Introduction
n-Hexane is a straight-chain hydrocarbon molecule commonly used as a solvent in various industrial applications. The paint and coating industries employ n-hexane in paint thinners and coatings for its ability to dissolve oils and resins. In the printing industry, the alkane is used in inks due to its quick-drying properties. The food processing industry relies on n-hexane for the extraction of vegetable oils from seeds and crops. In the shoemaking and textile industry, n-hexane is a component of glue and a solvent for cleaning and processing materials. This chemical's versatility makes it an essential component in many industrial applications.
Hydrocarbons like n-pentane and n-heptane are used for the same purposes as n-hexane. However, 6-carbon molecules like n-hexane are notorious for their significant neurologic toxicity. The general aspects, anatomical considerations, natural history, and patterns of spread associated with n-hexane toxicity are explained below.
General Information
n-Hexane exposure mainly occurs through inhalation, particularly in occupational settings like shoe factories where it is used as a solvent. Acute exposure to high concentrations can produce immediate symptoms, including lightheadedness, headache, and confusion, progressing to severe central nervous system (CNS) depression in extreme cases. Chronic exposure, however, poses a more insidious threat as the toxicity primarily stems from n-hexane's metabolites rather than the alkane itself. These metabolites, particularly 2,5-hexanedione, are implicated in the neurotoxic effects observed in workers.[1][2][3]
Anatomy
The primary target of n-hexane toxicity is the peripheral nervous system. Once absorbed, n-hexane is metabolized in the liver to several other compounds, including 2-hexanol, 2,5-hexanediol, and, ultimately, 2,5-hexanedione. The aliphatic compound's neurotoxic effects are attributed to these metabolites, which interfere with normal nerve function. Histological examinations of affected individuals reveal n-hexane–induced axonal swelling, as well as accumulation of neurofilaments and nerve degeneration, particularly in the distal regions of the nerves.[4]
Natural History
The progression of n-hexane–induced polyneuropathy has been well-documented over the past few decades. Initially found among shoe workers, the condition begins with nonspecific symptoms such as nausea, anorexia, and weight loss, followed by sensory disturbances like paresthesias in the lower extremities. Over time, the neuropathy progresses to flaccid paralysis and muscle atrophy, with significant impairment in motor and sensory conduction. Despite the cessation of exposure, recovery can be prolonged and is sometimes incomplete, with residual deficits persisting even after clinical recovery.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The etiology of n-hexane polyneuropathy is rooted in the chemical’s metabolic activation within the body, leading to the production of neurotoxic metabolites. When n-hexane is inhaled or absorbed through the skin, it undergoes a series of metabolic processes, primarily in the liver, mediated by the mixed-function oxidase enzyme system. These processes convert n-hexane into several intermediate compounds, including 2-hexanol and 2,5-hexanediol, which are further oxidized to form 2,5-hexanedione. The metabolite 2,5-hexanedione is primarily responsible for n-hexane's toxic effects on the peripheral nervous system.
