Introduction
An M-plasty is an excisional technique used to remove standing cutaneous deformities, also known as dog ears, from the end of a linear wound repair. Dog ears arise from the bunching of tissue when overly obtuse angles (>30 degrees) are used at the ends of surgical excisions. Many different techniques address dog ears. The primary non-excisional technique involves distributing the excess skin on one side of the incision evenly relative to the other side by placing sutures at larger intervals on the longer side of the incision relative to the shorter side. This approach may not work in all situations and is dependent upon the amount of excess tissue and the length of the wound. For example, this technique will have a limited impact on short incisions or large dog ears. The most commonly employed surgical option to remove a dog ear is to excise the excess tissue directly. A triangular piece of tissue, known as a Burow's triangle, can be removed anywhere along the length of the incision. Typically, a Burow's triangle is taken at the end of the incision, increasing the scar's final length.[1]
An M-plasty is an alternative to this technique and has the additional benefit of shortening the final wound length to conserve normal tissue.[2] In some instances, an M-plasty may be used on the end of an incision to avoid crossing an aesthetic subunit boundary or violating an otherwise intact and uninvolved structure, albeit at the expense of adding a fork to the end of the incision. This application of M-plasty may adversely impact the aesthetic acceptability of the final result.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Aesthetically, the face is divided up into several subunits: forehead, brows, orbits, nose, cheeks, mouth, chin, and ears, each of which has its own constituent parts with additional boundaries among them. In many cases, keeping scars within a single subunit or, preferable, between subunits can substantially improve cosmetic results. In these situations, using an M-plasty to limit or redirect the scar into subunit boundaries can be very helpful. Additionally, many anatomical structures on the face possess free margins, such as the nasal alae, the auricular helices, the eyebrows, the hairline, and the eyelids, violation of which is best avoided to prevent cicatricial notching; M-plasties can be very useful in these cases as well.[3][4]
Indications
An M-plasty is a useful technique for shortening the expected final scar length of an excision.[5][6][7] This can be beneficial when longer incisions are contraindicated to avoid crossing cosmetic boundaries or extending into sensitive structures. For example, an M-plasty can be used near the lateral canthus to remove a dog ear without disrupting the corner of the eye. This is also an ideal location for an M-plasty because the scar can be concealed within the crow’s feet. The M-plasty technique is also applicable in the glabellar region when complete fusiform excision would extend the scar into the medial canthi, but an M-plasty can be used to branch the incisions into the upper and lower eyelids.[8] While M-plasty is typically employed in the closure of wounds resulting from excision of skin lesions, it is also helpful in the closure of full-thickness skin graft donor site defects.[9]
Additionally, an M-plasty may be used to remove dog ears created by flaps. M-plasties can be added to either one or both ends of an incision to shorten a wound. Although M-plasties decrease the length of a scar, they increase its width by adding a fork to the end. This compromise may be cosmetically less noticeable than long, linear scars in some cases. For example, large tumors on the back may be less noticeable with an M-plasty on each end when compared to a longer, straight repair. The main goal of the M-plasty is to take an excision that would otherwise extend across cosmetic unit boundaries and keep the incision within a single unit.
Lastly, the use of the M-plasty has also been described for the orientation of pathological specimens, an application that may conserve suture and tissue at the same time.[10]
Contraindications
It is important to note that a traditional M-plasty, unlike a Z-plasty, does not alter tension vectors. For this reason, the contraindications for M-plasty are the same as the contraindications for primary closures. Primary wound closure is contraindicated when there would be too much tension on the wound to permit a reliable closure. Excess tension can lead to dehiscence and/or necrosis of the wound edges because of stretching and subsequent narrowing of the microvasculature in the subdermal plexus. Increased tension can also lead to poor cosmetic outcomes, such as wide, fish-mouth-like scars. More importantly, excessive tension can cause anatomic distortion of sensitive structures such as the eyelid, eyebrow, nasal ala, auricle, or lips.
