Introduction
The meaning of plagiocephaly is an oblique head.[1] The Greek word plagios means oblique, and kephale means head. Plagiocephaly is defined as an asymmetric shape of the head due to unilateral flattening. The term flathead can be used as a synonym. Plagiocephaly can be categorized into synostotic or deformational types.[2]
The International Classification of Diseases defines isolated synostotic plagiocephaly as a form of nonsyndromic craniosynostosis characterized by premature fusion of one coronal or lambdoid suture leading to skull deformity and facial asymmetry. Unilateral coronal synostosis produces anterior plagiocephaly.[3] Premature fusion of lambdoid suture causes synostotic posterior plagiocephaly.[4] Deformational plagiocephaly is due to intrauterine or postnatal deformational forces.[2] Deformational plagiocephaly is also known as positional plagiocephaly.[5]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
More than 95% of cases of nonsyndromic craniosynostosis are sporadic.[6] Positive family history is present in 8-15% of patients with nonsyndromic coronal synostosis.[7] In lambdoid synostosis, the incidence of positive family history is 0% to 6%. Closure of the coronal suture starts at approximately 24 years of age, while lambdoid starts at 26 years of age. Craniosynostosis is the premature closure of a suture forming an osseous bridging and usually causing an abnormal skull shape.
Intrauterine deformational forces include a fetus's odd position, irregular uterus shape, compression of the fetus' head when descends into the pelvis, or due to multiple fetus pregnancy. Postnatal deformational forces most commonly occur due to prolonged position of the head for long periods. The etiology of craniosynostosis can be multifactorial due to intrinsic bone abnormalities, genetic mutations, and environmental factors.[8] Craniosynostosis can be associated with metabolic conditions such as hypophosphatemia, rickets, and hyperthyroidism, pre-term delivery, low birth weight, exposure to teratogens, valproic acid, and shunted hydrocephalus. Experiments in mice have shown that fetal head constraint induces upregulation of transforming growth factor (TGF) beta receptor 1 and 2 and fibroblast growth factor receptor 2 (FGFR2) at the coronal suture, thus causing coronal synostosis.[9] The genetic mutations associated with unilateral coronal synostosis include the twisted family basic helix-loop-helix transcription factor TWIST, FGFR2, and FGFR3.[10]
The incidence of deformational plagiocephaly increased after the "Back to Sleep" campaign started in 1992, which promoted a supine position to prevent sleep-related infant deaths; however, the incidence of sudden infant death syndrome has decreased.[11] Potential risk factors for deformational plagiocephaly include assisted delivery with forceps, vacuum extractor, first-born child, male sex, the supine position at sleep, limited neck rotation, low level of activity, and lack of tummy time.[11][12] Tummy time is the awake time of the baby spent in the prone position. There is a high association with congenital muscular torticollis. Due to the torticollis, the infant may hold the neck and head in a preferred position for a prolonged period causing flattening of a part of the head.[13]
Epidemiology
The incidence of anterior plagiocephaly is around one out of 10,000 live births.[14] It occurs in 13% to 16% of children with craniosynostosis. The incidence of unilateral coronal craniosynostosis is four to seven times that of bilateral coronal synostosis. The male to female ratio is 1 to 2. Unilateral lambdoid synostosis represents 1 to 5% of craniosynostosis.[15][16] The approximate occurrence of lambdoid synostosis is one in 33,000 births.
