Introduction
Paroxysmal supraventricular tachycardia (PSVT) manifests as intermittent episodes of regular, sudden-onset, and spontaneously terminating tachycardia.[1] The incidence of this tachyarrhythmia is approximately 2.5 per 1000 in the general population, commonly encountered in emergency departments, and often affects individuals without underlying structural heart disease.[2][3] PSVT is the characteristic feature of atrioventricular nodal reentrant tachycardia (AVNRT), atrioventricular reentrant tachycardia (AVRT), and focal atrial tachycardia. AVNRT is the most common cause of PSVT in adults, followed by AVRT and atrial tachycardia.[1][4] Although patients with PSVT usually exhibit recurring palpitations, at times, PSVT may present with atypical symptoms such as shortness of breath, dizziness, chest pain, and syncope. This is particularly notable in older individuals with existing structural heart conditions.[3] Noncardiac symptoms, such as tinnitus, burping, chilling, sweating, absence-like seizures, panic attacks, and asthma-like attacks, have also been reported in patients with PSVT.[5][6][7]
A 12-lead electrocardiogram (ECG) is the most important initial investigation for patients presenting with PSVT. The common electrocardiographic findings include narrow complex tachycardia with a 1:1 atrioventricular association. However, AVNRT may present with atrioventricular or ventriculoatrial dissociation and atrial tachycardia commonly has a 2:1 atrioventricular conduction.[8][9] Treatment options include adenosine, beta-adrenergic antagonists, calcium channel blockers, vagal maneuvers, and rarely electrical cardioversion.[10] Over the past few decades, catheter ablation has emerged as the most effective and safest treatment option for PSVT and is associated with improved quality of life.[11]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The common forms of PSVT, including AVNRT and AVRT, are characterized by electrophysiologic and anatomic substrates in the form of different pathways. These pathways can be labeled as congenital anomalies, as these are present at the time of birth. However, the pathways may not be responsible for PSVT in every individual.[2] Accessory atrioventricular pathways are strongly associated with some congenital heart diseases, including Ebstein anomaly and transposition of the great arteries.[12] Reentry is the mechanism of arrhythmia in both the AVNRT and AVRT, and the atrial or ventricular extra stimuli trigger it.[13][14] Hence, PSVT can be induced by any physiologic/pathologic condition that triggers atrial or ventricular premature beats.[15] The commonly identified triggers may include physical activity, stress, caffeinated beverages, nicotine, hyperthyroidism, myocardial ischemia, infection, hypoxia, and hypovolemia.
Atrial tachycardia, a rare form of PSVT, is usually found in patients with structural heart diseases. However, focal atrial tachycardia can be found in young, healthy individuals without structural heart diseases and cardiomyopathies. This rare form of PSVT is commonly associated with congenital heart diseases, acquired valvular heart diseases, atrial cardiomyopathy, left ventricular systolic dysfunction, rheumatic heart diseases, intracardiac shunts, and cardiac surgical scars.[16] Atrial tachycardia is also reported in patients with rheumatoid arthritis and systemic lupus erythematosus, even in the absence of underlying structural heart diseases.[17]
Epidemiology
PSVT is the second most common tachyarrhythmia following atrial fibrillation. In the United States, the prevalence of PSVT is approximately 0.2%, and it has an incidence of 1 to 3 cases every 1000 patients.[2] In a population-based study, the overall risk of developing PSVT was found to be double in women compared to men, and the prevalence of PSVT was found to increase with age. AVNRT is found more commonly in patients who are middle-aged or older. PSVT with an accessory pathway is most common in adolescents, and its occurrence decreases with age.[2][18][19] Besides occurring in healthy individuals, PSVT can also occur after myocardial infarction, rheumatic heart disease, mitral valve prolapse, pneumonia, chronic lung disease, and pericarditis. Digoxin toxicity is often associated with PSVT.
AVNRT and atrioventricular reciprocating tachycardia account for over 90% of PSVT. More than 60% of the patients with PSVT are found to have AVNRT, and it is more commonly found in females compared to males.[20] Patients with AVNRT usually present during the second and third decades of life. However, some patients may not experience symptoms until their sixth or seventh decades of life.[21] AVRT is the second most common cause of PSVT and is found in up to 1% of the general population. Patients with AVRT commonly present at a young age, with a mean age for diagnosis of 34 in males and 21 in females.[22] The incidence of AVRT is higher in adolescence and gradually decreases with advancing age. Atrial tachycardia is a relatively rare form of PSVT, and its prevalence varies from 0.3% to 0.46%. The prevalence of atrial tachycardia is higher in symptomatic individuals with PSVT and those with underlying structural heart diseases.[23] Studies suggest that 5% to 10% of the patients undergoing electrophysiology study for PSVT are found to have atrial tachycardia.[24]
Pathophysiology
PSVT is often due to different reentry circuits in the heart, where less frequent causes include enhanced or abnormal automaticity and triggered activity. Reentry circuits include a pathway within and around the sinus node, within the atrial myocardium, within the atrioventricular node, or an accessory pathway involving the atrioventricular node.[25][26][27]
AVNRT: An extensive study of AVNRT suggests dual atrioventricular nodal physiology as the fundamental principle of the reentry circuit involving the atrioventricular node and surrounding atrial myocardium. The reentry circuit in AVNRT is formed by an antegrade and a retrograde limb (known as atrioventricular nodal pathways); both limbs have different conduction properties and refractory periods.[28] The atrioventricular nodal pathways are composed of atrio-nodal tissues, and their conduction properties differ from the compact atrioventricular node. So far, a fast atrioventricular nodal pathway and multiple slow pathways have been identified, and different combinations of these pathways result in different forms of AVNRT.[13] The most common form of AVNRT involves the slow atrioventricular nodal pathway as an antegrade and the fast pathway as a retrograde limb of the tachycardia circuit. This slow-fast AVNRT is commonly known as typical AVNRT. The other (atypical) forms of AVNRT may include a fast-slow and a slow-slow AVNRT.[29] A premature atrial complex commonly induces AVNRT. However, a premature ventricular complex may start AVNRT in rare cases.
AVRT: AVRT is a macroreentrant tachycardia that commonly involves the atrium and ventricle as part of the tachycardia circuit, in addition to the atrioventricular node and an accessory pathway.[30] Orthodromic AVRT is the most common form of AVRT. It is characterized by a reentry circuit that uses an atrioventricular node and the His-Purkinje conduction system as the antegrade limb and the accessory pathway as the retrograde limb. On the other hand, antidromic AVRT is characterized by antegrade conduction via the accessory pathway and retrograde conduction over the His-Purkinje system and atrioventricular node.[14] Usually, the accessory pathway directly connects the atrium to the ventricle, known as an atrioventricular accessory pathway. Rare forms of the accessory pathway include the atriofascicular pathway, nodofascicular pathway, nodoventricular pathway, and fasciculoventricular pathway.[31] AVRT can be induced with atrial and ventricular premature complexes.