Equipment
Equipment will vary depending on the size and location of the wound, but in general, terms will consist of the following:
- Skin marker
- Suture for the skin surface
- Suture for the deep layer
- Needle driver
- Forceps
- Suture scissors
- #15 blade scalpel
- Electrocautery or other hemostatic equipment
- Dissecting scissors, such as Metzenbaum or Kaye blepharoplasty
Personnel
This procedure can be performed by the surgeon alone. However, an assistant can be quite helpful and improves the procedure's efficiency. If excision of a skin lesion causes a defect that requires an M-plasty for closure, a pathologist may be necessary. Anesthetic and nursing requirements will be dictated by the size and location of the excision.
Preparation
Cutaneous surgery can be performed in an office setting. Sterile or nonsterile gloves may be used at the surgeon's discretion as the risk of surgical site infections in minor procedures is low, particularly when they are performed on the face, where the blood supply and immune response are robust. The skin is prepped with an antiseptic based on the site of surgery and the surgeon's preference.[11][12]
Patient Counseling
The surgeon should counsel the patient about the risks of the procedure, namely infection, bleeding, unsightly scarring, and the likelihood of recurrence of any lesion being excised. The patient should also receive a thorough explanation of the procedure. This explanation can be supplemented with visual aids such as a picture of the tumor with the planned excision illustrated. Visual aids can also show the patient how the closure will look after the excision is performed. When cosmetically sensitive areas, such as the face, are involved, the patient should also be counseled regarding the risk of dissatisfaction with the ultimate appearance of the scar. Scars located in cosmetically sensitive areas should be protected from sun exposure for roughly 12 months postoperatively to prevent the development of dyspigmentation.
Technique or Treatment
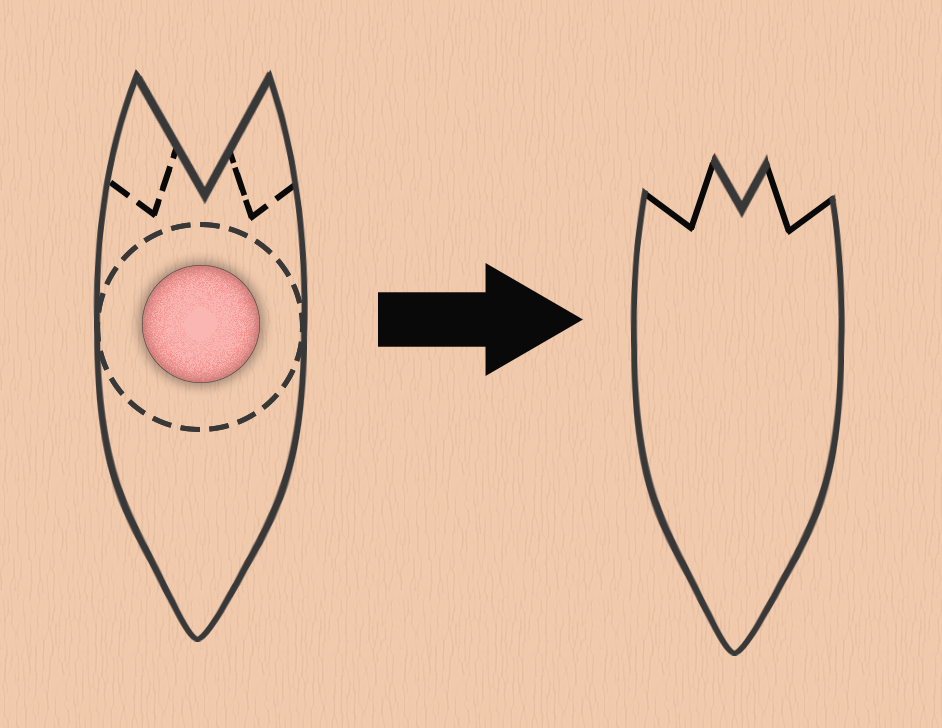
An M-plasty may be designed before excision or later in the repair process. The design is best visualized by first drawing out a fusiform excision. To add an M-plasty to one end of the excision, the peak of the planned excision is inverted or folded inward on itself to create an "M" (see figure) with 30 degrees angles at and between the tips of the M. Tips with angles substantially >30 degrees may result in additional standing cutaneous dog ear deformities. Take care not to make the M so deep that it intrudes on the lesion itself and compromises the oncological integrity of the resection, if applicable. It is preferable to draw the excision margins around the lesion first and then overlay the planned M-plasty. The skin is incised in the standard fashion. Undermining is performed in the appropriate plane depending on the body location, generally subdermal. The final configuration of an M-plasty is a "Y," with the base representing the linear closure and the arms of the "Y" representing the M-plasty. Sutures may be placed in either a running or an interrupted fashion and will often be placed in layers, depending on the depth and location of the excision. The tip of the M-plasty may benefit from the placement of a tip stitch to align the tissue properly.[6][13]
If an M-plasty is used to remove a dog ear, the dog ear is elevated with forceps, then two incisions are made at 45 degrees angles from the main incision on either side of the dog ear, and Burow's triangles are removed. This creates a "Y" shaped closure. The excess tissue is removed from the sides of the incision, sparing the "V" created between the two new incisions. The wound is then closed in the same fashion as above.
