Introduction
In 1901, René Le Fort, a French military surgeon, performed a series of experiments on 35 cadavers to determine the most common patterns of midfacial skeletal injuries that result from blunt trauma. Despite being an army physician, he eschewed the study of penetrating facial trauma, particularly gunshot wounds, as he termed them "veritable explosions in the face" and deemed them to be "without surgical interest."[1] Apocryphally, he is often reported to have dropped cannonballs onto severed heads to deliver the blunt force necessary for his studies; however, the literature contradicts this colorful story.
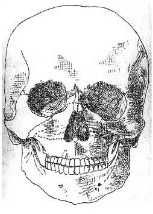
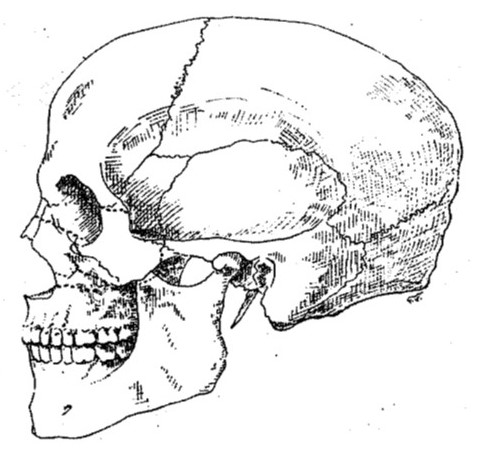
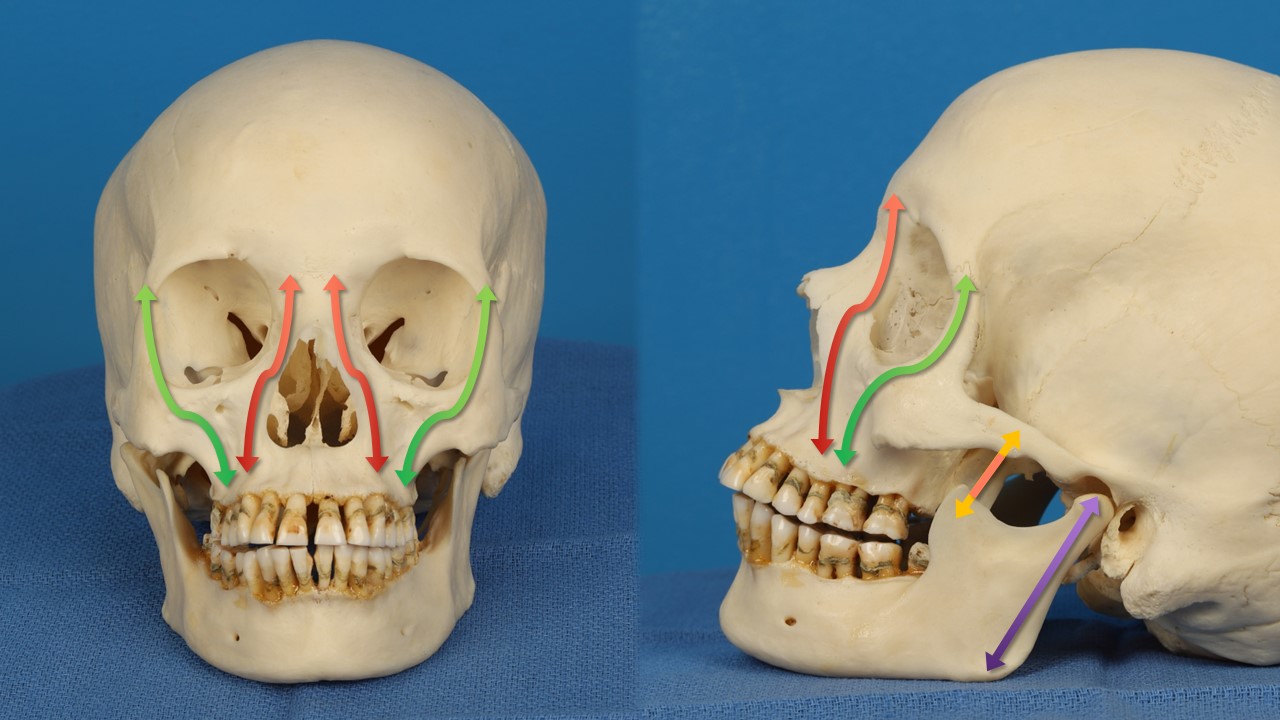
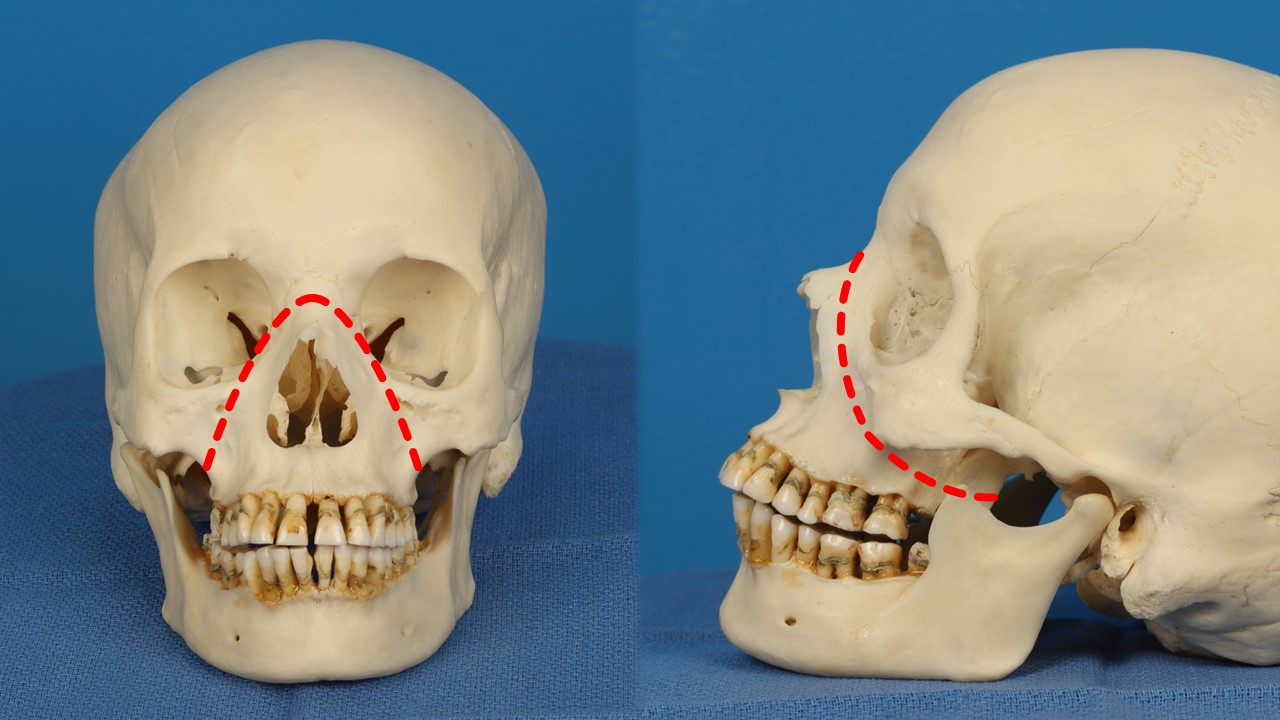
A combination of blows with a wooden club and a metal rod, stomping on the face, crushing with a vise, and "hurling" heads at the edge of a table was employed by his aides, after which the skulls were boiled to facilitate removal of the soft tissue for subsequent osseous examination.[1][2] Despite the lack of consistency in the experimental protocol to force, orientation, and mechanism of injury, Le Fort's work described many patterns in which fractures most commonly occur along the “lines of least resistance” (linea minoris resistentiae) that he identified (see Images. Facial Great Lines of Weakness, Profile View and Facial Great Lines of Weakness, Front View).[2] These patterns are now classified into 3 types based on their orientation: horizontal (type I), pyramidal (type II), and transverse (type III). All of these injuries separate the upper jaw from the skull and, by definition, involve fractures of the pterygoid plates of the sphenoid bone. The severe pattern fractures (pyramidal and transverse) occur more superiorly than the horizontal fracture, separating more of the facial skeleton from the neurocranium. These fractures are typically the result of greater forces applied to the central and upper midface.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Le Fort type I fractures typically result from a force directed in a downward direction just below the nose and above the teeth, while Le Fort type II fractures are caused by trauma to the lower or mid maxilla. Ahigh-energy impact to the nasal bridge and upper part of the maxilla leads to Le Fort type III fractures. The most common cause of Le Fort fractures described in the literature is motor vehicle accidents, accounting for 50% of these injuries, with higher speed collisions tending to result in higher grade fracture patterns, and motor vehicle accidents accounting for relatively fewer fractures in more developed nations. Lower energy mechanisms of injury, such as falls from standing and interpersonal violence, are more likely to result in lower-grade Le Fort fractures.[3]
Physical assaults are most likely to cause fractures of the nasal bones, orbit, and zygomatico-orbito-maxillary complex, although Le Fort type I fractures occur in 6% of cases, with Le Fort types II and III occurring in 5% and 3%, respectively.[4][5] Paralleling motor vehicle accidents, sports involving high-speed movement of the participant, such as skiing and mountain biking, are more likely to cause Le Fort fractures, while contact sports, such as rugby and American football, tend to result in non-Le Fort fractures.[6] Not surprisingly, as with other trauma, intoxication is frequently implicated in the causation of the injury, with drugs or alcohol involved in 13.6%, 18.1%, and 52.1% of incidents resulting in Le Fort I, II, and III fractures, respectively.[7]
Epidemiology
Le Fort fractures comprise a comparatively small proportion of all facial fractures, with nasal and mandible fractures being far more common. Depending on the study, Le Fort fractures may account for up to one-quarter of facial fractures; a Chinese series published in 2020 by Liu et al analyzed the characteristics of 829 patients with facial fractures and found that only 8.67% had Le Fort patterns, with 2.15% being type I, 4.64% type II, and 1.88% type III.[8] The authors also noted that 8.21% of the total fractures affected the maxilla but did not conform to a Le Fort pattern.
