Introduction
The tongue is a muscular organ formed by a complex arrangement of intrinsic and extrinsic muscles. Generally, the intrinsic muscles change the shape of the tongue, and the extrinsic muscles are in charge of moving it in different directions.[1]
The tongue is principally involved in digestion, taste perception, and speech but also plays an important role in breathing.[1] It is attached via the extrinsic muscles to the hyoid bone, mandible, styloid process, soft palate, and pharynx and divided into two parts by the V-shaped sulcus terminalis. These two parts, an anterior two-thirds and a posterior one-third, are structurally and developmentally distinct. The foramen cecum at the apex of the sulcus terminalis indicates the site of embryonic origin of the thyroglossal duct.[2][3][4]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The area of the tongue posterior to the sulcus terminalis is known as the root or base (posterior one-third of the tongue).[5] The body (anterior two-thirds of the tongue) is the largest part of the tongue and extends from the sulcus terminalis to the frenulum.[5] The body is further subdivided into anterior and posterior. The anterior body is the area below the hard palate, and the posterior body is underneath the soft palate.[5] A collection of nodular lymphatic tissue lies towards the posterior one-third of the tongue and is known as the lingual tonsil.
The tongue's functions mainly include taste, speech, and food manipulation in the oral cavity. It also plays an essential role in breathing.[1]
Taste Functions
Chemicals that interact with the taste buds in the tongue are referred to as "tastants." Taste buds themselves are found within the various papillae of the tongue. Tastants interact with gustatory cell receptors in the taste buds, resulting in the transduction of a taste sensation. The five broad categories of taste receptors are (1) sweet, (2) salty, (3) sour, (4) bitter, and (5) umami.
The taste buds are bulb-shaped structures responsible for taste perception, located within the lingual papillae and in the surface mucosa of the soft palate, oropharynx, epiglottis, and upper esophagus.[6] They are formed by basal cells and thin taste bud cells that converge into the taste pit.[6] The apical protrusions of the taste cells are known as microvilli. Afferent nerve fibers terminals are in contact with the taste buds in their lower third.[6]
The human tongue mainly has three types of gustatory papillae: vallate, fungiform, and filiform.[6] Almost half of the taste buds are located in the vallate papillae.[6]
Vallate papillae, also known as circumvallate papillae, are arranged in a V-shape anterior to the sulcus terminalis and studded with numerous taste buds.[6] The innervation of these papillae is by the glossopharyngeal nerve (CN IX).
Fungiform papillae are mushroom-shaped papillae (thin neck and large head). Filiform papillae are intertwined among them.[6]
Filiform papillae are the most abundant lingual papillae.[7] They are slim, cone-shaped projections distributed evenly on the tongue's surface and responsible for its rough texture. Filiform papillae are mainly involved in mechanical activities; they contain nerve endings that transmit texture, temperature, and pain.[7]
Foliate papillae are vestigial in humans, associated with the lingual tonsils, and located bilaterally on the posterior lateral borders of the tongue.[6]
Speech Functions
Speech is partly produced by manipulating the tongue in the mouth against the teeth and palate. The intrinsic muscles of the tongue are involved primarily in changing the shape of the tongue,[1] which is essential for speaking.
Food Manipulation Functions
The tongue moves the food around the mouth with the help of the buccinator muscle, mixes it with saliva, and helps to separate undesired particles.[5] It also enables the formation of the food bolus in the oral preparatory phase of swallowing. It also takes part in the oral phase of swallowing by elevating and sweeping posteriorly to propel the food bolus past the anterior tonsillar pillar, triggering the swallowing reflex.
Embryology
Tongue development begins in the embryo at approximately four weeks of gestation. Initially, two lateral lingual swellings and one medial swelling, called the tuberculum impar, form from the first pharyngeal arch. A second median swelling, known as the copula or hypobranchial eminence, develops from the mesoderm of the second, third, and fourth pharyngeal arches. A final third median swelling forms from the posterior portion of the fourth arch and develops into the epiglottis. Directly posterior to this swelling is the laryngeal orifice, which is accompanied on either side by the arytenoid swellings.