The prevalence of deformational plagiocephaly is 15 to 20% of infants.[17] However, a higher incidence of as much as 46.6% had been reported.[18] The prevalence is slightly higher in males at between 1 and 3 to 1 and usually diagnosed before four months of life. Before 1992, the incidence of deformational plagiocephaly was one in 300 infants. However, since the "Back to Sleep" campaign by the American Academy of Pediatrics, now called "Safe to Sleep," the incidence of deformational plagiocephaly has increased 400% to 600%.[16][19][20][21]
Secondary craniosynostosis can occur in systemic diseases such as rickets and hypothyroidism in newborns with microcephaly and following shunt placement for hydrocephalus.[22]
History and Physical
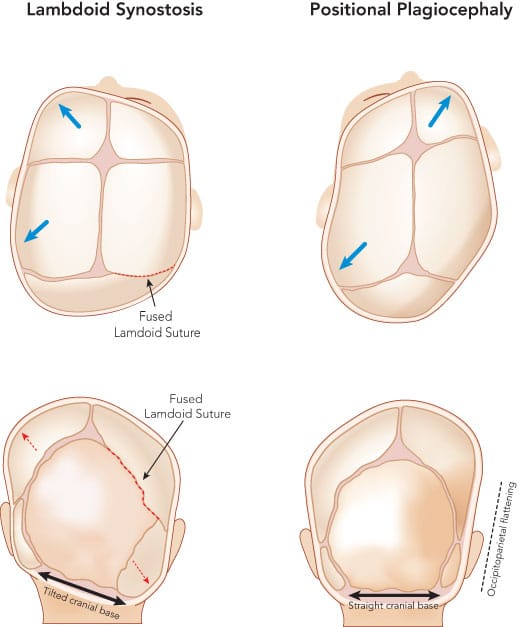
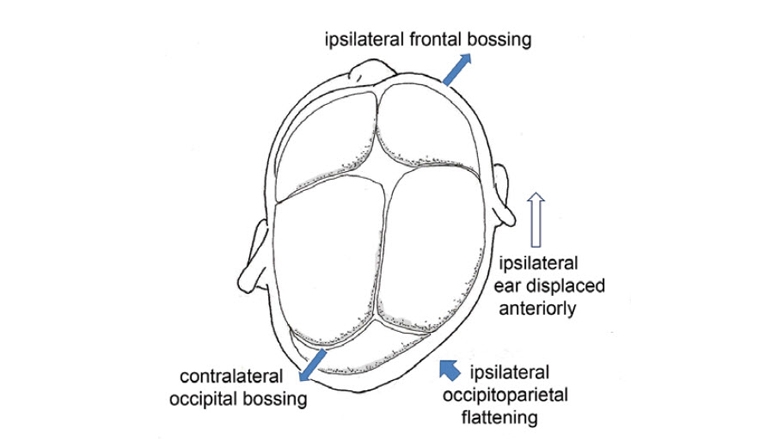
In synostotic anterior plagiocephaly, the forehead is flattened, and the supraorbital margin is high.[22] The forehead is pushed forward on the opposite side. There can be a deviation of the nasal septum to the normal side. Strabismus is seen in 50% to 60% due to dysfunction of superior oblique muscle secondary to changes in orbital roof and trochlea.[23] Deviation of mandible and change of occlusion may also be seen. A bony ridge can be palpated along the fused suture. In synostotic posterior plagiocephaly, frontal and occipital bossing occur on the opposite side.[22] There is a downward displacement of the ipsilateral ear and mastoid. When viewed from above, the skull resembles a trapezoid.
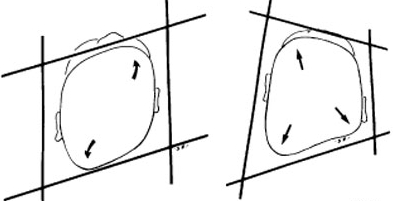
It is often challenging to distinguish deformational plagiocephaly from synostotic posterior plagiocephaly clinically.[16] Deformational plagiocephaly is more common. There are some points to differentiate deformational plagiocephaly from lambdoid synostotic plagiocephaly.[23] Lambdoid synostosis is present at birth; whereas, deformational plagiocephaly usually occurs some weeks after birth. History of a preferred sleeping position is noted in deformational plagiocephaly. The bony ridge along the suture and bulging mastoid are present in lambdoid synostosis. Frontal bossing is ipsilateral in deformational plagiocephaly; while, it is contralateral in lambdoid synostosis. There is contralateral occipital bossing in deformational plagiocephaly. Displacement of the ipsilateral ear is anterior in deformational plagiocephaly and posterior in synostosis. However, some authors have noted that ear position is not a very reliable sign to distinguish them.[16][24] The shape of the skull is a parallelogram in deformational plagiocephaly and trapezoid in lambdoid synostosis.
