Introduction
Stellate ganglion block (SGB) is used for the treatment of many medical conditions including complex regional pain syndrome and peripheral vascular disease. Historically, the anesthetic has been injected at the C6 or C7 vertebral level with the Chassignac’s tubercle, the cricoid cartilage, and the carotid artery serving as the anatomic landmarks to the procedure. Due to a high risk of side effects, for example, pneumothorax and vascular puncture, an image-guided approach is strongly suggested, even with the "safer" C6 approach.[1]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The sympathetic fibers for the head, neck, heart, and superior limbs arise from the first thoracic segments, ascend through the sympathetic chain, and synapse in the superior, middle, and inferior cervical ganglions. The stellate ganglion is present in 80% of the general population and is composed of the inferior cervical ganglion and the first thoracic ganglion fusion. It lies anterior to the neck of the first rib and extends to the inferior aspect of the transverse process of C7. Usually, it is located medial or posterior to the vertebral artery close to the dome of the pleura.
- If the inferior cervical ganglion and first thoracic ganglion are not fused, the stellate ganglion refers to the inferior cervical ganglion located adjacent to the anterior C7 tubercle.
- The preganglionic fibers of the stellate ganglion continue to travel through the cervical sympathetic chain, and the postganglionic fibers provide the sympathetic innervation of the upper limbs.
- SGB with local anesthetic exert their effect both on preganglionic and postganglionic fibers[2]
Indications
The pain relieved by sympathetic block is classified as sympathetically mediated pain (SMP) that consists of abnormal connections between sympathetic and sensory nervous systems.
The therapeutic effects of SGB are due to the block in neural connections in its region of innervation, the improvement in the blood supply of the region, the reduction of adrenal hormones plasma concentration. SGB can be used in medical conditions like post-traumatic stress disorder or a cluster headache based on its sedative effect. SGB can be used as a diagnostic tool to confirm an SMP.[3][4][5]
- Complex regional pain syndrome of the head and upper limbs
- Peripheral vascular disease
- Upper extremity embolism
- Postherpetic neuralgia
- Chronic post-surgical pain
- Hyperhidrosis
- Raynaud disease
- Scleroderma
- Orofacial pain
- Phantom limb
- Atypical chest pain
- A cluster or a vascular headache
- Post-traumatic stress disorder
- Meniere syndrome
- Intractable angina
- Refractory cardiac arrhythmias
Contraindications
Equipment
Fluoroscopic Technique
- C-arm image intensifier
- Contrast media
- 22-gauge spinal needle (9 cm length)
- Local anesthetic
- Non-particulate steroid[2]
Ultrasound-Guided Technique
- High frequency (6 to 13 MHz) linear transducer
- 22 to 25 gauge echo-enhanced needle
- Local anesthetic
- Non-particulate steroid[6]
Personnel
SGB requires a trained pain physician as it is a procedure of intermediate difficulty. A nurse is required to assist the patient during the injection for positioning. If the fluoroscopic technique is used, the assistance of a radiology technician is needed.[7]
Preparation
The patient's vital signs should be monitored before and immediately following the procedure. A peripheral venous catheter should be placed in all patients. It is important to obtain a detailed medical history before the procedure to rule out any contraindications and evaluate the risk/benefits ratio.[2]
Technique or Treatment
Ultrasound-Guided Technique