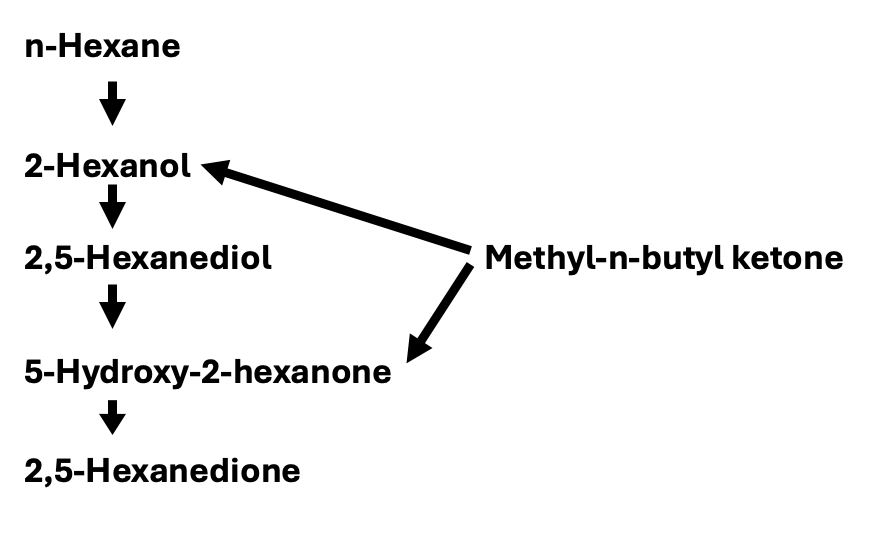
The metabolic pathway begins with the absorption and initial metabolism of n-hexane. Once in the bloodstream, n-hexane is transported to the liver, where liver enzymes, particularly the cytochrome P450 system, metabolize it to 2-hexanol. This intermediate is further oxidized to 2,5-hexanediol, and subsequent oxidation converts 2,5-hexanediol to 2,5-hexanedione (see Image. Formation of 2,5-hexanedione in the Body).
The neurotoxicity of 2,5-hexanedione involves several mechanisms. This metabolite forms covalent bonds with neurofilament proteins, leading to abnormal cross-linking. This disruption impairs the structural integrity and transport functions of the axons, causing axonal swelling and degeneration, particularly affecting the longer peripheral nerves. The altered neurofilaments interfere with the axonal transport system, which is essential for neuronal maintenance and function, resulting in the accumulation of proteins and organelles within the axon and contributing to its degeneration.
Peripheral nerves, especially the long nerves of the lower extremities, are particularly susceptible to damage due to their length and the metabolic demands placed on their axonal transport systems. This selective vulnerability explains the characteristic distal pattern of symptoms seen in n-hexane polyneuropathy.[5]
The clinical manifestations of n-hexane polyneuropathy correlate with the extent of exposure and the resultant neurotoxic burden of 2,5-hexanedione. Initial symptoms include nonspecific signs such as nausea, anorexia, and weight loss. Patients typically develop progressive paresthesias and numbness, particularly in the lower extremities. As the condition progresses, patients may experience muscle weakness, leading to flaccid paralysis and muscle atrophy. Neurologic improvement can occur gradually over several months upon removal from exposure. However, some patients may experience persistent residual deficits, including abnormalities seen during electromyography (EMG).[6]
Several factors influence the development of n-hexane polyneuropathy, including occupational exposure, duration and intensity of exposure, and ventilation and environmental conditions. High incidence rates are seen in industries using n-hexane as a solvent, such as shoe manufacturing. Chronic exposure, especially at high concentrations, increases the risk of developing polyneuropathy. Poor workplace ventilation worsens exposure risks, particularly in colder months when workplaces are less likely to be ventilated. Understanding these pathways is crucial for implementing effective preventive and monitoring strategies in at-risk occupational settings.[7]
Epidemiology
The epidemiology of n-hexane polyneuropathy demonstrates distinct patterns across different demographics and regions. In the United States, the condition has been seen predominantly among workers in industries with significant exposure to organic solvents, such as shoe manufacturing and automotive repair. The prevalence of n-hexane polyneuropathy among these workers underscores the occupational hazard posed by prolonged exposure to n-hexane.
Internationally, the incidence of n-hexane polyneuropathy varies and is influenced by industrial practices and regulatory standards. In some regions, such as parts of China and Italy, the disorder has been reported with higher frequency due to the extensive use of n-hexane in manufacturing processes. For instance, a study involving 122 shoe workers in Italy found a high prevalence of polyneuropathy, with the condition initially reported as more common among women. However, further analysis revealed that this gender disparity was more closely related to job roles than to gender itself.[8]
Seasonal variations in the onset of n-hexane polyneuropathy have also been documented. A notable increase in new cases during winter and spring suggests that environmental factors, such as ventilation and the volatility of hydrocarbons, play a significant role in the manifestation of the disease. Additionally, older workers and those with longer durations of exposure show a higher risk, reflecting the cumulative neurotoxic effects of n-hexane over time.
