Anatomy, Head and Neck: Inter-scalene Triangle
Anatomy, Head and Neck: Inter-scalene Triangle
Introduction
The interscalene triangle (sometimes termed simply the scalene triangle) is a region of the neck with fundamental importance to the function of the upper limbs, as the roots of the brachial plexus and the third part of the subclavian artery pass through it. The borders of the triangle are the lateral border of the scalenus anterior muscle, the medial border of the scalenus medius muscle, and the first rib inferiorly. Clinical manifestations of complications relating to the interscalene triangle include thoracic outlet syndrome, which can result in vascular or neurological compromise of the upper limb following compression at the interscalene triangle.[1] This may require surgical decompression if the effects of the condition are sufficiently deleterious on the daily activities of life or cause compromise of the upper limb.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The interscalene triangle is a paired structure situated at the root of the neck, with its apex pointed superiorly towards the base of the skull. The horizontal base of the triangle is formed by the superior border of the first rib. The 2 vertical sides of the triangle are formed by the scalenus anterior and scalenus medius muscles. The anterior covering of the scalene triangle (ie, the "roof" of the triangle) is the prevertebral fascia of the neck, which extends from the body of the T4 vertebra up to the base of the skull.[2] The angle of the aperture between the scalenus anterior and scalenus medius muscles is slight, such that only the roots of the brachial plexus and the corresponding part of the subclavian artery pass through (see Image. Superficial Neck Anatomy).
The first rib is the broadest and flattest of all the ribs and the most curved. Its head articulates with the body of the T1 vertebra, and the medial part articulates with the manubrium sternum. Features along its upper surface include a groove for the subclavian artery and the scalene tubercle, to which the scalenus anterior is attached. The anterior scalene arises from the transverse processes of the anterior tubercles of C3 to C6, terminating as a narrow tendon at the first rib attached to the scalene tubercle on the upper surface of it. The middle scalene arises from the lateral parts of C1 and C2 (atlas and axis), as well as the transverse processes of the posterior tubercles of C3 to C7, and also inserts into the first rib, at the quadrangular area between its neck and the subclavian groove.[3] The function of these muscles is to allow postural stability, flexion, and rotation of the neck, as well as assist in the elevation of the first rib, thus aiding with respiratory effort.[3][4][3]
Embryology
Neck muscles, like the anterior and middle scalene muscles, are derived from the embryonic mesoderm (see Image. Anterior Muscles of the Neck).[5] Specifically, the paraxial mesoderm is split into differential cell masses called somites. These then produce the sclerotome and dermomyotome, the latter producing the body wall muscles.
Blood Supply and Lymphatics
The subclavian artery and vein are at the base of the interscalene triangle.[3] The subclavian artery passes directly through the triangle with the brachial plexus, originating on the left side from the aortic arch and the right side from the brachiocephalic artery. The subclavian arteries ascend superolaterally from their origin before curving laterally and passing posteriorly to the anterior scalene triangle, thus entering the scalene triangle.[6] The subclavian vein remains at the lower border of the triangle.[7] Compression of these vascular structures can lead to weakness, numbness, and vascular compromise.[8]
Nerves
Within the upper part of the interscalene triangle lie the anterior rami of the third through fifth cervical spinal nerves. The base of the triangle is the location of the brachial plexus.[3] The plexus is involved with the motor and sensory function of the shoulder down to the fingertips. Injuries to this plexus can lead to significant deficits in quality of life.[9] As noted previously, the roots of the brachial plexus pass through the interscalene triangle. Subsequently, the divisions of the brachial plexus pass behind the clavicle, and the cords spread out distally in relation to the axillary artery before terminating in distinct branches that supply the musculature and cutaneous innervation of the upper limb.