In contrast, results from a 2022 study from Togo reported that Le Fort fractures represented 24.84% of all facial fractures, but a 2017 review from the United States indicated that only 24% of maxillary fractures follow strict Le Fort patterns, while 56% have Le Fort fractures in addition to other maxillary fractures and 20% bear no resemblance to Le Fort patterns at all.[3] This same study reported the incidence of type I fractures being slightly less than that of type II fractures and just over half that of type III fractures. There is a wide variety in the described incidence of Le Fort fractures, but it is generally accepted that males are more likely to suffer these injuries than females, with a ratio anywhere between 3:1 and 12:1.[3][9] The mean age of patients with Le Fort fractures lies between 20 and 30 years in most reports.[3][8][10][8] Interestingly, results from a 2021 study in Romania that examined the records of 1007 patients correlated higher rates of facial fractures—although not specifically Le Fort fractures—with lower educational levels and urban living.[11]
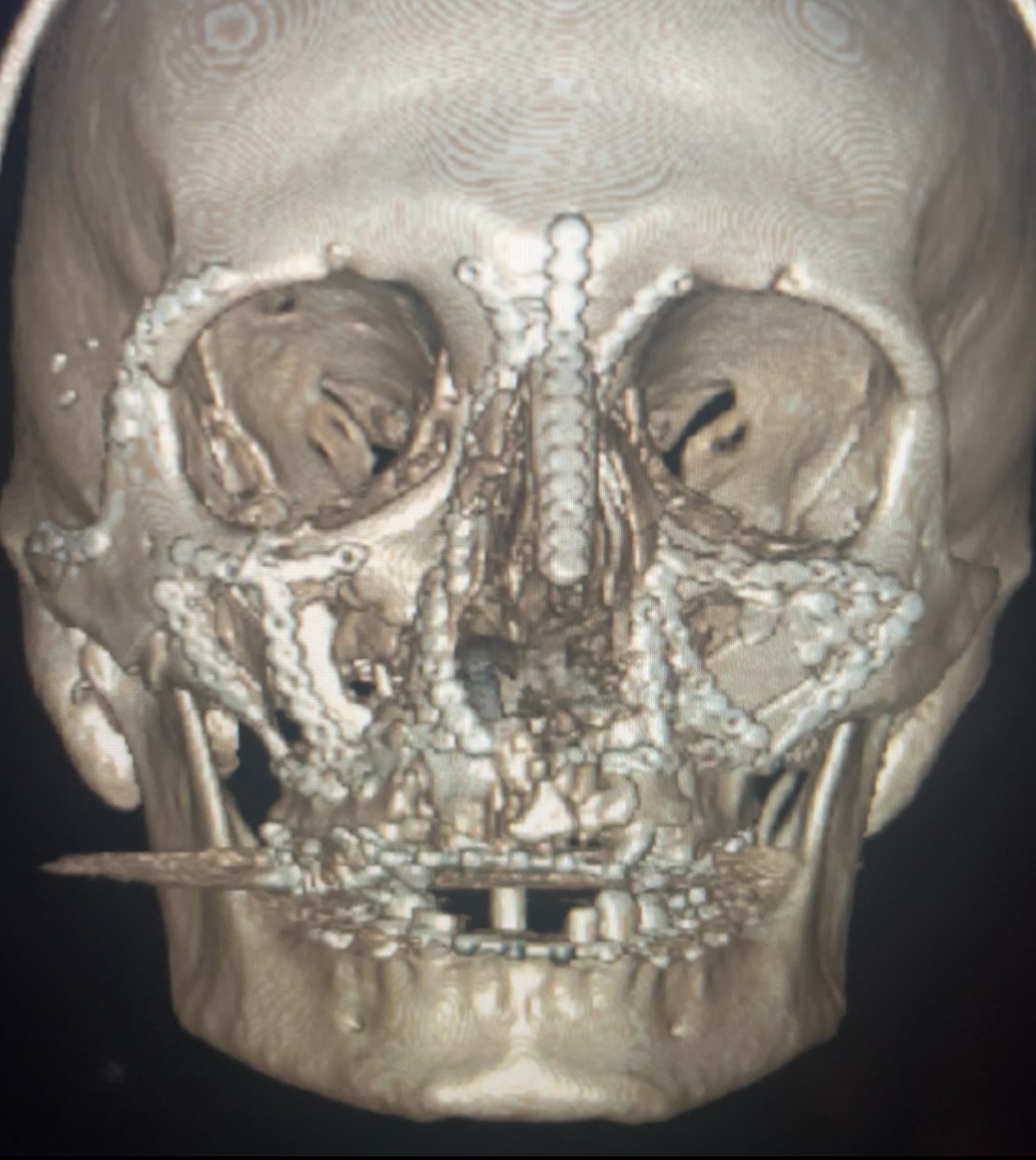
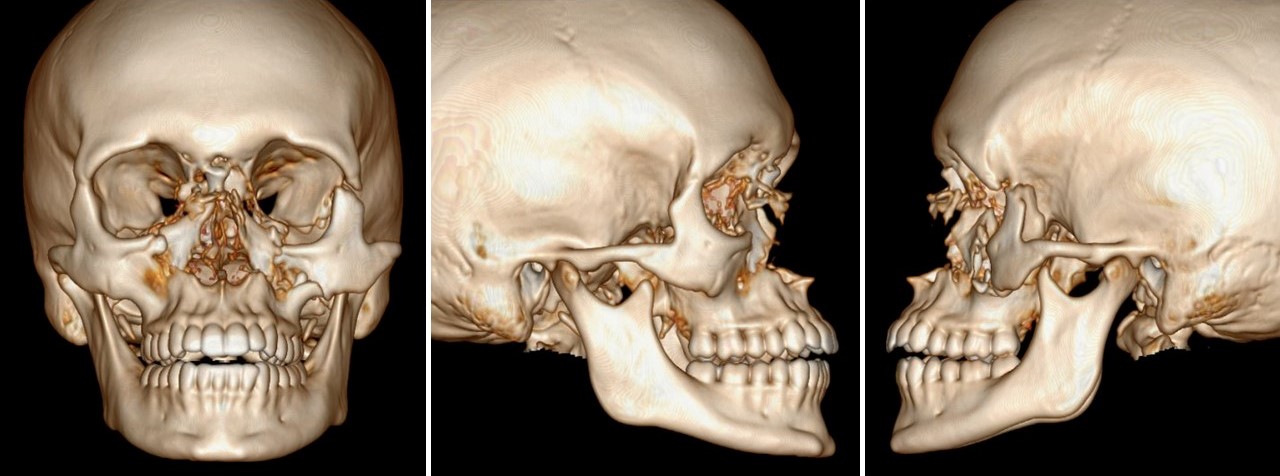
Pathophysiology
Le Fort fractures occur with high-energy, blunt force trauma to the midface, with different vectors and different impact points resulting in different fracture patterns. Le Fort fractures often occur asymmetrically, such as a type II injury on one side and a type III on the other, and more than one type of fracture may even coexist on the same side of the face, such as type I and II fractures concurrently (see Image. Le Fort Fractures of the Midface). These complex injuries seldom occur in isolation and are often associated with concomitant and sometimes life-threatening injuries.[12][13][14]
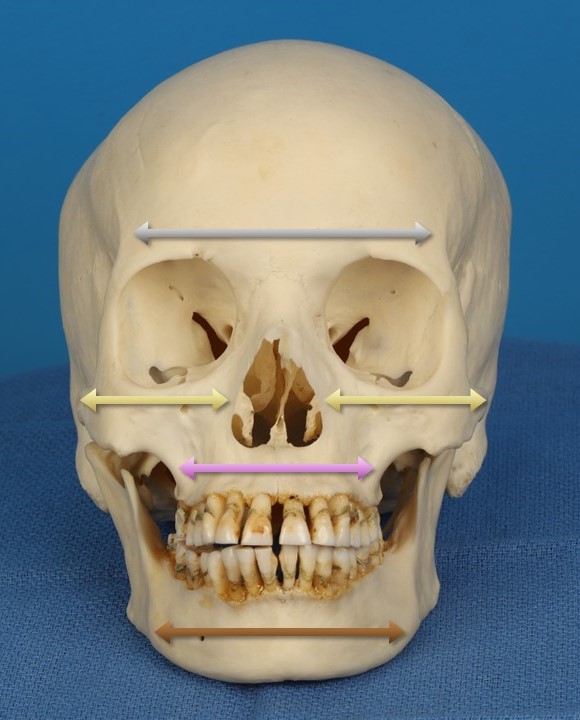
While not all facial fractures require fixation, such as the non-displaced orbital floor, zygoma, or frontal sinus fractures, Le Fort fractures typically necessitate intervention because they violate the structural buttresses of the face. The buttresses are the bony support elements that determine the facial width and height; when disrupted, the face will take on a dysmorphic appearance unless the fractures are adequately reduced. The vertical buttresses of the face are the nasomaxillary, zygomaticomaxillary, and pterygomaxillary buttresses, as well as the mandibular rami (see Image. Vertical Buttresses of the Face).
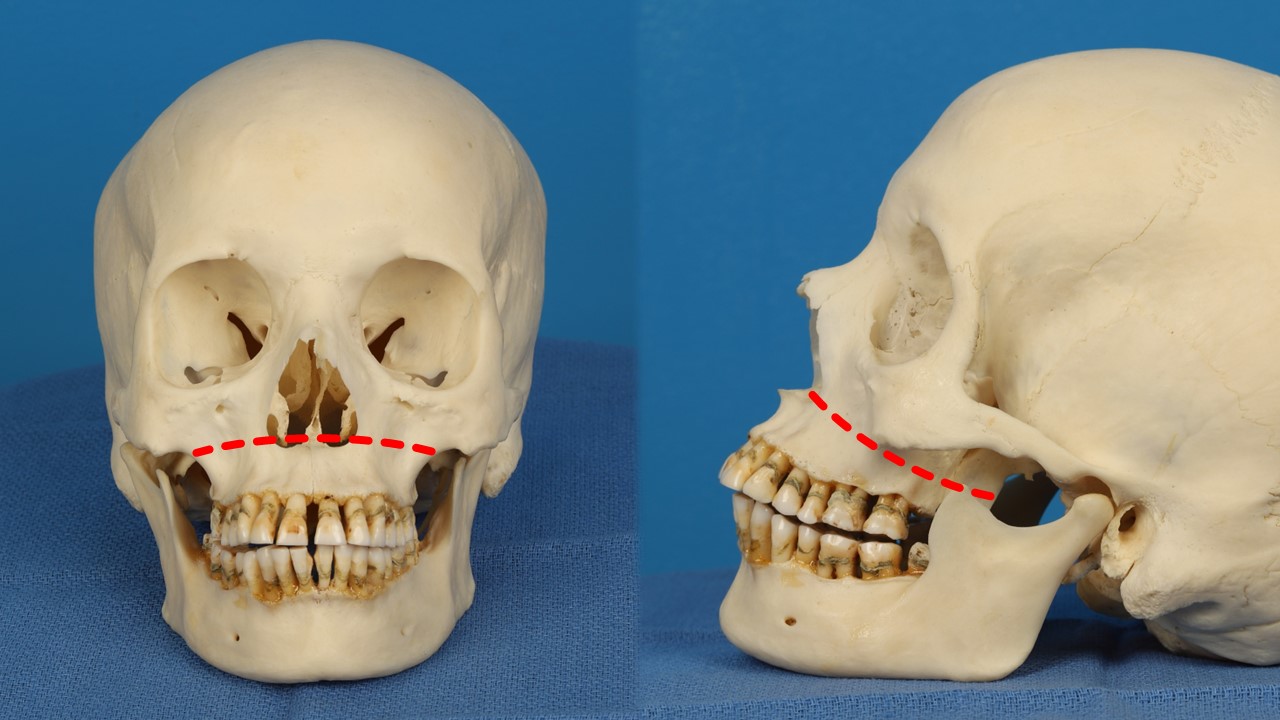
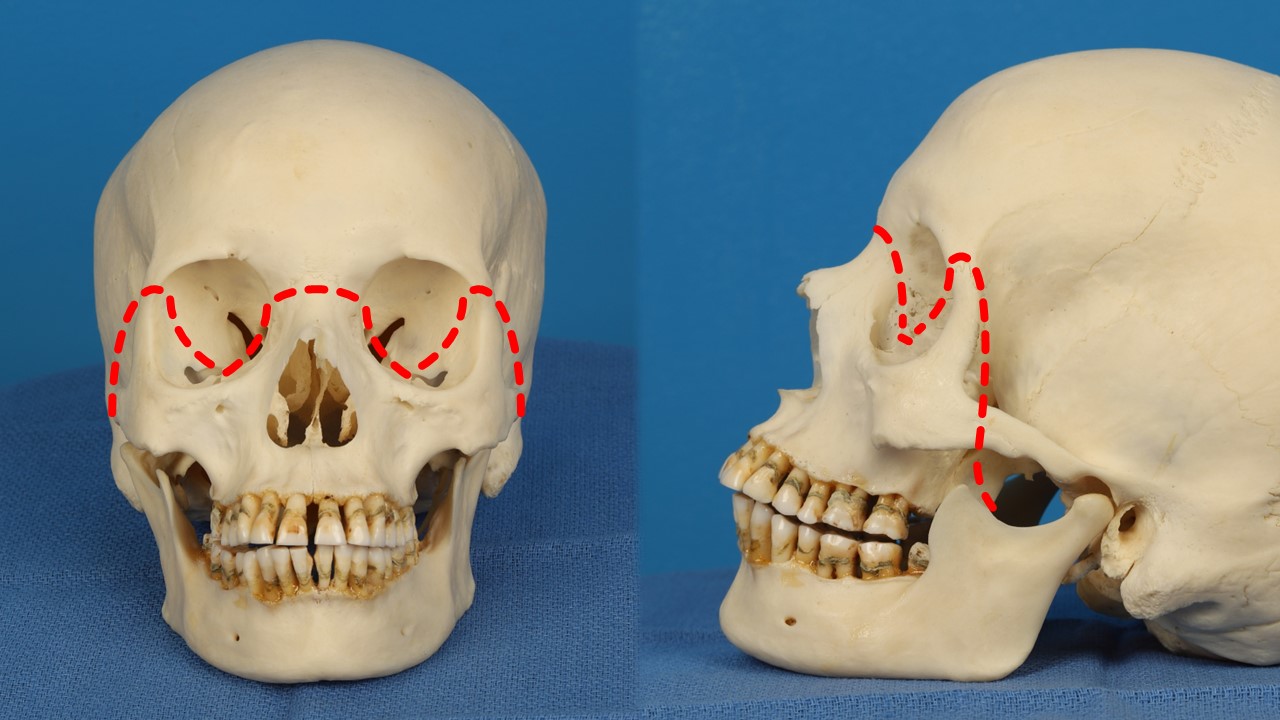
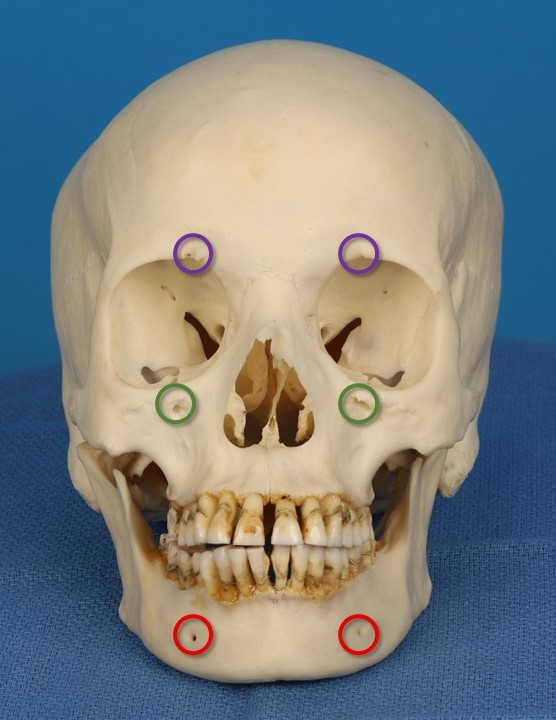