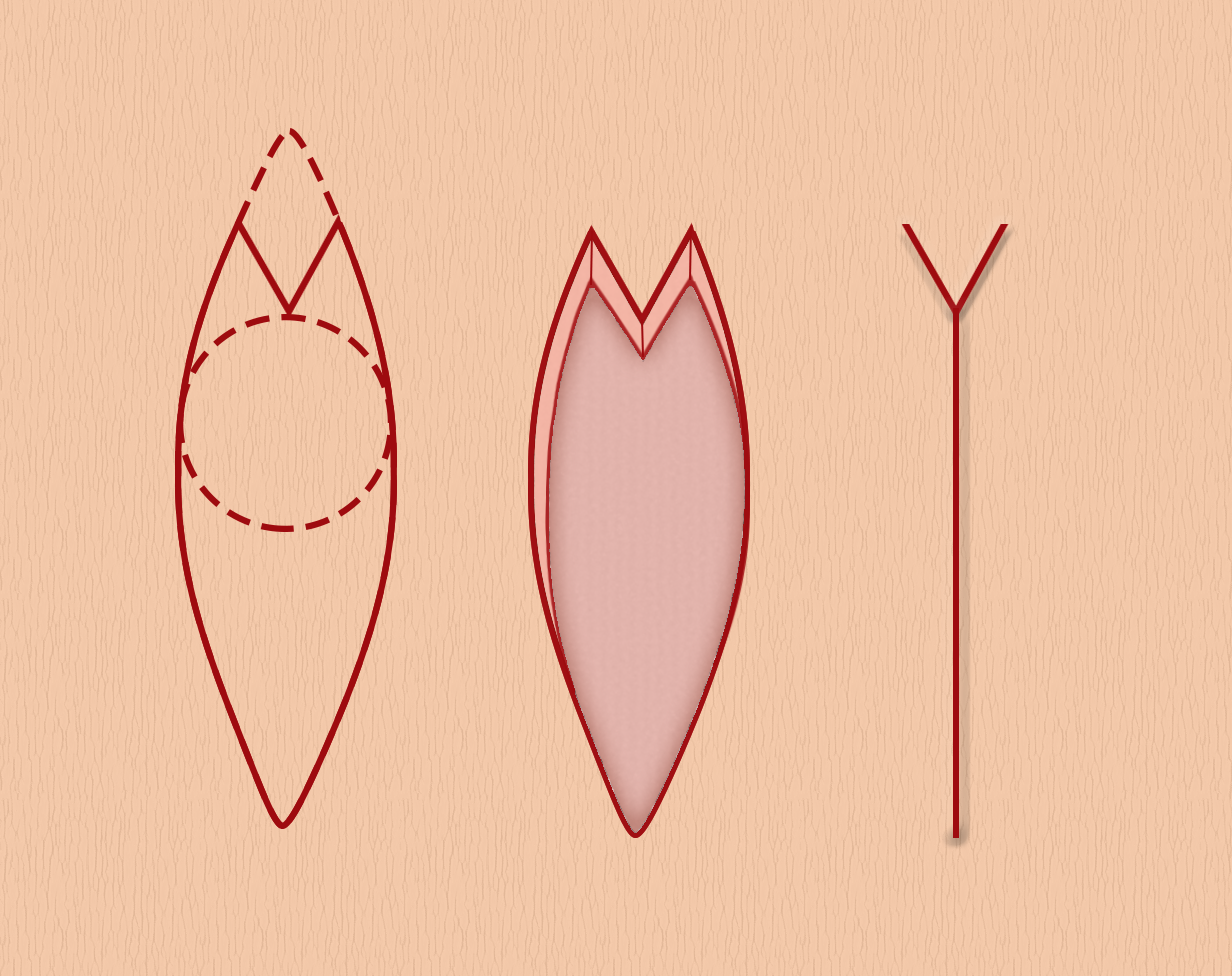
Nested M-Plasty
A nested M-plasty is a variant of a traditional M-plasty and can be described as an M-plasty within an M-plasty. If a standard M-plasty shortens the length of the scar and preserves healthy tissue, performing the process twice produces even shorter scars and preserves even more tissue, albeit at the expense of a more complicated procedure and a complex, branched scar. A standard M-plasty can be visualized as an ellipse with the peak of the ellipse folded inward. This produces two side-by-side triangles that are half the width of the original peak. A nested M-plasty repeats this process within one or both of those triangles. The triangles are folded on themselves again, creating four side-by-side triangles that are one-quarter the original width, resulting in a branching appearance (see figure). As with a regular M-plasty, tip stitches can be quite useful for this type of closure. This technique is best used on flat or concave surfaces as it can induce bunching of the skin, which typically flattens out with time. Bunching of skin over convex surfaces can be quite noticeable and tends to persist; it should therefore be avoided via meticulous incision design and closure[14].
M-Plasty Modifications
The modified M-plasty, described by Asken in 1986, uses a shortened ellipse with obtuse angles and places additional tangential incisions on opposite sides of the ellipse at either end of the wound. The closure is accomplished with local undermining and adjustment of tension vectors; the final scar is Y-shaped, like a traditional M-plasty but shorter still.[15] Another variant of the M-plasty modifies the angle of divergence between the two triangles such that they exceed 30 degrees and the bases of the triangles remain separated by a distance equal to the maximum width of the ellipse. Using this technique, the compressive forces that bunch up the skin begin to subside, and the M-plasty takes on some of the tension-altering characteristics of a V to Y advancement closure.[16]
Complications
Complications arising from M-plasty parallel those seen with any other wound closure technique. In addition to pain, bleeding, infection, and need for revision surgery, there remains the possibility of cosmetically unsatisfactory scarring. Patients may find that the forked nature of the final scar is noticeable, or the scar itself may ultimately become wide, raised, depressed, pigmented, pale, or erythematous. Standing cutaneous deformities may also arise if the M-plasty is not designed appropriately or if healing does not occur as expected. Management of unsightly scarring may include topical therapies, such as silicone gel or hydroquinone, skin resurfacing, ablative or non-ablative laser treatments, intense pulsed light treatments, and surgical revision.
Clinical Significance
The M-plasty is a tissue-sparing technique that permits primary wound closure while limiting incision length. The technique can also be used to remove standing cutaneous dog ear deformities. Every cutaneous surgeon should be facile with the planning and execution of M-plasty closures.
