain into the internal and external venous plexus. Through these plexuses, the blood drains into the main venous system with the help of azygos, lumbar, and hemiazygos veins.[12]
Nerves
The primary source of innervation of the posterior longitudinal ligament is the meningeal branch derived from the spinal nerve. It gives ascending and descending branches in the vertebral column.[13] There are transverse branches formed by the fusion of ascending and descending branches. The fusion of the transverse branches from the opposite side forms a network of nerve fibers superficially, which innervates the posterior longitudinal ligament in the vertebral segment. The posterior part of the annulus fibrosus is traversed by the nerve fibers forming a network deep in the intervertebral part of the posterior longitudinal ligament.[14]
There is no innervation of the deep layer of the nucleus pulposus or annulus fibrosus because they lack nerve fibers and nerve terminals. Only a few nerve terminals are present in the central part of the nucleus pulposus, but there are abundant nerve fibers in the peripheral zone. These nerve fibers in the peripheral zone play an important role in the regulation of movement and posture in the vertebral column.[13]
Muscles
There are three groups of muscle in the back; the superficial, intermediate, and deep muscle layers. The superficial layer consists of two muscles; splenius cervicis and splenius capitis. They play an important role in the extension of the neck and the movement of the shoulder.
The intermediate muscle group contains the longissimus, iliocostalis, and spinalis muscles. These form the erector spinae. All three muscles of the intermediate group have the same tendinous origin. These groups of muscles help in the flexion of the head and upper vertebral column and the movement of the thoracic cage. The deep layer consists of semispinalis, rotatores, and multifidus. The main function of this muscle group is the stabilization of the vertebral column and maintaining posture. These muscles also assist in balance and proprioception.[15]
Physiologic Variants
The posterior longitudinal ligament is narrower and weaker than the anterior longitudinal ligament. The PLL has an oval structure that varies from 2 to 2.25 mm in width at the level of L5-S1. From L5 upwards, the ligament forms a narrow band, which widens symmetrically at the level of each disc. The fibers of the annulus fibrosus and the edge of the vertebral body are the sites of attachment of the ligament. However, in some cases, it is attached to the posterior aspect of the vertebra.
The thickness of the ligaments at different levels is as follows:
- L5 1.3 mm
- L3 1.4 mm
- L2 0.9 mm [13]
The posterior longitudinal ligament seems to be most developed at the level of L3 and L4, where its average thickness is 1.4 mm. From L2 upwards, the ligament thins markedly. There is a thicker middle portion, approximately 2.5 to 4 mm in width, throughout the whole length of the ligament. The ligament in the mid-portion of each vertebral body covers the vascular foramina.[5]
Surgical Considerations
The pharmacologic management of the ossification of the longitudinal ligament is still not established. The standard treatment is surgical decompression of the spinal cord. Surgical management is done either by anterior decompression or by posterior decompression in modern medical practice.[16]
In the anterior surgical decompression, the ossified lesion is removed from the anterior side of the spine. Technically, this surgical procedure is difficult because of the anterior location of the posterior longitudinal ligament in the vertebral canal. Thus, posterior decompression is the choice of surgical procedure in treating the ossification of the posterior longitudinal ligament. Although posterior decompression is the surgical procedure of choice, complications may arise. Poor surgical outcomes are due to the following reasons.[17]
- Physiological kyphosis in the thoracic region
- The thoracic region of the spinal cord is the watershed region, predisposing to ischemic change.