The lateral lingual swellings increase in size, eventually merging and overlapping the tuberculum impar. The merger of these two swellings forms the anterior two-thirds of the tongue. The mucosa overlying this part of the tongue originates from the first arch; thus, the sensory innervation to this area is from the mandibular branch of the trigeminal nerve (CN V3). Meanwhile, the second, third, and fourth portions of the pharyngeal arch, which make up the copula, develop into the posterior one-third of the tongue. The mucosa overlying this part of the tongue has sensory innervation from the glossopharyngeal nerve (CN IX), which is a sign that the third arch overlaps that of the second. The third arch derivatives typically are associated with glossopharyngeal sensory innervation.
The epiglottis and epiglottic region of the tongue develop from the third median swelling, which arises from the posterior fourth pharyngeal arch. Innervation of this region is by the superior laryngeal nerve, which reflects its development from the fourth pharyngeal arch.
The muscles of the tongue predominantly derive from myoblasts that originate in occipital somites and thus are innervated by the hypoglossal nerve (CN XII).
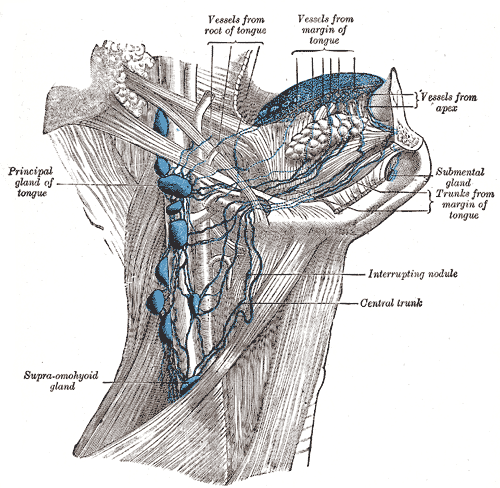
Blood Supply and Lymphatics
Blood supply to the tongue comes predominantly from the lingual artery, a branch of the external carotid artery.[8] Venous drainage is done by the lingual vein.
The lingual artery arises from the external carotid artery at the tip of the hyoid bone's greater horn, between the facial and superior thyroid arteries.[9][8] After branching from the external carotid artery, the lingual artery passes deep to the hyoglossus muscle and superficial to the middle pharyngeal constrictor muscle. It then gives rise to the following four arteries:
- The suprahyoid artery supplies the omohyoid, sternothyroid, and thyrohyoid muscles. They anastomose with the corresponding vessels from the opposite side.
- The dorsal lingual artery arises beneath the hyoglossus muscle and passes to the posterior part of the dorsum of the tongue. It supplies the mucous membrane of this region as well as the glossopalatine arch, lingual tonsils, soft palate, and epiglottis.[9] They anastomose with their corresponding vessels on the opposite side.
- The sublingual artery branches at the anterior border of the hyoglossus muscle before passing between the genioglossus muscle and mylohyoid muscle to the sublingual gland. It supplies the sublingual gland before giving branches to the mylohyoid muscle.[9] It also provides blood supply to the genioglossus, geniohyoid, and the gingival mucosa of the mandible.[9] One branch from the sublingual artery passes posterior to the alveolar process of the mandible and anastomoses with the corresponding artery from the other side. A second branch of the sublingual artery pierces the mylohyoid muscle and anastomoses with the submental branch of the facial artery.
- The deep lingual artery, which is the termination of the lingual artery, passes between the genioglossus muscle and inferior longitudinal muscle, supplying the apex of the tongue.[9]
The lymphatic vessels from the body of the tongue are divided into marginal and central. The marginal vessels drain the tongue's apex, marginal surface, and sublingual region into the submental and submandibular nodes.[10] Less often, they drain into the jugulodigastric or jugulo-omohyoid nodes. The central vessels are located at the tip of the tongue, travel through the mylohyoid muscle, and drain into the jugulo-omohyoid or jugulodigastric nodes.[10]
The dorsal vessels collect lymphatic drainage from the area posterior to the sulcus and drain into the jugulo-omohyoid and jugulodigastric nodes.
