Introduction
Optic nerve sheath meningiomas (ONSM) are rare benign tumors of the central nervous system. Although their growth is slow but progressive, their location is critical as it directly affects the anterior visual pathway and can lead to a severe visual loss. Treatment of this condition is still considered controversial, as the proximity of the tumor to the optic nerve makes it difficult to completely remove without secondary complications and sequelae.[1][2][3][4]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
ONSM is usually localized in the intraorbital or intracanalicular portions of the optic nerve sheath and originates from the cap cells of the arachnoid surrounding the nerve. The intraorbital portion is the most common site of origin (92%). About 95% of ONSM is unilateral. Rare bilateral tumors tend to occur in patients with neurofibromatosis type 2.[5][6]
Most tumors do not have a clear etiology, but they probably have a genetic influence. Meningiomas in particular can have an association with ionizing radiation and hormonal influences, although, there is not a clear association in ONSM.
Epidemiology
ONSM constitute about 2% of all orbital tumors and 1% of all meningiomas.[6][7] These tumors, like their intracranial counterpart, are predominant in middle-aged females. The mean age of presentation is usually less than for intracranial meningiomas because the visual problems make patients seek examination earlier. Although rare, they may be found in children but tend to be more aggressive.[8] Pediatric ONSM has an overall prevalence of between 1:95,000 and 1:525,000.[9] Approximately 5-6% of the cases are bilateral and associated with neurofibromatosis type 2.[6] Of those meningiomas that involve the orbit, only 10% are of primary orbital origin, while the remainders are of intracranial origin extending into the orbit.[6]
Pathophysiology
These tumors arise from the meningeal cells (arachnoid cap cells) lining the optic nerve sheath. They typically grow circumferentially around the optic nerve and can significantly compress its pial vascular supply. These tumors tend to follow the path of least resistance, and as a result of that, they can invade the entire path of the optic nerve, from the optic canal posteriorly to the globe anteriorly.[7][10][11]
Secondary ONSM is an extension of an intracranial meningioma growing into the orbit. A secondary ONSM is more common than primary ONSM, but it is not a true ONSM as it do not grow from the cells surrounding the nerve. Some meningiomas can grow as an en-plaque meningioma along the temporal dura and can easily extend into the orbit through the optic canal or the superior orbital fissure.
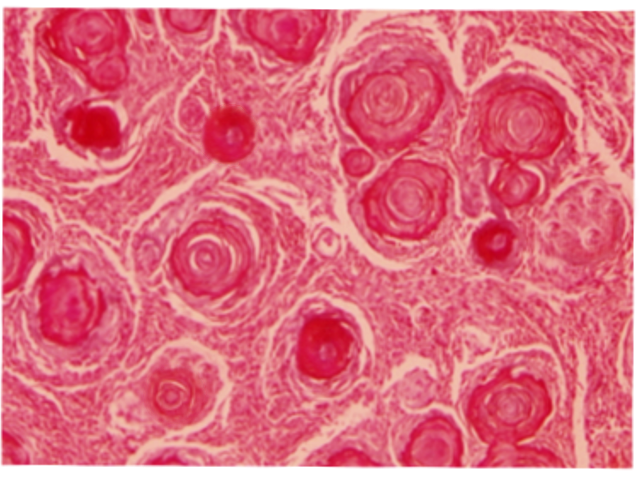
Histopathology
ONSMs arise from the arachnoid cap cells of the optic nerve sheath, and as such are on the inside of the dura. The tumor typically has a smooth lobulated contour. The optic nerve, which is usually circumferentially encased, gradually atrophies due to compression. The tumor may grow and extend into the chiasm through the optic foramen. Malignant transformation is rare.
History and Physical
The natural history of ONSM is characterized by slowly painless and progressive visual loss in the affected eye. If left untreated, this tumor can lead to complete blindness. Visual loss, optic atrophy, and optociliary shunt vessels is the classic triad in patients with an ONSM but most patients do not present the three components.[6][12] Proptosis and resistance to retropulsion are also other signs seen on examination, albeit not always present. Patients can also complain of transient visual loss associated with eye movement, or what is referred to as gaze-evoked amaurosis.
