Introduction
One of the first features of the human body to be noticed by another person is the face. The face is made up of many different muscles, nerves, bones, and organs and has an intriguing network of motor and sensory innervation. The motor innervation to the muscles located in the face is derived mainly from the facial nerve (CN VII) and trigeminal nerve (CN V). The facial nerve provides innervation to the muscles that are involved in creating facial expressions, whereas the trigeminal nerve innervates the muscles used in mastication.
The sensory innervation of the face comes from the trigeminal nerve. The trigeminal nerve subdivides into three main branches that split the face into three territories. The first branch from the trigeminal nerve is the ophthalmic nerve (CN V1). The ophthalmic nerve provides innervation to the forehead, eyes, and nose. The second branch of the trigeminal nerve is the maxillary nerve (CN V2). The maxillary nerve's sensory innervation follows the maxilla bone. The sensory territory of the maxillary nerve will be the cheeks and the upper lip mainly. The last branch from the trigeminal nerve is the mandibular nerve (CN V3). The mandibular nerve is responsible for providing sensory innervation to the regions that correspond to the mandible. These regions are the jawline, chin, and lower lip.
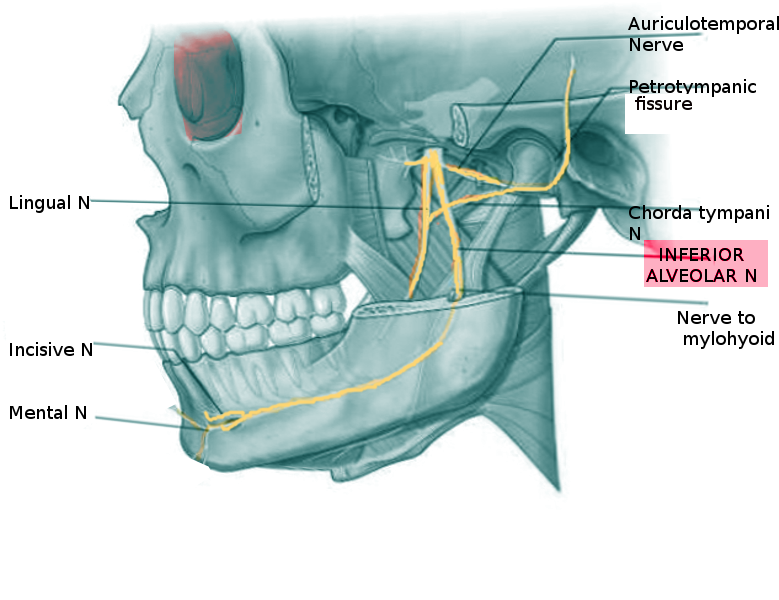
The branches of the trigeminal nerve will further divide into smaller nerve branches to optimally provide sensory innervation to their respective territories. For example, the maxillary nerve will branch into the superior alveolar nerves. Another example is the mandibular nerve branching into the inferior alveolar nerve. The inferior alveolar nerve will be responsible for sensory innervation to the cheek, lips, chin, teeth, and gingivae.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The sensory territories for the alveolar nerves divide between the superior alveolar nerves and the inferior alveolar nerves. The superior alveolar nerves will come from the branching of the maxillary nerve. The maxillary nerve will branch into the three superior alveolar nerves before it exits the infraorbital foramen. The superior alveolar nerves are named based on their anatomical location. The first branch is the anterior superior alveolar nerve. The anterior superior alveolar nerve travels toward the maxillary sinus. The sensory innervation of the anterior superior alveolar nerve includes the premolars (canine teeth and incisor teeth), maxillary sinus, and inferior meatus. The second branch of the maxillary nerve is the middle superior alveolar nerve. The middle superior alveolar nerve is responsible for providing additional sensory innervation to the sinuses and the maxillary premolar teeth. The third branch of the maxillary nerve is the posterior superior alveolar nerve. The posterior alveolar nerve provides sensory innervation to the cheeks, maxillary sinus, and gingivae. All of the alveolar nerve branches from the maxillary nerve provide sensory innervation to the gingivae and sinuses. These superior alveolar nerves have overlaps in their sensory territory innervation with one another. This provides collateral sensory innervation via a dental nerve plexus.[1]
The inferior alveolar nerve comes from a different branch of the trigeminal nerve. The inferior alveolar nerve is a mandibular nerve branch. The inferior alveolar nerve is responsible for sensory innervation to the gingivae on the lower jaw. The inferior alveolar nerve also branches into the mylohyoid nerve and the mental nerve. As the inferior alveolar nerve descends the mandible, it will branch into the mylohyoid nerve to provide motor innervation to the mylohyoid muscle and the anterior belly of the digastric muscle.[2] The inferior alveolar nerve will then travel in the mandibular foramen until it reaches the mental foramen. Once at the mental foramen, the inferior alveolar nerve exits and becomes the mental nerve. The mental nerve is responsible for innervating the chin, lower lip, and gingivae.[3]
Embryology
During embryology, the development of peripheral nerves derives from neural crest cells. The development of the structures in the face originates from the branchial apparatus. The branchial arch is made up of mesoderm and neural crest cells. The branchial arch will form the muscles, nerves, and bones in the face and neck. The first branchial arch will develop the first two branches of the trigeminal nerve. The maxillary nerve and the mandibular nerve and their innervation territories will form from the first branchial arch. As the face develops, the maxillary nerve and mandibular nerve will branch into their respective alveolar nerves, which means the alveolar nerves are derivatives of neural crest cells.