All Le Fort fractures disrupt the pterygomaxillary buttress, the only buttress not usually fixated due to its deep location within the midface. These buttresses resist forces directed superoinferiorly, but are prone to fracture when struck in an anteroposterior vector. The horizontal buttresses are the frontal bar, the inferior orbital rims, the zygomatic arches, the superior alveolar ridge, the hard palate, and the body of the mandible (see Image. Horizontal Buttresses of the Face). Type II Le Fort fractures necessarily disrupt the inferior orbital rim, and type III fractures violate the zygomatic arch. Importantly, type III Le Fort fractures always involve fractures of the naso-orbito-ethmoid complex.[15]
Classification of Fractures
Type I
Le Fort type I fractures run horizontally through the maxilla, above the roots of the teeth, separating the hard palate from the upper face (see Image. Le Fort I Horizontal Fracture). These fractures can be unilateral or bilateral and result from a force directed low on the maxillary rim in a downward direction, occurring in a horizontal plane at the level of the base of the nose. Le Fort type I fractures propagate through all 3 walls of the maxillary sinus and the ipsilateral pterygoid plates of the sphenoid bone. A bilateral fracture will also involve the nasal septum.
Type II
These fractures extend superiorly through the midface to include the nasal bridge, maxilla, lacrimal bones, orbital floor, and inferior orbital rim (see Image. Le Fort II Pyramidal Fracture). The Le Fort type II is a pyramidal pattern with the maxillary teeth at the base and the nasal bones at the apex. These fractures are typically bilateral. The fracture line begins near the nasion and extends obliquely through the nasal septum and lacrimal bones at the medial aspect of the orbits and then to the inferior orbital rims, continuing posteriorly above the hard palate (but below the zygoma) and through the pterygoid plates, resulting in a disarticulation of the central midface from the remainder of the skull. These fractures result from a high-energy impact on the lower or mid maxilla.
Type III
This type of fracture starts at the bridge of the nose and extends posteriorly along the medial wall and floor of the orbit, then through the lateral orbital wall and the zygomatic arch, continuing to propagate through the nasal septum and pterygoid plates (see Image. Le Fort III Transverse Fracture). The fractures run parallel to the base of the skull, separating the entire midfacial skeleton from the cranial base (craniofacial dissociation). Le Fort type III fractures may be associated with a cerebrospinal fluid (CSF) leak due to concomitant skull base injury. These fractures result from an impact to the nasal bridge or upper maxilla and involve the naso-orbito-ethmoid region, thus significantly complicating their repair.