The phrenic nerve is oblique to the anterior scalene and passes anteriorly to the subclavian artery (C3, C4, C5). The phrenic nerve controls the diaphragmatic muscles for breathing, and although the phrenic nerve is not within the triangle, it is similar to the subclavian vein in that, because of its relative location to the triangle, it is easily prone to compromise from pathologies affecting the interscalene triangle.[10] Another nerve associated with the interscalene triangle, although not within it, is the long thoracic nerve. One of its anterior branches, specifically C7, crosses within the triangle. This nerve becomes subcutaneous near the first and second rib and innervates the serratus anterior muscle.[11]
Muscles
The anterior scalene arises from the transverse processes of the anterior tubercles of C3 to C6, terminating as a narrow tendon at the first rib attached to the scalene tubercle on the upper surface of it. The middle scalene arises from the lateral parts of C1 and C2 (atlas and axis), as well as the transverse processes of the posterior tubercles of C3 to C7, and also inserts into the first rib, at the quadrangular area between its neck and the subclavian groove.[3] The function of these muscles is to allow postural stability, flexion, and rotation of the neck, as well as assist in the elevation of the first rib, thus aiding in respiratory effort.[3][4][3]
Physiologic Variants
Variations of the anterior scalene muscle include differing origins from C2 to C6, C3 to C5, or insertion into the second or third rib. Variations of the middle scalene include an origin from C1 (the atlas) and, like the anterior scalene, inserting onto the second rib.[3] In some patients, the scalene (specifically the anterior scalene) may become hypertrophied, contributing to future aneurysmal changes in the subclavian artery.
The anterior and middle scalene insertions on the first rib can vary, creating a narrow space and leading to a higher-than-normal subclavian artery and brachial plexus. This is important to consider during a surgical intervention in this area. Also, in some patients, the middle scalene can be inserted across the full length of the first rib. In rare cases, the middle and anterior scalene have fused, so the artery and plexus have to pierce through the muscular sheath. The muscles are not the only variants that can occur. The first rib can have structural anomalies that narrow the space, including fusion of ribs, abnormal positioning, and a healed fracture. All variations can make the structures harder to visualize and dictate further surgical or nonsurgical treatment.[7][12]
Surgical Considerations
Treatment of thoracic outlet syndrome can be via scalenectomy for upper thoracic outlet syndrome, and a first rib resection is an option for lower thoracic outlet syndrome. Both procedures can also be done simultaneously for the best results. Regardless, these are done to give the vasculature and nerves wider access to the rest of the upper extremity.[3] This procedure can be performed via a trans-axillary or a supraclavicular approach, and current evidence does not demonstrate any significant safety or complication rate differences between the 2 techniques.[13]
During the procedure, the scalenus anterior and medius muscles are identified and divided before the first rib is excised; however, using an interscalene approach, it is also possible to complete this without the division of the scalenus anterior.[14] Alternatively, as a conservative measure, instead of surgical intervention, scalene muscle injections can help to reduce pain. This injection is more effective in patients with thoracic outlet syndrome due to whiplash or traction injuries.[15]