Blood Supply and Lymphatics
The proximal blood supply to the maxillary nerve and the mandibular nerve at the region of the pons is the anterior inferior cerebellar arteries.[3] The distal blood supply to the maxillary, the mandibular nerve, and their nerve branches are from the external carotid artery. The external carotid artery is responsible for the perfusion of the external head and face. The distal blood supply also provides perfusion to the alveolar nerves. The blood supply to the trigeminal nerve will be from the basilar artery, cerebellar arteries, and vertebral arteries.[4]
The lymphatic drainage of the alveolar nerves and their sensory territories is toward the submental lymph nodes, the submandibular lymph nodes, and the preauricular lymph nodes. The lymph fluid will eventually be drained back into the right lymphatic duct and the thoracic duct. The right side of the face will drain into the right lymphatic duct, and the left side of the face will empty into the thoracic duct. Finally, the lymph in the right lymphatic duct and the thoracic duct will drain back to the central circulation.
Nerves
The alveolar nerves separate into the superior alveolar nerves and the inferior alveolar nerves. The superior alveolar nerves originate from the maxillary branch of the trigeminal nerve. The superior alveolar nerves divide into the anterior, middle, and posterior superior alveolar nerves. While the inferior alveolar nerve originates from the mandibular branch of the trigeminal nerve, the alveolar nerve will branch into the mental nerve. All of these alveolar nerves and their subdivisions will contribute to sensory innervation to the face and mouth.
Muscles
The maxillary nerve and the mandibular nerve provide motor innervation to the muscles involved in mastication. While the alveolar nerves are branches of the maxillary nerve and the mandibular nerve, they are purely sensory to the face and mouth.
Physiologic Variants
The superior alveolar nerves are three branches that come from the maxillary nerve. Numerous variations exist with the superior alveolar nerves. The origin, path, and branching patterns vary considerably. In some individuals, the dental plexus formed by the superior alveolar nerves maybe be larger or smaller. Some individuals may lack one of the superior alveolar nerve branches. For example, the middle alveolar nerve may be absent in some individuals.[1][5]
In contrast, the superior alveolar nerves, the inferior alveolar nerve, str usually only one nerve. The inferior alveolar nerve is typically the only alveolar nerve that branches from the mandibular nerve. The origin, path, and branching pattern of this nerve can also vary. In some cases, there is a bifid inferior alveolar nerve instead of just one nerve. The inferior alveolar nerve may also have small connections to the neighboring nerves. The path in the mandibular foramen may also vary. The path variations can be due to several factors. The most common cause of the path to differ is the variable shape of the mandible, which could cause the inferior alveolar nerve to travel lower or higher in the bone itself.[3][6]
Surgical Considerations
In surgery, the knowledge of the alveolar nerves is crucial. The alveolar nerves are important in providing sensory innervation to the teeth, gingivae, lower lip, and chin. If the alveolar nerves are damaged, there may be a permanent loss of sensation in those areas.[7][8][9][10]
In both plastic and oral and maxillofacial surgery, the jaw may require reconstruction, or the implantation of teeth may be necessary. It is important to reconstruct the jaw without damaging the alveolar nerves. In some dental implantations, the alveolar nerves may become translocated during the procedure.