Atrial Tachycardia: Although atrial tachycardia is a broad term that includes all supraventricular tachyarrhythmias originating from the atrium and does not require the atrioventricular node for maintenance of tachycardia, focal atrial tachycardia is the most common atrial tachycardia in patients presenting with PSVT. The mechanism of focal atrial tachycardia may include automaticity, triggered activity, or a micro reentry.[16] It is difficult to determine the actual mechanism of focal atrial tachycardia on a surface ECG; however, the initiation and termination of tachycardia may differentiate the automatic focal atrial tachycardia from micro reentry. Focal atrial tachycardia is usually found in patients with structurally normal hearts and commonly arises from crista terminalis, annulus of atrioventricular valves, interatrial septum, pulmonary veins, and coronary sinus ostium. Microreentrant atrial tachycardia is usually found in patients with diseased atria and cardiomyopathies.[32]
History and Physical
The severity of symptoms in patients with PSVT depends on any underlying structural heart disease, the frequency of PSVT episodes, and the patient's hemodynamic reserve. Usually, patients with PSVT present with symptoms of palpitations, neck fullness, anxiety, and fatigue. Other symptoms may include dizziness, syncope, nausea, shortness of breath, pain or discomfort in the chest, anxiety, fatigue, diaphoresis, and polyuria secondary to the atrial natriuretic factor secreted mainly by the heart's atria in response to atrial stretch.[3] Dizziness and palpitations are the most common symptoms. Patients with PSVT and a known history of coronary artery disease may present with a myocardial infarction secondary to the stress on the heart. Patients with PSVT and a known history of heart failure may present with acute decompensated heart failure. Frequent PSVTs, especially atrial tachycardia, can result in new-onset heart failure secondary to tachycardia-induced cardiomyopathy.[33]
A detailed history of patients with PSVT should include their medical and cardiac history, time of symptom onset, prior episodes, and treatments received. The patient's current medication list must be obtained. Patients' engagement in physical activities such as exercise or outdoor sports should be part of the history intake. Patients with symptomatic PSVT tend to avoid engaging in such hobbies, so this history is relevant. Patients presenting with PSVTs should receive a thorough physical examination, including vital signs (respiratory rate, blood pressure, temperature, and heart rate), to assess their hemodynamic stability.[34] Although the clinical examination is usually unremarkable in patients with PSVT, it helps exclude underlying structural heart diseases and valvular lesions. During the episode of PSVT, patients usually have tachycardia, distended neck veins, and may experience a loud first heart sound, whereas patients with cardiomyopathy may have S3 and other signs of decompensated heart failure.[35]
Evaluation
PSVT is commonly diagnosed in the emergency department. Hemodynamic assessment should focus on the initial evaluation of a patient presenting with symptoms suggestive of PSVT. After establishing the hemodynamic stability and performing a detailed physical examination, a 12-lead ECG should be the initial diagnostic test. Comparing a 12-lead ECG during tachycardia with an ECG during sinus rhythm (if available) is essential. An ECG during tachycardia helps understand the PSVT mechanism in most patients. However, on many occasions, ECG may not differentiate atypical AVNRT from atrial tachycardia and orthodromic AVRT.[36]
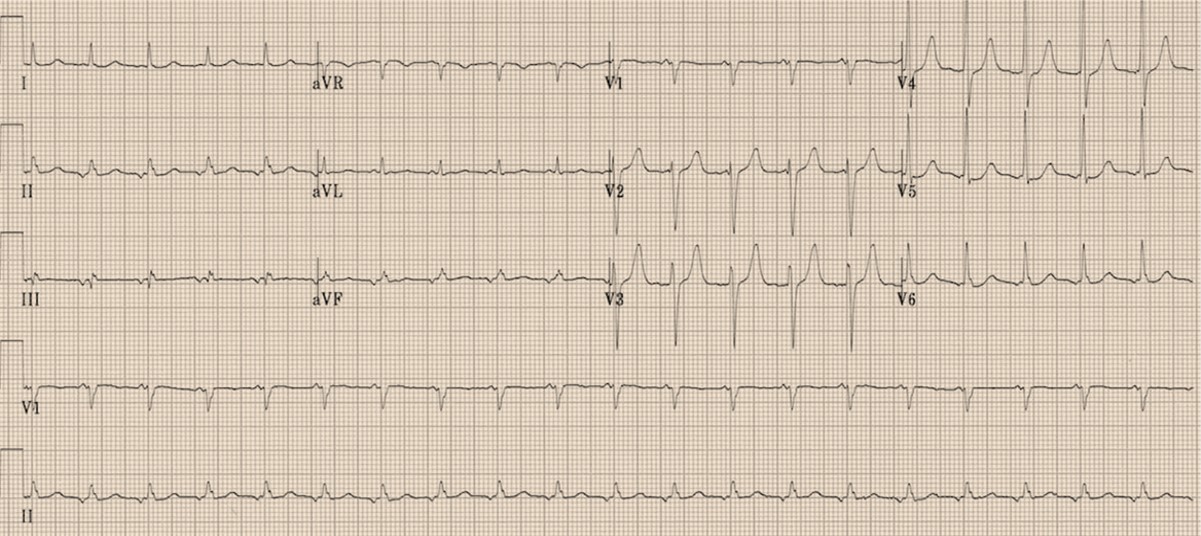
Essential components of ECG interpretation during PSVT include the rate of tachycardia, P-wave morphology, the correlation between the P wave and the QRS complex, and QRS morphology. The characteristic feature of PSVT is a narrow QRS complex; however, it may present with a wide QRS complex due to an underlying bundle branch block, rate-related aberrancy, or preexcitation caused by a bystander pathway (see Image. Narrow Complex Tachycardia With Incomplete Right Bundle Branch).[37]
As part of the initial evaluation in a selected group of patients presenting with symptomatic PSVTs, additional tests may be considered, including renal function, electrolytes, and thyroid function testing. A transthoracic echocardiogram is required to evaluate left ventricular systolic function and exclude structural heart diseases.[38][39]
Electrocardiogram Features of Paroxysmal Supraventricular Tachycardia
Essential components of ECG interpretation during PSVT include the rate of tachycardia, P-wave morphology, the correlation between the P wave and the QRS complex, and QRS morphology. A narrow QRS complex is the characteristic feature of PSVT; however, it may present with a wide QRS complex due to an underlying bundle branch block, rate-related aberrancy, or preexcitation caused by an accessory pathway.[37] The relation between PR and RP intervals is a useful electrocardiographic feature to differentiate PSVT in the emergency department. However, it is limited by the fast rate of tachycardia, the absence of a 1:1 atrioventricular association, and the absence of identifiable P waves. When the RP interval is shorter compared to the PR interval, the tachycardia is labeled as a short RP tachycardia, and typical AVNRT is the most common differential of short RP tachycardia followed by orthodromic AVRT.
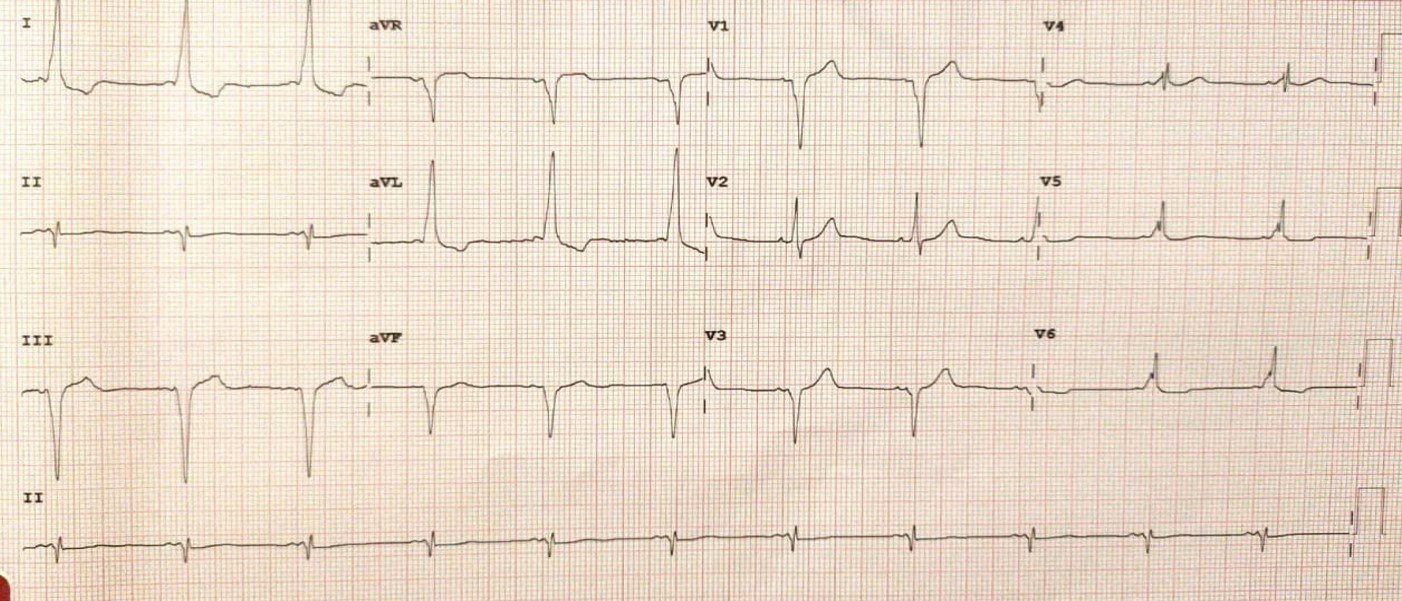
Rarely, atrial tachycardia with a gross first-degree atrioventricular block or a conduction delay in the atrium may present as short RP tachycardia.[40][41] When the RP interval is longer compared to the PR interval, it excludes typical AVNRT, and the common differentials include atrial tachycardia, atypical AVNRT, and orthodromic AVRT with a decremental accessory pathway (see Image. Narrow Complex Tachycardia with Prolonged RP Interval).