Even after the surgical treatment, re-progression of ossification may occur. For young patients without any neurological deficits, strict radiological follow-up is recommended. For those with progressive deficits, surgery is the only possible treatment choice.[16]
Clinical Significance
Ossification of the posterior longitudinal ligament (OPLL) is an ectopic calcification in the tissue of the PLL. About 70% of the cases of OPLL develop in the cervical spine, but the condition may also be seen in the thoracic and lumbar spine. OPLL occurs more in males than in females. The symptoms commonly present in the 5th and 6th decades of life.[16]
Clinical Presentation
- Mild pain and discomfort in the early stage
- Clumsiness, dysesthesia, and tingling sensation in the hands
- Lower extremity symptoms, such as gait disturbances, may appear as the disease progresses. These may appear suddenly. Quadriplegia may occur even in apparently mild injuries.[17]
Pathogenesis
- The cause of the ossification of the posterior longitudinal ligament is still unknown; it appears to be a multifactorial disease. Genetic and non-genetic factors such as diet, obesity, age, diabetes mellitus, and physical strain on the posterior longitudinal ligament play an important role in the development of the disease.[18]
- Hypertrophic changes in the ligament itself are one of the mechanisms of ossification of the posterior longitudinal ligament.[19]
Diagnosis
A diagnosis of ossification of the posterior longitudinal ligament is based on radiological findings and clinical presentation. Since plain radiological examination has limitations, a CT scan or MRI is useful in diagnosing the condition. A CT scan will demonstrate the accurate shape and size of the ossified mass. CT can also help to classify the type of OPLL. Three-dimensional CT is sometimes used to quantify the volume of OPLL. MRI is used to detect the compression from OPLL and also helps to detect the extent of spinal cord compression.[20]
Other Issues
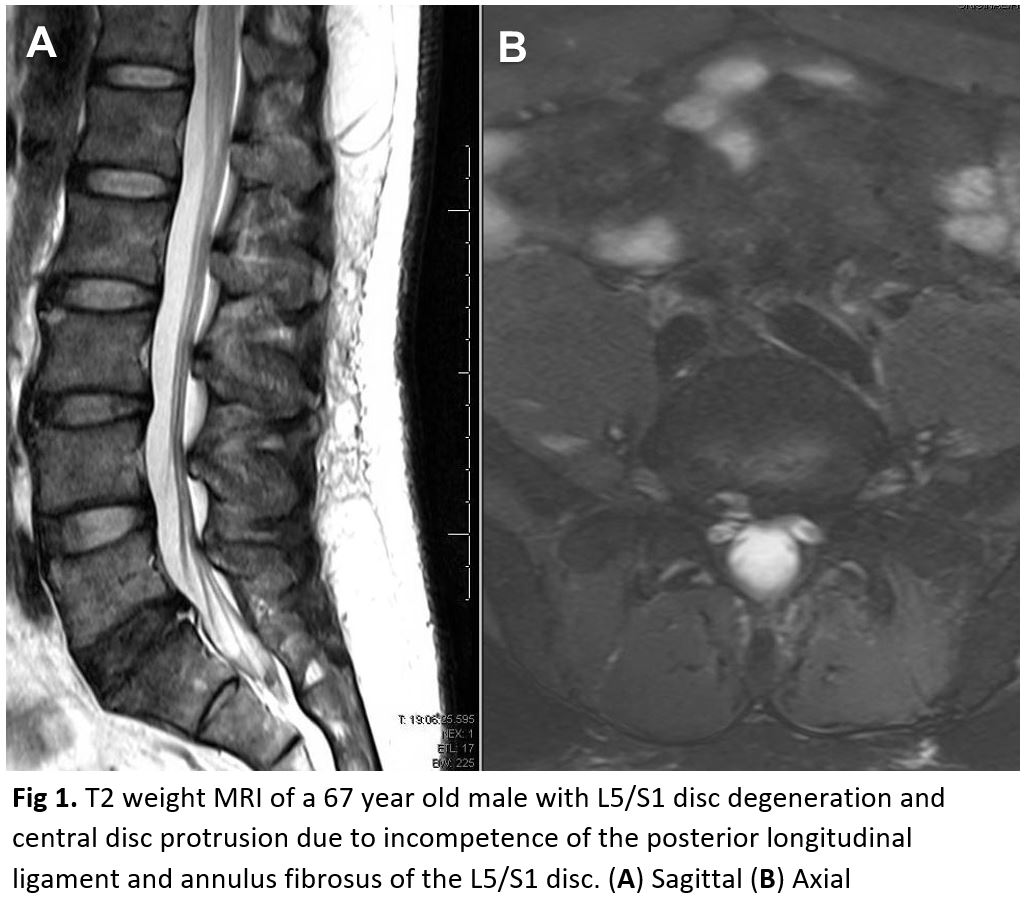
The displacement of the nucleus pulposus of the intervertebral disc into the dural sac is termed intradural disc herniation.[21] An intradural herniation is rare, occurring primarily in the lumbar spine (92%), about 5% in the thoracic spine, and about 3% in the cervical region. The exact cause of intradural herniation is still unknown, but the calcification of the posterior spinal longitudinal ligament is said to be the most likely cause of the herniation.[22]
Media
(Click Image to Enlarge)
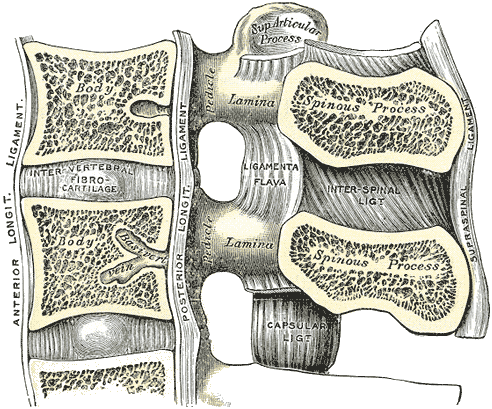