The patient is supine with the neck slightly extended and the head slightly rotated contralaterally to the approached side. The site is cleaned and draped, and the transducer is placed perpendicular to the tracheal axis at the cricoid cartilage and is moved inferiorly until the superior aspect of the thyroid gland is visualized. Later, the transducer should be relocated laterally to visualize the anterior aspect of the Chassaignac’s tubercle on the C6 transverse process. The carotid artery, internal jugular vein, thyroid gland, trachea, Longus colli, and Longus capitis muscle, prevertebral fascia, the root of C6 spinal nerve, and transverse process of C6 can be identified (see Figure 1). Color Doppler should be used to detect the position of the vessels. With an in-plane approach, the needle is placed beside the trachea with a lateral to medial direction. The tip must reach the prevertebral fascia of the Longus colli muscle located between the posterior aspect of the carotid artery and the tip of the C6 anterior tubercle. Injury to vessels and nerves should be avoided. An aspiration test must be done to avoid the suction of blood or cerebrospinal fluid, then a local anesthetic is injected, and the diffusion of the injectate is seen in real-time. The injection is suggested not inferior to the C6 level because the vertebral artery is left unprotected at the C7 level due to its absent or rudimentary anterior tubercle. Five milliliters of a local anesthetic such as lidocaine 2% is injected until the fluid spread along the paravertebral fascia to the stellate ganglion.[8][9][6][10]
Fluoroscopic-Guided Technique
The patient is placed in a supine position, and an anteroposterior view is obtained with the C-arm to identify C6 by counting up from T1. Then the C-arm is tilted to line up the superior aspect of the C6 vertebral body and is rotated obliquely at approximatively 25 to 30 degrees ipsilaterally to obtain a foraminal view. The target is the junction of the vertebral body and the uncinate process (of C6). Under an oblique view, the needle is inserted laterally with a lateral to medial trajectory and remains over the vertebral body or slightly medial to avoid injury to vessels, spinal nerves, and disc. The position needs to be checked through the anteroposterior and lateral views. A small amount of contrast media (0.5 to 1 ml) can be injected first to localize the needle. A tiny test dose of local anesthetic is then administered to reduce the risk of intravascular injection further. Then 10 ml of a local anesthetic such as lidocaine 1% is injected. The same procedure can be performed at the C7 level if needed, but the physicians must be aware of the higher risks of vascular puncture at the C7 level.[2]
Complications
- Vascular puncture (carotid artery, internal jugular vein, inferior thyroid artery, vertebral artery)
- Neural puncture (vagus nerve, recurrent nerve, brachial plexus roots)
- Pneumothorax
- Thyroid injury
- Esophageal and tracheal puncture
- Transient Horner syndrome
- Intravascular injection
- Neuraxial, phrenic nerve or brachial plexus spread of local anesthetic
- Infections[3][4][5]
Clinical Significance
A sympathetic block as SGB can be useful in the diagnosis and treatment of SMP in the upper limb, head, and neck regions; it can also be used in the treatment of medical conditions as post-traumatic stress disorder, cluster headache, or intractable angina.[11][12][13][3][4][5]
Enhancing Healthcare Team Outcomes
Stellate ganglion blockade should only be performed by professionals with knowledge of the anatomy and how to manage the complications. The procedure should be done under fluoroscopic guidance to minimize complications. A nurse should be dedicated to monitoring the patient vital signs continuously. At the end of the procedure, a chest x-ray should be obtained and a gross neurological exam should be performed.
Media
(Click Image to Enlarge)
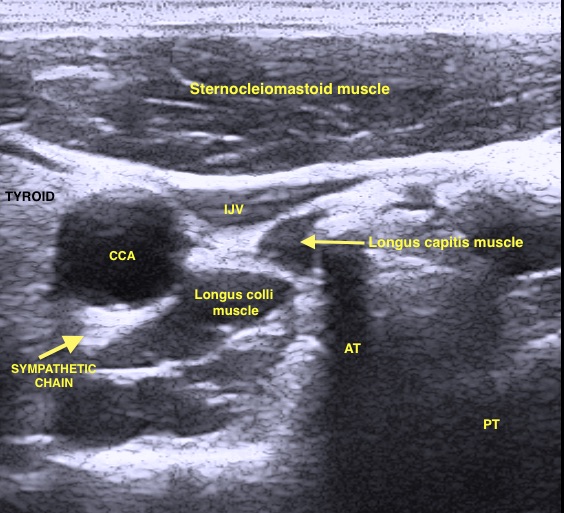