Increased intracranial pressure (ICP) features can be present in 15-20% of children with coronal or lambdoid synostosis.[25] However, the clinical features such as headache, vomiting, altered sensorium, and bulging fontanelle may not be found in many patients. Papilledema is the most reliable sign of intracranial hypertension in children with craniosynostosis, with a specificity of 98%.[26] Chronically raised ICP can lead to blindness due to optic atrophy and subnormal intelligence.[25]
Evaluation
Computed tomographic (CT) scan with three-dimensional (3D) reconstruction is the principal imaging modality for evaluating craniosynostosis.[16][27][28] A 64-slice multidetector CT scan helps in assessing vault and skull base with reasonably low radiation.[29] Premature fusion of a suture restricts the growth perpendicular to the affected suture.[30] There will be compensatory overgrowth along the other patent sutures. The CT findings of a prematurely fused suture are peri-sutural sclerosis, bony bridging, or the absence of the suture. In deformational plagiocephaly, the CT shows a patent lambdoid suture, and the frontal bossing is ipsilateral, as opposed to lambdoid synostosis. There is no significant distortion of the anteroposterior axis of the skull base in deformational plagiocephaly.[31] The chondrocranium is symmetric in deformational plagiocephaly.
The findings in unilateral coronal synostosis are a shallow ipsilateral anterior cranial fossa, contralateral frontal bossing, and an elevated roof and lateral wall of the ipsilateral orbit called the "harlequin eye" sign. The findings of unilateral lambdoid synostosis are ipsilateral occipitoparietal flattening, contralateral frontal and occipitoparietal bossing, a unilateral small posterior cranium, and a tilted skull base. There is an ipsilateral deviation of the posterior fossa in the endocranial skull base view of unilateral lambdoid synostosis. Morphometric analysis of the skull base with the help of 3D CT can differentiate the three causes of plagiocephaly.[32] The skull base asymmetry is in the anterior and middle cranial fossae for coronal synostosis and in the posterior and middle cranial fossae for lambdoid synostosis.
Lambdoid synostosis can cause crowding of the posterior fossa and herniation of the caudal part of the cerebellum into the foramen magnum resulting in Chiari malformation.[25] Hydrocephalus and syringomyelia can also be associated; these are better appreciated in brain magnetic resonance imaging (MRI). However, a conventional MRI will not show the sutures satisfactorily. A new gradient-echo sequence is known as "Black Bone" MRI can show a patent suture as a hyperintensity signal, but it will be absent if the suture is closed.[33]
Anthropometric measurements help to assess the severity of plagiocephaly.[19] These are taken with calipers. The change observed in deformational plagiocephaly is the difference between the diagonal occipital-frontal transcranial diameters. This is the transdiagonal difference and will quantify the degree of asymmetry in deformational plagiocephaly. The severity of deformational plagiocephaly can be assessed by the difference between the diagonal lengths on each head's side.[13] A difference of 9 to 12 mm is defined as mild to moderate, and if more than 12 mm as severe asymmetry. An index named cranial vault asymmetry index can be calculated as 100 times the difference between cranial diagonal diameters divided by the shorter cranial diagonal diameter. A value greater than 3.5 indicates severe asymmetry.