Lumbar Vertebral Anatomy. This medial sagittal section shows the relationship between the anterior longitudinal ligament, vertebral bodies, intervertebral fibrocartilage, posterior longitudinal ligament, vertebral laminae, ligamenta flava, superior articular processes, pedicles, spinous processes, interspinal ligament, capsular ligament, and supraspinal ligament.
Gray's Anatomy
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Loughenbury PR, Wadhwani S, Soames RW. The posterior longitudinal ligament and peridural (epidural) membrane. Clinical anatomy (New York, N.Y.). 2006 Sep:19(6):487-92 [PubMed PMID: 16283649]
Putz R. [Anatomic-functional viewpoints in treatment of injuries of the spine]. Langenbecks Archiv fur Chirurgie. Supplement. Kongressband. Deutsche Gesellschaft fur Chirurgie. Kongress. 1992:():256-62 [PubMed PMID: 1493274]
Behrsin JF, Briggs CA. Ligaments of the lumbar spine: a review. Surgical and radiologic anatomy : SRA. 1988:10(3):211-9 [PubMed PMID: 3147534]
Oshima H, Ishihara H, Urban JP, Tsuji H. The use of coccygeal discs to study intervertebral disc metabolism. Journal of orthopaedic research : official publication of the Orthopaedic Research Society. 1993 May:11(3):332-8 [PubMed PMID: 8326439]
Level 3 (low-level) evidenceWiltse LL. Anatomy of the extradural compartments of the lumbar spinal canal. Peridural membrane and circumneural sheath. Radiologic clinics of North America. 2000 Nov:38(6):1177-206 [PubMed PMID: 11131629]
Salaud C, Ploteau S, Hamel O, Armstrong O, Hamel A. Morphometric study of the posterior longitudinal ligament at the lumbar spine. Surgical and radiologic anatomy : SRA. 2018 May:40(5):563-569. doi: 10.1007/s00276-017-1964-2. Epub 2017 Dec 29 [PubMed PMID: 29288395]
Nakagawa H, Mikawa Y, Watanabe R. Elastin in the human posterior longitudinal ligament and spinal dura. A histologic and biochemical study. Spine. 1994 Oct 1:19(19):2164-9 [PubMed PMID: 7809748]
Schellinger D, Manz HJ, Vidic B, Patronas NJ, Deveikis JP, Muraki AS, Abdullah DC. Disk fragment migration. Radiology. 1990 Jun:175(3):831-6 [PubMed PMID: 2343133]
Misawa H, Ohtsuka K, Nakata K, Kinoshita H. Embryological study of the spinal ligaments in human fetuses. Journal of spinal disorders. 1994 Dec:7(6):495-8 [PubMed PMID: 7873846]
Butt AM, Gill C, Demerdash A, Watanabe K, Loukas M, Rozzelle CJ, Tubbs RS. A comprehensive review of the sub-axial ligaments of the vertebral column: part II histology and embryology. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2015 Jul:31(7):1061-6. doi: 10.1007/s00381-015-2730-6. Epub 2015 May 5 [PubMed PMID: 25939717]
Bosmia AN, Hogan E, Loukas M, Tubbs RS, Cohen-Gadol AA. Blood supply to the human spinal cord: part I. Anatomy and hemodynamics. Clinical anatomy (New York, N.Y.). 2015 Jan:28(1):52-64. doi: 10.1002/ca.22281. Epub 2013 Jun 27 [PubMed PMID: 23813725]