Clinical Significance
Interscalene Block
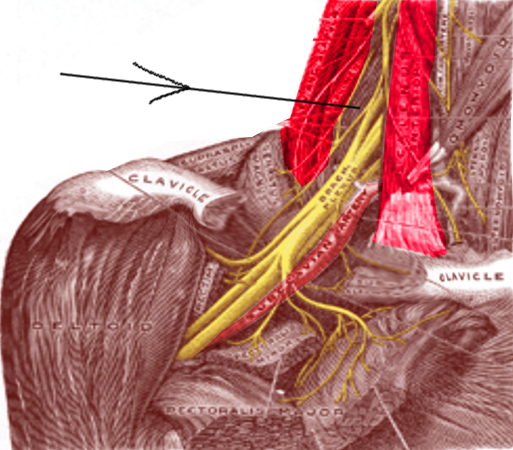
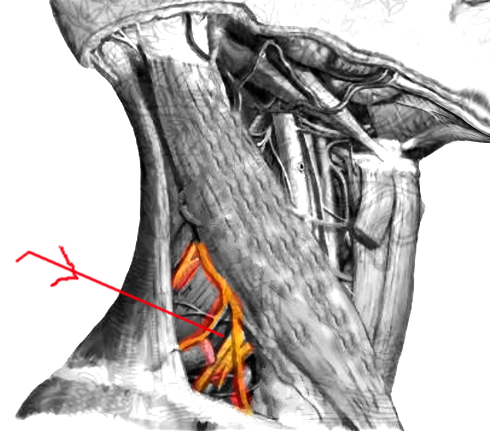
After surgery in the postoperative period, nerve blocks may be used to decrease the pain experienced by the patient (see Image. Interscalene Block). One widely used example of such a nerve block is the inter-scalene nerve block, used specifically in many upper extremity injuries.[16] This nerve block can be used before or after shoulder surgery, allowing anesthesia of the suprascapular, lateral pectoral, musculocutaneous, axillary nerves, and parts of the cervical plexus.[17] The needle is inserted in a mediolateral fashion to reduce the risk of damage to important associated nearby nervous structures, including the long thoracic and dorsal scapular nerves.[2] The risk of long-term complications following interscalene nerve blocks was found in 1 prospective trial to be 0.4%; however, given the critical nature of the upper limb to daily life, any dysfunction is highly impactful on a patient's quality of life (see Image. Interscalene Block).[18][19][20]
Thoracic Outlet Syndrome
Thoracic outlet syndrome (TOS) is a common syndrome due to abnormal regional anatomy or injuries to the associated structures, with an incidence of between 3 and 8 in 1000 people.[21] Importantly, the interscalene triangle is 1 of 3 sites where compression of the critical neurovascular structures traveling between the neck and the upper limb can be compressed. The 3 sites of compression causing thoracic outlet syndrome are the interscalene triangle, the costoclavicular space, and the sub-pectoral space. The causes for this syndrome are myriad and include supernumerary scalene muscles, congenital abnormalities of the first rib, cervical ribs, fibrous bands, aneurysms, and trauma.[22] Indeed, the clinical entity of thoracic outlet syndrome is a group of pathological entities depending both on the site of compression and on the specific structure that is being compressed and causing symptoms: neurogenic TOS (compression of the brachial plexus), arterial TOS (compression of the subclavian artery), venous TOS (compression of the subclavian vein), and disputed TOS (non-specific TOS with no clear origin.)[23]
For these reasons, thoracic outlet syndrome has long been considered difficult to diagnose, not least because there is no formal clinical diagnostic test.[24] The clinical history is important and may include neck, occiput, chest, shoulder, and upper limbs pain and paraesthesia, weakness, or heaviness in the affected upper limb. On examination of the patient, Raynaud phenomenon may be upper limb ischemia, upper limb swelling, cyanosis, muscle atrophy, or wasting, depending on the cause and site of compression.[24] Furthermore, palpation of the interscalene triangle may reproduce the symptoms if this is the level at which compression occurs. Thoracic outlet syndrome is notorious for lacking a specific clinical presentation.[25]
In general, the neurovascular structures in the triangle undergo compression. The compression of the subclavian artery is more diagnostic of TOS than the compression of the subclavian vein because vein compression can occur in non-TOS patients.[25] Diagnostic testing for this condition includes clinic maneuvers and imaging.
