Introduction
The superior vena cava (SVC) is a large, significant vein responsible for returning deoxygenated blood collected from the body to the right atrium. It is present within the superior and middle mediastinum. The superior vena cava handles the venous return of blood from structures located superior to the diaphragm. In contrast, its counterpart, the inferior vena cava, handles venous return from the portion of the body inferior to the diaphragm. The impedance of flow in the superior vena cava by thrombosis or external compression can cause hemodynamic compromise depending on the severity and acuity of the obstruction.[1]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The right and left brachiocephalic veins, also known as the innominate veins, join to form the superior vena cava posterior to the inferior border of the first right costal cartilage. These veins carry blood from the chest wall, esophagus, lungs, neck, and pericardium. The superior vena cava descends downwards vertically, running posterior to the second and third intercostal spaces. At the level of the right second costal cartilage, the SVC receives the azygos vein via the azygos arch, having looped over the right lung hilum from posterior to anterior to reach the SVC.[2] At this point, the superior vena cava also penetrates the fibrous pericardium and continues within it until its termination.
Within the superior mediastinum, the superior vena cava is related to the parietal pleura of the right lung. The right phrenic nerve runs directly laterally along its surface, and the right vagus nerve descends with the trachea posteromedially to the SVC.[3][4] The right lung root is directly posterior.
The SVC drains into the right atrium at the level of the third costal cartilage via a valveless orifice at the superior part of the sinus venarum, a smooth part of the posterior wall of the right atrium. The superior vena cava terminates in the superior portion of the sinus venarum, a quadrangular smooth-walled space posterior to the crista terminalis that receives both the superior and inferior vena cava.[5] The orifice of the SVC lies directly posterolateral to the auricle of the right atrium.
In adults, the superior vena cava is 7 cm long and approximately 2 cm wide. In developing children, studies have shown that the superior vena cava's size most closely corresponds with the child's height, reaching adult dimensions at approximately 10 to 12 years of age.[6][7]
Embryology
The superior vena cava derives from the proximal portion of the right anterior cardinal vein and the right common cardinal vein at a point that is caudal to the transverse anastomosis in the embryo. During week eight of development, a large anastomosis formed via the thymic and thyroid veins shunts blood from the left anterior cardinal vein towards the right.[8] Superior to this anastomosis, the anterior cardinal veins become the internal jugular veins. The cardinal veins are responsible for venous return; they represent the primary drainage system during embryonic development. The anterior cardinal veins drain the cephalic portion of the embryo, while the posterior cardinal veins drain the remaining embryonic blood. The anterior and posterior cardinal veins merge before entering the sinus venosus.[9]
At this point, they become the short common cardinal veins. The right brachiocephalic vein forms from the right anterior cardinal vein at a point that is cranial to the transverse anastomosis. The left brachiocephalic vein forms from a portion of the left anterior cardinal vein and transverse intercardinal anastomosis. During embryonic development, several malformations may occur, including left superior vena cava, double superior vena cava, as well as improper pulmonary venous drainage into the super vena cava.[9]
Blood Supply and Lymphatics