Treatment / Management
Conservative treatment should be adopted for patients with deformational plagiocephaly and mild unilateral synostosis.[22] Meticulous evaluation by physical examination and diagnostic evaluation should be done to rule out synostosis before adopting a conservative approach for posterior plagiocephaly.[34] The treatment of deformational plagiocephaly is conservative with modification of sleep posture, counter positioning, physiotherapy for torticollis, tummy time, and helmet.[1][4][35] A helmet can be used for those who are not showing improvement with repositioning techniques. Helmet therapy for deformational plagiocephaly was introduced in 1979 by Clarren et al., who used a fiberglass model.[36] The helmet functions as a molding device. Currently, the helmet is custom-made for each child.[5] The optimal age for helmet therapy is 5-6 months, and it is not effective after 18 months of age.[4] Helmet therapy can cause contact dermatitis and pressure sores.[5] However, there is a lack of Class I evidence supporting the use of a helmet in deformational plagiocephaly.[37] If the deformity is severe, the Congress of Neurological Surgeons recommends helmet therapy if used during the appropriate period of infancy.[38](A1)
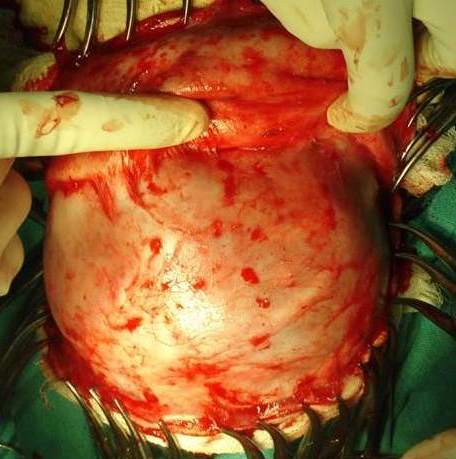
Surgical treatment is indicated in nonsyndromic craniosynostosis to reduce the morphologic abnormality, prevent increased ICP, and prevent psychosocial issues. Surgical aims are to achieve sufficient intracranial volume for brain growth and correct the skull's shape.[15] The steps are the removal of the fused suture and remodeling of both hypoplastic and compensatory growth abnormalities.[4] The optimal age for surgery is between 6 and 12 months of age, the most active phase of the brain and head development.
The surgical options are open craniotomy with reconstruction or endoscopic suturectomy. The procedures are fronto-orbital remodeling for anterior plagiocephaly and occipital advancement for posterior plagiocephaly.[39] The surgical techniques described are open calvarial reconstruction, strip craniectomy with implantation, barrel stave osteotomy, endoscopic suture release, and cranial distraction osteogenesis.[8][16][40] In an open procedure, the fused suture is identified, the bone flap with the suture is removed and remodeled, and fixation is done with resorbable plates.[22] In cranial distraction osteogenesis, distractors are applied to the osteotomised sites, and slow incremental distraction is done over weeks.[40] Some patients have associated torticollis with synostotic posterior plagiocephaly.[16][27] Release of sternocleidomastoid may have to be done for associated refractory torticollis.[16] Successful surgery can resolve preoperative papilledema that is present in two-thirds of the patients with posterior synostotic plagiocephaly.[28](B2)
The cranial bones are flexible until the age of six months and can be easily manipulated by the endoscopic approach.[22] Open surgery is preferred after six months. A shorter operative time, less blood loss, and faster recovery are the advantages of endoscopic surgery. Nowadays, endoscopically assisted minimally invasive procedures are done more often.[41] However, a remodeling helmet should be used after the endoscopic procedure. Improvement in ophthalmic outcomes with a reduction in amblyopia, astigmatism, and strabismus has been observed in children with unilateral coronal synostosis after endoscopic strip craniectomy and helmet therapy.[42](B2)
Differential Diagnosis
The principal differential diagnosis in plagiocephaly determines if it is deformational (positional) or synostotic due to a suture's premature closure. Anterior plagiocephaly is due to coronal synostosis. Posterior plagiocephaly should be differentiated as synostotic or deformational.
Facts noted in history are the presence at birth, preferred sleep position, and improvement with time.[23] Craniosynostosis is congenital, whereas deformational plagiocephaly usually develops in the neonatal period. History of a preferred sleep position will be present in cases of deformational plagiocephaly. The deformity in synostosis worsens with time. The deformities caused by position improve as the child develops head control.