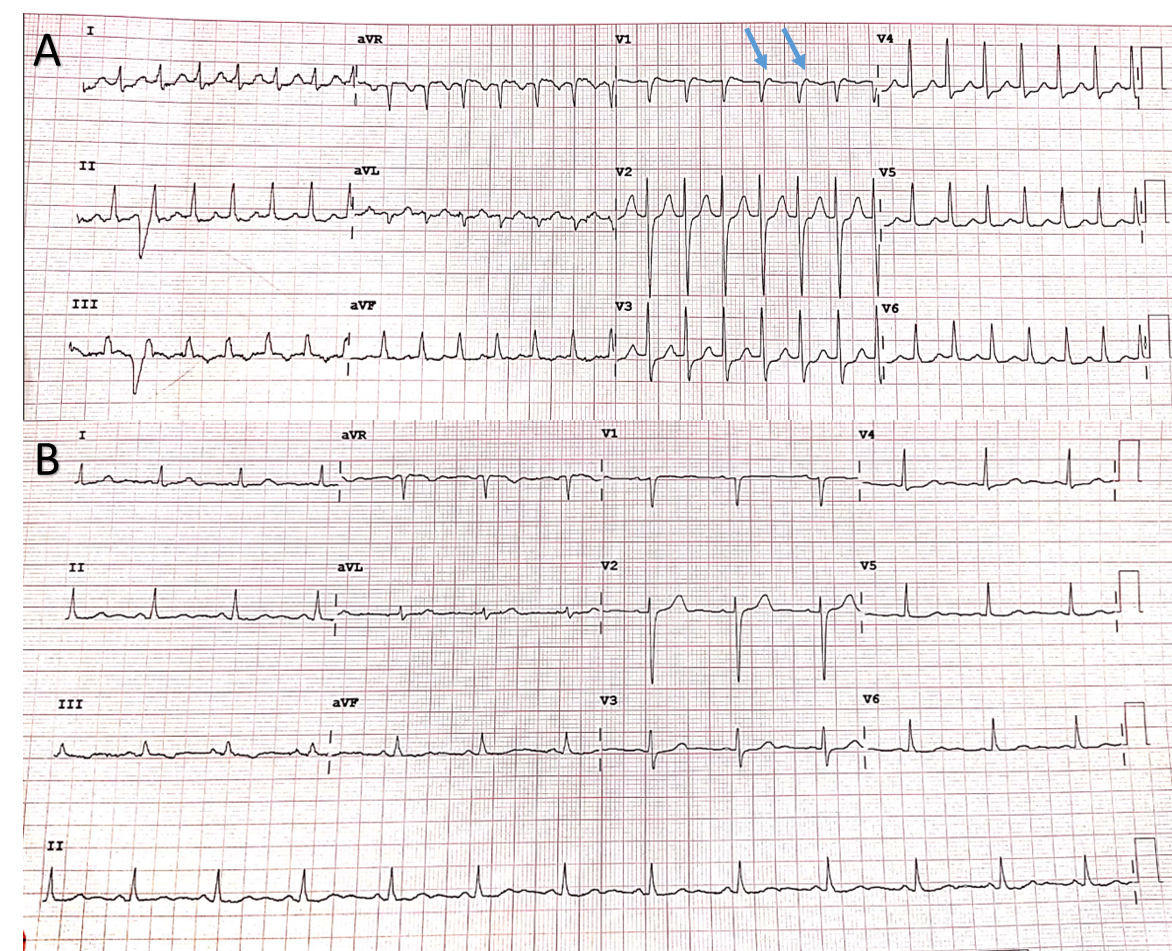
The characteristic ECG features of typical AVNRT include a narrow complex tachycardia with a short RP interval, and the retrograde P waves are usually buried in the QRS complex due to simultaneous activation of the atria and ventricles.[15][42] Characteristically, the retrograde P waves are found in the terminal part of the QRS complex, creating the appearance of a "pseudo" R wave in lead V1 and a "pseudo" S wave in the inferior leads when compared to the ECG in sinus rhythm (see Image. Narrow Complex Tachycardia versus Sinus Rhythm: Pseudo R Waves). Atypical forms of AVNRT are characterized by distinct retrograde P waves (inverted in inferior leads), with an RP interval usually longer than the PR interval. In rare cases, AVNRT may present with ventriculoatrial dissociation, and retrograde P waves are not found with each QRS complex.[29]
AVRT is a macroreentrant tachycardia, categorized into orthodromic and antidromic AVRT. Orthodromic AVRT is the most common form of AVRT and is characterized by antegrade conduction over the His-Purkinje conduction system and retrograde conduction over the accessory pathway. During orthodromic AVRT, the ECG shows a 1:1 ventriculoatrial association, featuring distinct retrograde P waves. The RP interval is longer than a typical AVNRT due to sequential activation of the ventricle and atrium.[43] During sinus rhythm, the ECG may show a short PR interval with a characteristic delta wave due to preexcitation (see Image. Sinus Rhythm with Short PR Interval and Delta Wave). However, an absence of preexcitation does not rule out orthodromic AVRT.[44] Antidromic AVRT is a rare form of pathway-mediated PSVT. Its ECG features include wide complex tachycardia due to a fully preexcited QRS complex that does not meet the criteria of a typical bundle branch block. The P waves are usually not visible; however, if P waves are visible, these have a 1:1 association with the QRS complex. Atrioventricular dissociation rules out AVRT, as the atrium and ventricle are obligatory parts of the tachycardia circuit in atrioventricular accessory pathway-mediated tachycardias.[45]
The ECG features of focal atrial tachycardia include a distinct P wave with a long RP interval. The origin of tachycardia determines the P-wave morphology; usually, it is different from the sinus P waves. Atrial tachycardia may present with a 2:1 atrioventricular association; in rare cases, it may present with atrioventricular Wenckebach. The above-discussed electrocardiographic features accurately differentiate PSVT in >80% of the patients; however, 20% of the patients with PSVT require an electrophysiology study to diagnose and determine the mechanism of tachycardia accurately.[46]
Electrophysiology Study For Paroxysmal Supraventricular Tachycardia
An electrophysiology study is recommended for all patients experiencing symptomatic, documented PSVT to determine the mechanism of tachycardia and strategize the ablation procedure. An invasive electrophysiology study helps localize the arrhythmia and provides definitive treatment when followed by catheter ablation.[1] The clinical SVT is induced during the electrophysiology study, and different diagnostic maneuvers are performed to define the tachycardia circuit, especially in AVNRT and pathway-mediated PSVT. Each type of PSVT has characteristic electrophysiology findings, and these arrhythmias respond to diagnostic maneuvers in a characteristic way.[47]
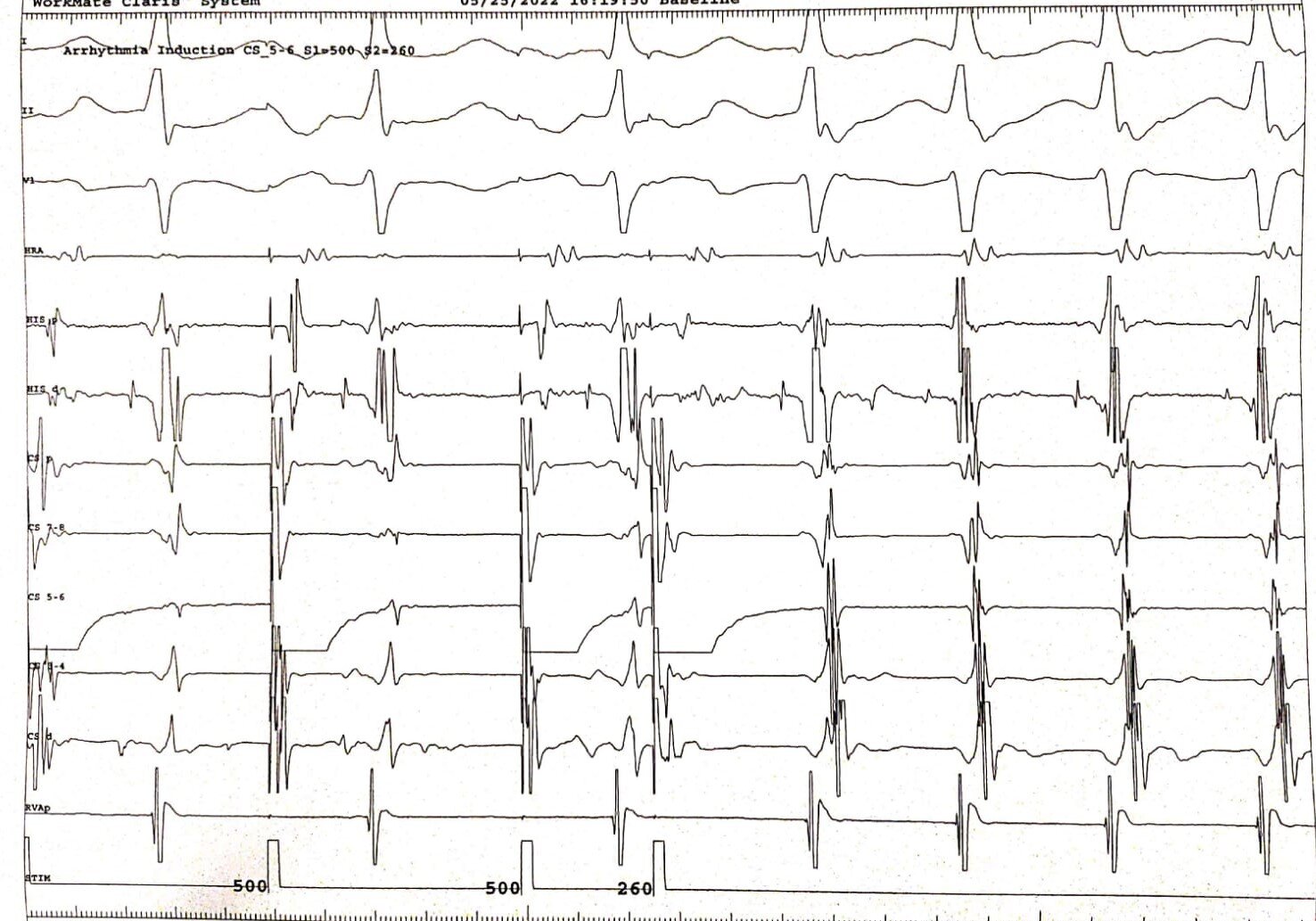
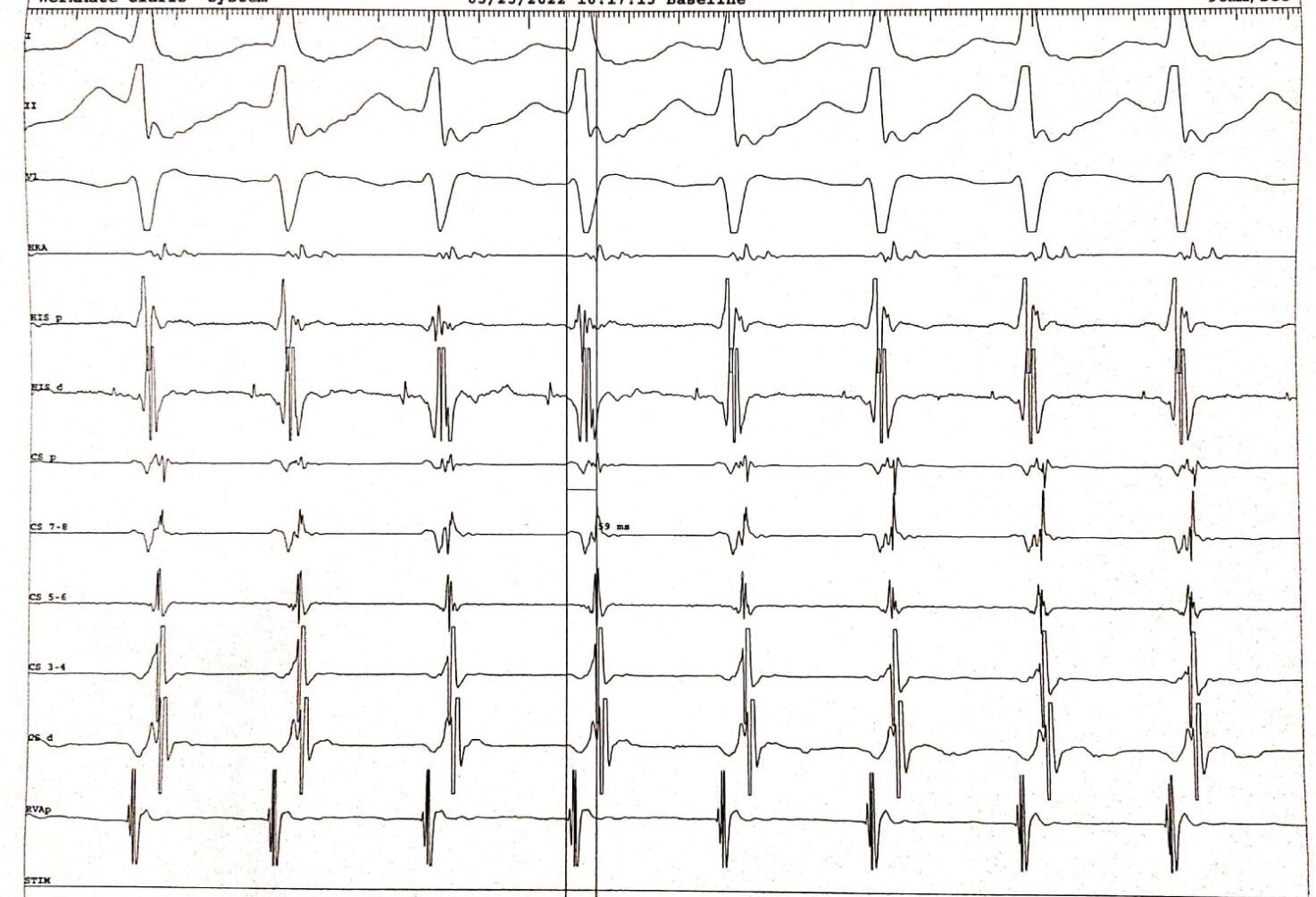
The characteristic electrophysiology features of typical AVNRT include reproducible initiation of tachycardia with an A-H jump and echo beat (see Image. Typical AVNRT Induction with Atrial Extra Stimulus) and a ventriculoatrial interval of <70 ms during tachycardia due to simultaneous activation of the atrium and ventricles (see Image. Narrow Complex Tachycardia: Short Ventriculoatrial Interval). The other feature may include concentric atrial activation, a V-A-V response after right ventricular overdrive pacing with a long post-pacing interval (PPI).[29]