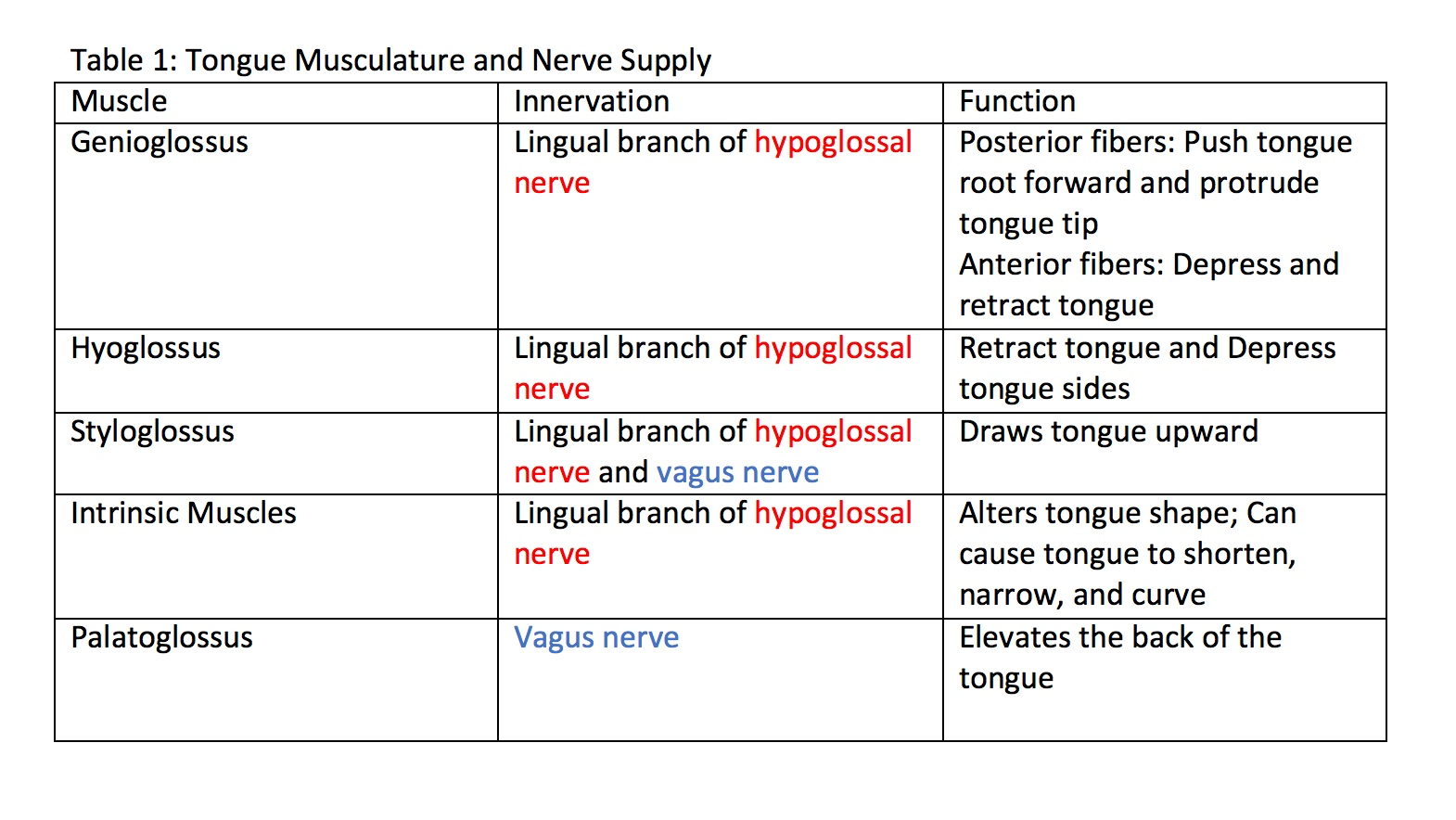
Nerves
The hypoglossal nerve (CN XII) provides motor innervation to all of the intrinsic and extrinsic muscles of the tongue except for the palatoglossus muscle, which is innervated by the vagus nerve (CN X).[11][12] It runs superficial to the hyoglossus muscle. Lesions of the hypoglossal nerve cause deviation of the tongue to the ipsilateral (i.e., damaged) side.