The child with unilateral lambdoid synostosis has a thick ridge over the fused suture, with compensatory contralateral parietal and frontal bossing.[43] There is an ipsilateral occipitomastoid bulge, with a posteroinferior displacement of the ipsilateral ear. These characteristics are opposite to the findings in the children with deformational plagiocephaly. In the view from above, the shape of the head will be trapezoid in lambdoid synostosis and parallelogram in deformational plagiocephaly. A 3D CT will confirm the diagnosis. Torticollis is most commonly associated with deformational plagiocephaly. Chiari malformation can be present with lambdoid synostosis.
Prognosis
In deformational plagiocephaly, satisfactory outcomes can be achieved with conservative treatments if the treatments are initiated at an early stage of the disease.[13] The plasticity of the skull is good in infancy. Physiotherapy can improve congenital muscular torticollis.
There is evidence that nonsyndromic single suture synostosis can result in persistent neuropsychological deficits. Surgical intervention improves motor and cognitive function, especially in severe craniosynostosis. Long-term follow-up after surgery often found normal academic and social function.[28] If untreated or uncontrolled, craniosynostosis can lead to raised ICP and cognitive impairment.[25] Surgical correction of synostotic plagiocephaly produces significant improvements in the skull's shape and achieves high parent satisfaction.
Complications
Deformational plagiocephaly usually corrects with frequent repositioning of the baby; however, it can produce cosmetic deformities if not treated adequately. Untreated unilateral coronal plagiocephaly may cause strabismus, astigmatism, amblyopia, and mandible malalignment.[42]
Surgical complications after synostotic plagiocephaly correction are usually relatively few and minor and do not produce permanent sequela.[16][28] The following complications are associated with the surgical treatment of isolated and syndromic craniosynostosis.[22][39][40][44] Those patients with craniofacial syndromes are more prone to complications. Blood transfusion is reduced with the use of an endoscopic procedure compared to an open procedure.[41]
- Excessive blood loss
- Venous air embolism
- Consumption coagulopathy
- Cerebrospinal fluid leak
- Dural tears
- Hyperthermia
- Hypoactivity
- Wound infection local
- Epidural abscess
- Ear infections
- Subcutaneous hematoma
- Epidural hematoma
- Residual plagiocephaly
- Reoperation
Helmet therapy can lead to complications, although very rare.[13]
- Inadequate correction
- Pressure damage to the skin at the site of application
- Scalp erosion, ulcer, and temporary hair loss
- Contact allergic dermatitis
Postoperative and Rehabilitation Care
The child should be monitored after surgery in the pediatric intensive care unit.[44] This is especially mandatory after open surgery. Volume, hemoglobin, hematocrit, and cardiovascular status should be closely monitored. Paracetamol can be given to relieve pain. Sedatives should be avoided in an extubated child. Invasive monitoring can be discontinued the next day if the child is stable.
Deterrence and Patient Education
Early diagnosis and appropriate treatment of synostotic plagiocephaly can prevent aesthetic sequelae in children.
Deformational plagiocephaly treatment primarily includes position behavior modification; however, in some cases, additional measures are necessary, including helmet therapy.[34]
Education should be given to parents regarding positioning and the use of tummy time. Intervention should be started as soon as the diagnosis is made.
Deformational plagiocephaly will not cause any developmental or neurocognitive delay.[28]
Enhancing Healthcare Team Outcomes
Healthcare professionals must teach parents regarding measures to prevent plagiocephaly.[5] The first measure is to encourage lying on each side in the supine position. The second measure is to promote prone position during awake time (tummy time) for 10 to 15 minutes at least three times per day with a goal of 30 minutes per day.[19] The management of plagiocephaly is challenging and complex. It is critical to make a correct diagnosis between lambdoid synostotic plagiocephaly and deformational plagiocephaly, as the first requires surgical intervention.