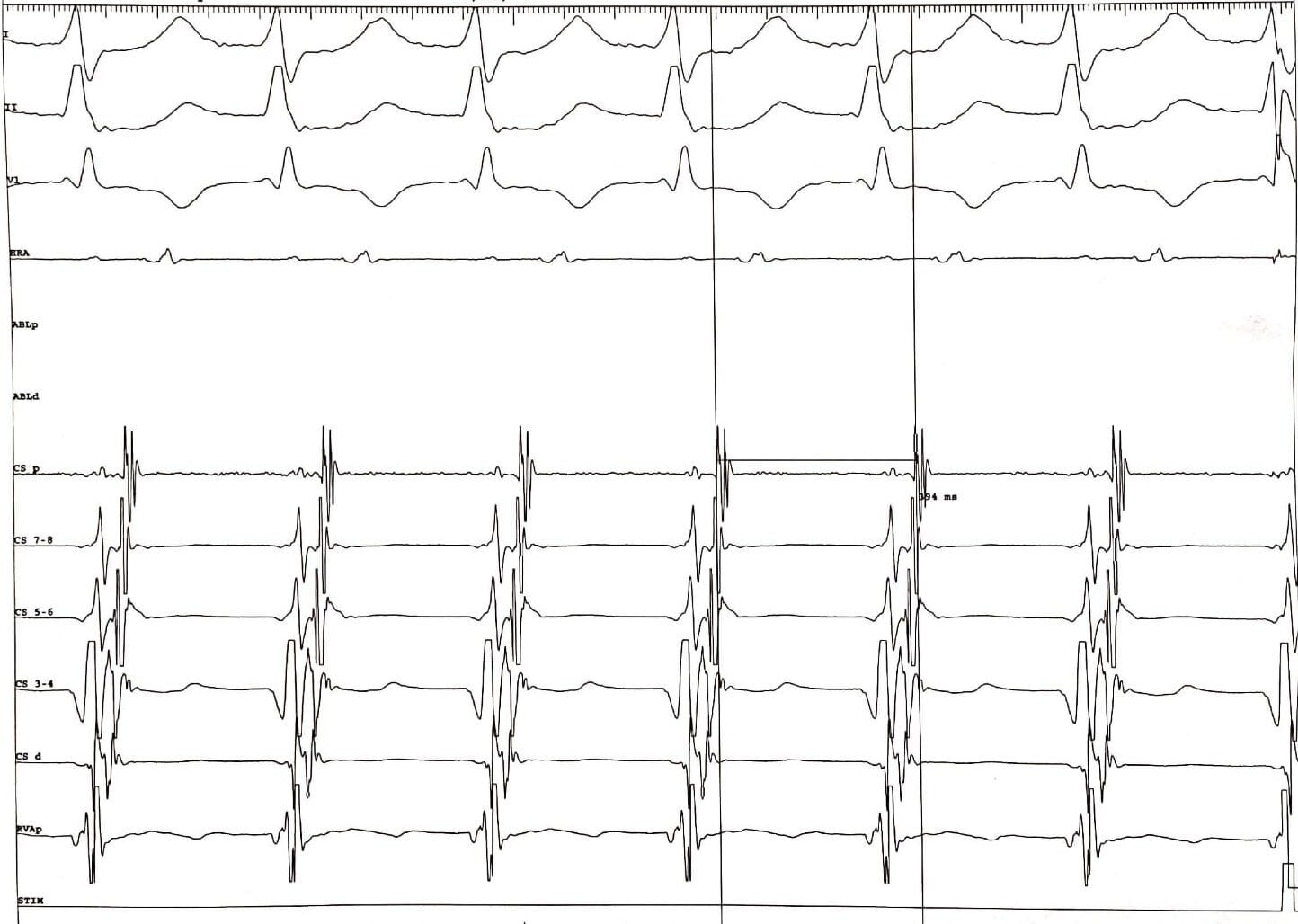
The orthodromic AVRT is characterized by a ventriculoatrial interval longer than 70 ms, and the earliest atrial activation is noted near the atrial end of the accessory pathway (see Image. Orthodromic AVRT: Long Ventriculoatrial Interval). A His-synchronous ventricular extra stimulus can delay the next atrial activation or terminate the tachycardia without capturing the atrium. The right ventricular overdrive pacing results in a V-A-V response with a relatively short PPI (except in the left lateral pathway, where the tachycardia circuit does not involve the right ventricular apex).[48] The characteristic electrophysiologic features of atrial tachycardia may include the continuation of tachycardia following an atrioventricular block and a V-A-A-V response upon cessation of right ventricular overdrive pacing.[49]
Treatment / Management
Initial Management
In the case of most symptomatic patients with PSVT, the emergency department is the primary point of contact in the hospital, so the emergency medicine team carries out the initial management. The initial treatment of PSVT in a patient depends on the type of rhythm present on the ECG and the hemodynamic stability of the patient. Patients presenting with hypotension, shortness of breath, chest pain, shock, or altered mental status are considered hemodynamically unstable, and they should undergo an urgent electric cardioversion.[50] If, on the initial evaluation, a patient with PSVT is found to be hemodynamically stable, vagal maneuvers are recommended as the first treatment choice. The commonly performed vagal maneuvers include carotid sinus massage and Valsalva maneuvers.[51] Overall, the success rate of vagal maneuvers is <30%, and carotid sinus massage is contraindicated in the presence of carotid bruit.(B2)
If the vagal maneuvers are ineffective or can not be performed, adenosine is the drug of choice for the initial management of PSVT. The non-randomized trials have proven that adenosine successfully terminates atrioventricular node–dependent PSVTs (AVNRT and AVRT) in 75% to 95% of the patients. Adenosine should be administered as a bolus via a large-bore intravenous cannula placed in one of the proximal veins. The recommended initial dose is 6 mg, followed by an intravenous flush. If tachycardia persists, a higher dose can be repeated after 2 min.[52] The common side effects of adenosine include bronchospasm resulting in shortness of breath and chest discomfort, flushing, and a transient atrioventricular block. However, these effects are short-lived due to the very short half-life of adenosine.[53] Intravenous beta blockers and non-dihydropyridine calcium channel blockers are recommended as an alternative option if adenosine is ineffective or can not be administered. Electrical cardioversion can be considered in hemodynamically stable patients if vagal maneuvers and intravenous drug therapy fail to terminate the tachycardia and the patients are symptomatic.[1][54](A1)
Ongoing Management
Ongoing and long-term care is an essential component of PSVT management, especially in patients with recurrent symptoms resulting in frequent hospital visits. Over the last few decades, catheter ablation has revolutionized the treatment of PSVT. It has an excellent success rate in AVNRT and AVRT with relatively low complications.[55] Catheter ablation is performed by targeting the critical component of the tachycardia circuit. In AVNRT, the slow pathway is targeted, whereas AVRT is treated by ablating the accessory pathway.(B3)