Diagnostic modalities for investigating suspected thoracic outlet syndrome include ultrasonography, chest radiography, CT angiography, magnetic resonance angiography, dedicated venography or arteriography, nerve conduction studies, or needle electromyography.[20] Different criteria can be used to help diagnose TOS. These criteria include weakness or pain in the upper body and face, tenderness of the anterior or middle scalene, positive Tinel sign, positive neck tilt test, and positive costoclavicular compression test.[15]
Media
(Click Image to Enlarge)
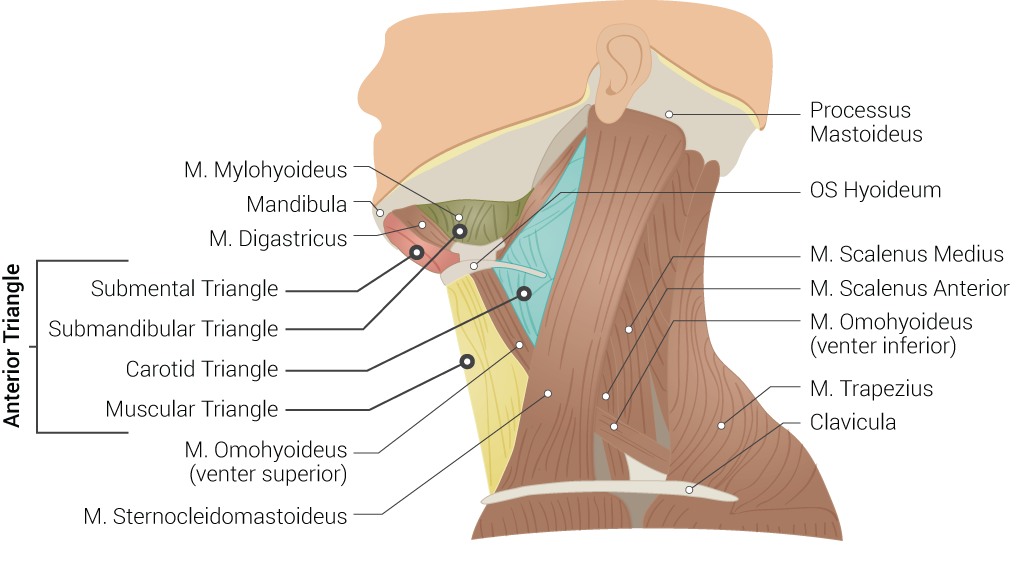
Superficial Neck Anatomy. This left lateral-view illustration shows the anterior and posterior triangles. The anterior triangle is further divided into the submental, submandibular, carotid, and muscular triangles. The muscles in this illustration include the mylohyoideus, digastricus, omohyoideus (venter superior and inferior), sternocleidomastoideus, scalenus medius and anterior, and trapezius. Bony structures include the mandible, mastoid process, left hyoid, and clavicle.
Contributed by B Palmer
(Click Image to Enlarge)
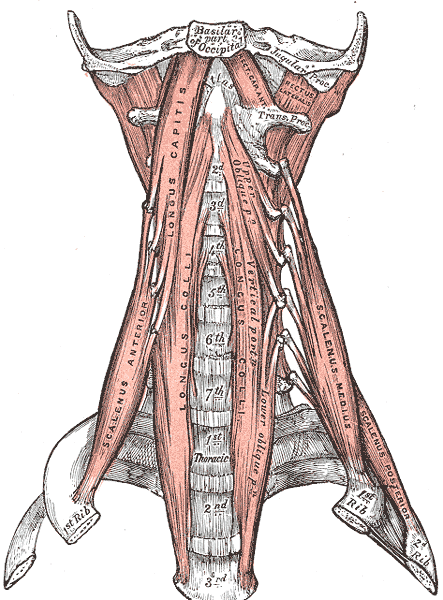
Anterior Muscles of the Neck. Anterior muscles of the neck include the basilar part of the occipital, jugular process, scalenus anterior, longus capitis, longus colli, scalenus medius and posterior, atlas, thoracic vertebrae, and cervical vertebrae.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
References
Urschel HC, Patel A. Thoracic Outlet Syndromes. Current treatment options in cardiovascular medicine. 2003 Apr:5(2):163-168 [PubMed PMID: 12686013]
Kim HJ, Park SH, Shin HY, Choi YS. Brachial plexus injury as a complication after nerve block or vessel puncture. The Korean journal of pain. 2014 Jul:27(3):210-8. doi: 10.3344/kjp.2014.27.3.210. Epub 2014 Jun 30 [PubMed PMID: 25031806]
Dahlstrom KA, Olinger AB. Descriptive anatomy of the interscalene triangle and the costoclavicular space and their relationship to thoracic outlet syndrome: a study of 60 cadavers. Journal of manipulative and physiological therapeutics. 2012 Jun:35(5):396-401. doi: 10.1016/j.jmpt.2012.04.017. Epub 2012 May 17 [PubMed PMID: 22608284]
Chiti L,Biondi G,Morelot-Panzini C,Raux M,Similowski T,Hug F, Scalene muscle activity during progressive inspiratory loading under pressure support ventilation in normal humans. Respiratory physiology & neurobiology. 2008 Dec 31 [PubMed PMID: 18952011]
Theis S, Patel K, Valasek P, Otto A, Pu Q, Harel I, Tzahor E, Tajbakhsh S, Christ B, Huang R. The occipital lateral plate mesoderm is a novel source for vertebrate neck musculature. Development (Cambridge, England). 2010 Sep 1:137(17):2961-71. doi: 10.1242/dev.049726. Epub [PubMed PMID: 20699298]