The right and left brachiocephalic, or innominate, veins converge to form the superior vena cava at the level of the right first costal cartilage. These veins form at the venous angle from the subclavian and jugular veins merging posteriorly to the sternoclavicular joints. The brachiocephalic veins carry deoxygenated blood returning to the heart from the pericardium, lungs, esophagus, chest wall, and neck. The left brachiocephalic vein is more horizontal in its orientation and is longer than the more vertical and shorter right brachiocephalic vein. The right brachiocephalic vein is approximately 2 to 3 cm long and sits anterior to the innominate artery. The left brachiocephalic vein is approximately 6 cm long and lies anterior to the left subclavian vein and common carotid arteries, posterior to the manubrium, and superior to the aortic arch. The left superior intercostal vein joins with the left brachiocephalic vein; the azygos vein joins with the right brachiocephalic vein. The vertebral, internal thoracic, and inferior thyroid veins are all tributaries of the brachiocephalic veins.[7]
The azygos vein is another vein that drains into the superior vena cava. This vein is unpaired. It runs along the right aspect of the thoracic vertebral column and enters into the thorax at the aortic hiatus of the diaphragm. The azygos vein forms from the joining of the right subcostal and ascending lumbar veins. The hemiazygos veins, bronchial veins, pericardial veins, esophageal veins, and posterior right intercostal veins all drain into the azygos vein.[2]
Nerves
Sympathetic axons originating from the right stellate ganglion descend along the superior vena cava. Most of these axons travel to the posterior surface of the heart. However, some extend onto the anterior side of the heart. These axons provide sympathetic innervation for the sinoatrial node. Cardiac parasympathetic nerves also run along the length of the superior vena cava. Efferent vagal nerve fibers travel through a pad of fat located in between the proximal aorta and medial superior vena cava.[10][11][12]
Muscles
As with other arteries and veins, the superior vena cava is made up of three total layers of muscle. The innermost endothelial lining of the superior vena cava is known as the tunica intima. The middle layer, comprised of smooth muscle tissue, is known as the tunica media. This is the layer that receives input from the nervous system. The outermost layer is the tunica adventitia. It consists of collagen and elastic connective tissue. This outmost layer is primarily responsible for the superior vena cava’s flexibility.[13]
Physiologic Variants
Persistent Left Superior Vena Cava (PLSVC)
PLSVC is the anomalous presence of a persistent embryological left anterior cardinal vein that remains as a left superior vena cava and is present in approximately 0.3% of the population.[14] In patients with congenital heart disease, its prevalence is increased, up to 10%.[15] However, this anomaly may be undetected throughout life or only be diagnosed during cardiac investigation or intervention. When the PLSVC drains aberrantly into the left atrium, this can also be asymptomatic but, if causing significant right to left cardiac shunting, may present with cyanosis, respiratory distress, and progressive fatigue.[16]
Double Superior Vena Cava
Double superior vena cava, or SVC duplication, is the commonest subset of PLSVC in which there remains a morphologically normal right superior vena cava to accompany the left superior vena cava.[17] For this reason, given that the right superior vena cava will have normal drainage into the right atrium, it is even more likely to not be symptomatic during life and be identified only incidentally.[18][19]
Surgical Considerations
Obstruction of the superior vena cava from a mediastinal mass or thrombus may require surgical intervention. Trauma to the thoracic region, damage from long-term central line catheterization, or damage from chronic use of pacing electrodes can also result in a need for surgical repair of the superior vena cava.[6] Great care is necessary when clamping off the superior vena cava for surgical repair, as venous return from the head and neck will be impaired under these circumstances, and such impairment could potentially lead to poor patient outcomes.[20] Access to the superior vena cava for open surgical bypass of obstruction can be achieved through a combination of a right neck incision and median sternotomy.[21]