History and Physical
As with any trauma, the obtained medical history should elucidate the mechanism of injury, associated injuries, and any suspected substance use. A thorough review of systems should include neurological considerations such as loss of consciousness, mental status changes, dizziness, nausea, headache, change in visual acuity or diplopia, new onset rhinorrhea, hearing loss, numbness, and weakness. For facial trauma, identifying difficulty breathing, speaking, or swallowing is also critical because of the risk of airway compromise with these injuries. Ideally, medical and surgical histories and a list of medications and allergies should be obtained. Some of this information may need to come from a witness, friend, or family member if the patient is unconscious or intubated.
The physical examination should include complete primary and secondary trauma surveys, paying particular attention to the patient's airway and any bleeding occurring within it. If necessary, orotracheal intubation or a surgical airway should be employed. The skin is examined for lacerations, abrasions, avulsions, hematomas, and foreign bodies, paying close attention to the scalp, where hair may hide these injuries. A complete cranial nerve examination should be performed, as maxillary fractures frequently cause injury to the infraorbital nerves, leading to midfacial hypesthesia. Peripheral neurological assessment will help assess potential spinal injury; a cervical collar will most likely remain in place until the spine can be radiographically cleared.
The face and skull should be palpated carefully, appreciating any deformities, bony step-offs, or instability. The premaxilla should be grasped and rocked back and forth. This maneuver may identify anything from loose incisors to dentoalveolar fractures to Le Fort fractures, with the extent of the injury determined by how much surrounding bone moves with the palate, if any at all. Loose or missing teeth should be noted during an intraoral examination along with any mandibular step-offs, mucosal lacerations, or ecchymosis. The patient's occlusion should be documented using the Angle classification to identify an anterior open bite, which may indicate a Le Fort fracture or bilateral mandibular condyle fractures. Open bites may also indicate mandibular injury, particularly lateral open bites, resulting from contralateral condylar fractures.