Level 3 (low-level) evidenceConnolly MR, Auchincloss HG. Anatomy and Embryology of the Thoracic Outlet. Thoracic surgery clinics. 2021 Feb:31(1):1-10. doi: 10.1016/j.thorsurg.2020.09.007. Epub [PubMed PMID: 33220766]
Atasoy E. Thoracic outlet syndrome: anatomy. Hand clinics. 2004 Feb:20(1):7-14, v [PubMed PMID: 15005377]
Wijeratna MD,Troupis JM,Bell SN, The use of four-dimensional computed tomography to diagnose costoclavicular impingement causing thoracic outlet syndrome. Shoulder [PubMed PMID: 27582945]
Ferreira SR, Martins RS, Siqueira MG. Correlation between motor function recovery and daily living activity outcomes after brachial plexus surgery. Arquivos de neuro-psiquiatria. 2017 Sep:75(9):631-634. doi: 10.1590/0004-282X20170090. Epub [PubMed PMID: 28977143]
Hamada T, Usami A, Kishi A, Kon H, Takada S. Anatomical study of phrenic nerve course in relation to neck dissection. Surgical and radiologic anatomy : SRA. 2015 Apr:37(3):255-8. doi: 10.1007/s00276-014-1343-1. Epub 2014 Jul 16 [PubMed PMID: 25026999]
Safran MR. Nerve injury about the shoulder in athletes, part 2: long thoracic nerve, spinal accessory nerve, burners/stingers, thoracic outlet syndrome. The American journal of sports medicine. 2004 Jun:32(4):1063-76 [PubMed PMID: 15150060]
Qaja E,Honari S,Rhee R, Arterial thoracic outlet syndrome secondary to hypertrophy of the anterior scalene muscle. Journal of surgical case reports. 2017 Aug; [PubMed PMID: 28928918]
Level 3 (low-level) evidenceAboul Hosn M, Goffredo P, Man J, Nicholson R, Kresowik T, Sharafuddin M, Sharp WJ, Pascarella L. Supraclavicular Versus Transaxillary First Rib Resection for Thoracic Outlet Syndrome. Journal of laparoendoscopic & advanced surgical techniques. Part A. 2020 Jul:30(7):737-741. doi: 10.1089/lap.2019.0722. Epub 2020 May 15 [PubMed PMID: 32412829]
Abdel Ghany W, Nada MA, Toubar AF, Desoky AE, Ibrahim H, Nassef MA, Mahran MG. Modified Interscalene Approach for Resection of Symptomatic Cervical Rib: Anatomic Review and Clinical Study. World neurosurgery. 2017 Feb:98():124-131. doi: 10.1016/j.wneu.2016.10.113. Epub 2016 Oct 28 [PubMed PMID: 27989967]
Lee GW, Kwon YH, Jeong JH, Kim JW. The efficacy of scalene injection in thoracic outlet syndrome. Journal of Korean Neurosurgical Society. 2011 Jul:50(1):36-9. doi: 10.3340/jkns.2011.50.1.36. Epub 2011 Jul 31 [PubMed PMID: 21892402]
Yan Z,Chen Z,Ma C, Liposomal bupivacaine versus interscalene nerve block for pain control after shoulder arthroplasty: A meta-analysis. Medicine. 2017 Jul; [PubMed PMID: 28682872]
