Introduction
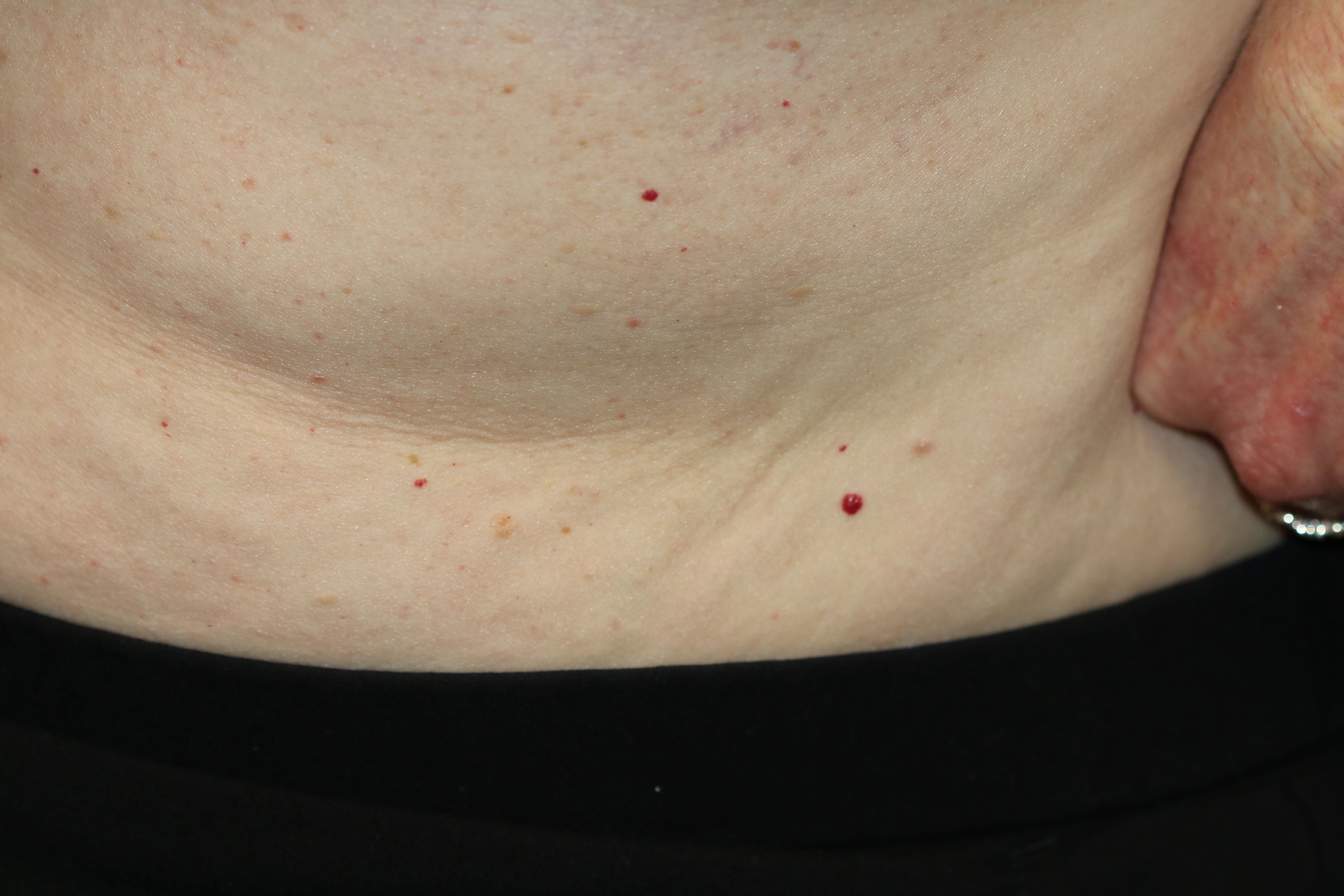
Cherry hemangiomas are common benign cutaneous vascular proliferations. They are also known as cherry angiomas, adult hemangiomas, or senile angiomas as their number tends to increase with age.[1] They were named Campbell De Morgan spots, after the name of a surgeon who worked at Middlesex Hospital from 1842 to 1875.[2] See Image. Cherry Hemangioma. According to the current classification by the International Society for Vascular Anomalies (ISSVA) for benign vascular tumors, cherry hemangiomas are not included, although they have distinct clinical and histopathological features and are highly prevalent in adults.[1]
In the international literature, Campbell De Morgan spots have variously been known as senile angiomas, angioma eruption, angioma tuberosum, senile ectasia, angioma nodulare cutis, perles sanguines, ruby spots, and cancerodermes. Although De Morgan (1811 to 1876) associated these spots with the presence of cancer, this is not a common finding.