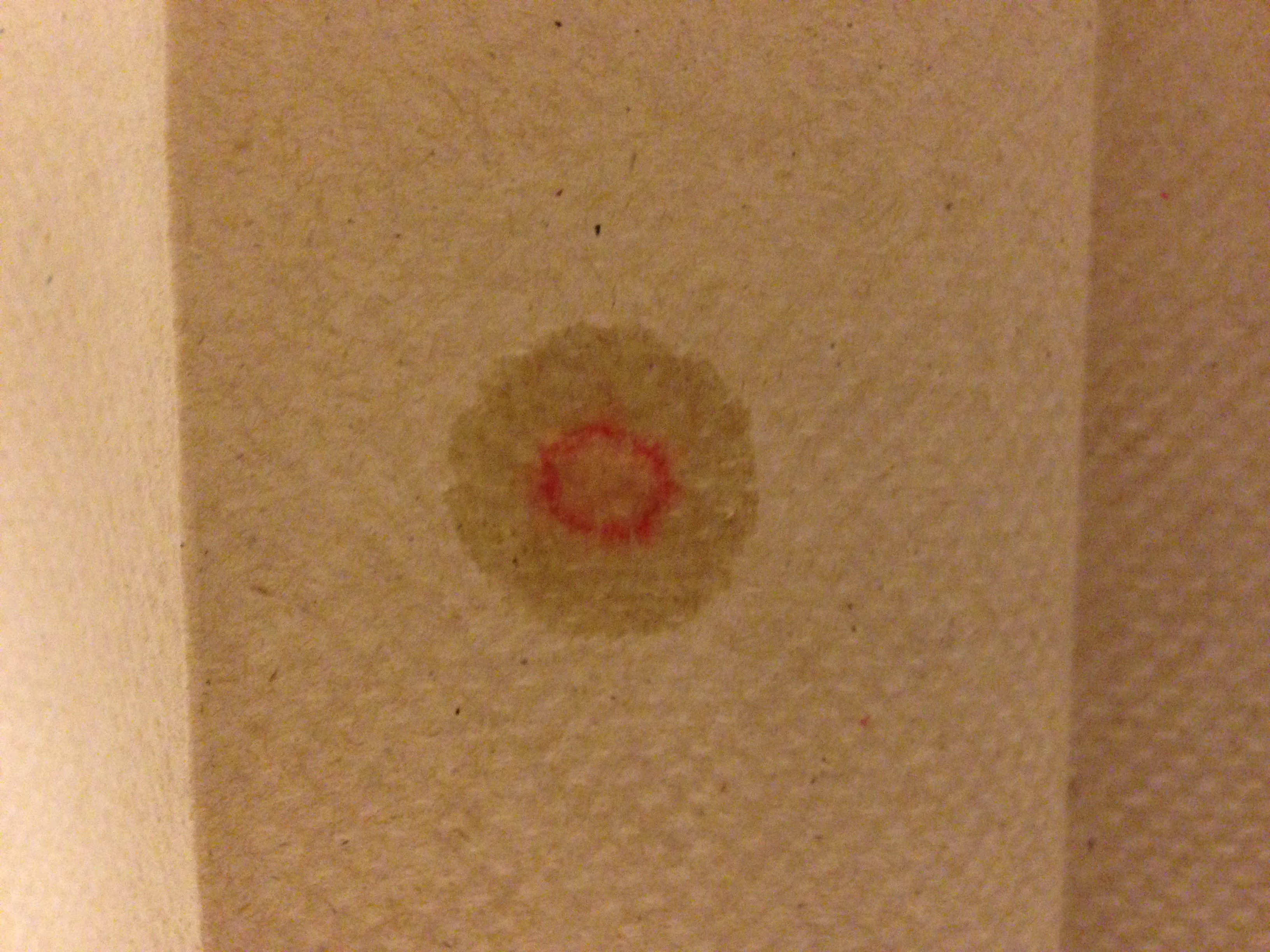
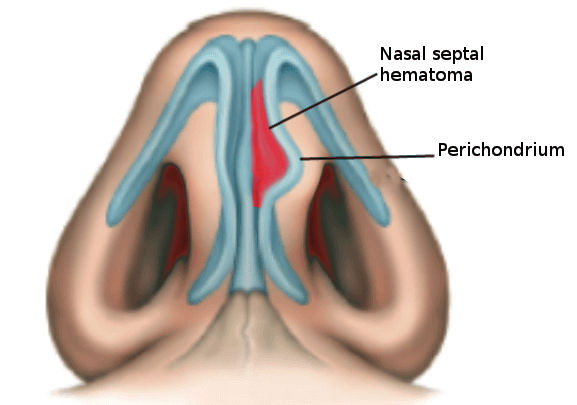
It is recommended that an ophthalmologist evaluate the globes and orbits for suspected higher-grade fractures, mainly to rule out globe injury before fracture repair. The nose should also be examined, especially if there is epistaxis or new-onset rhinorrhea. A "halo sign" of clear fluid diffusing away from a drop of blood on a paper towel or a piece of filter paper may be caused by a CSF leak, and evaluation of the fluid for glucose, β-2 transferrin or β-trace protein may be necessary (see Image. Halo Sign for Cerebral Spinal Fluid). The halo sign is, however, relatively nonspecific and can also be caused by mucoid rhinorrhea or tears mixed with blood.[16] Suspicion for a CSF leak should be higher in patients with hemotympanum, periorbital ecchymosis (raccoon eyes), or mastoid ecchymosis (Battle sign) (see Image. Skull Base Fractures). Any blow to the face powerful enough to be suspected of causing midfacial fractures also has the potential to cause a nasal septal fracture and hematoma, which should also be specifically ruled out by examination. If present, a septal hematoma should be incised, and a drain should be left in place to prevent reaccumulation (see Image. Nasal Septal Hematoma).
Le Fort Type I
Le Fort type I fractures present with a swollen upper lip, anterior open bite malocclusion, ecchymosis of the maxillary buccal vestibule and palate, and mobility of the maxilla.
Le Fort Type II
With Le Fort type II fractures, there is significant deformity and swelling, mobility of the maxilla and nose as a combined segment, bilateral periorbital edema and ecchymosis, epistaxis, anterior open bite malocclusion, ecchymosis of the maxillary buccal vestibule and palate, and possible CSF rhinorrhea. Since the fracture involves the inferior orbital rim and floor, there may be diplopia or sensory deficits in the infraorbital region extending down to the upper lip.
Le Fort Type III
Le Fort type III fractures include naso-orbito-ethmoid complex fractures, which often present with traumatic telecanthus. Additionally, there will be bilateral periorbital edema and ecchymosis, ecchymosis of the maxillary buccal vestibule and palate, elongation and flattening of the face (dish-face deformity), orbital hooding, enophthalmos, epistaxis, and potentially ecchymosis over the mastoid region, CSF rhinorrhea, CSF otorrhea, and hemotympanum.
Evaluation
The initial evaluation of patients with maxillofacial trauma should follow Advanced Trauma Life Support (ATLS) protocols. The primary survey includes airway and cervical spine stabilization, breathing and ventilatory support, attention to circulation and hemorrhage control, disability and neurologic evaluation, and exposure and environment control. Airway obstruction associated with fractures of the midfacial skeleton can be life-threatening if not recognized promptly and managed appropriately. Nasotracheal intubation is contraindicated when there is a potential skull base fracture due to the risk of intracranial misdirection of the tube.
Orotracheal intubation is typically preferred, although this can be very challenging in upper airway hemorrhage. Video laryngoscopy may help treat airway edema or injury; this method is ineffective if there is significant bleeding due to obstruction of the camera lens. A surgical airway, such as a tracheostomy or cricothyroidotomy, may be required if orotracheal intubation is impractical due to obstruction from anatomical distortion, edema, or hemorrhage. The risk of life-threatening hemorrhage in Le Fort II and III injuries is higher than that associated with other facial injuries.
In patients with complex maxillofacial trauma, other associated injuries should be evaluated and excluded or treated, depending upon the mechanism of injury. Common concomitant injuries include skull fracture (40.7%), closed head injury (5.4%), and cervical spine injury (5.4%).[17][18][19][20] More often than not, a patient with facial fractures transported by ambulance will have a cervical spine collar in place, which may complicate airway management.
Despite the importance of the physical examination, the sine qua non of facial trauma evaluation is fine-cut (≤3 mm slices) computed tomography (CT), particularly because patients are often unable to comply with physical examination after polytrauma. CT is the most effective means of assessing the extent of bone and soft tissue involvement.[21] Three-dimensional reconstructions of the 2-dimensional images obtained by the scanner are helpful for both the surgeon and the patient to appreciate the extent of the injuries and inform the reconstructive plan; soft tissue injuries remain better evaluated in 2 dimensions, however.[22] A chest x-ray may also be added to assess for aspirated missing teeth. If there is penetrating trauma to the midface, there may also be injury to the brain and major vascular structures. Therefore, a CT of the head and diagnostic angiography should also be considered. CT imaging also excellent for identifying concomitant skeletal injuries in the cervical spine, skull, and face. Palatal fractures are commonly associated with Le Fort injuries, as are frontal sinus, zygomatico-orbito-maxillary complex, orbital floor, and mandibular fractures.