Taste to the anterior two-thirds of the tongue is achieved through innervation from the chorda tympani nerve, a branch of the facial nerve (CN VII).[13] General sensation to the anterior two-thirds of the tongue is by innervation from the lingual nerve, a branch of the mandibular branch of the trigeminal nerve (CN V3).[14] The lingual nerve is located deep and medial to the hyoglossus muscle and is associated with the submandibular ganglion.
On the other hand, taste perception in the posterior third of the tongue is accomplished through innervation from the glossopharyngeal nerve (CN IX), which also provides general sensation to the posterior one-third of the tongue.[15][16] Taste perception also is performed by both the epiglottis and the epiglottic region of the tongue, which receives taste and general sensation from innervation by the internal laryngeal branch of the vagus nerve (CN X).[17] Damage to the vagus nerve (CN X) causes contralateral deviation (away from the injured side) of the uvula.
Muscles
The tongue is formed by eight paired muscles: four intrinsic and four extrinsic. The intrinsic muscles' most particular feature is that they have no insertions in bone - they arise and insert within the tongue.[5] By contrast, the extrinsic muscles do attach to osseous structures: either the hyoid bone, mandible, or styloid process.[5]
The muscles of the tongue are separated and surrounded by connective tissue structures, named median septum, paramedian septum, and lateral septum.[5] The median septum is in the midline of the tongue and gives rise to the transverse muscles; the paramedian septum separates the inferior longitudinal muscle from the genioglossus muscle. The lateral septum surrounds the inferior longitudinal muscle.[5]
Intrinsic Muscles Of The Tongue
The Superior Longitudinal Muscle
The superior longitudinal muscle is located immediately underneath the mucosa of the dorsal surface of the tongue [5] and is superior to the transverse and vertical muscles.[11] Although usually depicted as a slim muscle, it is thick in the center and thinners in its periphery.[11]
If the superior longitudinal muscle contracts in insolation, the tongue shortens and, therefore, widens. It also participates in the dorsiflexion of the tip of the tongue.[5]
The Inferior Longitudinal Muscle
The inferior longitudinal muscle is a thin and oval in cross-section muscle.[11] It lies between the paramedian septum and the lateral septum.[11] The fibers of the inferior longitudinal muscle join the anterior fibers of the hyoglossus, genioglossus, and styloglossus muscles, forming the ventral area of the tip of the tongue.[11]
Similar to the superior longitudinal muscle, contraction of the inferior longitudinal muscle results in shortening and thickening of the tongue.[5] It also participates in the ventroflexion of the tip of the tongue.[5]
The Transverse Muscle
The transverse muscles extend laterally from the median septum and more anteriorly and posteriorly when compared to the vertical muscles.[5]
Contraction of the transverse muscles lengthens and thinners the tongue.[5]
The Vertical Muscle
The vertical muscle is formed by fibers arranged almost in a vertical direction, which intersect with fibers running transversally (transverse muscle fibers).[11]
The contraction of the vertical muscle flattens the tongue: simultaneous widening and elongation.[5]
Extrinsic Muscles Of The Tongue
The Genioglossus Muscle
The genioglossus is a large, fan-shaped muscle that makes up the thickness of the tongue posteriorly.[11] Its insertion into the midline of the dorsum of the tongue creates the typical concave shape important for speech and swallowing functions.[5]
The genioglossus muscle originates from the inner surface of the mandible, more specifically from the superior mental spine of the symphysis menti. From here, it extends posteriorly within the tongue, from the root to the tip.[11] Its bony attachment is in the body of the hyoid bone.