Overall, the epidemiological data highlight the occupational nature of n-hexane polyneuropathy. Industry practices, environmental conditions, and regulatory measures across different regions influence variations in frequency.[9]
Pathophysiology
n-Hexane polyneuropathy primarily results from the effects of the metabolite 2,5-hexanedione, which disrupts neurofilament cross-linking and axonal transport, leading to axonal swelling and degeneration. These abnormal changes particularly affect the long peripheral nerves. The most common clinical findings include progressive paresthesias, muscle weakness, and flaccid paralysis, often beginning in the lower extremities and advancing to involve all 4 limbs. Neurologic symptoms are typically accompanied by weight loss and, in severe cases, muscular atrophy and hypochromic anemia.[10]
Histopathology
The histopathology of peripheral nerves damaged by n-hexane toxicity is distinct. The process begins with an increase in the number of 10-nm axonal neurofilaments, leading to the accumulation of these filaments in swellings on the proximal sides of the nodes of Ranvier in the distal regions of large, myelinated fibers. As exposure continues, axonal swellings spread in a retrograde fashion up the nerve, eventually involving smaller myelinated and unmyelinated fibers. These swellings displace the paranodal myelin sheaths, leaving denuded areas near the nodes of Ranvier, which can reverse if exposure ceases early enough, allowing for Schwann cell proliferation and remyelination of the axons.
With continued n-hexane exposure, the damaged axons may not undergo remyelination and, instead, break down, similar to what occurs in transected fibers. Modeling n-hexane toxicity in rats indicates that axonal degeneration leads to clinical manifestations, such as muscle weakness and atrophy, particularly noticeable in the hind limbs and progressing to the front limbs in severe cases. The fibers most susceptible to n-hexane toxicity in rats are those in the tibial nerve serving the calf muscles, followed by the plantar nerve branches supplying the flexor digitorum brevis and sensory plantar nerve branches innervating the digits.
Histopathological examination also reveals that n-hexane toxicity can affect the CNS, though to a lesser extent than the peripheral nerves. In cases of prolonged exposure, axonal degeneration can extend into the spinal cord and brainstem. Additionally, exposure can lead to pathological changes in respiratory tissues, as observed in studies with rabbits showing epithelial desquamation, mucosal atrophy, and goblet cell metaplasia in the trachea and bronchi. In severe cases, n-hexane-related pulmonary damage may result in centrilobular emphysema and scattered foci of pulmonary fibrosis, indicating the alkane's broader systemic impact beyond the nervous system.[11]
Toxicokinetics
The toxicokinetics of n-hexane begin with absorption primarily via inhalation due to the compound's high volatility. Approximately 20% to 30% of inhaled n-hexane is absorbed systemically in humans. The absorption occurs via passive diffusion through the epithelial cell membranes in the respiratory tract. Once absorbed, n-hexane is distributed throughout the body, with preferential accumulation in body fat, liver, brain, and muscle tissues. This distribution pattern is due to n-hexane’s lipophilic nature, leading to higher concentrations in fatty tissues than in organs like the kidneys, heart, lungs, and blood.
The metabolism of n-hexane primarily occurs in the liver, where it is processed by mixed-function oxidases. These enzymes convert n-hexane into several metabolites, including the neurotoxic compound 2,5-hexanedione. This metabolite is primarily responsible for the neurotoxic effects associated with chronic n-hexane exposure. The metabolic pathway involves the initial hydroxylation of n-hexane to 2-hexanol, followed by further oxidation to 2,5-hexanediol and finally to 2,5-hexanedione. Studies show that approximately 10% to 20% of absorbed n-hexane is excreted unchanged in the exhaled air. Meanwhile, 2,5-hexanedione is the major metabolite found in urine, accounting for a sizable part of the substance’s biotransformation.
