Introduction
A fibroadenoma is a painless, unilateral, benign (non-cancerous) breast tumor that is a solid, not fluid-filled, lump. It occurs most commonly in women between 14 and 35 but can be found at any age. Fibroadenomas shrink after menopause and, therefore, are less common in post-menopausal women. Fibroadenomas are often referred to as a 'breast mouse' due to their high mobility. Fibroadenomas are a marble-like mass comprising both epithelial and stromal tissues located under the skin of the breast. These firm, rubbery masses with regular borders are often variable in size.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The causes of fibroadenoma are debatable, but professionals believe that the lesion has a hormonal etiology related to the increased sensitivity of breast tissue to the female reproductive hormone estrogen. Fibroadenoma usually grows during pregnancy and tends to shrink during menopause. This supports the hormonal etiologic theory. Females who take oral contraceptives before 20 years of age tend to suffer from fibroadenoma at higher rates than the general population.
Epidemiology
Fibroadenoma tends to occur in early life. It is most commonly found in adolescents and less commonly in postmenopausal women. The incidence of fibroadenoma decreases with age and is generally found in females before 30 in the general population. It is estimated that 10% of the world's female population suffers from fibroadenoma once in a lifetime.
Pathophysiology
Hormonal
Fibroadenoma arises from stromal and epithelial connective tissue cells that are functionally and mechanically important in the breast. These tissues contain receptors for both estrogen and progesterone. For this reason, fibroadenomas tend to proliferate during pregnancy because of excessive production of female reproductive hormones. Hormone sensitivity causes excessive proliferation of breast connective tissues.
Genetics
Mediator complex subunit 12 (MED12) gene is also important in the pathophysiology of fibroadenomas.
Histopathology