Enhancing Healthcare Team Outcomes
M-plasty is usually performed by a plastic or cosmetic surgeon and an assistant or nurse, occasionally with the efforts of an anesthesiologist. Patients with skin lesions approaching aesthetic boundaries or who have undergone excisions that left standing cutaneous deformities should be referred for evaluation for scar revision and potential M-plasty. The procedure should be performed by a surgeon who has experience with cutaneous procedures and wound management. [Level 4]
Nursing, Allied Health, and Interprofessional Team Interventions
Depending on the location of the wound, nurses may be called upon to remove sutures one to two weeks after surgery. When procedures occur in cosmetically sensitive areas, such as the face, nursing staff may also counsel patients on the importance of protecting the healing wound from ultraviolet light exposure to minimize unsightly scar formation. Patients should keep the wound covered or apply sunscreen with a solar protection factor (SPF) of at least 30 when outside and should continue to do this until the scar has matured completely, approximately one year after surgery.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
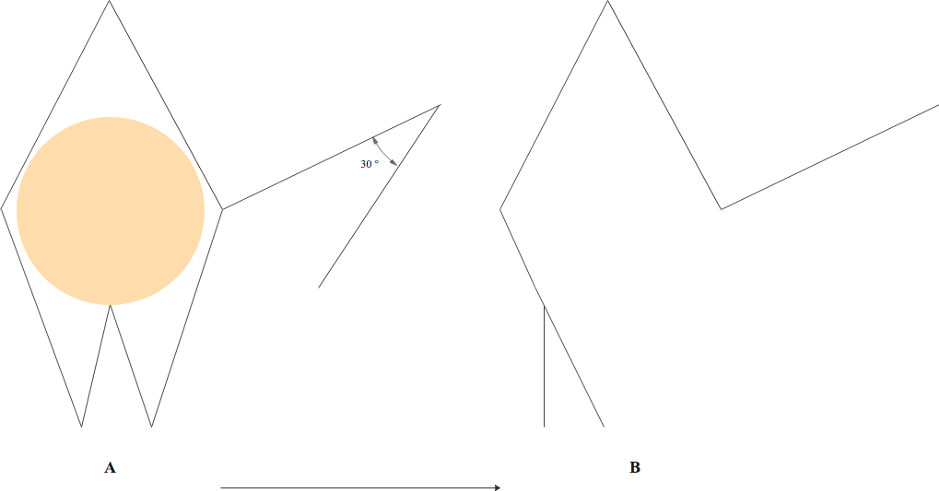
Webster Rhombic Flap Modification. A 30° flap tip angle is combined with M-plasty to close the defect base. A: The defect (orange) is extended into a modified rhomboid shape with a 30° flap. B: Wound closure lines follow flap transposition with an M-plasty closure of the defect base and donor site.
Contributed by E Wilkinson and P Macneal, MBChB
Webster R, Davidson T, Smith R. The thirty degree transposition flap. Laryngoscope. 1978;88.(1):85–94
(Click Image to Enlarge)
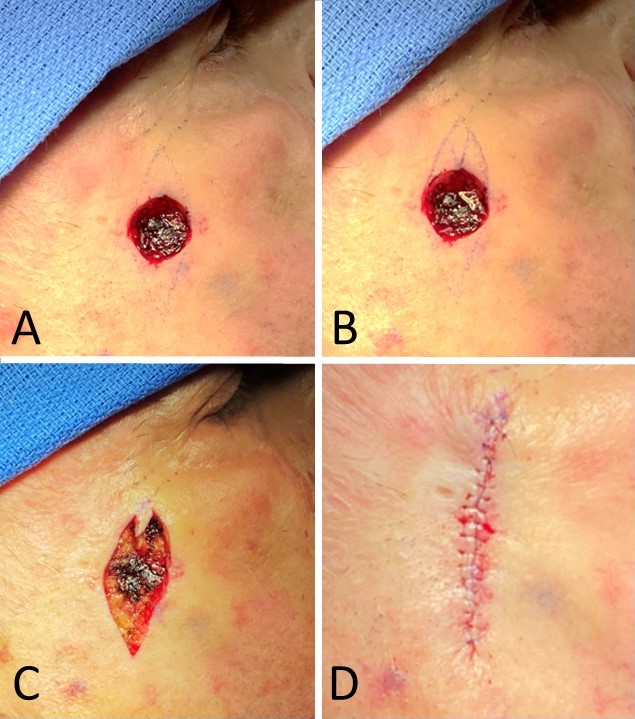
M-Plasty Technique. The M-plasty closes basal cell carcinoma resection defect inferolateral to the eye. This technique was used at the superomedial end of the incision to hide it in the crow's feet rhytides. A) Defect with standard fusiform excision and closure planned. B) The defect with M-plasty is planned at the superomedial end. C) M-plasty and inferolateral Burow's triangle excised. D) The incision is closed, with the final shape in the form of the letter Y.