Excretion of n-hexane and its metabolites involves several routes. Unchanged n-hexane is exhaled through the lungs, while 2,5-hexanedione and other metabolites are excreted in the urine. The excretion rate and pattern suggest that a portion of n-hexane and its metabolites enter intermediary metabolism, contributing to systemic toxicity. Saturation of n-hexane metabolism occurs at high exposure levels (≥3,000 ppm in rats), which is significantly higher than typical occupational exposure levels. This saturation indicates that the body's ability to metabolize and clear n-hexane is overwhelmed at these concentrations, leading to increased toxicity.[12]
Comparative toxicokinetic studies have shown that rats are a suitable model for studying n-hexane neurotoxicity, with similar absorption, distribution, metabolism, and excretion patterns observed in humans. While mild neurotoxic effects can be produced in other species like chickens and mice, these effects do not progress to the severe neurotoxicity seen in humans and rats. Therefore, understanding the toxicokinetics of n-hexane in these animal models helps predict human health risks and develop safety guidelines for occupational exposure. Further research into the molecular mechanisms and species-specific responses to n-hexane is crucial for refining these predictive models and improving protective measures for workers.[13]
History and Physical
When evaluating a patient for possible n-hexane toxicity, a comprehensive medical history is essential to identify potential exposure and correlate clinical symptoms. The history should begin with a detailed account of the patient's occupational and environmental exposures, including jobs in industries where n-hexane is used, such as shoe manufacturing, printing, or automotive repair. Inquiry about the duration and intensity of exposure, protective measures used, and whether similar symptoms are present among coworkers is crucial. A detailed description of the work environment, including ventilation and use of solvents, helps in assessing the risk of significant n-hexane exposure.
Additionally, the history should explore the onset and progression of symptoms, which typically include numbness and tingling in the extremities, muscle weakness, and, potentially, flaccid paralysis. Documenting the temporal relationship between exposure and symptom onset provides vital diagnostic clues.
The physical examination should focus on the nervous system, looking for signs consistent with peripheral neuropathy. A thorough neurological exam should assess muscle strength, reflexes, and sensory function. Common findings in n-hexane toxicity include decreased or absent tendon reflexes, particularly in the Achilles tendon, muscle atrophy, and sensory deficits in a glove-and-stocking distribution. Observing gait abnormalities and signs of motor weakness is essential. In addition to peripheral neuropathy, the patient should be examined for signs of CNS involvement, such as mental status changes, coordination difficulties, and hyperreflexia, which may indicate concurrent exposure to other neurotoxic solvents.[14]
Evaluation
Confirmatory diagnostic tests are critical in substantiating the diagnosis of n-hexane toxicity. Electromyography (EMG) and nerve conduction studies (NCS) are essential tools, often revealing slowed motor and sensory conduction velocities. These studies can detect subclinical neuropathy even in asymptomatic individuals and help differentiate n-hexane–induced neuropathy from other causes. Laboratory tests may include blood work to rule out other causes of neuropathy, such as diabetes or vitamin deficiencies, and urine tests to measure n-hexane metabolites, particularly 2,5-hexanedione. However, urinary metabolite levels must be interpreted with caution due to potential confounding exposures to similar solvents.[15]
Besides the standard diagnostic approaches, specific tests for n-hexane exposure can be informative. Measuring urinary levels of 2,5-hexanedione and other metabolites before and after a work shift provides a more accurate assessment of exposure. Exhaled n-hexane may also correlate well with ambient levels and urinary metabolites, offering an alternative monitoring method. These biological tests alone, however, are insufficient to confirm neural dysfunction. Therefore, NCS is still the gold standard for finding early neural impairment in exposed individuals. Such studies should be performed in properly equipped laboratories and interpreted by experienced neurologists.[16]
Finally, a comprehensive medical evaluation for n-hexane toxicity involves integrating history, physical examination, and diagnostic tests to confirm exposure and assess neural function. Early diagnosis and intervention are crucial for preventing long-term damage. Treatment focuses on removing the patient from exposure, as no specific therapies are currently available to reverse the neurotoxic effects of n-hexane. Supportive care and regular follow-up with repeat physical examinations and NCS are essential to monitor recovery and manage any residual deficits. This integrated approach ensures accurate diagnosis, effective management, and prevention of further cases of n-hexane toxicity in occupational settings.[17]
Treatment / Management
The primary approach to treating n-hexane neuropathy involves cessation of further exposure to the toxin. This crucial step halts the progression of the disease and initiates recovery. Symptomatic treatment is also important to manage the discomfort and other manifestations of neuropathy. Medications such as gabapentin, pregabalin, duloxetine, and amitriptyline are commonly used to alleviate neuropathic pain. Additionally, physical therapy and rehabilitation may help improve muscle strength and coordination, addressing any motor deficits that have developed.