Sonographic visualisation of sympathetic chain at C6 vertebral level. You can appreciate posterior (PT) and anterior (AT) tubercle of C6 transverse process. You can see also carotid artery (CCA) and internal jugular vein (IJV) partially compressed by probe pressure. Muscles and tyroid and muscles position is clearly evidenced. Contributed by Emanuele Piraccini MD and Giulia Biondi MD
References
McLean B. Safety and Patient Acceptability of Stellate Ganglion Blockade as a Treatment Adjunct for Combat-Related Post-Traumatic Stress Disorder: A Quality Assurance Initiative. Cureus. 2015 Sep 10:7(9):e320. doi: 10.7759/cureus.320. Epub 2015 Sep 10 [PubMed PMID: 26487996]
Level 2 (mid-level) evidenceWang D. Image Guidance Technologies for Interventional Pain Procedures: Ultrasound, Fluoroscopy, and CT. Current pain and headache reports. 2018 Jan 26:22(1):6. doi: 10.1007/s11916-018-0660-1. Epub 2018 Jan 26 [PubMed PMID: 29374352]
Duong S, Bravo D, Todd KJ, Finlayson RJ, Tran Q. Treatment of complex regional pain syndrome: an updated systematic review and narrative synthesis. Canadian journal of anaesthesia = Journal canadien d'anesthesie. 2018 Jun:65(6):658-684. doi: 10.1007/s12630-018-1091-5. Epub 2018 Feb 28 [PubMed PMID: 29492826]
Level 1 (high-level) evidenceGunduz OH, Kenis-Coskun O. Ganglion blocks as a treatment of pain: current perspectives. Journal of pain research. 2017:10():2815-2826. doi: 10.2147/JPR.S134775. Epub 2017 Dec 14 [PubMed PMID: 29276402]
Level 3 (low-level) evidenceDatta R, Agrawal J, Sharma A, Rathore VS, Datta S. A study of the efficacy of stellate ganglion blocks in complex regional pain syndromes of the upper body. Journal of anaesthesiology, clinical pharmacology. 2017 Oct-Dec:33(4):534-540. doi: 10.4103/joacp.JOACP_326_16. Epub [PubMed PMID: 29416250]
Narouze S. Ultrasound-guided stellate ganglion block: safety and efficacy. Current pain and headache reports. 2014 Jun:18(6):424. doi: 10.1007/s11916-014-0424-5. Epub [PubMed PMID: 24760493]
Imani F, Hemati K, Rahimzadeh P, Kazemi MR, Hejazian K. Effectiveness of Stellate Ganglion Block Under Fuoroscopy or Ultrasound Guidance in Upper Extremity CRPS. Journal of clinical and diagnostic research : JCDR. 2016 Jan:10(1):UC09-12. doi: 10.7860/JCDR/2016/14476.7035. Epub 2016 Jan 1 [PubMed PMID: 26894152]
Chang KV, Lin CP, Hung CY, Özçakar L, Wang TG, Chen WS. Sonographic Nerve Tracking in the Cervical Region: A Pictorial Essay and Video Demonstration. American journal of physical medicine & rehabilitation. 2016 Nov:95(11):862-870 [PubMed PMID: 27362696]
Bhatia A, Flamer D, Peng PW. Evaluation of sonoanatomy relevant to performing stellate ganglion blocks using anterior and lateral simulated approaches: an observational study. Canadian journal of anaesthesia = Journal canadien d'anesthesie. 2012 Nov:59(11):1040-7. doi: 10.1007/s12630-012-9779-4. Epub 2012 Sep 6 [PubMed PMID: 22956268]
Level 2 (mid-level) evidenceChang KV, Wu WT, Özçakar L. Ultrasound-Guided Interventions of the Cervical Spine and Nerves. Physical medicine and rehabilitation clinics of North America. 2018 Feb:29(1):93-103. doi: 10.1016/j.pmr.2017.08.008. Epub 2017 Oct 7 [PubMed PMID: 29173667]
Peterson K, Bourne D, Anderson J, Mackey K, Helfand M. Evidence Brief: Effectiveness of Stellate Ganglion Block for Treatment of Posttraumatic Stress Disorder (PTSD). 2017 Feb:(): [PubMed PMID: 28742302]
Wei K, Feldmann RE Jr, Brascher AK, Benrath J. Ultrasound-guided stellate ganglion blocks combined with pharmacological and occupational therapy in Complex Regional Pain Syndrome (CRPS): a pilot case series ad interim. Pain medicine (Malden, Mass.). 2014 Dec:15(12):2120-7. doi: 10.1111/pme.12473. Epub [PubMed PMID: 25537318]
Level 3 (low-level) evidenceMulvaney SW, Lynch JH, Hickey MJ, Rahman-Rawlins T, Schroeder M, Kane S, Lipov E. Stellate ganglion block used to treat symptoms associated with combat-related post-traumatic stress disorder: a case series of 166 patients. Military medicine. 2014 Oct:179(10):1133-40. doi: 10.7205/MILMED-D-14-00151. Epub [PubMed PMID: 25269132]
Level 2 (mid-level) evidence