According to light and electron microscopic studies of telangiectasia, cherry hemangiomas are a type of papular telangiectasia. These true capillary hemangiomas consist of newly formed capillaries with narrow lumens and prominent endothelial cells arranged in a lobular pattern in the papillary dermis.[3] Cherry hemangiomas generally appear as multiple spots, 1 to 5 mm in size, bright red, and dome-shaped papules mostly on the trunk or upper limbs and rarely on hands, feet, and face.[3]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
There is no well-known cause of cherry angiomas. Some of the associations and possible etiologies of these lesions are as follows.
- Aging: Since these lesions are seen mostly in old age, the aging process can be a cause of their development.[3]
- Genetic mutation: Some studies have seen somatic missense mutations in GNAQ (Q209H, Q209R, R183G) and GNA11 (Q209H) genes in these lesions.[4]
- Pregnancy
Eruptive cherry angiomas: This term indicates the sudden development of multiple and extensive cherry angiomas. They may be seen in the following conditions:
- A side effect of topical nitrogen mustard used for the treatment of vitiligo[5]
- A side effect of cyclosporine[6]
- Chronic graft-host disease[7]
- Lymphoproliferative diseases and multicentric Castleman disease (MCD): The possible mechanism is hypersecretion of vascular endothelial growth factor in response to elevated interleukin 6 levels. Therefore, it is suggested that if the patient presents with sudden multiple cherry angiomas along with systemic symptoms and lymphadenopathy, the patient should be evaluated for multicentric Castleman disease (MCD) and other lymphoproliferative disorders.[8]
- A side effect of ramucirumab: The underlying mechanism for this is ramucirumab-induced somatic activating VEGFR2 mutation.[9]
- Human herpesvirus-8 (HHV8): It is frequently found in eruptive cherry hemangiomas (52.9%)[10]
Epidemiology
Cherry hemangiomas are seen in about 7% of adolescents and 75% of adults over 75 years of age.[2] These lesions develop in adults in the third or fourth decade of life. About 5% to 41% of people begin to have cherry hemangiomas in their 20s. These lesions begin as small red macules or papules. They are initially 1mm in size and can reach up to 2.3 mm by the age of 50 but are usually less than 3.5 mm.[2]
Cherry hemangiomas are distributed equally in individuals of all races and ethnicities. They do not show any gender predisposition.