The chronology of recovery from n-hexane neuropathy typically begins with the cessation of exposure, after which initial symptom improvement may be observed within a few weeks. However, full recovery may be prolonged, potentially over several months to years, depending on the severity of the exposure and the extent of neural damage. In some cases, patients may experience incomplete recovery, with persistent residual deficits such as muscle weakness or sensory disturbances. Regular follow-up and monitoring through EMG and NCS are essential to track the progress of recovery and adjust treatment plans accordingly.
The prognosis for recovery from n-hexane neuropathy largely depends on the duration and intensity of exposure, as well as the promptness of removal from the source of n-hexane. While many patients experience significant improvement, some may have lasting neurological deficits. These persistent issues often require long-term management and rehabilitation to improve functional outcomes. Early intervention and comprehensive care, including occupational therapy and psychosocial support, are critical to improving the overall prognosis and quality of life for affected individuals.[18]
Differential Diagnosis
Other diseases or chemical exposures should also be considered as a source of neuropathy. Conditions such as diabetes, chronic alcohol use, vitamin deficiencies, chronic kidney disease, and autoimmune disorders like Guillain-Barré syndrome and chronic inflammatory demyelinating polyneuropathy can all lead to neuropathy, with symptoms resembling those induced by n-hexane exposure.
Diabetic neuropathy, for instance, is a common complication of diabetes characterized by numbness, tingling, and weakness in a glove-and-stocking distribution. Alcoholic neuropathy, resulting from chronic alcohol misuse, presents with distal sensory loss, motor weakness, and autonomic dysfunction. Similarly, deficiencies in essential vitamins such as B1, B6, B12, and E can cause symmetrical sensory and motor neuropathy, while uremic neuropathy is a common complication in patients with chronic kidney disease. Autoimmune diseases like Guillain-Barré syndrome and chronic inflammatory demyelinating polyneuropathy can also cause peripheral neuropathy with similar sensory and motor deficits.
Besides neurologically impairing diseases, various chemicals are known to induce neuropathy akin to that caused by n-hexane. Acrylamide, used in various industrial processes, can cause peripheral neuropathy characterized by sensory and motor deficits similar to the ones produced by n-hexane. Arsenic exposure, whether through contaminated drinking water or occupational settings, leads to peripheral neuropathy, with symptoms including pain, numbness, and weakness.
Chronic lead exposure, often from occupational sources or contaminated water, primarily affects motor function, resulting in neuropathy. Thallium, used in certain manufacturing processes and historically in rodenticides, can cause painful peripheral neuropathy. Moreover, methyl-n-butyl ketone and methyl-ethyl-ketone are chemicals that can induce neuropathy. Methyl-n-butyl ketone, like n-hexane, is metabolized to 2,5-hexanedione, leading to similar neurotoxic effects. Although methyl-ethyl-ketone is less toxic, it can enhance the neurotoxic effects of n-hexane and other solvents, contributing to peripheral neuropathy.