Level 1 (high-level) evidenceFeigl GC, Litz RJ, Marhofer P. Anatomy of the brachial plexus and its implications for daily clinical practice: regional anesthesia is applied anatomy. Regional anesthesia and pain medicine. 2020 Aug:45(8):620-627. doi: 10.1136/rapm-2020-101435. Epub 2020 May 28 [PubMed PMID: 32471922]
Borgeat A, Ekatodramis G, Kalberer F, Benz C. Acute and nonacute complications associated with interscalene block and shoulder surgery: a prospective study. Anesthesiology. 2001 Oct:95(4):875-80 [PubMed PMID: 11605927]
Gelabert HA, Rigberg DA, O'Connell JB, Jabori S, Jimenez JC, Farley S. Transaxillary decompression of thoracic outlet syndrome patients presenting with cervical ribs. Journal of vascular surgery. 2018 Oct:68(4):1143-1149. doi: 10.1016/j.jvs.2018.01.057. Epub 2018 Apr 25 [PubMed PMID: 29705086]
Camporese G, Bernardi E, Venturin A, Pellizzaro A, Schiavon A, Caneva F, Strullato A, Toninato D, Forcato B, Zuin A, Squizzato F, Piazza M, Stramare R, Tonello C, Di Micco P, Masiero S, Rea F, Grego F, Simioni P. Diagnostic and Therapeutic Management of the Thoracic Outlet Syndrome. Review of the Literature and Report of an Italian Experience. Frontiers in cardiovascular medicine. 2022:9():802183. doi: 10.3389/fcvm.2022.802183. Epub 2022 Mar 22 [PubMed PMID: 35391849]
Illig KA, Donahue D, Duncan A, Freischlag J, Gelabert H, Johansen K, Jordan S, Sanders R, Thompson R. Reporting standards of the Society for Vascular Surgery for thoracic outlet syndrome. Journal of vascular surgery. 2016 Sep:64(3):e23-35. doi: 10.1016/j.jvs.2016.04.039. Epub [PubMed PMID: 27565607]
Ajalat MJ, Pantoja JL, Ulloa JG, Cheng MJ, Patel RP, Chun TT, Gelabert HA. A Single Institution 30-Year Review of Abnormal First Rib Resection for Thoracic Outlet Syndrome. Annals of vascular surgery. 2022 Jul:83():53-61. doi: 10.1016/j.avsg.2021.12.080. Epub 2022 Jan 6 [PubMed PMID: 34998937]
Ciampi P, Scotti C, Gerevini S, De Cobelli F, Chiesa R, Fraschini G, Peretti GM. Surgical treatment of thoracic outlet syndrome in young adults: single centre experience with minimum three-year follow-up. International orthopaedics. 2011 Aug:35(8):1179-86. doi: 10.1007/s00264-010-1179-1. Epub 2010 Dec 24 [PubMed PMID: 21184222]
Level 2 (mid-level) evidencePovlsen S, Povlsen B. Diagnosing Thoracic Outlet Syndrome: Current Approaches and Future Directions. Diagnostics (Basel, Switzerland). 2018 Mar 20:8(1):. doi: 10.3390/diagnostics8010021. Epub 2018 Mar 20 [PubMed PMID: 29558408]
Level 3 (low-level) evidenceLaBan MM, Zierenberg AT, Yadavalli S, Zaidan S. Clavicle-induced narrowing of the thoracic outlet during shoulder abduction as imaged by computed tomographic angiography and enhanced by three-dimensional reformation. American journal of physical medicine & rehabilitation. 2011 Jul:90(7):572-8. doi: 10.1097/PHM.0b013e31821a70ff. Epub [PubMed PMID: 21552107]