Pathophysiology
Cherry angiomas mostly appear with age. Although they are found to have an association with some malignancies, they are mostly developed in healthy individuals. These lesions begin as bright red, flat macules and grow to become 1 to 5 mm red papules. They are usually asymptomatic but can bleed with trauma.[3] They can appear on both sun-exposed and unexposed skin but usually spare mucous membranes. These lesions are present in the dermal papillae, and they consist of tortuous and spherical dilatations of capillary loops.[11]
It has been noted that the color of the cherry angiomas changes with hypoxia; they become blue rather than red. The small spots are noted to turn blue sooner than the larger ones. Once the patient is restored to cardiovascular stability, the lesions revert to their ruddy red color.[12]
Histopathology
Histologic examination of these lesions shows that they are located immediately under the epidermis in the papillary dermis and have a distinct structure from surrounding tissues.[13] These are true capillary hemangiomas that consist of newly formed capillaries that have narrow lumens and are lined by prominent endothelial cells that are arranged in a lobular pattern.[3] The capillaries forming cherry hemangioma show perivascular hyalinized sheaths. On immunohistochemical staining, perivascular hyalinized sheath and intercapillary connective tissue of the hemangiomas show marked staining for type VI collagen.[14]
History and Physical
Cherry hemangiomas are dome-shaped, bright, ruby-colored papules with a pale halo. They are small, well-demarcated, and often separated by septa. They are usually 1 to 5 millimeters in diameter. They occur most often as multiple lesions, usually found on the trunk or proximal extremities. They are rarely seen on the face, hands, and feet. When found in the form of multiple adjoining angiomas, they are said to form a polypoid angioma. These lesions most often blanch with applied pressure, but some are fibrotic and may not blanch completely.[15]
These lesions are the most common type of acquired vascular proliferation of the skin. They are diagnosed clinically by appearance. These lesions have no malignant potential. Although they have no malignant potential, they may be confused with amelanotic melanoma, which, in contrast, is more friable.[4]
Evaluation
Cherry hemangiomas are diagnosed clinically by appearance. Optical coherence tomography, which is a low energy light-based imaging device, can be used to evaluate cherry hemangiomas before treating them with laser therapy. This imaging study determines the extent and depth of these lesions, which is useful in predicting the response of these lesions to laser therapy.[16] If there is a concern for malignancy, the lesion should be excised and sent for histopathologic examination.[4]
Although cherry hemangiomas are diagnosed clinically by appearance, their histopathologic findings are essentially the same as true capillary hemangiomas.[3] These histopathologic findings include a thinned epidermis and many newly developed, polypoid, neovascularized capillaries. These capillaries have thin narrow lumens along with prominent endothelial cells. The endothelial cells are most often arranged in a lobular fashion in the papillary dermis.[1] The newly formed capillaries are found early, while these capillaries dilate later. Therefore, late-stage tumors often tend to have increased dilated vessels.[3] The proliferative activation of endothelial cells may therefore be specific to the early stage and may disappear in the later stage.[1]
In addition to these findings, collagen fibers between blood vessels appear to be homogenous and show edematous changes. The epidermis may be atrophic, as characterized by loss of rete ridges. The epidermal collarette is similar in appearance to pyogenic granuloma. In addition, immunohistochemical staining demonstrates no abnormality in the expression or distribution of alpha-smooth-muscle actin and type IV collagen on the capillaries of cherry hemangiomas that have undergone proliferation. The dilated and congested vessels demonstrated through immunohistochemical staining may be responsible for the bright ruby-red appearance of cherry hemangiomas.[3] The atrophic epidermis and proximity to the epidermis also demonstrated through immunohistochemical staining, may be responsible for the ease of bleeding of these lesions secondary to trauma.