Given the wide range of potential causes, a detailed history and thorough diagnostic workup are essential for accurate diagnosis and appropriate management of peripheral neuropathy. Understanding the patient's occupational and environmental exposures, along with a comprehensive medical history, can help differentiate between these various etiologies and guide effective treatment strategies.[19]
Prognosis
The prognosis for n-hexane polyneuropathy varies depending on the duration and intensity of exposure and the promptness of withdrawal from the toxic environment. When exposure to n-hexane is halted, many patients experience an initial worsening of symptoms within the first few weeks, followed by gradual improvement. Recovery can take several months to years. Some individuals achieve significant recovery, while others may continue to have residual neurological deficits such as muscle weakness or sensory disturbances.
Long-term outcomes are generally favorable with prompt discontinuation of exposure and early symptomatic treatment. However, the severity of initial axonal damage can influence the degree of recovery. In cases of severe exposure, patients may have prolonged recovery courses and potentially permanent disabilities. Regular follow-up with EMG and NCS is essential to monitor recovery and adjust treatment strategies.
Complications
The potential complications of n-hexane polyneuropathy are primarily related to the alkane's toxic effects on the peripheral nervous system. Persistent motor and sensory deficits, leading to significant disability, comprise the condition's major complications. Patients may experience ongoing muscle weakness, reduced reflexes, and sensory disturbances such as numbness and tingling, particularly in the lower extremities. In severe cases, weakness can progress to flaccid paralysis, significantly impacting mobility and quality of life.
Another significant complication is chronic pain, which can be challenging to manage. Neuropathic pain associated with n-hexane polyneuropathy may be severe and debilitating, requiring long-term pain management strategies. Medications such as gabapentin, pregabalin, and antidepressants like amitriptyline and duloxetine are often prescribed, but their efficacy can vary, and side effects can limit their use.
In addition to peripheral neuropathy, some patients with severe or prolonged exposure to n-hexane may develop CNS involvement. Symptoms may include cognitive deficits, ataxia, and even spasticity, indicating broader neurotoxic effects beyond the peripheral nerves. CNS involvement can complicate the clinical picture and requires comprehensive neuropsychological evaluation and management.
Consultations
Since neuropathy can arise from many etiologies, consultation with a neurologist and neurophysiologist is important to establish the type of neuropathy, refine the differential diagnosis, and begin long-term treatment. Consultation with medical toxicologists and occupational health physicians may be particularly helpful in determining whether n-hexane has caused a patient's symptoms, investigating workplace exposures, and developing mitigation strategies.
Deterrence and Patient Education
Patient education on neuropathies is crucial to managing the condition and preventing further complications. Neuropathies, which involve damage to the peripheral nerves, can arise from various causes, including diabetes, vitamin deficiencies, chronic alcohol abuse, autoimmune diseases, and exposure to toxic substances like n-hexane. Patients need to understand the symptoms of neuropathy, which may include numbness, tingling, pain, and weakness in the affected areas. Educating patients about the importance of early diagnosis and consistent monitoring can help manage the symptoms more effectively and prevent further nerve damage. Regular check-ups and communication with healthcare providers are vital in managing the condition and adjusting treatment plans as needed.
Specifically, for n-hexane neuropathy, patient education should emphasize the critical role of workplace safety in prevention. Patients working in industries where n-hexane is used, such as shoe manufacturing or automotive repair, should be informed about the risks associated with prolonged exposure to this solvent. These individuals need to understand the importance of using personal protective equipment like gloves and masks, ensuring proper ventilation in their work environment, and following safety protocols to minimize exposure. Additionally, educating patients about recognizing the early symptoms of n-hexane neuropathy, such as lightheadedness, headache, and confusion, can prompt early intervention and reduce the risk of severe neurological damage.