A fibroadenoma is a well-circumscribed, non-encapsulated lesion with pushing borders that does not infiltrate the adjacent breast parenchyma. They are characterized by a cellular proliferation of stroma and glands (benign breast ducts). The ratio between stroma to glands is relatively constant throughout the entire lesion. The stroma is uniform, hypovascular, and composed of spindle-shaped cells with bland oval to elongated nuclei. There is no stromal cell pleomorphism present. Smooth muscle, cartilage, and bone may be identified in the stroma. Stromal mitosis, although rare, can be seen, especially in fibroadenomas of younger women, and does not indicate malignancy. In older women, the stroma can be hyalinized.
The glands in a fibroadenoma consist of the normal bi-cell layer in breast ducts. The inner glandular layer comprises cuboidal to columnar-shaped cells with uniform nuclei. The inner cell layer is supported by an outer myoepithelial cell layer. The myoepithelial layer is intact throughout the entire lesion, designating a fibroadenoma's benign nature. Benign alterations such as usual ductal hyperplasia, apocrine metaplasia, squamous metaplasia, cystic changes, and sclerosing adenosis can involve the epithelium. Calcifications can also be in the glands. In pregnancy, the epithelium may show lactation changes.
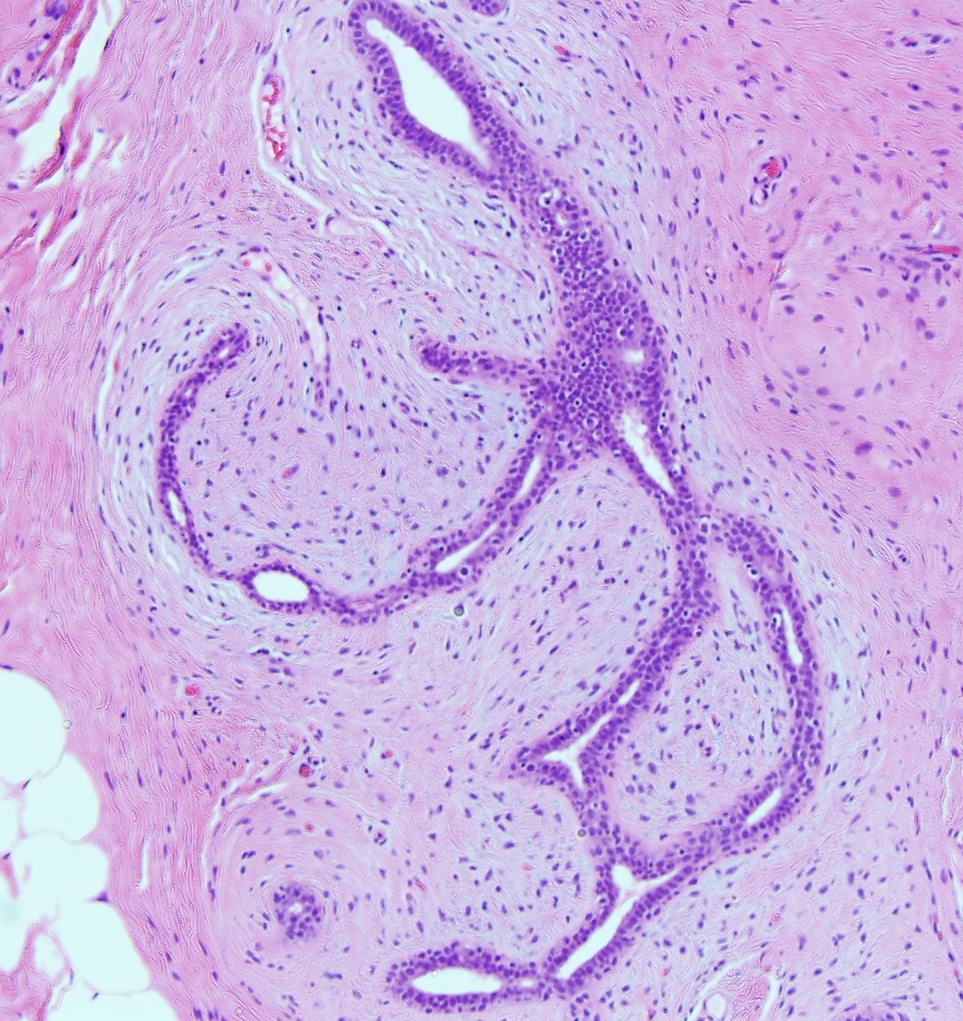
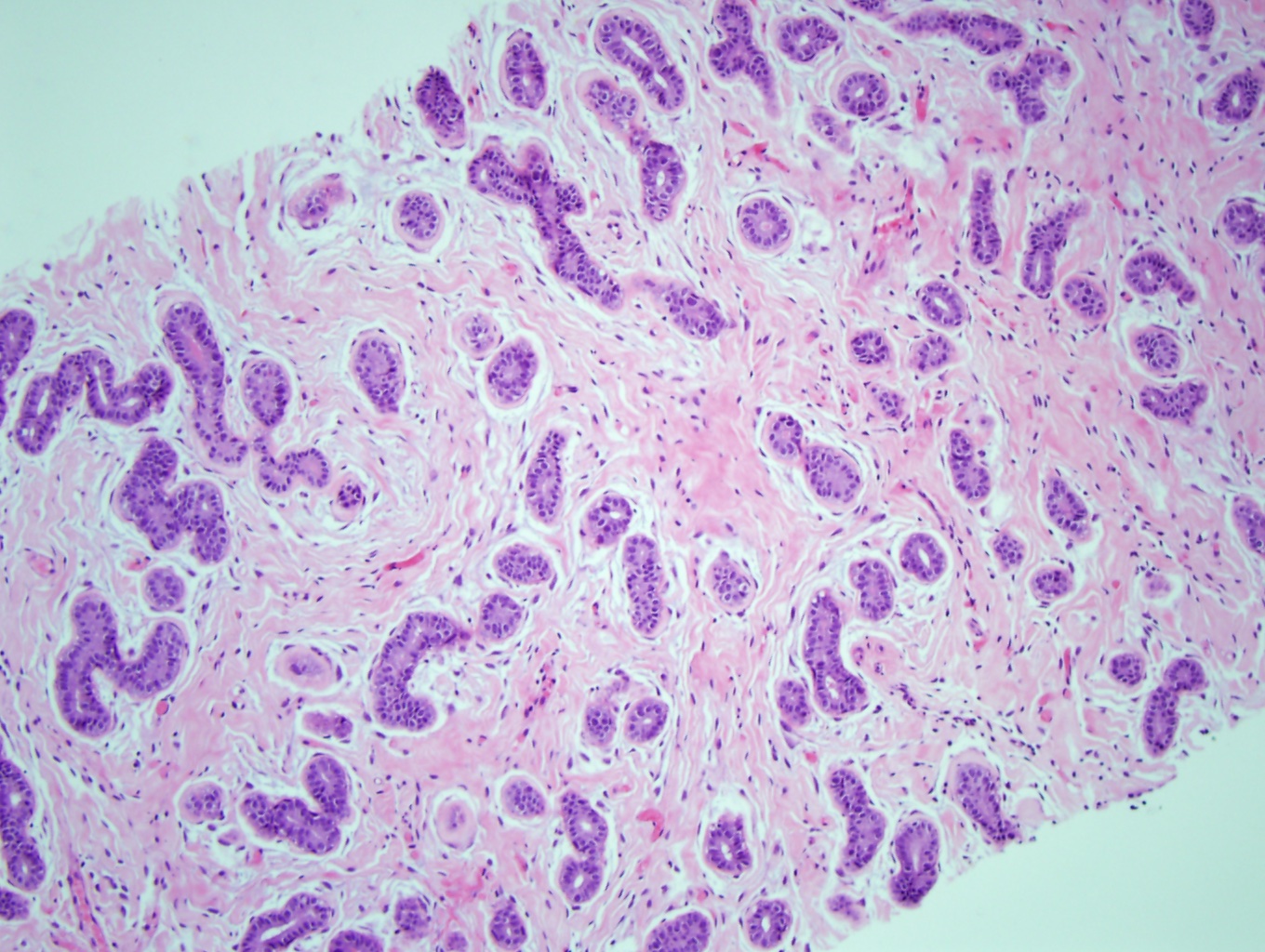
Fibroadenomas have 2 histological growth patterns: the intracanalicular pattern (see Image. Fibroadenoma With an Intracanalicular Pattern) and the pericanalicular pattern. The stroma compresses and distorts the glands into cleft-like spaces in the intracanalicular pattern (see Image. Fibroadenoma With Proliferating Stroma Compressing Glands in the Breast). The stroma surrounds the glands without distorting them, and the glands maintain their open lumens in the pericanalicular pattern (see Image. Fibroadenoma With Pericanalicular Pattern).
Histological variants of fibroadenomas exist. A myxoid fibroadenoma has prominent blue-tinged myxoid changes in the stroma (see Image. Myxoid Fibroadenoma). Although uncommon, some patients with myxoid fibroadenomas can have Carney complex (an autosomal dominant disorder characterized by endocrine tumors, myxomas, skin hyperpigmentation, and blue nevi, among others).