In the early stages, patients can present with chronic optic nerve edema. This occurs because the tumor compresses the intraorbital portion of the optic nerve. Eventually, the edema subsides, and optic pallor develops. Optociliary shunt vessels can develop in about 30% of patients as the optic disc edema resolves. These represent venous collaterals that are connected to the choroidal circulation. They appear after chronic central retinal vein obstruction, such as in ONSM, but can also be found in other conditions such as central retinal vein occlusion, optic nerve glioma, and sphenoid wing meningioma. When vision is affected, there is a relative afferent pupillary deficit in the involved eye. Visual field defects can be present in the affected eye and are not specific; these can be seen as altitudinal defects, generalized constriction, or enlarged blind spots.
Evaluation
The diagnosis of ONSM is confirmed with magnetic resonance imaging (MRI), especially with gadolinium-enhanced fat-suppression sequences. The MRI has become the gold standard for the diagnosis and has obviated the need for tissue biopsy. On MRI, they appear isointense to grey matter on both T1 and T2 weighted imaging. ONSM is a sensitive lesion to gadolinium contrast, demonstrating vivid enhancement which contrasts with the non-enhancing optic nerve. On MRI axial images, it will present with the characteristic "tram-track" sign, which corresponds to the enhancing outer ONSM encircling the inner non-enhancing optic nerve. On the coronal images, this will be seen as a "doughnut" or "non-enhancing dot" sign. Typical appearances of ONSMs on imaging are tubular expansion of the meninges surrounding the optic nerve (62%), globular (23%), fusiform (11%), and focal enlargement of the optic nerve (4%).[13] An optic nerve glioma will demonstrate uniform enhancement of the optic nerve and will not have the classic tram track sign.
A computed tomographic (CT) scan of the orbit and head can show the bony anatomy and hyperostosis produced in secondary tumors. Calcifications can also be seen in the ONSM. CT scans can also demonstrate the classic tram track sign.
Treatment / Management
Observation is the acceptable management in cases where the visual function is intact or remains stable, especially in patients who maintain a central visual acuity of 20/50 or better. Neuro-ophthalmologists will closely follow these patients with a thorough examination, including serial visual fields and peripapillary retinal nerve fiber layer optical coherence tomography.[14][15] Repeat MRI every year is recommended.[4][16](A1)
Tumor resection is almost impossible without incurring a severe visual loss, due to the intimal relationship of the ONSM to the optic nerve. However, surgical resection can be justified in cases of disfiguring proptosis where the visual function has significantly decreased or in cases of intracranial extension. If the eye with the ONSM is blind and the tumor is confined to the orbit the patient should be observed as they grow very slowly, although, some surgeons advocate surgically resecting the tumor to avoid extension to other areas. If the eye is blind and intracranial extension is present, the tumor and the nerve should be removed. Some authors favor surgical intervention as a primary treatment not only stop disease progression and reduce the risk of subsequent vision loss, but also, to some extent, reverse visual deficits that have already occurred.[7]
Transnasal endoscopic optic nerve decompression has been recently proposed and has showed stabilization of the disease and in some cases improvement from the baseline visual deficit.[17][18]
Conventional radiotherapy has been used both pre-operatively and postoperatively for many years.[3][19] More recently stereotactic radiotherapy (STR) has been employed as an alternative to surgery, and may well be superior. In cases where visual function decreases, SRT has become the modality of choice since it delivers the appropriate amount of radiation to the tumor in a localized fashion. Risks of radiation-induced retinopathy or optic neuropathy are prevalent.[20][21] (B2)
Differential Diagnosis
Differential diagnoses include:
- Adult optic neuritis
- Optic nerve glioma
- Orbital lymphoma
- Orbital metastases
- Sarcoidosis[22]
- Idiopathic orbital inflammatory disease (orbital pseudotumor)
Prognosis
The mortality risk from ONSM is practically null. If the tumor is left untreated, progressive vision loss will occur. The tumor produces direct compression of the optic nerve and compromises its vascular supply, and in some cases infiltrates the optic nerve.[7] Most patients will progress to blindness in the eye. At that point a decision regarding surgery is assessed. For those cases where expert surgery is performed, there is approximately 33% - 50% chance for worsening the vision.[7]
Complications
- Permanent vision loss
- Proptosis
- Intracranial injury after surgery
- Cerebrospinal fluid leakage
- Extension of the tumor into chiasm
Postoperative and Rehabilitation Care
Neuro-ophthalmology follow up with regular visual acuity examination and visual field testing are recommended.
An MRI with contrast should be performed every 12 months to assess for growth or recurrence of the disease.