Treatment / Management
Initial Management
The primary evaluation and stabilization of the patient should be performed in conjunction with a trauma surgeon. Definitive surgery should be performed after life-threatening injuries have been addressed following ATLS protocols. Consultations from all relevant specialists should be obtained, depending upon the extent of injuries revealed by physical examination and CT scanning. Commonly, an otolaryngologist, plastic surgeon, or oral surgeon will be the primary attending, but the expertise of a neurosurgeon, ophthalmologist, or dentist may also be required. Surgery to reconstruct the midface is typically scheduled a few days after the injury to allow time for some of the soft tissue edema to subside. Surgery is ideally performed before a week has passed to preempt early healing of displaced bone fragments into extra-anatomical positions.
Preparation for Surgery
In the operating room, the airway may be secured via an orotracheal tube passed through a gap in the teeth or behind the teeth, through the floor of the mouth and out below the chin (submental intubation), or via a tracheostomy.[23] For Le Fort type I fractures without concomitant skull base injury, nasotracheal intubation may be an option as well. The decision regarding the route of airway protection is informed by the patient's anatomy and the extent of the injuries. Once the airway is secure and general anesthesia induced, the operating table may be rotated to the side to provide the surgeon and assistant more room to maneuver around the patient's head, if desired.
Prophylactic antibiotics are administered because implants will be placed, potentially through the mouth, but there is no evidence that continuing antibiosis beyond 24 hours after surgery is beneficial.[24][25] Antibiotic prophylaxis in patients with CSF leaks remains controversial and should be considered at the discretion of the treating neurosurgeon; likewise, many clinicians will provide antibiotics when the paranasal sinuses are involved in the fractures. Open or contaminated maxillofacial trauma also provides a strong indication for prophylactic antibiosis, according to the American Association for the Surgery of Trauma Critical Care Committee, even if reduction and fixation of fractures are not necessary.[26](B2)
Steroids may help reduce postoperative edema and nausea, while tranexamic acid limits intraoperative bleeding and postoperative bruising.[27][28] Administration of a long-acting paralytic medication may facilitate manipulation of the mandible, but paralysis will also prevent twitching of facial muscles if electrocautery is applied near facial nerve branches. The decision of whether or not to request paralytic medications will depend upon the access required during surgery. Infiltration of local anesthetic with epinephrine is recommended, as it will reduce the intraoperative bleeding and potentially the opioid requirement as well.[29][30][31] If orbital surgery is anticipated, corneal shields may be placed; alternatively, the eyes may be closed and protected with sterile adhesive dressings or temporary tarsorrhaphy sutures. The surgical field includes the full face to provide landmarks for intraoperative reference.(A1)
Maxillomandibular Fixation
Facial reconstruction begins with the establishment of occlusion. In the absence of a mandible fracture, this process is comparatively simple: the maxilla is adjusted until the upper dentition fits into the wear facets on the mandibular dentition, and the jaws are wired together over Erich arch bars, maxillomandibular fixation (MMF) screws, or hybrid systems. In the event of a palate fracture, which may occur with Le Fort type I injuries, the bony segments should be reduced and fixated with plates or lag screws before placement of MMF. While often unavailable, any information on the patient's pretraumatic occlusion status is helpful. Edentulous individuals may need dentures fixated to the maxilla and mandible to perform MMF, and using the dentures provides the added benefit of rigidly splinting any palatal or mandibular body fractures. While concomitant displaced mandible fractures may complicate MMF, the same principles apply: restore the pretraumatic occlusion and then fixate the mandible to the maxilla.
Exposure
After MMF is achieved, all of the fractures are surgically exposed before they are reduced or fixated to prevent inadvertent misalignment of bone fragments. Some fractures may be accessed via lacerations, but additional incisions will be required more often than not. Exposure to a Le Fort type I fracture only requires an upper gingivolabial sulcus incision from first molar to first molar, typically made with monopolar electrocautery roughly 5 mm superior to the gingival margin to ensure enough soft tissue remains on both sides of the incision to permit suture closure. A periosteal elevator, such as a Molt #9, is then used to expose the maxilla and the transverse fractures extending laterally from the base of the piriform aperture.
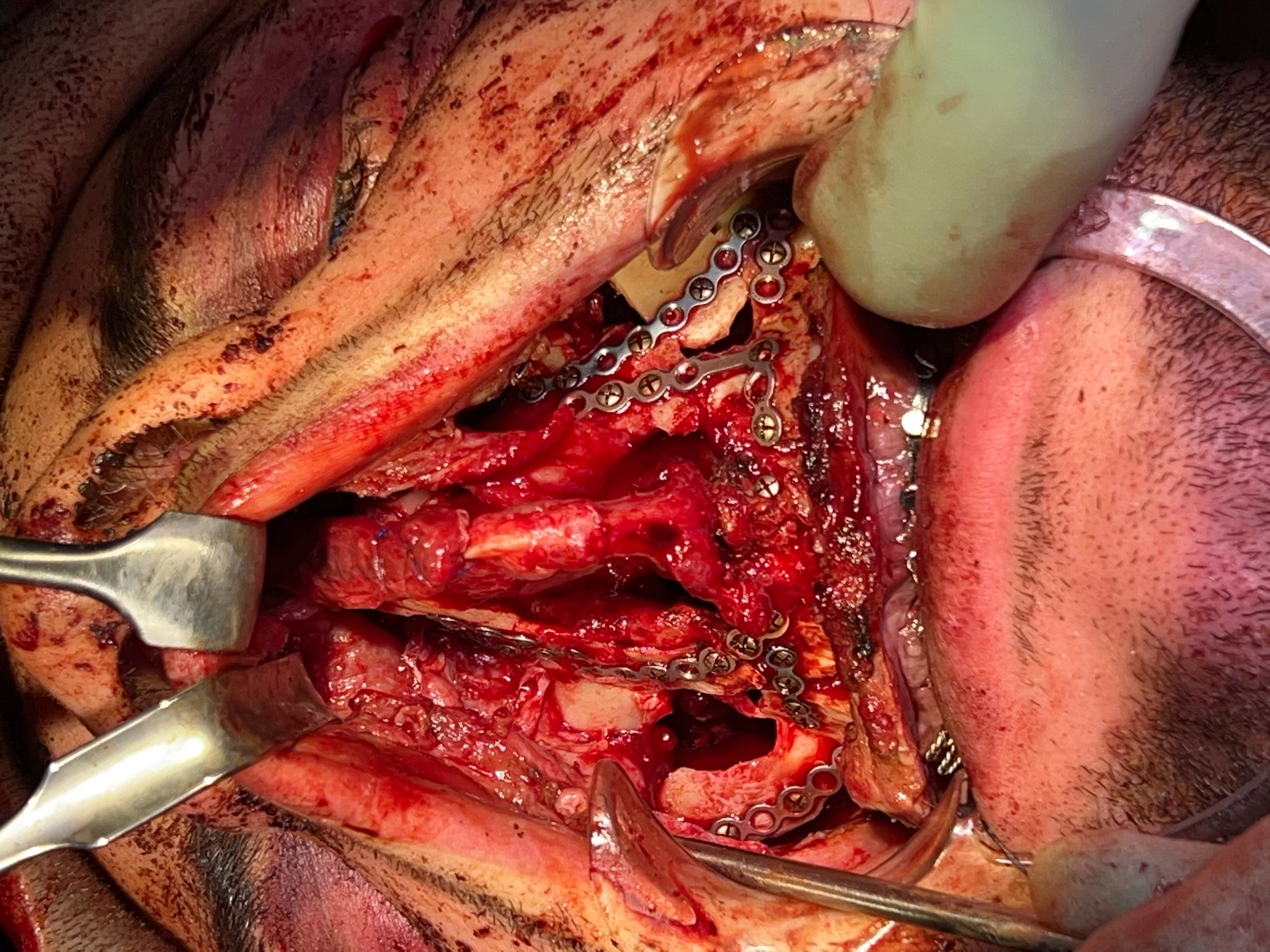
A Le Fort type II fracture may require greater exposure than a type I fracture due to its greater superior extent. A midfacial degloving approach may be necessary for these injuries, which adds circumvestibular intercartilaginous incisions within the nares and a full transfixion anterior nasal septal incision. These circumvestibular incisions allow elevation of the soft tissue envelope away from the nasal bones and upper lateral cartilages and connection of the gingivolabial sulcus incision to the floor of the nasal cavity. After bilateral subperiosteal elevation is performed to the level of the inferior orbital rims, taking care to preserve the infraorbital neurovascular bundles that emerge from the infraorbital foramina (see Image. Trigeminal Foramina of the Face), the midfacial soft tissue may be elevated as a unit that includes the lower third of the nose. This provides exposure of the entire anterior maxilla, including the frontal processes (see Image. Open Reduction and Internal Fixation of Midface Fractures).