Gofur EM, Singh P. Anatomy, Back, Vertebral Canal Blood Supply. StatPearls. 2023 Jan:(): [PubMed PMID: 31082127]
Tkaczuk H. Tensile properties of human lumbar longitudinal ligaments. Acta orthopaedica Scandinavica. 1968:():Suppl 115:1+ [PubMed PMID: 5707337]
Kojima Y, Maeda T, Arai R, Shichikawa K. Nerve supply to the posterior longitudinal ligament and the intervertebral disc of the rat vertebral column as studied by acetylcholinesterase histochemistry. I. Distribution in the lumbar region. Journal of anatomy. 1990 Apr:169():237-46 [PubMed PMID: 2384336]
Level 3 (low-level) evidenceHenson B, Kadiyala B, Edens MA. Anatomy, Back, Muscles. StatPearls. 2024 Jan:(): [PubMed PMID: 30725759]
Smith ZA, Buchanan CC, Raphael D, Khoo LT. Ossification of the posterior longitudinal ligament: pathogenesis, management, and current surgical approaches. A review. Neurosurgical focus. 2011 Mar:30(3):E10. doi: 10.3171/2011.1.FOCUS10256. Epub [PubMed PMID: 21361748]
Matsuyama Y, Yoshihara H, Tsuji T, Sakai Y, Yukawa Y, Nakamura H, Ito K, Ishiguro N. Surgical outcome of ossification of the posterior longitudinal ligament (OPLL) of the thoracic spine: implication of the type of ossification and surgical options. Journal of spinal disorders & techniques. 2005 Dec:18(6):492-7; discussion 498 [PubMed PMID: 16306836]
Level 2 (mid-level) evidenceOno K, Yonenobu K, Miyamoto S, Okada K. Pathology of ossification of the posterior longitudinal ligament and ligamentum flavum. Clinical orthopaedics and related research. 1999 Feb:(359):18-26 [PubMed PMID: 10078125]
Kondo S, Onari K, Watanabe K, Hasegawa T, Toguchi A, Mihara H. Hypertrophy of the posterior longitudinal ligament is a prodromal condition to ossification: a cervical myelopathy case report. Spine. 2001 Jan 1:26(1):110-4 [PubMed PMID: 11148654]
Level 3 (low-level) evidenceSartip KA, Dong T, Ndukwe M, East JE, Graves JA, Davis B, Midyett FA, Duerinckx A. Ossification of the Posterior Longitudinal Ligament: Imaging Findings in the Era of Cross-Sectional Imaging. Journal of computer assisted tomography. 2015 Nov-Dec:39(6):835-41. doi: 10.1097/RCT.0000000000000303. Epub [PubMed PMID: 26418541]
Level 2 (mid-level) evidenceYang HS, Oh YM, Eun JP. Cervical Intradural Disc Herniation Causing Progressive Quadriparesis After Spinal Manipulation Therapy: A Case Report and Literature Review. Medicine. 2016 Feb:95(6):e2797. doi: 10.1097/MD.0000000000002797. Epub [PubMed PMID: 26871842]
Level 3 (low-level) evidenceD'Andrea G, Trillò G, Roperto R, Celli P, Orlando ER, Ferrante L. Intradural lumbar disc herniations: the role of MRI in preoperative diagnosis and review of the literature. Neurosurgical review. 2004 Apr:27(2):75-80; discussion 81-2 [PubMed PMID: 14564663]
Level 3 (low-level) evidence