A multidisciplinary team to manage complex syndromic craniosynostosis cases is needed and requires the combined efforts of a pediatric neurosurgeon, plastic surgeon, and maxillofacial surgeons. The nurses will closely monitor the patient's vital signs, administer medications, evaluate scalp dressings, and assist with the family's education. In the postoperative period for pain, wound infection prophylaxis, and vomiting, the pharmacist will ensure that the patient is on the right analgesics, antiemetics, and appropriate antibiotics.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Kim SY,Park MS,Yang JI,Yim SY, Comparison of helmet therapy and counter positioning for deformational plagiocephaly. Annals of rehabilitation medicine. 2013 Dec; [PubMed PMID: 24466513]
Margulis A,Hatuel V,Weinberg A,Neuman A,Israel Z,Wexler MR, [Plagiocephaly in children: etiology, differential diagnosis and helmet treatment]. Harefuah. 1999 Apr 2; [PubMed PMID: 15532593]
Kronig SAJ,Kronig ODM,Vrooman HA,Veenland JF,Van Adrichem LNA, Quantification of Severity of Unilateral Coronal Synostosis. The Cleft palate-craniofacial journal : official publication of the American Cleft Palate-Craniofacial Association. 2020 Oct 20; [PubMed PMID: 33078622]
Orra S,Tadisina KK,Gharb BB,Rampazzo A,Doumit G,Papay F, The danger of posterior plagiocephaly. Eplasty. 2015; [PubMed PMID: 25987949]
Cummings C, Positional plagiocephaly. Paediatrics [PubMed PMID: 23024590]
Timberlake AT,Persing JA, Genetics of Nonsyndromic Craniosynostosis. Plastic and reconstructive surgery. 2018 Jun; [PubMed PMID: 29579021]
Greenwood J,Flodman P,Osann K,Boyadjiev SA,Kimonis V, Familial incidence and associated symptoms in a population of individuals with nonsyndromic craniosynostosis. Genetics in medicine : official journal of the American College of Medical Genetics. 2014 Apr; [PubMed PMID: 24071792]
Garrocho-Rangel A,Manriquez-Olmos L,Flores-Velazquez J,Rosales-Berber MA,Martinez-Rider R,Pozos-Guillen A, Non-syndromic craniosynostosis in children: Scoping review. Medicina oral, patologia oral y cirugia bucal. 2018 Jul 1; [PubMed PMID: 29924758]
Level 2 (mid-level) evidenceHunenko O,Karmacharya J,Ong G,Kirschner RE, Toward an understanding of nonsyndromic craniosynostosis: altered patterns of TGF-beta receptor and FGF receptor expression induced by intrauterine head constraint. Annals of plastic surgery. 2001 May; [PubMed PMID: 11352430]
Level 3 (low-level) evidenceMulliken JB,Gripp KW,Stolle CA,Steinberger D,Müller U, Molecular analysis of patients with synostotic frontal plagiocephaly (unilateral coronal synostosis). Plastic and reconstructive surgery. 2004 Jun; [PubMed PMID: 15253176]
Bialocerkowski AE,Vladusic SL,Wei Ng C, Prevalence, risk factors, and natural history of positional plagiocephaly: a systematic review. Developmental medicine and child neurology. 2008 Aug; [PubMed PMID: 18754894]
Level 1 (high-level) evidenceDe Bock F,Braun V,Renz-Polster H, Deformational plagiocephaly in normal infants: a systematic review of causes and hypotheses. Archives of disease in childhood. 2017 Jun; [PubMed PMID: 28104626]
Level 1 (high-level) evidenceJung BK,Yun IS, Diagnosis and treatment of positional plagiocephaly. Archives of craniofacial surgery. 2020 Apr; [PubMed PMID: 32380806]