Contraction of the genioglossus muscle protrudes the tongue.[5] The muscle's horizontal and oblique (posterior fascicles) compartments are believed to be responsible for this action.[5]
In addition, the genioglossus muscle is believed to be involved in the depression of the body of the tongue, ventroflexion, and probably, retrusion of the tip of the tongue.[5]
The Styloglossus Muscle
The styloglossus muscle arises from the styloid process (a thin bony projection of the temporal bone) and stylomandibular ligament.[5]
The styloglossus is more lateral than the other tongue muscles. Its contraction results in retrusion of the tongue; it also elevates the tongue's lateral margin.[5]
The Hyoglossus Muscle
The hyoglossus muscle has a quadrangular shape in its lower two-thirds and a fan shape in its upper third.[11] It originates from the lateral region of the anterior aspect of the body of the hyoid bone.[11]
Contraction of the hyoglossus muscle results in retrusion and depression of the tongue's lateral margin.[11]
The Palatoglossus Muscle (Glossopharyngeal Muscle)
It is the only extrinsic muscle of the tongue that is not innervated by the hypoglossal nerve but by the vagus nerve (CN X).[12] Contraction of the palatoglossus muscle elevates the posterior tongue, closes the oropharyngeal isthmus, aids in the initiation of swallowing, and prevents the spill of saliva from the vestibule into the oropharynx by maintaining the palatoglossal arch.
It originates from the anterior region of the soft palate, extends inferiorly, forms the palatopharyngeal arch, and inserts into the tongue's lateral borders.[5]
In Summary
Intrinsic Muscles
- The superior longitudinal muscle shortens and widens the tongue and curls it upward (dorsiflexion).
- The inferior longitudinal muscle shortens and widens the tongue and curls it downward (ventroflexion).
- The transverse muscle elongates and narrows the tongue.
- The vertical muscle flattens the tongue.
Extrinsic Muscles
- The genioglossus muscle protrudes the tongue.
- The styloglossus muscle retrudes the tongue and elevates its lateral margins.
- The hyoglossus muscle retrudes the tongue and depresses its lateral margins.
- The palatoglossus muscle elevates the posterior tongue, closes the oropharyngeal isthmus, aids in the initiation of swallowing, and prevents the spill of saliva from the vestibule into the oropharynx by maintaining the palatoglossal arch.
Surgical Considerations
Thyroglossal duct cysts can develop when there is a remnant at the point of embryologic origin of the thyroid gland, the foramen cecum. The thyroid gland begins to develop on the floor of the embryologic pharynx at the point called the foramen cecum, which is located at the dorsum of the posterior tongue. The developing gland then relocates to its ultimate destination in the anterior neck by migrating down the thyroglossal duct anterior to the hyoid and thyroid cartilages before stopping anterolateral to the superior aspect of the trachea.
The thyroglossal duct ordinarily disappears, but remnants of its epithelium may remain, allowing for the potential development of a thyroglossal duct cyst in this area. These cysts generally occur in the neck, close to or inferior to the body of the hyoid bone. They form a swelling at the anterior midline of the neck that is painless, fluctuant, and moves upon swallowing. Thyroglossal duct cysts are typically removed surgically.[18][19]
Clinical Significance
Ankyloglossia
Ankyloglossia, also known as tongue tie, refers to a short lingual frenulum, which limits the movement of the tongue and may affect speaking, eating, and swallowing.[20] In the most common form of ankyloglossia, the frenulum extends to the tip of the tongue. Ankyloglossia can be corrected by surgically severing the lingual frenulum.[21][22]
Fissured tongue
Also known as a scrotal or plicated tongue, it occurs when several small furrows form on the dorsal surface of the tongue. It can be an oral manifestation of psoriasis. It is generally painless and benign and is often associated with other syndromes, e.g., Down syndrome.[23]
Geographic tongue
A geographic tongue, also known as benign migratory glossitis, is a benign, asymptomatic condition characterized by large red patches with a greyish-white border covering the dorsum of an otherwise normal tongue. It is caused by inflammation of the mucous membrane of the tongue, which results in the loss of lingual papillae. The lesions are known to migrate over time. The name arises from the map-like appearance of the tongue in this condition.[24][25]
Obstruction Of The Airway
The tongue tends to fall posteriorly, thus obstructing the airway. Paralysis or total relaxation of the genioglossus muscle presents a risk of suffocation, which can occur during general anesthesia. An artificial airway is made using intubation, which prevents the tongue from falling backward and blocking the airway.