[1] A cellular fibroadenoma has more stromal cellularity than usual. In a juvenile fibroadenoma, there is an increase in stromal cellularity and a greater degree of epithelial hyperplasia, commonly seen in young girls and adolescents. A complex fibroadenoma has sclerosing adenosis, epithelial calcifications, or papillary apocrine changes and is greater than 3 mm in size.[2]
Despite the patterns and histological variants of fibroadenomas, this does not change the benign nature of the lesion. Rarely, atypical ductal hyperplasia, atypical lobular hyperplasia, ductal carcinoma in situ, lobular carcinoma in situ, and invasive carcinomas can involve a fibroadenoma. These patients are treated according to their high-risk, pre-cancer, or cancerous lesions.[3]
History and Physical
Age is the most important factor in the incidence of fibroadenoma. Therefore, when obtaining a medical history, age is the most important factor which should be considered. A family history of breast cancer is also significant. Female patients who have first-degree relatives with breast cancer should be monitored and observed more carefully for malignant features than patients without this family history. Fibroadenoma most commonly occurs in the upper outer quadrant of the breast. On physical examination, it has the following features:
- Non-tender or painless
- Mobile
- Solitary
- Rapidly growing solid lump with rubbery consistency and regular borders.
Evaluation
After a thorough history and physical examination, the following imaging modalities are used to diagnose fibroadenomas.
Diagnostic Mammogram
A mammogram uses X-rays to evaluate the suspicious masses in women above 35 years of age. Fibroadenoma on a mammogram appears as a distinct area from other breast tissue, with smooth, round edges. See Figure 1. Mammographic features of fibroadenomas are variable from a well-circumscribed discrete oval mass hypodense or isodense of breast glandular tissue to a mass with macro lobulation or partially obscured margins. Involuting fibroadenomas in older, typically postmenopausal patients may contain calcification, often producing the classic, coarse popcorn calcification appearance.