Consultations
- Neurosurgeon
- Neuro-opthalmologist
- Radiation Oncologist
- Neurology
- Neuroradiologist
Deterrence and Patient Education
The patient should be educated about the management and prognosis of ONSMs as they are slowly progressive. Patients need to have clear information so they can make informed decisions about their tumors. Some patients demonstrate clinical stability despite tumor growth, and some patients have rapid vision loss even without an increase in tumor size. All patients should be encouraged to have clinical follow-up evaluations.
Enhancing Healthcare Team Outcomes
Optic nerve sheath meningiomas are best managed by an interprofessional team of neurosurgeons, neuro-ophthalmologists, radiation oncologists, and neurologists. The treatment depends on size, mass effect, and symptoms. Unfortunately despite optimal treatment, vision loss may be unavoidable in most patients. To improve outcomes, prompt consultation with an interprofessional group of specialists is recommended.
Media
(Click Image to Enlarge)
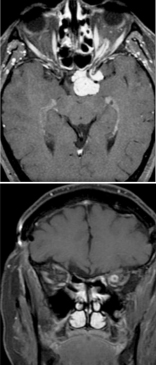
Optic Nerve Sheath Meningioma. Upper axial contrast-enhanced MRI reveals a "tram-track" sign in a patient with optic nerve sheath meningioma, where the thickened optic nerve sheath enhances, creating a tram-track appearance. The lower coronal MRI displays the "bull's eye" appearance of the optic nerve, characterized by a hyperintense ring due to the thickened enhancing optic nerve sheath meningioma.
Contributed by BCK Patel, MD, FRCS
References
Hong S, Usami K, Hirokawa D, Ogiwara H. Pediatric meningiomas: a report of 5 cases and review of literature. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2019 Nov:35(11):2219-2225. doi: 10.1007/s00381-019-04142-y. Epub 2019 Apr 18 [PubMed PMID: 31001646]
Level 3 (low-level) evidenceShaikh M, Khera P, Yadav T, Garg P. Dural Ectasia of the Optic Nerve: A Rare Presentation in Neurofibromatosis Type I. Journal of neurosciences in rural practice. 2019 Apr-Jun:10(2):349-351. doi: 10.4103/jnrp.jnrp_232_18. Epub [PubMed PMID: 31001034]
Kheir V, Faouzi M, Borruat FX. Visual Outcomes of Fractionated Radiotherapy in Optic Nerve Sheath Meningioma: A Retrospective Study. Klinische Monatsblatter fur Augenheilkunde. 2019 Apr:236(4):526-529. doi: 10.1055/a-0828-7335. Epub 2019 Feb 27 [PubMed PMID: 30812038]
Level 2 (mid-level) evidencePandit R,Paris L,Rudich DS,Lesser RL,Kupersmith MJ,Miller NR, Long-term efficacy of fractionated conformal radiotherapy for the management of primary optic nerve sheath meningioma. The British journal of ophthalmology. 2018 Dec 20; [PubMed PMID: 30573496]
Furdová A, Babál P, Kobzová D. Optic nerve orbital meningioma. Ceska a slovenska oftalmologie : casopis Ceske oftalmologicke spolecnosti a Slovenske oftalmologicke spolecnosti. 2018 Spring:74(1):23-30 [PubMed PMID: 30541293]
Parker RT, Ovens CA, Fraser CL, Samarawickrama C. Optic nerve sheath meningiomas: prevalence, impact, and management strategies. Eye and brain. 2018:10():85-99. doi: 10.2147/EB.S144345. Epub 2018 Oct 24 [PubMed PMID: 30498385]
Rassi MS, Prasad S, Can A, Pravdenkova S, Almefty R, Al-Mefty O. Prognostic factors in the surgical treatment of intracanalicular primary optic nerve sheath meningiomas. Journal of neurosurgery. 2018 Sep 21:131(2):481-488. doi: 10.3171/2018.4.JNS173080. Epub [PubMed PMID: 30239315]
Narayan D, Rajak S, Patel S, Selva D. Cystic change in primary paediatric optic nerve sheath meningioma. Orbit (Amsterdam, Netherlands). 2016 Aug:35(4):236-8. doi: 10.1080/01676830.2016.1176212. Epub 2016 Jun 16 [PubMed PMID: 27310300]
Levin LA, Jakobiec FA. Optic nerve tumors of childhood: a decision-analytical approach to their diagnosis. International ophthalmology clinics. 1992 Winter:32(1):223-40 [PubMed PMID: 1537660]