Contemporary guidelines recommend an electrophysiology study and ablation as the first line of treatment in symptomatic PSVT.[56] Catheter ablation can be considered even in asymptomatic patients in the presence of manifest preexcitation with a short refractory period of the accessory pathway. It is strongly recommended for patients with high-risk professions.[57] Catheter ablation significantly reduces the cost of recurrent hospitalization, improves the quality of life, and cures AVNRT and AVRT in >95% of symptomatic patients.[58](A1)
However, if ablation is not feasible, medical therapy can be used for the long-term management of PSVT. Commonly recommended drugs include oral beta blockers and non-dihydropyridine calcium channel blockers, whereas amiodarone, flecainide, digoxin, and sotalol can be used in select groups of patients.[56] Selective atrioventricular node–blocking drugs should not be prescribed in patients with manifest preexcitation and symptomatic PSVT; these drugs promote the rapid conduction of atrial fibrillation through the accessory pathway and may increase the risk of ventricular fibrillation.[59] All patients with symptomatic PSVT should receive clear instructions on performing vagal maneuvers. When the tachycardia episodes last longer, vagal maneuvers become relatively less effective due to a strong sympathetic response. Hence, the patients should be advised to initiate vagal maneuvers when SVT begins.(A1)
Differential Diagnosis
The differential diagnosis for PSVT includes AVNRT, AVRT, focal atrial tachycardia, multifocal atrial tachycardia, atrial flutter, atrial fibrillation, inappropriate sinus tachycardia, sinoatrial node reentrant tachycardia, junctional ectopic tachycardia, and nonparoxysmal junctional tachycardia.[60][46]
Prognosis
In the absence of structural heart disease, the prognosis for PSVT is reasonably good, and most patients have longevity comparable to the general population. In patients with structural heart disease, the prognosis is determined by the underlying structural heart diseases. PSVT can occur suddenly, lasting from a few seconds to several days. Most patients develop anxiety and a sense of doom, and others may develop a hemodynamic compromise. A lot of patients with recurrent symptoms may report an impaired quality of life due to frequent visits to the emergency department.[61] Symptomatic patients with Wolff-Parkinson-White (WPW) syndrome are estimated to have an annual risk of sudden cardiac death (SCD) ranging from 0.1% to 0.3%.[62] The older studies suggest a lifetime risk of SCD ranging from 3% to 4% in patients with symptomatic WPW syndrome. The predictors of SCD may include a short refractory period with the accessory pathway, multiple pathways, inducible AVRT, male gender, and a history of syncope.[63]
Complications
Younger patients who do not have structural heart diseases tolerate PSVT very well. However, patients with underlying structural heart diseases may develop syncope or signs and symptoms of heart failure, resulting in recurrent hospitalization. Tachycardia-induced cardiomyopathy has also been reported in patients with incessant PSVT.[64] A very fast heart rate during PSVT can lead to myocardial ischemia in elderly patients and those with coronary artery diseases. Rarely, incessant PSVT may degenerate into life-threatening ventricular arrhythmias.[65]
Deterrence and Patient Education
Educating patients about the common symptoms and complications of PSVT and establishing closed-loop communication between patients and their healthcare providers can further improve the management of these rhythms. Patient education should be provided through online literature, videos, and pamphlets, if available. The risk of SCD associated with WPW syndrome should be explained to the patients, and catheter ablation should be recommended as the primary treatment option.