Clinical Significance
Complete or partial obstruction of the superior vena cava can occur, resulting in a condition known as superior vena cava syndrome. Causes of the obstruction may include intrinsic stenosis, extrinsic compression, or thrombosis of the vein. Malignancy is the single most common cause, with cancer of the lung, lymphoma, or metastatic cancers resulting in the majority of superior vena cava obstructions.[22]
The clinical presentation of superior vena cava syndrome may vary widely and depends on a variety of factors, including the severity, speed, and location of the obstruction. Patients with a slowly developing obstruction may show few or no symptoms, as collateral veins from the azygos system compensate to some degree.[23] The location of these collateral channels depends upon the location of the blockage. If the obstruction occurs in the area of the superior vena cava located before the azygos vein, the right superior intercostal veins will serve as the primary collateral pathway for azygos vein drainage. This pathway is often the most asymptomatic. If the obstruction occurs at the azygos vein, collateral channels will form between the superior vena cava and inferior vena cava via the internal mammary veins, superior and inferior epigastric veins, and the iliac vein. If the obstruction occurs past the point at which the azygos vein drains into the superior vena cava, the blood will move via channels from the azygos and hemiazygos veins into the ascending lumbar and lumbar veins, which will drain into the inferior vena cava and allow return into the right atrium.[24][25]
When the superior vena cava suffers more acute obstruction, it can result in upstream effects causing tributary veins in the head and neck to appear enlarged. It can also result in clinical symptomology, including shortness of breath, cough, angina, facial flushing, headache, bilateral upper extremity swelling, and dysphagia. Patients with an obstructed superior vena cava may have a positive Pemberton sign - described as a facial plethora and venous engorgement upon raising both arms above the head.[26] Neurological symptoms such as syncope, dizziness, and confusion are possible but less common presenting signs.[23]
Treatment of SVC syndrome depends on the cause. In the context of cancer, chemotherapy or radiation are options, as well as surgical resection of the mass if possible. In these cases, endovascular stenting may also be trialed however, although providing good short-term outcomes, it has been shown to likely require multiple repeat future interventions.[21][27] In the event of a thrombus, anticoagulation may be indicated to prevent further clot formation. Stent placement is considered a first-line treatment option here. CT is the imaging modality of choice for diagnosing a superior vena cava obstruction. Plain radiographs may also be used to detect indirect signs of a mediastinal mass but do not provide sufficient 3D anatomical accuracy for treatment planning.[25][28][29][30]
Media
(Click Image to Enlarge)
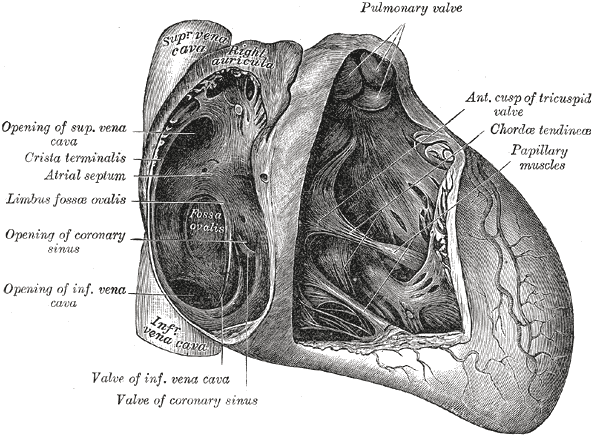
Anatomy of the Heart. This illustration shows the anatomic relationships between the pulmonary valve, the anterior cusp of the tricuspid valve, chordae tendineae, papillary muscles, the valve of the coronary sinus, the valve of inferior vena cava, the coronary sinus, the limbus fossae ovalis, the crista terminalis, the atrial septum, and the superior vena cava.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
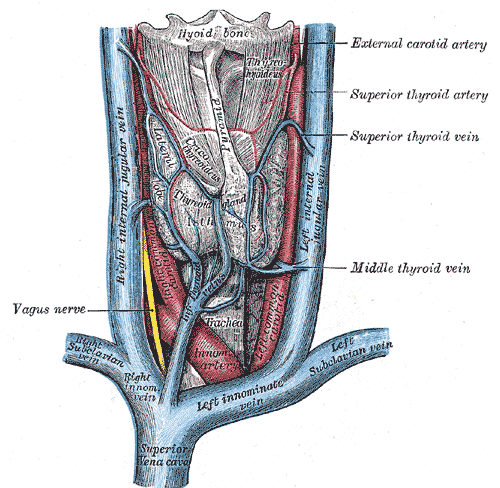
Veins and Arteries of the Neck. Superior vena cava, left and right innominate vein, left and right subclavian vein, left and right internal jugular vein, innominate arteries, hyoid bone, thyroid gland, and trachea.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
References