Lekovic GP, Schwartz MS, Hanna G, Go J. Intra-Orbital Meningioma Causing Loss of Vision in Neurofibromatosis Type 2: Case Series and Management Considerations. Frontiers in surgery. 2018:5():60. doi: 10.3389/fsurg.2018.00060. Epub 2018 Oct 9 [PubMed PMID: 30356733]
Level 2 (mid-level) evidenceJacobi DM. Optic nerve sheath meningioma. Clinical & experimental optometry. 2019 Mar:102(2):188-190. doi: 10.1111/cxo.12819. Epub 2018 Jul 28 [PubMed PMID: 30054955]
Frisèn L,Royt WF,Tengroth BM, Optociliary veins, disc pallor and visual loss. A triad of signs indicating spheno-orbital meningioma. Acta ophthalmologica. 1973 [PubMed PMID: 4801582]
Saeed P, Rootman J, Nugent RA, White VA, Mackenzie IR, Koornneef L. Optic nerve sheath meningiomas. Ophthalmology. 2003 Oct:110(10):2019-30 [PubMed PMID: 14522782]
Level 2 (mid-level) evidenceSibony P, Strachovsky M, Honkanen R, Kupersmith MJ. Optical coherence tomography shape analysis of the peripapillary retinal pigment epithelium layer in presumed optic nerve sheath meningiomas. Journal of neuro-ophthalmology : the official journal of the North American Neuro-Ophthalmology Society. 2014 Jun:34(2):130-6. doi: 10.1097/WNO.0000000000000107. Epub [PubMed PMID: 24625774]
Loo JL, Tian J, Miller NR, Subramanian PS. Use of optical coherence tomography in predicting post-treatment visual outcome in anterior visual pathway meningiomas. The British journal of ophthalmology. 2013 Nov:97(11):1455-8. doi: 10.1136/bjophthalmol-2013-303449. Epub 2013 Aug 21 [PubMed PMID: 23966371]
Level 2 (mid-level) evidenceHénaux PL, Bretonnier M, Le Reste PJ, Morandi X. Modern Management of Meningiomas Compressing the Optic Nerve: A Systematic Review. World neurosurgery. 2018 Oct:118():e677-e686. doi: 10.1016/j.wneu.2018.07.020. Epub 2018 Aug 3 [PubMed PMID: 30010062]
Level 1 (high-level) evidenceMaza G, Subramaniam S, Yanez-Siller JC, Otto BA, Prevedello DM, Carrau RL. The Role of Endonasal Endoscopic Optic Nerve Decompression as the Initial Management of Primary Optic Nerve Sheath Meningiomas. Journal of neurological surgery. Part B, Skull base. 2019 Dec:80(6):568-576. doi: 10.1055/s-0039-1677689. Epub 2019 Jan 10 [PubMed PMID: 31750042]
Hunt PJ, DeMonte F, Tang RA, Su SY, Raza SM. Surgical Resection of an Optic Nerve Sheath Meningioma: Relevance of Endoscopic Endonasal Approaches to the Optic Canal. Journal of neurological surgery reports. 2017 Apr:78(2):e81-e85. doi: 10.1055/s-0037-1600897. Epub [PubMed PMID: 28413768]
Sasano H, Shikishima K, Aoki M, Sakai T, Tsutsumi Y, Nakano T. Efficacy of intensity-modulated radiation therapy for optic nerve sheath meningioma. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2019 Oct:257(10):2297-2306. doi: 10.1007/s00417-019-04424-w. Epub 2019 Aug 3 [PubMed PMID: 31377848]
Liu JK, Forman S, Hershewe GL, Moorthy CR, Benzil DL. Optic nerve sheath meningiomas: visual improvement after stereotactic radiotherapy. Neurosurgery. 2002 May:50(5):950-5; discussion 955-7 [PubMed PMID: 11950397]
Level 3 (low-level) evidenceRatnayake G, Oh T, Mehta R, Hardy T, Woodford K, Haward R, Ruben JD, Dally MJ. Long-term treatment outcomes of patients with primary optic nerve sheath meningioma treated with stereotactic radiotherapy. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2019 Oct:68():162-167. doi: 10.1016/j.jocn.2019.07.005. Epub 2019 Aug 7 [PubMed PMID: 31401001]
Micieli JA, Streutker CJ, McIntyre K. Isolated Optic Perineuritis as the Presenting Sign of Sarcoidosis. Journal of neuro-ophthalmology : the official journal of the North American Neuro-Ophthalmology Society. 2020 Jun:40(2):255-257. doi: 10.1097/WNO.0000000000000822. Epub [PubMed PMID: 31490345]