Enhancing Healthcare Team Outcomes
Good teamwork and effective interprofessional communication are key factors in improving the outcomes of patients with PSVT. Although emergency medical technicians are often the first to encounter patients and provide treatment for PVST, interprofessional team members involved in treating PSVT include emergency department physicians and nurses, cardiologists with expertise in rhythm management, cardiology nurses, primary care providers, and pharmacists. In addition to treating PVST, team members can provide education on medication side effects and compliance, and check for drug interactions.
Media
(Click Image to Enlarge)
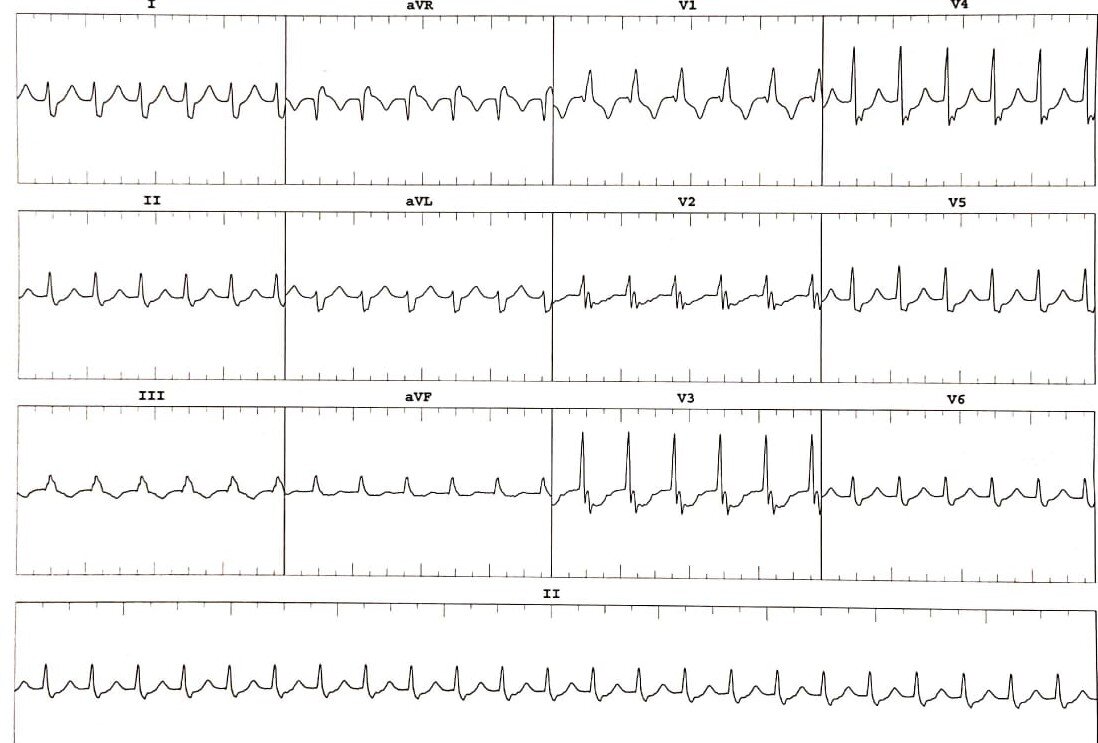
Narrow Complex Tachycardia With Incomplete Right Bundle Branch. A 12-lead ECG shows a narrow complex tachycardia (with incomplete right bundle branch). The P waves are not distinctly visible. However, a negative deflection at the end of the QRS complex in lead II could be a retrograde P wave, creating the impression of "pseudo S" wave.
Contributed by Intisar Ahmed
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Page RL, Joglar JA, Caldwell MA, Calkins H, Conti JB, Deal BJ, Estes NA III, Field ME, Goldberger ZD, Hammill SC, Indik JH, Lindsay BD, Olshansky B, Russo AM, Shen WK, Tracy CM, Al-Khatib SM. 2015 ACC/AHA/HRS guideline for the management of adult patients with supraventricular tachycardia: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Heart rhythm. 2016 Apr:13(4):e136-221. doi: 10.1016/j.hrthm.2015.09.019. Epub 2015 Sep 25 [PubMed PMID: 26409100]
Level 1 (high-level) evidenceOrejarena LA, Vidaillet H Jr, DeStefano F, Nordstrom DL, Vierkant RA, Smith PN, Hayes JJ. Paroxysmal supraventricular tachycardia in the general population. Journal of the American College of Cardiology. 1998 Jan:31(1):150-7 [PubMed PMID: 9426034]
Yetkin E, Ozturk S, Cuglan B, Turhan H. Clinical presentation of paroxysmal supraventricular tachycardia: evaluation of usual and unusual symptoms. Cardiovascular endocrinology & metabolism. 2020 Dec:9(4):153-158. doi: 10.1097/XCE.0000000000000208. Epub 2020 May 15 [PubMed PMID: 33225230]
Kadish A, Passman R. Mechanisms and management of paroxysmal supraventricular tachycardia. Cardiology in review. 1999 Sep-Oct:7(5):254-64 [PubMed PMID: 11208235]
Ozturk S, Turhan H, Yetkin E. Asthma-like attacks terminated by slow pathway ablation. Annals of thoracic medicine. 2017 Apr-Jun:12(2):127-128. doi: 10.4103/1817-1737.203739. Epub [PubMed PMID: 28469725]
Yetkin E, Kaleagzi FC. Recovery of absence seizure-like symptoms in a patient after slow pathway radiofrequency ablation. International journal of cardiology. 2015 Mar 1:182():44-5. doi: 10.1016/j.ijcard.2014.12.111. Epub 2014 Dec 27 [PubMed PMID: 25576718]
Level 3 (low-level) evidenceYetkin G, Ozturk S, Yetkin E. Chilling-Like Attacks Terminated by Slow Pathway Ablation. Current cardiology reviews. 2020:16(4):338-340. doi: 10.2174/1573403X15666191212100050. Epub [PubMed PMID: 31830887]
Kara M, Korkmaz A, Ozeke O, Cay S, Ozcan F, Topaloglu S, Aras D. Manifest 1:2 tachycardia or atrioventricular nodal reentrant tachycardia with complete ventriculoatrial dissociation. Journal of cardiovascular electrophysiology. 2020 Jun:31(6):1563-1564. doi: 10.1111/jce.14465. Epub 2020 Apr 7 [PubMed PMID: 32255532]
Buttà C, Tuttolomondo A, Giarrusso L, Pinto A. Electrocardiographic diagnosis of atrial tachycardia: classification, P-wave morphology, and differential diagnosis with other supraventricular tachycardias. Annals of noninvasive electrocardiology : the official journal of the International Society for Holter and Noninvasive Electrocardiology, Inc. 2015 Jul:20(4):314-27. doi: 10.1111/anec.12246. Epub 2014 Dec 22 [PubMed PMID: 25530184]
Level 3 (low-level) evidenceAhmad F, Abu Sneineh M, Patel RS, Rohit Reddy S, Llukmani A, Hashim A, Haddad DR, Gordon DK. In The Line of Treatment: A Systematic Review of Paroxysmal Supraventricular Tachycardia. Cureus. 2021 Jun:13(6):e15502. doi: 10.7759/cureus.15502. Epub 2021 Jun 7 [PubMed PMID: 34268033]
Level 1 (high-level) evidenceBrachmann J, Lewalter T, Kuck KH, Andresen D, Willems S, Spitzer SG, Straube F, Schumacher B, Eckardt L, Danilovic D, Thomas D, Hochadel M, Senges J. Long-term symptom improvement and patient satisfaction following catheter ablation of supraventricular tachycardia: insights from the German ablation registry. European heart journal. 2017 May 1:38(17):1317-1326. doi: 10.1093/eurheartj/ehx101. Epub [PubMed PMID: 28329395]
Doevendans PA, Wellens HJ. Wolff-Parkinson-white syndrome: a genetic disease? Circulation. 2001 Dec 18:104(25):3014-6 [PubMed PMID: 11748090]
Wu J, Wu J, Olgin J, Miller JM, Zipes DP. Mechanisms underlying the reentrant circuit of atrioventricular nodal reentrant tachycardia in isolated canine atrioventricular nodal preparation using optical mapping. Circulation research. 2001 Jun 8:88(11):1189-95 [PubMed PMID: 11397786]
Level 3 (low-level) evidenceJabbour F,Grossman SA, Atrioventricular Reciprocating Tachycardia. StatPearls. 2022 Jan [PubMed PMID: 30969587]
Katritsis DG, Camm AJ. Atrioventricular nodal reentrant tachycardia. Circulation. 2010 Aug 24:122(8):831-40. doi: 10.1161/CIRCULATIONAHA.110.936591. Epub [PubMed PMID: 20733110]
Liwanag M, Willoughby C. Atrial Tachycardia. StatPearls. 2024 Jan:(): [PubMed PMID: 31194392]
Subhani F, Ahmed I, Manji AA, Saeed Y. Atrial Tachycardia Associated With a Tachycardia-Induced Cardiomyopathy in a Patient With Systemic Lupus Erythematosus. Cureus. 2020 Nov 22:12(11):e11626. doi: 10.7759/cureus.11626. Epub 2020 Nov 22 [PubMed PMID: 33376640]
Porter MJ, Morton JB, Denman R, Lin AC, Tierney S, Santucci PA, Cai JJ, Madsen N, Wilber DJ. Influence of age and gender on the mechanism of supraventricular tachycardia. Heart rhythm. 2004 Oct:1(4):393-6 [PubMed PMID: 15851189]
Tada H, Oral H, Greenstein R, Pelosi F Jr, Knight BP, Strickberger SA, Morady F. Analysis of age of onset of accessory pathway-mediated tachycardia in men and women. The American journal of cardiology. 2002 Feb 15:89(4):470-1 [PubMed PMID: 11835934]