Di Rocco C,Paternoster G,Caldarelli M,Massimi L,Tamburrini G, Anterior plagiocephaly: epidemiology, clinical findings,diagnosis, and classification. A review. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2012 Sep; [PubMed PMID: 22872257]
Rhodes JL,Tye GW,Fearon JA, Craniosynostosis of the lambdoid suture. Seminars in plastic surgery. 2014 Aug; [PubMed PMID: 25210507]
Borad V,Cordes EJ,Liljeberg KM,Sylvanus TS,Lim PK,Wood RJ, Isolated Lambdoid Craniosynostosis. The Journal of craniofacial surgery. 2019 Nov-Dec; [PubMed PMID: 31633668]
Renz-Polster H,De Bock F, Deformational plagiocephaly: The case for an evolutionary mismatch. Evolution, medicine, and public health. 2018; [PubMed PMID: 30151193]
Level 3 (low-level) evidenceMawji A,Vollman AR,Fung T,Hatfield J,McNeil DA,Sauvé R, Risk factors for positional plagiocephaly and appropriate time frames for prevention messaging. Paediatrics [PubMed PMID: 25382999]
Looman WS,Flannery AB, Evidence-based care of the child with deformational plagiocephaly, Part I: assessment and diagnosis. Journal of pediatric health care : official publication of National Association of Pediatric Nurse Associates [PubMed PMID: 22726709]
Hauck FR,Tanabe KO, Beyond [PubMed PMID: 28806464]
Marshall JM, Shahzad F. Safe Sleep, Plagiocephaly, and Brachycephaly: Assessment, Risks, Treatment, and When to Refer. Pediatric annals. 2020 Oct 1:49(10):e440-e447. doi: 10.3928/19382359-20200922-02. Epub [PubMed PMID: 33034660]
Kajdic N,Spazzapan P,Velnar T, Craniosynostosis - Recognition, clinical characteristics, and treatment. Bosnian journal of basic medical sciences. 2018 May 20; [PubMed PMID: 28623672]
Ghizoni E,Denadai R,Raposo-Amaral CA,Joaquim AF,Tedeschi H,Raposo-Amaral CE, Diagnosis of infant synostotic and nonsynostotic cranial deformities: a review for pediatricians. Revista paulista de pediatria : orgao oficial da Sociedade de Pediatria de Sao Paulo. 2016 Dec; [PubMed PMID: 27256993]
Smartt JM Jr,Reid RR,Singh DJ,Bartlett SP, True lambdoid craniosynostosis: long-term results of surgical and conservative therapy. Plastic and reconstructive surgery. 2007 Sep 15; [PubMed PMID: 17805129]
Choi JW,Lim SY,Shin HJ, Craniosynostosis in Growing Children : Pathophysiological Changes and Neurosurgical Problems. Journal of Korean Neurosurgical Society. 2016 May; [PubMed PMID: 27226849]
Tuite GF,Chong WK,Evanson J,Narita A,Taylor D,Harkness WF,Jones BM,Hayward RD, The effectiveness of papilledema as an indicator of raised intracranial pressure in children with craniosynostosis. Neurosurgery. 1996 Feb; [PubMed PMID: 8869054]
Vannier MW,Hildebolt CF,Marsh JL,Pilgram TK,McAlister WH,Shackelford GD,Offutt CJ,Knapp RH, Craniosynostosis: diagnostic value of three-dimensional CT reconstruction. Radiology. 1989 Dec; [PubMed PMID: 2813770]
Level 2 (mid-level) evidenceAbboud H,Rifi L,Melhaoui A,Arkha Y,El Ouahabi A, Diagnosis, Management, and Outcome in 9 Children with Unilateral Posterior Synostotic Plagiocephaly. World neurosurgery. 2020 Aug; [PubMed PMID: 32389879]
Khanna PC,Thapa MM,Iyer RS,Prasad SS, Pictorial essay: The many faces of craniosynostosis. The Indian journal of radiology [PubMed PMID: 21431034]