Preventive measures in the workplace are paramount to reducing the incidence of n-hexane neuropathy. Employers and employees should work together to implement safety measures, including regular monitoring of air quality, using safer alternatives to n-hexane when possible, and adhering to occupational safety guidelines. Training sessions on the proper use of personal protective equipment and the importance of workplace hygiene can greatly reduce exposure risk. By fostering a culture of safety and awareness, workplaces can protect their employees from the harmful effects of n-hexane and other toxic substances, thereby enhancing overall health and productivity.
Enhancing Healthcare Team Outcomes
Enhancing outcomes for patients with n-hexane neuropathy involves a multifaceted approach that integrates clinical skills, strategic planning, ethical considerations, and robust interprofessional communication. Physicians and advanced practitioners play a crucial role in the early identification and management of n-hexane neuropathy. Measures include taking detailed occupational histories, performing thorough physical examinations, and utilizing diagnostic tools such as EMG and NCS. Early and accurate diagnosis is essential for preventing further exposure and mitigating the disease's progression. Additionally, advanced practitioners should develop individualized treatment plans that address both symptomatic relief and rehabilitation needs, ensuring a comprehensive approach to patient care.
Effective care coordination and interprofessional communication are vital for enhancing patient-centered care and outcomes in n-hexane neuropathy. Nurses, pharmacists, physical therapists, and occupational health specialists must collaborate closely to monitor the patient’s condition, manage medications, and provide rehabilitative support. Nurses are essential in educating patients about their condition, treatment options, and strategies for avoiding further exposure. Pharmacists can contribute by managing and advising on the safe use of medications for neuropathic pain and other symptoms, ensuring that drug interactions are minimized and therapy is optimized. Physical therapists and occupational therapists play a pivotal role in helping patients regain functional abilities and improve their quality of life through tailored rehabilitation programs.
Ethics and responsibilities also play a significant part in enhancing patient outcomes. Healthcare professionals must advocate for safer workplace environments and better regulatory policies to prevent n-hexane exposure. Advocacy measures should include participating in workplace safety assessments, recommending appropriate personal protective equipment, and ensuring proper ventilation systems in industries that use n-hexane. The ethical practice involves not only treating the symptoms but also addressing the root cause of exposure, thus preventing future cases. By working together, the interprofessional team can ensure comprehensive care, improve patient safety, and enhance overall team performance, ultimately leading to better health outcomes for patients with n-hexane neuropathy.
Media
(Click Image to Enlarge)
References
Bates MN, Pope K, So YT, Liu S, Eisen EA, Hammond SK. Hexane exposure and persistent peripheral neuropathy in automotive technicians. Neurotoxicology. 2019 Dec:75():24-29. doi: 10.1016/j.neuro.2019.08.008. Epub 2019 Aug 21 [PubMed PMID: 31445054]
Huang CC. Polyneuropathy induced by n-hexane intoxication in Taiwan. Acta neurologica Taiwanica. 2008 Mar:17(1):3-10 [PubMed PMID: 18564821]
Liu CH, Huang CY, Huang CC. Occupational neurotoxic diseases in taiwan. Safety and health at work. 2012 Dec:3(4):257-67. doi: 10.5491/SHAW.2012.3.4.257. Epub 2012 Nov 30 [PubMed PMID: 23251841]