Liuba I, Jönsson A, Säfström K, Walfridsson H. Gender-related differences in patients with atrioventricular nodal reentry tachycardia. The American journal of cardiology. 2006 Feb 1:97(3):384-8 [PubMed PMID: 16442401]
Kanjwal K, Kanjwal S, Ruzieh M. Atrioventricular Nodal Reentrant Tachycardia in Very Elderly Patients: A Single-center Experience. The Journal of innovations in cardiac rhythm management. 2020 Feb:11(2):3990-3995. doi: 10.19102/icrm.2020.110202. Epub 2020 Feb 15 [PubMed PMID: 32368371]
Fitzsimmons PJ, McWhirter PD, Peterson DW, Kruyer WB. The natural history of Wolff-Parkinson-White syndrome in 228 military aviators: a long-term follow-up of 22 years. American heart journal. 2001 Sep:142(3):530-6 [PubMed PMID: 11526369]
Level 2 (mid-level) evidencePoutiainen AM, Koistinen MJ, Airaksinen KE, Hartikainen EK, Kettunen RV, Karjalainen JE, Huikuri HV. Prevalence and natural course of ectopic atrial tachycardia. European heart journal. 1999 May:20(9):694-700 [PubMed PMID: 10208790]
Level 2 (mid-level) evidenceSteinbeck G, Hoffmann E. 'True' atrial tachycardia. European heart journal. 1998 May:19 Suppl E():E10-2, E48-9 [PubMed PMID: 9717019]
Xie B, Thakur RK, Shah CP, Hoon VK. Clinical differentiation of narrow QRS complex tachycardias. Emergency medicine clinics of North America. 1998 May:16(2):295-330 [PubMed PMID: 9621846]
Krahn AD, Yee R, Klein GJ, Morillo C. Inappropriate sinus tachycardia: evaluation and therapy. Journal of cardiovascular electrophysiology. 1995 Dec:6(12):1124-8 [PubMed PMID: 8720214]
Brugada P, Wellens HJ. The role of triggered activity in clinical ventricular arrhythmias. Pacing and clinical electrophysiology : PACE. 1984 Mar:7(2):260-71 [PubMed PMID: 6200854]
Level 3 (low-level) evidenceTai CT, Chen SA, Chiang CE, Lee SH, Wen ZC, Chiou CW, Ueng KC, Chen YJ, Yu WC, Huang JL, Chang MS. Complex electrophysiological characteristics in atrioventricular nodal reentrant tachycardia with continuous atrioventricular node function curves. Circulation. 1997 Jun 3:95(11):2541-7 [PubMed PMID: 9184584]
Katritsis DG, Josephson ME. Classification, Electrophysiological Features and Therapy of Atrioventricular Nodal Reentrant Tachycardia. Arrhythmia & electrophysiology review. 2016 Aug:5(2):130-5. doi: 10.15420/AER.2016.18.2. Epub [PubMed PMID: 27617092]
Obel OA, Camm AJ. Accessory pathway reciprocating tachycardia. European heart journal. 1998 May:19 Suppl E():E13-24, E50-1 [PubMed PMID: 9717020]
Kulig J, Koplan BA. Cardiology patient page. Wolff-Parkinson-White syndrome and accessory pathways. Circulation. 2010 Oct 12:122(15):e480-3. doi: 10.1161/CIRCULATIONAHA.109.929372. Epub [PubMed PMID: 20937983]
Markowitz SM, Thomas G, Liu CF, Cheung JW, Ip JE, Lerman BB. Atrial Tachycardias and Atypical Atrial Flutters: Mechanisms and Approaches to Ablation. Arrhythmia & electrophysiology review. 2019 May:8(2):131-137. doi: 10.15420/aer.2019.17.2. Epub [PubMed PMID: 31114688]
Link MS. Clinical practice. Evaluation and initial treatment of supraventricular tachycardia. The New England journal of medicine. 2012 Oct 11:367(15):1438-48. doi: 10.1056/NEJMcp1111259. Epub [PubMed PMID: 23050527]
Fox DJ, Tischenko A, Krahn AD, Skanes AC, Gula LJ, Yee RK, Klein GJ. Supraventricular tachycardia: diagnosis and management. Mayo Clinic proceedings. 2008 Dec:83(12):1400-11. doi: 10.1016/S0025-6196(11)60791-X. Epub [PubMed PMID: 19046562]
Ganz LI, Friedman PL. Supraventricular tachycardia. The New England journal of medicine. 1995 Jan 19:332(3):162-73 [PubMed PMID: 7800009]
Bibas L, Levi M, Essebag V. Diagnosis and management of supraventricular tachycardias. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne. 2016 Dec 6:188(17-18):E466-E473. doi: 10.1503/cmaj.160079. Epub 2016 Oct 24 [PubMed PMID: 27777258]
Abedin Z. Differential diagnosis of wide QRS tachycardia: A review. Journal of arrhythmia. 2021 Oct:37(5):1162-1172. doi: 10.1002/joa3.12599. Epub 2021 Aug 9 [PubMed PMID: 34621415]
Josephson ME, Wellens HJ. Electrophysiologic evaluation of supraventricular tachycardia. Cardiology clinics. 1997 Nov:15(4):567-86 [PubMed PMID: 9403161]
Obel OA, Camm AJ. Supraventricular tachycardia. ECG diagnosis and anatomy. European heart journal. 1997 May:18 Suppl C():C2-11 [PubMed PMID: 9152669]
Nasir M, Sturts A, Sturts A. Common Types of Supraventricular Tachycardia: Diagnosis and Management. American family physician. 2023 Jun:107(6):631-641 [PubMed PMID: 37327167]
Ip JE, Thomas G, Cheung JW, Liu CF, Markowitz SM, Lerman BB. Recognition of short RP atrial tachycardia due to intra-atrial conduction delay: utility of a septal AH/HA Ratio {1. Europace : European pacing, arrhythmias, and cardiac electrophysiology : journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology. 2017 Nov 1:19(11):1780. doi: 10.1093/europace/eux105. Epub [PubMed PMID: 28575185]
Katritsis DG, Ellenbogen KA, Becker AE. Atrial activation during atrioventricular nodal reentrant tachycardia: studies on retrograde fast pathway conduction. Heart rhythm. 2006 Sep:3(9):993-1000 [PubMed PMID: 16945788]
Keating L, Morris FP, Brady WJ. Electrocardiographic features of Wolff-Parkinson-White syndrome. Emergency medicine journal : EMJ. 2003 Sep:20(5):491-3 [PubMed PMID: 12954704]
Level 3 (low-level) evidenceCardona-Guarache R, Han FT, Nguyen DT, Chicos AB, Badhwar N, Knight BP, Johnson CJ, Heaven D, Scheinman MM. Ablation of Supraventricular Tachycardias From Concealed Left-Sided Nodoventricular and Nodofascicular Accessory Pathways. Circulation. Arrhythmia and electrophysiology. 2020 May:13(5):e007853. doi: 10.1161/CIRCEP.119.007853. Epub 2020 Apr 14 [PubMed PMID: 32286853]
Bagliani G, De Ponti R, Sciarra L, Zingarini G, Leonelli FM. Accessory Pathway-Mediated Tachycardias: Precision Electrocardiology Through Standard and Advanced Electrocardiogram Recording Techniques. Cardiac electrophysiology clinics. 2020 Dec:12(4):475-493. doi: 10.1016/j.ccep.2020.08.008. Epub 2020 Sep 30 [PubMed PMID: 33161997]
Kalbfleisch SJ, el-Atassi R, Calkins H, Langberg JJ, Morady F. Differentiation of paroxysmal narrow QRS complex tachycardias using the 12-lead electrocardiogram. Journal of the American College of Cardiology. 1993 Jan:21(1):85-9 [PubMed PMID: 8417081]