Clinical Significance
Dentists commonly inject the superior and inferior alveolar nerves with local anesthetic for dental procedures. The knowledge of the location of these nerves will guide a successful nerve block. But it is crucial to take into consideration the many variations in the nerves. If the classic approach to the nerve block is insufficient, the operator should consider that maybe there is a slight variation in the location of the alveolar nerves.[11]
Dental pain can highlight the importance of the sensory innervation of the alveolar nerves. When a tooth or gingivae is damaged, that region will send pain signals to the brain'. This is a common presentation seen in patients with cavities, cracked teeth, dental abscesses, and oral ulcers.
Other Issues
Since the superior alveolar nerves are branches of the maxillary nerve, and the inferior alveolar nerve is a branch of the mandibular nerve. Any injury to the maxillary nerve, the mandibular nerve, or the trigeminal nerve can result in damage or loss of function in the alveolar nerves.[7][8]
Media
References
Murakami G, Ohtsuka K, Sato I, Moriyama H, Shimada K, Tomita H. The superior alveolar nerves: their topographical relationship and distribution to the maxillary sinus in human adults. Okajimas folia anatomica Japonica. 1994 Mar:70(6):319-28 [PubMed PMID: 8041567]
Toth J, Lappin SL. Anatomy, Head and Neck, Mylohyoid Muscle. StatPearls. 2023 Jan:(): [PubMed PMID: 31424877]
Carter RB,Keen EN, The intramandibular course of the inferior alveolar nerve. Journal of anatomy. 1971 Apr; [PubMed PMID: 5575310]
Ćetković M, Štimec BV, Mucić D, Dožić A, Ćetković D, Reçi V, Çerkezi S, Ćalasan D, Milisavljević M, Bexheti S. Arterial supply of the trigeminal ganglion, a micromorphological study. Folia morphologica. 2020:79(1):58-64. doi: 10.5603/FM.a2019.0062. Epub 2019 Jul 8 [PubMed PMID: 31282551]
Heasman PA. Clinical anatomy of the superior alveolar nerves. The British journal of oral & maxillofacial surgery. 1984 Dec:22(6):439-47 [PubMed PMID: 6239647]
Wolf KT, Brokaw EJ, Bell A, Joy A. Variant Inferior Alveolar Nerves and Implications for Local Anesthesia. Anesthesia progress. 2016 Summer:63(2):84-90. doi: 10.2344/0003-3006-63.2.84. Epub [PubMed PMID: 27269666]
Kang F,Sah MK,Fei G, Determining the risk relationship associated with inferior alveolar nerve injury following removal of mandibular third molar teeth: a systematic review. Journal of stomatology, oral and maxillofacial surgery. 2019 Aug 30; [PubMed PMID: 31476533]
Level 1 (high-level) evidenceShen H, Wang S, Zhi Y, Si J, Shi J. Effects of inferior alveolar nerve rupture on bone remodeling of the mandible: A preliminary study. Medicine. 2019 Aug:98(35):e16897. doi: 10.1097/MD.0000000000016897. Epub [PubMed PMID: 31464921]
Gallesio C, Berrone M, Ruga E, Boffano P. Surgical extraction of impacted inferior third molars at risk for inferior alveolar nerve injury. The Journal of craniofacial surgery. 2010 Nov:21(6):2003-7. doi: 10.1097/SCS.0b013e3181f535b8. Epub [PubMed PMID: 21119486]
Schreiber A, Mattavelli D, Ferrari M, Rampinelli V, Lancini D, Ravanelli M, Bertazzoni G, Rodella LF, Buffoli B, Doglietto F, Nicolai P. Anterior superior alveolar nerve injury after extended endoscopic medial maxillectomy: a preclinical study to predict neurological morbidity. International forum of allergy & rhinology. 2017 Oct:7(10):1014-1021. doi: 10.1002/alr.22001. Epub 2017 Aug 14 [PubMed PMID: 28806496]
Kojima Y, Murouchi T, Akiba M, Oka T. Ultrasound-guided inferior alveolar nerve block for postoperative analgesia after mandibular sequestrectomy: A single-center retrospective study. Journal of clinical anesthesia. 2020 Mar:60():39-40. doi: 10.1016/j.jclinane.2019.08.026. Epub 2019 Aug 20 [PubMed PMID: 31442855]
Level 2 (mid-level) evidence