Nascimbene A, Angelini P. Superior vena cava thrombosis and paradoxical embolic stroke due to collateral drainage from the brachiocephalic vein to the left atrium. Texas Heart Institute journal. 2011:38(2):170-3 [PubMed PMID: 21494530]
Level 3 (low-level) evidencePiciucchi S, Barone D, Sanna S, Dubini A, Goodman LR, Oboldi D, Bertocco M, Ciccotosto C, Gavelli G, Carloni A, Poletti V. The azygos vein pathway: an overview from anatomical variations to pathological changes. Insights into imaging. 2014 Oct:5(5):619-28. doi: 10.1007/s13244-014-0351-3. Epub 2014 Aug 30 [PubMed PMID: 25171956]
Level 3 (low-level) evidenceFell SC. Surgical anatomy of the diaphragm and the phrenic nerve. Chest surgery clinics of North America. 1998 May:8(2):281-94 [PubMed PMID: 9619305]
Furlow PW, Mathisen DJ. Surgical anatomy of the trachea. Annals of cardiothoracic surgery. 2018 Mar:7(2):255-260. doi: 10.21037/acs.2018.03.01. Epub [PubMed PMID: 29707503]
McKay T, Thomas L. Prominent crista terminalis and Eustachian ridge in the right atrium: Two dimensional (2D) and three dimensional (3D) imaging. European journal of echocardiography : the journal of the Working Group on Echocardiography of the European Society of Cardiology. 2007 Aug:8(4):288-91 [PubMed PMID: 16621718]
Level 3 (low-level) evidenceSanjeev S, Karpawich PP. Superior vena cava and innominate vein dimensions in growing children : an aid for interventional devices and transvenous leads. Pediatric cardiology. 2006 Jul-Aug:27(4):414-9 [PubMed PMID: 16830087]
Nadesan T, Keough N, Suleman FE, Lockhat Z, van Schoor AN. Apprasial of the surface anatomy of the Thorax in an adolescent population. Clinical anatomy (New York, N.Y.). 2019 Sep:32(6):762-769. doi: 10.1002/ca.23351. Epub 2019 Mar 3 [PubMed PMID: 30758865]
Vuillemin M, Pexieder T. Normal stages of cardiac organogenesis in the mouse: II. Development of the internal relief of the heart. The American journal of anatomy. 1989 Feb:184(2):114-28 [PubMed PMID: 2712003]
Level 3 (low-level) evidenceSondermeijer BM, Macgillavry MR, Tan HL. Left superior vena cava, a remnant of embryological development. Netherlands heart journal : monthly journal of the Netherlands Society of Cardiology and the Netherlands Heart Foundation. 2008 May:16(5):173-4 [PubMed PMID: 18566698]
Schauerte P, Mischke K, Plisiene J, Waldmann M, Zarse M, Stellbrink C, Schimpf T, Knackstedt C, Sinha A, Hanrath P. Catheter stimulation of cardiac parasympathetic nerves in humans: a novel approach to the cardiac autonomic nervous system. Circulation. 2001 Nov 13:104(20):2430-5 [PubMed PMID: 11705820]
Qin M, Zhang Y, Liu X, Jiang WF, Wu SH, Po S. Atrial Ganglionated Plexus Modification: A Novel Approach to Treat Symptomatic Sinus Bradycardia. JACC. Clinical electrophysiology. 2017 Sep:3(9):950-959. doi: 10.1016/j.jacep.2017.01.022. Epub 2017 Apr 26 [PubMed PMID: 29759719]
Level 2 (mid-level) evidenceManousiouthakis E, Mendez M, Garner MC, Exertier P, Makita T. Venous endothelin guides sympathetic innervation of the developing mouse heart. Nature communications. 2014 May 29:5():3918. doi: 10.1038/ncomms4918. Epub 2014 May 29 [PubMed PMID: 24875861]
Level 3 (low-level) evidencePhillippi JA. On vasa vasorum: A history of advances in understanding the vessels of vessels. Science advances. 2022 Apr 22:8(16):eabl6364. doi: 10.1126/sciadv.abl6364. Epub 2022 Apr 20 [PubMed PMID: 35442731]
Level 3 (low-level) evidenceGustapane S, Leombroni M, Khalil A, Giacci F, Marrone L, Bascietto F, Rizzo G, Acharya G, Liberati M, D'Antonio F. Systematic review and meta-analysis of persistent left superior vena cava on prenatal ultrasound: associated anomalies, diagnostic accuracy and postnatal outcome. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2016 Dec:48(6):701-708. doi: 10.1002/uog.15914. Epub 2016 Nov 1 [PubMed PMID: 26970258]
Level 1 (high-level) evidenceBatouty NM, Sobh DM, Gadelhak B, Sobh HM, Mahmoud W, Tawfik AM. Left superior vena cava: cross-sectional imaging overview. La Radiologia medica. 2020 Mar:125(3):237-246. doi: 10.1007/s11547-019-01114-9. Epub 2019 Dec 10 [PubMed PMID: 31823296]