Treatment / Management
These lesions are most often asymptomatic but may bleed with trauma.[17] Patients may want to remove a cherry hemangioma, most often for either cosmetic reasons or for the prevention of bleeding following trauma.[18] Treatment for smaller lesions includes local anesthesia with 1% lidocaine, followed by electrocauterization. Larger lesions are often treated with shave excision, with electrocauterization of the base. In addition, cryotherapy may be employed. Superficial lesions may also be treated with CO2 laser therapy.[17]
Although traditionally cryosurgery, electrosurgery, or curettage have been employed in the treatment of cherry hemangioma, more recently, pulsed dye laser or intense pulsed light has been used with success. Krypton and 532 nm diode lasers work very well in eradicating these lesions.[19] Patients should be advised that the removal of these lesions may cause scarring.[18]
Differential Diagnosis
In addition to amelanotic melanoma, the differential diagnosis of cherry hemangioma includes lobular capillary hemangioma, pyogenic granuloma, acquired tufted hemangioma, glomeruloid hemangioma, targetoid hemosiderotic hemangioma, angiolymphoid hyperplasia with eosinophilia, and spindle cell hemangioma.[4]
Prognosis
The prognosis for most patients is excellent. These lesions are most often asymptomatic.[17]
Complications
These lesions may bleed with trauma.[17] Patients may want to remove a cherry hemangioma most often for either cosmetic reasons or for the prevention of bleeding following trauma.[18] Patients should be advised that the removal of these lesions may cause scarring.[18]
Deterrence and Patient Education
Due to the association of cherry hemangioma with certain chemicals, patients should be advised to avoid topical nitrogen mustard therapy, bromides, or other chemicals.[20] These are noted to be increasingly used in tropical climates. In addition, these lesions are often found to be larger in patients with diabetes.[21] They are found with an increased expansion rate in tropical climates. Cherry hemangiomas are often associated with liver transplants, graft versus host disease, and patients who are immunocompromised secondary to cyclosporine treatment. They may also be seen in patients with cerebral cavernous malformations. In addition, there has been a reported case of familial nevus flammeus with early-onset cherry hemangiomas.[20]
Cherry hemangiomas have been found in increasing numbers in middle-aged to older adults. The numbers of these lesions tend to increase in number as a patient’s age increases. Most often, these lesions develop after the third decade of age. They are found in only 5% of adolescents, but 75% of adults over 75 years of age. In addition, multiple cherry hemangiomas have been reported in nursing home patients with a strong association with infections.[21]
Enhancing Healthcare Team Outcomes
Cherry hemangiomas are the most common type of acquired vascular proliferation of the skin and are diagnosed clinically by appearance.[4] The physical exam may demonstrate a well-demarcated, dome-shaped, bright, ruby-colored papule with a pale halo. If there is a concern for malignancy, the lesion must be excised and sent for histopathologic examination, involving coordination of care amongst providers. Once histopathologic findings return, demonstrating a thinned epidermis, newly developed, polypoid, neovascularized capillaries, coordination with further providers is warranted for excision.[1]
Although these lesions are most often asymptomatic, they may bleed with trauma, and patients may want to remove the lesion for either cosmetic reasons or for prevention of bleeding following trauma. The involvement of a provider capable of electrocauterization, shave excision, cryotherapy, CO2 laser therapy, curettage, pulsed dye laser, or intense pulsed light is warranted.[18] In order to optimize outcomes following the diagnosis of cherry hemangioma, prompt coordination of an interprofessional team is recommended.
Media
(Click Image to Enlarge)
References
Fernandez-Flores A, Colmenero I. Campbell de Morgan Spots (Cherry Angiomas) Show Endothelial Proliferation. The American Journal of dermatopathology. 2018 Dec:40(12):894-898. doi: 10.1097/DAD.0000000000001216. Epub [PubMed PMID: 30024413]