Contributed by MH Hohman, MD, FACS
References
Dzubow LM. The dynamics of dog-ear formation and correction. The Journal of dermatologic surgery and oncology. 1985 Jul:11(7):722-8 [PubMed PMID: 4008741]
Meybodi F, Pham M, Sedaghat N, Elder E, French J. The Modified M-plasty Approach to Mastectomy: Avoiding the Lateral Dog-ear. Plastic and reconstructive surgery. Global open. 2022 Feb:10(2):e4116. doi: 10.1097/GOX.0000000000004116. Epub 2022 Feb 18 [PubMed PMID: 35198347]
Field LM. The combination of a cheek advancement-rotation flap with an M-plasty for upper preauricular excisions. The Journal of dermatologic surgery and oncology. 1985 Oct:11(10):974-6 [PubMed PMID: 4044981]
Field LM. Hairline reconstruction utilizing modified winged V-plastic hair-bearing flaps and focal anastomotic line excisions. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 1996 Nov:22(11):937-40 [PubMed PMID: 9063509]
Level 3 (low-level) evidenceWeisberg NK, Nehal KS, Zide BM. Dog-ears: a review. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2000 Apr:26(4):363-70 [PubMed PMID: 10759826]
Webster RC, Davidson TM, Smith RC, Kitchens GG, Clairmont AA, Schwartzenfeld TH, Smith RR, White BJ Jr, Bush J, Cook TA, Johnson CM, White MF. M-plasty techniques. The Journal of dermatologic surgery. 1976 Nov:2(5):393-6 [PubMed PMID: 993442]
Modica LA, Leicht SS. M-plasty for large cheek defects. American family physician. 1987 Jan:35(1):123-4 [PubMed PMID: 3799414]
Level 3 (low-level) evidenceCamacho FM, García-Hernandez MJ, Pérez-Bernal AM. M-plasty in the treatment of carcinomas located on the interglabellar region. European journal of dermatology : EJD. 1998 Dec:8(8):548-50 [PubMed PMID: 9889425]
Level 2 (mid-level) evidenceDaichi M, Fumio O, Nobuhiro S. M-plasty for Full-Thickness Skin Graft Donor Site. Eplasty. 2015:15():ic54 [PubMed PMID: 26483862]
Swanson NA, Tromovitch TA, Stegman SJ, Glogau RG. The M-plasty as a means of orienting a surgical specimen for the pathologist. The Journal of dermatologic surgery and oncology. 1980 Sep:6(9):706-7 [PubMed PMID: 6999047]
Xia Y, Cho S, Greenway HT, Zelac DE, Kelley B. Infection rates of wound repairs during Mohs micrographic surgery using sterile versus nonsterile gloves: a prospective randomized pilot study. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2011 May:37(5):651-6. doi: 10.1111/j.1524-4725.2011.01949.x. Epub 2011 Apr 1 [PubMed PMID: 21457390]
Level 3 (low-level) evidenceRhinehart MB, Murphy MM, Farley MF, Albertini JG. Sterile versus nonsterile gloves during Mohs micrographic surgery: infection rate is not affected. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2006 Feb:32(2):170-6 [PubMed PMID: 16442035]
Level 2 (mid-level) evidenceSalasche SJ, Roberts LC. Dog-ear correction by M-plasty. The Journal of dermatologic surgery and oncology. 1984 Jun:10(6):478-82 [PubMed PMID: 6373868]
Krishnan RS, Donnelly HB. The nested M-plasty for scar length shortening. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2008 Sep:34(9):1236-8. doi: 10.1111/j.1524-4725.2008.34265.x. Epub 2008 Jun 12 [PubMed PMID: 18554292]
Asken S. A modified M-plasty. The Journal of dermatologic surgery and oncology. 1986 Apr:12(4):369-73 [PubMed PMID: 3514717]
Wisco OJ, Wentzell JM. When an M is a V: vector analysis calls for redesign of the M-plasty. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2009 Aug:35(8):1271-6. doi: 10.1111/j.1524-4725.2009.01223.x. Epub 2009 May 15 [PubMed PMID: 19469795]