Level 2 (mid-level) evidenceAzizova A, Onder O, Arslan S, Ardali S, Hazirolan T. Persistent left superior vena cava: clinical importance and differential diagnoses. Insights into imaging. 2020 Oct 15:11(1):110. doi: 10.1186/s13244-020-00906-2. Epub 2020 Oct 15 [PubMed PMID: 33057803]
Demos TC, Posniak HV, Pierce KL, Olson MC, Muscato M. Venous anomalies of the thorax. AJR. American journal of roentgenology. 2004 May:182(5):1139-50 [PubMed PMID: 15100109]
Albay S, Cankal F, Kocabiyik N, Yalcin B, Ozan H. Double superior vena cava. Morphologie : bulletin de l'Association des anatomistes. 2006 Mar:90(288):39-42 [PubMed PMID: 16929820]
Level 3 (low-level) evidenceFarazi-Chongouki C, Dalianoudis I, Ninos A, Diamantopoulos P, Filippou D, Pierrakakis S, Skandalakis P. Double superior vena cava: presentation of two cases and review of the literature. Acta chirurgica Belgica. 2019 Oct:119(5):316-321. doi: 10.1080/00015458.2018.1438564. Epub 2018 Feb 19 [PubMed PMID: 29458311]
Level 3 (low-level) evidenceRaut MS, Das S, Sharma R, Daniel E, Motihar A, Verma A, Kar S, Maheshwari A, Shivnani G, Kumar A. Superior vena cava clamping during thoracic surgery: Implications for the anesthesiologist. Annals of cardiac anaesthesia. 2018 Jan-Mar:21(1):85-87. doi: 10.4103/aca.ACA_125_17. Epub [PubMed PMID: 29336403]
De Raet JM, Vos JA, Morshuis WJ, van Boven WJ. Surgical management of superior vena cava syndrome after failed endovascular stenting. Interactive cardiovascular and thoracic surgery. 2012 Nov:15(5):915-7. doi: 10.1093/icvts/ivs316. Epub 2012 Jul 27 [PubMed PMID: 22843656]
Level 3 (low-level) evidenceWilson LD, Detterbeck FC, Yahalom J. Clinical practice. Superior vena cava syndrome with malignant causes. The New England journal of medicine. 2007 May 3:356(18):1862-9 [PubMed PMID: 17476012]
Yu JB, Wilson LD, Detterbeck FC. Superior vena cava syndrome--a proposed classification system and algorithm for management. Journal of thoracic oncology : official publication of the International Association for the Study of Lung Cancer. 2008 Aug:3(8):811-4. doi: 10.1097/JTO.0b013e3181804791. Epub [PubMed PMID: 18670297]
Katabathina VS, Restrepo CS, Betancourt Cuellar SL, Riascos RF, Menias CO. Imaging of oncologic emergencies: what every radiologist should know. Radiographics : a review publication of the Radiological Society of North America, Inc. 2013 Oct:33(6):1533-53. doi: 10.1148/rg.336135508. Epub [PubMed PMID: 24108550]
Sheth S, Ebert MD, Fishman EK. Superior vena cava obstruction evaluation with MDCT. AJR. American journal of roentgenology. 2010 Apr:194(4):W336-46. doi: 10.2214/AJR.09.2894. Epub [PubMed PMID: 20308479]
Keshvani N, Yek C, Johnson DH. Pemberton's sign in SVC syndrome from metastatic renal cell carcinoma. BMJ case reports. 2018 Mar 28:2018():. pii: bcr-2018-224190. doi: 10.1136/bcr-2018-224190. Epub 2018 Mar 28 [PubMed PMID: 29593001]
Level 3 (low-level) evidenceKalra M, Gloviczki P, Andrews JC, Cherry KJ Jr, Bower TC, Panneton JM, Bjarnason H, Noel AA, Schleck C, Harmsen WS, Canton LG, Pairolero PC. Open surgical and endovascular treatment of superior vena cava syndrome caused by nonmalignant disease. Journal of vascular surgery. 2003 Aug:38(2):215-23 [PubMed PMID: 12891100]
Level 2 (mid-level) evidenceNiazi AK, Reese AS, Minko P, O'Donoghue D, Ayad S. Superior Vena Cava Syndrome and Otorrhagia During Cardiac Surgery. Cureus. 2019 May 5:11(5):e4602. doi: 10.7759/cureus.4602. Epub 2019 May 5 [PubMed PMID: 31309025]
Nunnelee JD. Superior vena cava syndrome. Journal of vascular nursing : official publication of the Society for Peripheral Vascular Nursing. 2007 Mar:25(1):2-5; quiz 6 [PubMed PMID: 17324762]
Fagedet D, Thony F, Timsit JF, Rodiere M, Monnin-Bares V, Ferretti GR, Vesin A, Moro-Sibilot D. Endovascular treatment of malignant superior vena cava syndrome: results and predictive factors of clinical efficacy. Cardiovascular and interventional radiology. 2013 Feb:36(1):140-9. doi: 10.1007/s00270-011-0310-z. Epub 2011 Dec 7 [PubMed PMID: 22146975]
Level 2 (mid-level) evidence