Yin H, Guo Y, Zeng T, Zhao X, Xie K. Correlation between levels of 2, 5-hexanedione and pyrrole adducts in tissues of rats exposure to n-hexane for 5-days. PloS one. 2013:8(9):e76011. doi: 10.1371/journal.pone.0076011. Epub 2013 Sep 30 [PubMed PMID: 24098756]
Garcia HD. Acceptable Limits for n-Hexane in Spacecraft Atmospheres. Aerospace medicine and human performance. 2021 Dec 1:92(12):956-961. doi: 10.3357/AMHP.5942.2021. Epub [PubMed PMID: 34986934]
Peters J, Staff NP. Update on Toxic Neuropathies. Current treatment options in neurology. 2022 May:24(5):203-216. doi: 10.1007/s11940-022-00716-5. Epub 2022 Apr 6 [PubMed PMID: 36186669]
. Toxicological Profile for n-Hexane. 1999 Jul:(): [PubMed PMID: 38442219]
Cianchetti C, Abbritti G, Perticoni G, Siracusa A, Curradi F. Toxic polyneuropathy of shoe-industry workers. A study of 122 cases. Journal of neurology, neurosurgery, and psychiatry. 1976 Dec:39(12):1151-61 [PubMed PMID: 1011025]
Level 3 (low-level) evidenceZhu J, Su S, Wen C, Wang T, Xu H, Liu M. Application of multiple occupational health risk assessment models in the prediction of occupational health risks of n-Hexane in the air-conditioned closed workshop. Frontiers in public health. 2022:10():1017718. doi: 10.3389/fpubh.2022.1017718. Epub 2022 Dec 7 [PubMed PMID: 36568752]
Grisold W, Carozzi VA. Toxicity in Peripheral Nerves: An Overview. Toxics. 2021 Sep 11:9(9):. doi: 10.3390/toxics9090218. Epub 2021 Sep 11 [PubMed PMID: 34564369]
Level 3 (low-level) evidenceGuimarães-Costa R, Schoindre Y, Metlaine A, Lefaucheur JP, Camdessanché JP, Maisonobe T, Léger JM. N-hexane exposure: a cause of small fiber neuropathy. Journal of the peripheral nervous system : JPNS. 2018 Jun:23(2):143-146. doi: 10.1111/jns.12261. Epub 2018 Mar 26 [PubMed PMID: 29542204]
dos Santos CR, Meyer Passarelli MM, de Souza Nascimento E. Evaluation of 2,5-hexanedione in urine of workers exposed to n-hexane in Brazilian shoe factories. Journal of chromatography. B, Analytical technologies in the biomedical and life sciences. 2002 Oct 5:778(1-2):237-44 [PubMed PMID: 12376131]
Filser JG, Peter H, Bolt HM, Fedtke N. Pharmacokinetics of the neurotoxin n-hexane in rat and man. Archives of toxicology. 1987:60(1-3):77-80 [PubMed PMID: 3619648]
Jørgensen NK, Cohr KH. N-hexane and its toxicologic effects: a review. Scandinavian journal of work, environment & health. 1981 Sep:7(3):157-68 [PubMed PMID: 20120580]
Li X, Wang Q, Li M, Wang S, Zhang C, Xie K. Hair pyrrole adducts serve as biomarkers for peripheral nerve impairment induced by 2,5-hexanedione and n-hexane in rats. PloS one. 2018:13(12):e0209939. doi: 10.1371/journal.pone.0209939. Epub 2018 Dec 31 [PubMed PMID: 30596762]
Fedtke N, Bolt HM. Detection of 2,5-hexanedione in the urine of persons not exposed to n-hexane. International archives of occupational and environmental health. 1986:57(2):143-8 [PubMed PMID: 3949398]
Cardona A, Marhuenda D, Martí J, Brugnone F, Roel J, Perbellini L. Biological monitoring of occupational exposure to n-hexane by measurement of urinary 2,5-hexanedione. International archives of occupational and environmental health. 1993:65(1):71-4 [PubMed PMID: 8354578]
Smyth D, Kramarz C, Carr AS, Rossor AM, Lunn MP. Toxic neuropathies: a practical approach. Practical neurology. 2023 Apr:23(2):120-130. doi: 10.1136/pn-2022-003444. Epub 2023 Jan 25 [PubMed PMID: 36697225]
Callaghan BC, Gao L, Li Y, Zhou X, Reynolds E, Banerjee M, Pop-Busui R, Feldman EL, Ji L. Diabetes and obesity are the main metabolic drivers of peripheral neuropathy. Annals of clinical and translational neurology. 2018 Apr:5(4):397-405. doi: 10.1002/acn3.531. Epub 2018 Feb 14 [PubMed PMID: 29687018]