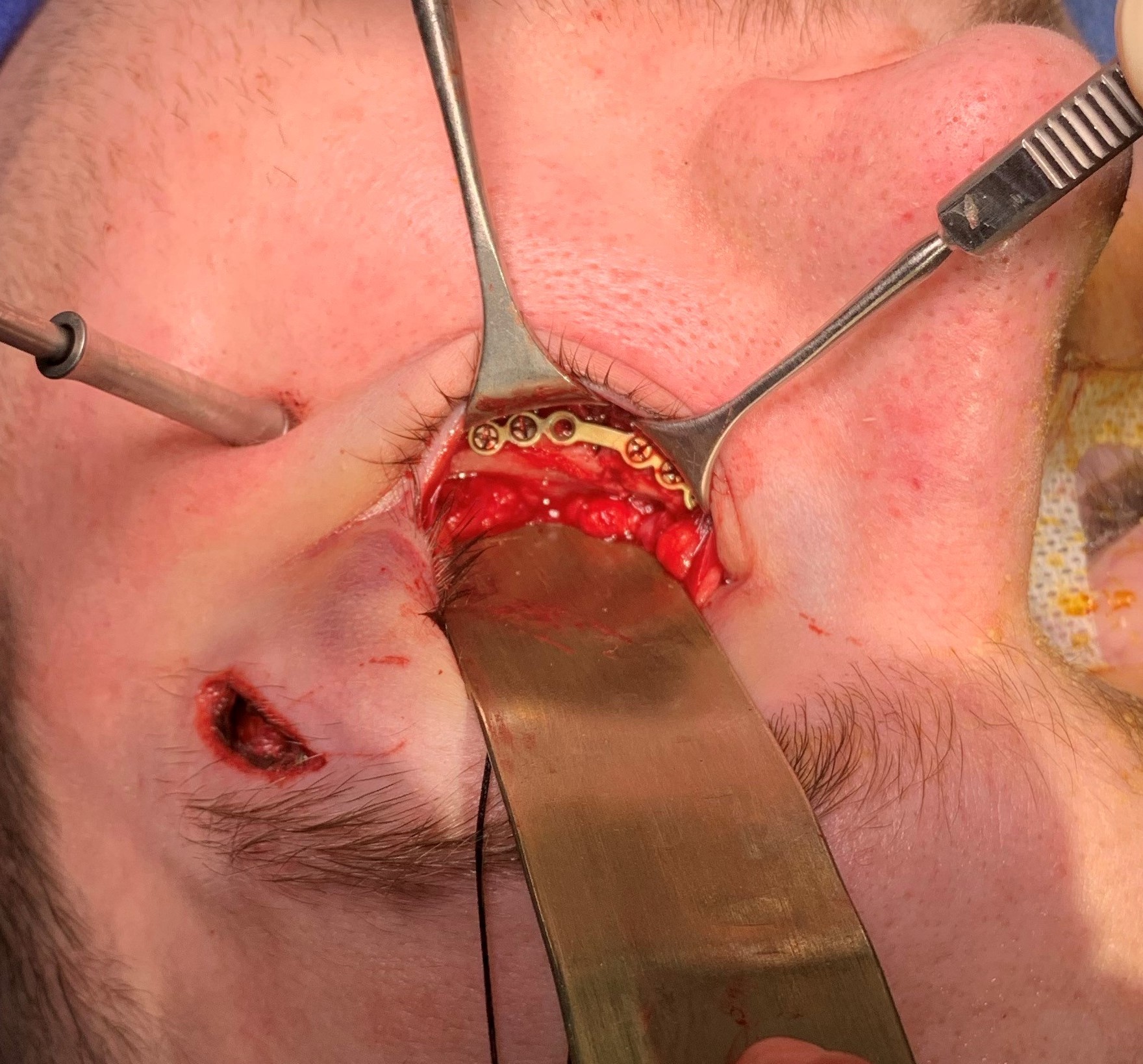
Even greater exposure is required to access Le Fort type III fractures. Typically, a coronal incision is employed, as it will provide access to the naso-orbito-ethmoid region and the zygomatic arches (see Image. Coronal Approach to the Craniofacial Skeleton). The coronal incision is made across the crown of the head, from ear to ear, through the scalp, and down to the bone. Subperiosteal elevation then proceeds down the forehead towards the brows. Laterally, the conjoint tendons fixate the frontalis muscle and galea aponeurotica to the periosteum at the temporal line, creating a barrier to complete anterior scalp elevation in a single plane (see Image. Fascial Planes of the Face).
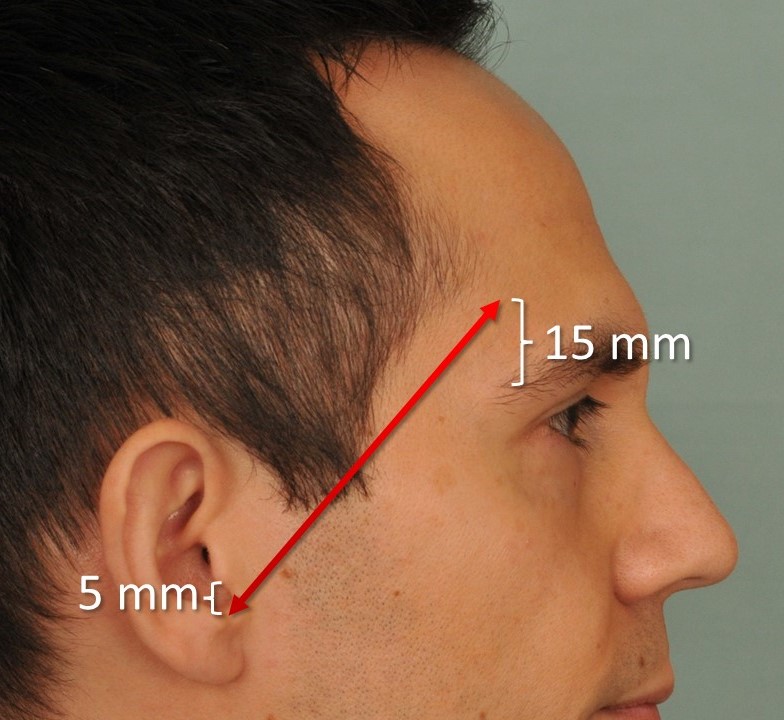
In the temporal regions, lateral to the conjoint tendons, elevation may be performed either on the superficial aspect of the temporalis muscle fascia (deep temporal fascia) or the muscle itself. This plane is used to approach and then divide the conjoint tendon, thus making the central and lateral dissections contiguous. The temporalis fascia can also be followed inferiorly down to the zygomatic arch. Maintaining a plane of dissection deep to the temporoparietal fascia (superficial temporal fascia) will avoid causing injury to the frontal branch of the facial nerve, particularly when operating in the region of the Pitanguy line (see Image. Pitanguy Line).
The supraorbital neurovascular bundle emerges from a notch or foramen situated in the midpupillary line of the superior orbital rim (see Image. Trigeminal Foramina of the Face), which should be protected to avoid postoperative hypesthesia of the forehead, even though scalp anesthesia posterior to the coronal incision is expected. If a periosteal flap is needed for frontal sinus obliteration or skull base reconstruction, it can be peeled off the underside of the coronal flap to provide the desired thickness of soft tissue, or it can be developed off the skull directly during coronal flap elevation (see Image. Pericranial Flap Elevation). Orbital access may also be required to reduce a Le Fort type III fracture, often via transconjunctival incisions to expose the orbital floor.