Ludwig angina infection, once established, evolves to include the tongue. The tongue may enlarge to two or three times its usual size and tends to distend posteriorly into the hypopharynx, superiorly against the palate, and anteriorly out of the oral cavity. Any immediate posterior extension of this process will ultimately involve the epiglottis. The styloglossus muscle creates the connection between the submandibular parapharyngeal spaces, otherwise known as the buccopharyngeal gap, as it leaves the tongue and passes in between the middle and superior constrictor muscles before attaching to the styloid process. Cellulitis of the submandibular space may spread into the pharyngeal space and, from there, into the retropharyngeal space of the mediastinum.
The tongue plays a major role in breathing; as such, it is involved in the collapse of the upper airway in obstructive sleep apnoea syndrome patients.[1]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)

Arteries and Veins of the Tongue. Internal jugular vein, dorsalis linguae artery, lingual vein, veins of dorsum of tongue, and hypoglossal nerve.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Kajee Y, Pelteret JP, Reddy BD. The biomechanics of the human tongue. International journal for numerical methods in biomedical engineering. 2013 Apr:29(4):492-514. doi: 10.1002/cnm.2531. Epub 2013 Jan 14 [PubMed PMID: 23319169]
Mills N, Pransky SM, Geddes DT, Mirjalili SA. What is a tongue tie? Defining the anatomy of the in-situ lingual frenulum. Clinical anatomy (New York, N.Y.). 2019 Sep:32(6):749-761. doi: 10.1002/ca.23343. Epub 2019 Feb 19 [PubMed PMID: 30701608]
Alaoui F, Souissi A, Jendoubi F, Mokni M. Caviar tongue: A lingual physiological variation. Presse medicale (Paris, France : 1983). 2018 Oct:47(10):925-926. doi: 10.1016/j.lpm.2018.06.010. Epub 2018 Sep 11 [PubMed PMID: 30217364]
Hamad Y, Warren DK. Black Hairy Tongue. The New England journal of medicine. 2018 Sep 6:379(10):e16. doi: 10.1056/NEJMicm1800351. Epub [PubMed PMID: 30184449]
Sanders I, Mu L. A three-dimensional atlas of human tongue muscles. Anatomical record (Hoboken, N.J. : 2007). 2013 Jul:296(7):1102-14. doi: 10.1002/ar.22711. Epub 2013 May 6 [PubMed PMID: 23650264]
Witt M. Anatomy and development of the human taste system. Handbook of clinical neurology. 2019:164():147-171. doi: 10.1016/B978-0-444-63855-7.00010-1. Epub [PubMed PMID: 31604544]
Gravina SA, Yep GL, Khan M. Human biology of taste. Annals of Saudi medicine. 2013 May-Jun:33(3):217-22. doi: 10.5144/0256-4947.2013.217. Epub [PubMed PMID: 23793421]
Level 3 (low-level) evidenceLettau J, Bordoni B. Anatomy, Head and Neck, Lingual Artery. StatPearls. 2023 Jan:(): [PubMed PMID: 32119400]
Buffoli B, Verzeletti V, Rezzani R, Rodella LF. Unusual branch of the lingual artery supplies the infrahyoid muscles. Anatomical science international. 2020 Jan:95(1):153-155. doi: 10.1007/s12565-019-00501-6. Epub 2019 Aug 23 [PubMed PMID: 31444702]
Gvetadze SR, Ilkaev KD. Lingual lymph nodes: Anatomy, clinical considerations, and oncological significance. World journal of clinical oncology. 2020 Jun 24:11(6):337-347. doi: 10.5306/wjco.v11.i6.337. Epub [PubMed PMID: 32874949]