MURISON AR, SUTHERLAND JW, WILLIAMSON AM. De Morgan's spots. British medical journal. 1947 May 10:1(4505):634-6 [PubMed PMID: 20248075]
Kim JH, Park HY, Ahn SK. Cherry Angiomas on the Scalp. Case reports in dermatology. 2009 Nov 11:1(1):82-86 [PubMed PMID: 20652121]
Level 3 (low-level) evidenceKlebanov N,Lin WM,Artomov M,Shaughnessy M,Njauw CN,Bloom R,Eterovic AK,Chen K,Kim TB,Tsao SS,Tsao H, Use of Targeted Next-Generation Sequencing to Identify Activating Hot Spot Mutations in Cherry Angiomas. JAMA dermatology. 2019 Feb 1; [PubMed PMID: 30601876]
Ma HJ, Zhao G, Shi F, Wang YX. Eruptive cherry angiomas associated with vitiligo: provoked by topical nitrogen mustard? The Journal of dermatology. 2006 Dec:33(12):877-9 [PubMed PMID: 17169094]
Level 3 (low-level) evidenceDe Felipe I, Redondo P. Eruptive angiomas after treatment with cyclosporine in a patient with psoriasis. Archives of dermatology. 1998 Nov:134(11):1487-8 [PubMed PMID: 9828895]
Level 3 (low-level) evidenceSoo JK, Mortimer PS. Eruptive angiomas associated with graft-versus-host disease. The British journal of dermatology. 2006 Feb:154(2):376-8 [PubMed PMID: 16433816]
Level 3 (low-level) evidenceFajgenbaum DC,Rosenbach M,van Rhee F,Nasir A,Reutter J, Eruptive cherry hemangiomatosis associated with multicentric Castleman disease: a case report and diagnostic clue. JAMA dermatology. 2013 Feb; [PubMed PMID: 23426475]
Level 3 (low-level) evidenceEspinosa Lara P, Medina-Puente C, Riquelme Oliveira A, Jiménez-Reyes J. Eruptive cherry angiomas developing in a patient treated with ramucirumab. Acta oncologica (Stockholm, Sweden). 2018 May:57(5):709-711. doi: 10.1080/0284186X.2017.1410287. Epub 2017 Nov 30 [PubMed PMID: 29188737]
Borghi A, Benedetti S, Corazza M, Gentili V, Ruina G, Di Luca D, Virgili A, Caselli E. Detection of human herpesvirus 8 sequences in cutaneous cherry angiomas. Archives of dermatological research. 2013 Sep:305(7):659-64. doi: 10.1007/s00403-013-1346-5. Epub 2013 Apr 2 [PubMed PMID: 23545752]
Level 3 (low-level) evidenceBraverman IM, Ken-Yen A. Ultrastructure and three-dimensional reconstruction of several macular and papular telangiectases. The Journal of investigative dermatology. 1983 Dec:81(6):489-97 [PubMed PMID: 6417247]
Lawes EG, Campbell de Morgan and his spots. Annals of the Royal College of Surgeons of England. 1984 Jan [PubMed PMID: 19310918]
Sala F, Crosti C, Menni S, Piccinno R. Cherry hemangioma: an SEM study. Journal of cutaneous pathology. 1984 Dec:11(6):531-3 [PubMed PMID: 6520262]
Tamm E, Jungkunz W, Marsch WC, Lütjen-Drecoll E. Increase in types IV and VI collagen in cherry haemangiomas. Archives of dermatological research. 1992:284(5):275-82 [PubMed PMID: 1444576]
Karadag AS,Parish LC, Campbell de Morgan Spot, Better Known As a Cherry Angioma. Skinmed. 2016; [PubMed PMID: 27871342]
Aldahan AS, Mlacker S, Shah VV, Chen LL, Nouri K, Grichnik JM. Utilization of Optical Coherence Tomography in the Evaluation of Cherry Hemangiomas. Journal of drugs in dermatology : JDD. 2016 Jun 1:15(6):713-4 [PubMed PMID: 27272077]
Jairath V,Dayal S,Jain VK,Jindal N,Gogna P,Sehrawat M,Kaur S,Verma P, Is sclerotherapy useful for cherry angiomas? Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2014 Sep; [PubMed PMID: 25099289]
Aversa AJ, Miller OF 3rd. Cryo-curettage of cherry angiomas. The Journal of dermatologic surgery and oncology. 1983 Nov:9(11):930-1 [PubMed PMID: 6630708]
Patel BC. The krypton yellow-green laser for the treatment of facial vascular and pigmented lesions. Seminars in ophthalmology. 1998 Sep:13(3):158-70 [PubMed PMID: 9813106]
Askari N, Vaez-Mahdavi MR, Moaiedmohseni S, Khamesipour A, Soroush MR, Moin A, Jalaie S, Ghazanfari Z, Faghihzadeh E, Ghazanfari T. Association of chemokines and prolactin with cherry angioma in a sulfur mustard exposed population--Sardasht-Iran cohort study. International immunopharmacology. 2013 Nov:17(3):991-5. doi: 10.1016/j.intimp.2012.12.016. Epub 2013 Jan 29 [PubMed PMID: 23370299]
Level 2 (mid-level) evidenceBorghi A,Minghetti S,Battaglia Y,Corazza M, Predisposing factors for eruptive cherry angiomas: New insights from an observational study. International journal of dermatology. 2016 Nov; [PubMed PMID: 27229271]
Level 2 (mid-level) evidence