Breast Ultrasound
Ultrasound uses sound waves to detect the features of fibroadenomas in women younger than 35 years of age. Ultrasound easily differentiates solid from the cystic masses. On ultrasound, a fibroadenoma is typically seen as a well-circumscribed, round to ovoid, or macrolobulated mass with generally uniform hypoechogenicity.[4][5] If necessary, a minimally invasive biopsy may be performed via a core needle biopsy[6]
Treatment / Management
In the majority of cases, fibroadenomas need no treatment. They shrink and disappear over time, but if their size is large and they are compressing other breast tissues, they should be removed. Many females decide against the surgery because the lesions are harmless and involve no long-term risk of malignancy. Surgery also distorts the shape of a breast.
Surgery
Doctors might decide to remove the fibroadenoma if it is massive and continues to increase in size. Indications for surgical intervention include rapid growth, size greater than 2 cm, and patient request. There are 2 surgical procedures used to remove a fibroadenoma:
- Lumpectomy or excisional biopsy: In this procedure, the surgeon removes the fibroadenoma and sends it to the laboratory for further evaluation.
- Cryoablation: Surgeons use a cryoprobe to freeze and destroy the cellular structure of fibroadenoma. A core needle biopsy must be performed before cryoablation to confirm the fibroadenoma.
Differential Diagnosis
THe differential diagnoses for breast fibroadenoma include the following:
- Breast cyst
- Breast carcinoma
- Phyllodes tumor
- Breast lymphoma
- Metastasis to the breast from another primary site
Prognosis
The prognosis of fibroadenoma is good because it is a benign mass that shrinks in size over time in most cases.
Complications
Breast cancer risk may slightly increase in patients with a complex fibroadenoma. This type of lesion may contain calcified breast tissue.
Enhancing Healthcare Team Outcomes
An interprofessional approach to fibroadenoma is recommended. The majority of breast lesions in young women are identified on an incidental breast exam either by the patient or the healthcare provider. Even though fibroadenomas are benign lesions, sometimes the histology may need to be confirmed. Healthcare workers should never assume that all firm, rubbery lesions are benign. If ever in doubt, get a radiologist or surgeon to perform a biopsy. Missing a malignant breast lesion in a young female can lead to poor outcomes.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Lozada JR, Burke KA, Maguire A, Pareja F, Lim RS, Kim J, Gularte-Merida R, Murray MP, Brogi E, Weigelt B, Reis-Filho JS, Geyer FC. Myxoid fibroadenomas differ from conventional fibroadenomas: a hypothesis-generating study. Histopathology. 2017 Oct:71(4):626-634. doi: 10.1111/his.13258. Epub 2017 Jul 5 [PubMed PMID: 28513873]
Krings G, Bean GR, Chen YY. Fibroepithelial lesions; The WHO spectrum. Seminars in diagnostic pathology. 2017 Sep:34(5):438-452. doi: 10.1053/j.semdp.2017.05.006. Epub 2017 May 28 [PubMed PMID: 28688536]
Feliciano YZ, Freire R, Net J, Yepes M. Ductal and lobular carcinoma in situ arising within an enlarging biopsy proven fibroadenoma. BMJ case reports. 2021 Jan 19:14(1):. doi: 10.1136/bcr-2020-237017. Epub 2021 Jan 19 [PubMed PMID: 33468635]
Level 3 (low-level) evidenceWoodard S, Schetter S, Millington K. Diagnosis and imaging characteristics of a juvenile fibroadenoma in a 2-year-old patient: a case report. Radiology case reports. 2018 Feb:13(1):6-10. doi: 10.1016/j.radcr.2017.11.008. Epub 2017 Dec 14 [PubMed PMID: 29487631]
Level 3 (low-level) evidenceNamazi A, Adibi A, Haghighi M, Hashemi M. An Evaluation of Ultrasound Features of Breast Fibroadenoma. Advanced biomedical research. 2017:6():153. doi: 10.4103/2277-9175.219418. Epub 2017 Nov 30 [PubMed PMID: 29285483]
Neville G, Neill CO, Murphy R, Corrigan M, Redmond PH, Feeley L, Bennett MW, O'Connell F, Browne TJ. Is excision biopsy of fibroadenomas based solely on size criteria warranted? The breast journal. 2018 Nov:24(6):981-985. doi: 10.1111/tbj.13069. Epub 2018 May 25 [PubMed PMID: 29802656]