Abd-El-Malek S. Observations on the morphology of the human tongue. Journal of anatomy. 1939 Jan:73(Pt 2):201-210.3 [PubMed PMID: 17104752]
Walker HK, Hall WD, Hurst JW, Walker HK. Cranial Nerves IX and X: The Glossopharyngeal and Vagus Nerves. Clinical Methods: The History, Physical, and Laboratory Examinations. 1990:(): [PubMed PMID: 21250227]
Rinaldi V, Cappadona M, Gaffuri M, Torretta S, Pignataro L. Chorda tympani nerve, may it have a role in stabilizing middle ear pressure? Medical hypotheses. 2013 Jun:80(6):726-7. doi: 10.1016/j.mehy.2013.02.021. Epub 2013 Mar 21 [PubMed PMID: 23523289]
Fagan SE, Roy W. Anatomy, Head and Neck, Lingual Nerve. StatPearls. 2023 Jan:(): [PubMed PMID: 31536258]
Simon E, Mertens P. [Functional anatomy of the glossopharyngeal, vagus, accessory and hypoglossal cranial nerves]. Neuro-Chirurgie. 2009 Apr:55(2):132-5. doi: 10.1016/j.neuchi.2009.01.018. Epub 2009 Mar 21 [PubMed PMID: 19304301]
Mansour Y, Kulesza R. A rare variation of the glossopharyngeal nerve. Anatomy & cell biology. 2021 Jun 30:54(2):285-288. doi: 10.5115/acb.21.005. Epub [PubMed PMID: 33850061]
Heckmann JG, Heckmann SM, Lang CJ, Hummel T. Neurological aspects of taste disorders. Archives of neurology. 2003 May:60(5):667-71 [PubMed PMID: 12756129]
Pitner H, Elmaraghy C, Fischer B, Onwuka A, Rabe A, Walz P. Diagnostic Accuracy of Midline Pediatric Neck Masses. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2019 Jun:160(6):1111-1117. doi: 10.1177/0194599819827845. Epub 2019 Feb 5 [PubMed PMID: 30717638]
Amos J, Shermetaro C. Thyroglossal Duct Cyst. StatPearls. 2023 Jan:(): [PubMed PMID: 30085599]
Suter VG, Bornstein MM. Ankyloglossia: facts and myths in diagnosis and treatment. Journal of periodontology. 2009 Aug:80(8):1204-19. doi: 10.1902/jop.2009.090086. Epub [PubMed PMID: 19656020]
Madani FM, Kuperstein AS. Normal variations of oral anatomy and common oral soft tissue lesions: evaluation and management. The Medical clinics of North America. 2014 Nov:98(6):1281-98. doi: 10.1016/j.mcna.2014.08.004. Epub 2014 Sep 22 [PubMed PMID: 25443677]
Kapoor P. The Tongue Tie: Untied. Indian pediatrics. 2018 Oct 15:55(10):917 [PubMed PMID: 30426963]
Pei Y, Beaman GM, Mansfield D, Clayton-Smith J, Stewart M, Newman WG. Clinical and genetic heterogeneity in Melkersson-Rosenthal Syndrome. European journal of medical genetics. 2019 Jun:62(6):103536. doi: 10.1016/j.ejmg.2018.09.003. Epub 2018 Sep 11 [PubMed PMID: 30217753]
Bett JVS, Batistella EÂ, Melo G, Munhoz EA, Silva CAB, Guerra ENDS, Porporatti AL, De Luca Canto G. Prevalence of oral mucosal disorders during pregnancy: A systematic review and meta-analysis. Journal of oral pathology & medicine : official publication of the International Association of Oral Pathologists and the American Academy of Oral Pathology. 2019 Apr:48(4):270-277. doi: 10.1111/jop.12831. Epub 2019 Feb 12 [PubMed PMID: 30673134]
Level 1 (high-level) evidenceS Kurtipek G, Sarı N, T Akyürek F. Geographic tongue that responds to the treatment of pregabalin: Can it be a new treatment choice? Dermatologic therapy. 2019 Jan:32(1):e12776. doi: 10.1111/dth.12776. Epub 2018 Nov 18 [PubMed PMID: 30365234]