Steven D, Bonnemeier H, Deneke T, Estner HL, Kriatselis C, Kuniss M, Luik A, Neuberger HR, Shin DI, Sommer P, Tilz RR, Thomas D, von Bary C, Voss F, Eckardt L. [How to approach the patient with supraventricular tachycardia in the EP lab: A systematic overview]. Herzschrittmachertherapie & Elektrophysiologie. 2015 Jun:26(2):167-72. doi: 10.1007/s00399-015-0373-7. Epub 2015 Jun 2 [PubMed PMID: 26031513]
Level 1 (high-level) evidenceKnight BP, Ebinger M, Oral H, Kim MH, Sticherling C, Pelosi F, Michaud GF, Strickberger SA, Morady F. Diagnostic value of tachycardia features and pacing maneuvers during paroxysmal supraventricular tachycardia. Journal of the American College of Cardiology. 2000 Aug:36(2):574-82 [PubMed PMID: 10933374]
Veenhuyzen GD, Quinn FR, Wilton SB, Clegg R, Mitchell LB. Diagnostic pacing maneuvers for supraventricular tachycardia: part 1. Pacing and clinical electrophysiology : PACE. 2011 Jun:34(6):767-82. doi: 10.1111/j.1540-8159.2011.03076.x. Epub 2011 Mar 25 [PubMed PMID: 21438892]
Neumar RW, Otto CW, Link MS, Kronick SL, Shuster M, Callaway CW, Kudenchuk PJ, Ornato JP, McNally B, Silvers SM, Passman RS, White RD, Hess EP, Tang W, Davis D, Sinz E, Morrison LJ. Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010 Nov 2:122(18 Suppl 3):S729-67. doi: 10.1161/CIRCULATIONAHA.110.970988. Epub [PubMed PMID: 20956224]
DiMarco JP, Miles W, Akhtar M, Milstein S, Sharma AD, Platia E, McGovern B, Scheinman MM, Govier WC. Adenosine for paroxysmal supraventricular tachycardia: dose ranging and comparison with verapamil. Assessment in placebo-controlled, multicenter trials. The Adenosine for PSVT Study Group. Annals of internal medicine. 1990 Jul 15:113(2):104-10 [PubMed PMID: 2193560]
Level 2 (mid-level) evidenceMadsen CD, Pointer JE, Lynch TG. A comparison of adenosine and verapamil for the treatment of supraventricular tachycardia in the prehospital setting. Annals of emergency medicine. 1995 May:25(5):649-55 [PubMed PMID: 7741343]
Level 2 (mid-level) evidenceSingh S, McKintosh R. Adenosine. StatPearls. 2024 Jan:(): [PubMed PMID: 30085591]
Stec S, Kryński T, Kułakowski P. Efficacy of low energy rectilinear biphasic cardioversion for regular atrial tachyarrhythmias. Cardiology journal. 2011:18(1):33-8 [PubMed PMID: 21305483]
Level 1 (high-level) evidenceNakagawa H, Jackman WM. Catheter ablation of paroxysmal supraventricular tachycardia. Circulation. 2007 Nov 20:116(21):2465-78 [PubMed PMID: 18025404]
Level 3 (low-level) evidencePage RL, Joglar JA, Caldwell MA, Calkins H, Conti JB, Deal BJ, Estes NAM 3rd, Field ME, Goldberger ZD, Hammill SC, Indik JH, Lindsay BD, Olshansky B, Russo AM, Shen WK, Tracy CM, Al-Khatib SM. 2015 ACC/AHA/HRS Guideline for the Management of Adult Patients With Supraventricular Tachycardia: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Journal of the American College of Cardiology. 2016 Apr 5:67(13):e27-e115. doi: 10.1016/j.jacc.2015.08.856. Epub 2015 Sep 24 [PubMed PMID: 26409259]
Level 1 (high-level) evidencePage RL, Joglar JA, Caldwell MA, Calkins H, Conti JB, Deal BJ, Estes NAM 3rd, Field ME, Goldberger ZD, Hammill SC, Indik JH, Lindsay BD, Olshansky B, Russo AM, Shen WK, Tracy CM, Al-Khatib SM. 2015 ACC/AHA/HRS Guideline for the Management of Adult Patients With Supraventricular Tachycardia: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Journal of the American College of Cardiology. 2016 Apr 5:67(13):1575-1623. doi: 10.1016/j.jacc.2015.09.019. Epub 2015 Sep 24 [PubMed PMID: 26409258]
Level 1 (high-level) evidenceBathina MN, Mickelsen S, Brooks C, Jaramillo J, Hepton T, Kusumoto FM. Radiofrequency catheter ablation versus medical therapy for initial treatment of supraventricular tachycardia and its impact on quality of life and healthcare costs. The American journal of cardiology. 1998 Sep 1:82(5):589-93 [PubMed PMID: 9732885]
Level 2 (mid-level) evidenceHarper RW, Whitford E, Middlebrook K, Federman J, Anderson S, Pitt A. Effects of verapamil on the electrophysiologic properties of the accessory pathway in patients with the Wolff-Parkinson-White syndrome. The American journal of cardiology. 1982 Dec:50(6):1323-30 [PubMed PMID: 7148709]
Katritsis DG, Josephson ME. Differential diagnosis of regular, narrow-QRS tachycardias. Heart rhythm. 2015 Jul:12(7):1667-76. doi: 10.1016/j.hrthm.2015.03.046. Epub 2015 Mar 28 [PubMed PMID: 25828600]
Meissner A, Stifoudi I, Weismüller P, Schrage MO, Maagh P, Christ M, Butz T, Trappe HJ, Plehn G. Sustained high quality of life in a 5-year long term follow-up after successful ablation for supra-ventricular tachycardia. results from a large retrospective patient cohort. International journal of medical sciences. 2009:6(1):28-36 [PubMed PMID: 19158961]
Level 2 (mid-level) evidenceLaaouaj J, Jacques F, O'Hara G, Champagne J, Sarrazin JF, Nault I, Philippon F. Wolff-Parkinson-White as a bystander in a patient with aborted sudden cardiac death. HeartRhythm case reports. 2016 Sep:2(5):399-403. doi: 10.1016/j.hrcr.2016.05.004. Epub 2016 May 13 [PubMed PMID: 28491720]
Level 3 (low-level) evidenceObeyesekere M, Gula LJ, Skanes AC, Leong-Sit P, Klein GJ. Risk of sudden death in Wolff-Parkinson-White syndrome: how high is the risk? Circulation. 2012 Feb 7:125(5):659-60. doi: 10.1161/CIRCULATIONAHA.111.085159. Epub 2012 Jan 3 [PubMed PMID: 22215858]
Meti N, Mongeon FP, Guerra PG, O'Meara E, Khairy P. Incessant atrioventricular nodal reentrant tachycardia with tachycardia-induced cardiomyopathy, biventricular thrombosis, and pulmonary emboli. HeartRhythm case reports. 2016 Mar:2(2):142-145. doi: 10.1016/j.hrcr.2015.11.012. Epub 2016 Jan 15 [PubMed PMID: 28491653]
Level 3 (low-level) evidenceMoondra V, Sangha R, Greenberg ML. Spontaneous deterioration of atrioventricular nodal reentrant tachycardia to polymorphic ventricular tachycardia in the absence of heart disease. Pacing and clinical electrophysiology : PACE. 2011 Feb:34(2):e14-7. doi: 10.1111/j.1540-8159.2010.02737.x. Epub [PubMed PMID: 20345622]
Level 3 (low-level) evidence