Kim HJ,Roh HG,Lee IW, Craniosynostosis : Updates in Radiologic Diagnosis. Journal of Korean Neurosurgical Society. 2016 May; [PubMed PMID: 27226852]
Sze RW,Hopper RA,Ghioni V,Gruss JS,Ellenbogen RG,King D,Hing AV,Cunningham ML, MDCT diagnosis of the child with posterior plagiocephaly. AJR. American journal of roentgenology. 2005 Nov; [PubMed PMID: 16247160]
Captier G,Leboucq N,Bigorre M,Canovas F,Bonnel F,Bonnafé A,Montoya P, Plagiocephaly: morphometry of skull base asymmetry. Surgical and radiologic anatomy : SRA. 2003 Jul-Aug; [PubMed PMID: 14504821]
Eley KA,Watt-Smith SR,Sheerin F,Golding SJ, [PubMed PMID: 25038852]
Level 2 (mid-level) evidenceKalra R,Walker ML, Posterior plagiocephaly. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2012 Sep; [PubMed PMID: 22872253]
O'Broin ES,Allcutt D,Earley MJ, Posterior plagiocephaly: proactive conservative management. British journal of plastic surgery. 1999 Jan; [PubMed PMID: 10343585]
Clarren SK,Smith DW,Hanson JW, Helmet treatment for plagiocephaly and congenital muscular torticollis. The Journal of pediatrics. 1979 Jan; [PubMed PMID: 758420]
Goh JL,Bauer DF,Durham SR,Stotland MA, Orthotic (helmet) therapy in the treatment of plagiocephaly. Neurosurgical focus. 2013 Oct; [PubMed PMID: 24079781]
Level 1 (high-level) evidenceTamber MS,Nikas D,Beier A,Baird LC,Bauer DF,Durham S,Klimo P Jr,Lin AY,Mazzola C,McClung-Smith C,Mitchell L,Tyagi R,Flannery AM, Guidelines: Congress of Neurological Surgeons Systematic Review and Evidence-Based Guideline on the Role of Cranial Molding Orthosis (Helmet) Therapy for Patients With Positional Plagiocephaly. Neurosurgery. 2016 Nov; [PubMed PMID: 27759675]
Level 1 (high-level) evidenceEsparza J,Hinojosa J,García-Recuero I,Romance A,Pascual B,Martínez de Aragón A, Surgical treatment of isolated and syndromic craniosynostosis. Results and complications in 283 consecutive cases. Neurocirugia (Asturias, Spain). 2008 Dec; [PubMed PMID: 19112545]
Level 3 (low-level) evidenceNoto M,Imai K,Masuoka T,Sakahara D,Kunihiro N, Retrospective Review and Analysis of Complications Due to Cranial Distraction for Craniosynostosis. The Journal of craniofacial surgery. 2020 Nov 4; [PubMed PMID: 33156168]
Level 2 (mid-level) evidenceArts S,Delye H,van Lindert EJ, Intraoperative and postoperative complications in the surgical treatment of craniosynostosis: minimally invasive versus open surgical procedures. Journal of neurosurgery. Pediatrics. 2018 Feb; [PubMed PMID: 29171801]
MacKinnon S,Proctor MR,Rogers GF,Meara JG,Whitecross S,Dagi LR, Improving ophthalmic outcomes in children with unilateral coronal synostosis by treatment with endoscopic strip craniectomy and helmet therapy rather than fronto-orbital advancement. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus. 2013 Jun; [PubMed PMID: 23791406]
Level 2 (mid-level) evidenceHuang MH,Gruss JS,Clarren SK,Mouradian WE,Cunningham ML,Roberts TS,Loeser JD,Cornell CJ, The differential diagnosis of posterior plagiocephaly: true lambdoid synostosis versus positional molding. Plastic and reconstructive surgery. 1996 Oct; [PubMed PMID: 8823012]
Level 2 (mid-level) evidenceMathijssen IM, Guideline for Care of Patients With the Diagnoses of Craniosynostosis: Working Group on Craniosynostosis. The Journal of craniofacial surgery. 2015 Sep; [PubMed PMID: 26355968]