Transconjunctival approaches are classified as either preseptal or postseptal. In the preseptal approach, most dissection occurs anterior to the orbital septum, which is then opened to allow intraorbital access. In contrast, the postseptal approach involves initial dissection posterior to the orbital septum, which remains intact. The postseptal approach is commonly used in trauma surgery (see Image. Left Orbital Floor Fracture, Transconjunctival, Post-Septal Approach). Because of the high likelihood of concomitant injuries with Le Fort type III fractures, other incisions may be required to access all of the facial fractures, for example, intraoral incisions to fixate mandibular fractures.
Reduction
Once all of the fractures have been exposed, other than the pterygoid plate fractures, any displaced bony segments must be reduced back into their anatomical positions. This is a comparatively simple Le Fort type I fracture process that may be performed manually or using Rowe disimpaction forceps. Due to the action of the pterygoid muscles, the large maxillary segment will tend to be displaced posteriorly and inferiorly, resulting in the characteristic anterior open bite finding on physical examination. The likelihood of a higher grade Le Fort fracture existing without any comminution is low, which typically reduces the bony segments to a painstaking process. However, some bone may be discarded if it neither contributes to a buttress nor impacts cosmesis, such as small fragments of the anterior face of the maxilla. Larger bone segments, such as the zygomas, may be manipulated back into anatomical positions with the use of a large bone hook or a Carroll-Girard screw.
Fixation
When a limited number of bony segments are present, the order in which they are fixated is not necessarily critical; the general principle is to secure mobile segments to stable ones.[32][33][34] When comminuted panfacial fractures occur, it may be helpful to proceed from lateral to medial, using the zygomatic arches to establish the width of the face. Then, the naso-orbito-ethmoid region and maxillary alveolar ridge can be used to set midfacial projection. Last, the midface's anterior buttresses and the mandible's rami will determine the facial height.
In the case of accompanying condylar fractures, reestablishing mandibular height may be very challenging, making the achievement of correct occlusion with MMF critical. When fixating bony fragments, larger segments are typically addressed before smaller ones. Buttresses are fixated with 2 mm plates, and 1.3 mm plates are used for thinner bone. Monocortical screws are typically used, but care must still be taken to avoid injuring tooth roots. For very thin bony fragments, pre-drilling holes for the screws will help to prevent additional fracturing. Saline irrigation should be applied whenever drilling is performed to keep the area cool and avoid osteocyte injury, which is highly sensitive to temperatures greater than 40 ºC (104 ºF).
Substantial bone fragments may be fixated with self-drilling screws for the sake of operative efficiency. When excessive comminution leaves defects greater than 5 mm in width, bone grafting should be performed to bridge the gaps using a split calvarium, rib, or iliac crest. For the naso-orbito-ethmoid region, transnasal wiring is critical for reestablishing a correct intercanthal relationship and alleviating traumatic telecanthus. A 28 gauge wire is passed through the bony segments that bear the medial canthal ligaments, running through the upper nasal vault such that the wires are visible intranasally and terminate around a screw placed in the glabella for stability. The wire should be tightened until the intercanthal distance is excessively narrow, as widening inevitably occurs during healing.
Closure
Closure is accomplished in layers, with suspension of the midfacial soft tissues that were elevated during exposure of the fractures to the remaining periosteum occurring first. This step is critical to prevent the development of midfacial soft tissue ptosis, which can result in disfigurement or noticeable asymmetry if the surgical approach is unilateral. In the case of extensive subperiosteal dissection, as with midfacial degloving, no periosteum may be suspended, and midface lifting with sutures or implantable suspension devices may be used instead.[35][36]
Other techniques are also routinely employed to prevent soft tissue distortion, including alar cinching sutures placed into the nasal base via the gingivolabial sulcus incision and V to Y advancement at the center of the same incision. The alar cinch prevents the widening of the alar base due to maxillary advancement, and the V to Y advancement prevents unsightly thinning of the upper lip during the healing process.[37][38] Last, the release of MMF and removal of arch bars is performed if no mandibular fracture is present. If maintenance of MMF is required for mandibular fractures, early mobilization by advancement from wires to guiding elastics will reduce the risk of temporomandibular joint ankylosis.[39]
Postoperative Care
Significant edema inevitably results after repairing midfacial fractures despite judicious use of corticosteroids for the first 24 hours postoperatively; patients will benefit from additional conservative measures, such as cold packs, head of bed elevation, and activity restrictions to reduce heavy lifting, straining, and nose blowing. Antibiotics may be prescribed for the first day after surgery, and oral hygiene with chlorhexidine mouthwash or similar should be encouraged. A soft diet is most appropriate initially unless MMF is maintained postoperatively due to mandibular fractures. A CT scan is usually performed within the first 24 hours after surgery to evaluate the success of the bony reduction.
Differential Diagnosis
The differential diagnoses of Le Fort fractures may include:
- Naso-orbito-ethmoid fracture
- Frontal bone fracture
- Nasal bone fracture
- Zygomatico-orbito-maxillary complex (tripod) fracture
- Orbital floor fracture
- Maxillary sinus fracture
- Mandible fracture
- Dentoalveolar fracture.
Prognosis
The treatment outcome for Le Fort fractures depends on the mechanism of injury, location and severity, and presence of concomitant injuries. The mortality rate for Le Fort fractures is higher than that for simple midface fractures, particularly for higher-grade fractures, as they are often associated with polytrauma. Le Fort fractures by themselves are not life-threatening, however. Higher-grade fractures, particularly when combined with other facial fractures, substantially raise the risk of persistent facial deformity.
Complications
Complications of Le Fort fractures may include:
- CSF leak (Le Fort type II and III fractures)
- Epistaxis
- Epiphora
- Nasal obstruction
- Facial hypesthesia or dysesthesia
- Visual deficit
- Malocclusion
- Persistent facial deformity
- Need for revision surgical procedures.
Consultations
Patients with Le Fort fractures typically present to the emergency department, and consultation is usually requested from the facial trauma service, which may include otolaryngologists, plastic surgeons, facial plastic surgeons, and oral surgeons. If a periocular injury is present, an ophthalmology or oculoplastic surgery consult should be requested, and if a CSF leak, skull base, posterior table frontal sinus, or cranial vault fracture is identified, a neurosurgical opinion should be sought. Radiology will also become involved in the patient's care through diagnostic imaging.
Deterrence and Patient Education
Given that the most common causes of Le Fort midfacial fractures are motor vehicle accidents, interpersonal violence, and falls, prevention of these injuries is focused on seat belt wear and home safety as well as avoidance of inebriation, which increases the risk of motor vehicle accidents, interpersonal violence, and falls that can produce craniofacial injuries.[40][41][42] Additionally, when participating in high-speed sporting activities, such as skiing, bicycling, snowmobiling, or motocross, helmet wear with face protection will help minimize the risk of facial trauma.
In 1983, legislation in the United Kingdom required the use of seatbelts in motor vehicles, resulting in a two-thirds reduction in the incidence of maxillofacial fractures from road traffic accidents in the ensuing 2 years.[43] Subsequent retrospective reviews have concurred that using seat belts or a combination of seat belts and airbags significantly decreases the risk of maxillofacial fractures. However, airbag deployment without seat belt use does not appear to decrease the risk of facial injury.[44][45][46] There have been several case reports of Le Fort midfacial fractures occurring in patients who have failed to wear seat belts but whose airbags deployed during a collision. Another important but very preventable risk factor for facial fractures in motor vehicle accidents is alcohol consumption, which has been shown to increase the incidence of facial fractures.[47] When road traffic accidents involve motorcycles, helmet use, particularly helmet use with face protection, is known to decrease the rates of facial fractures.[47][48] Fall prevention in the home may also reduce the incidence of Le Fort fractures, especially for older adults. These interventions include physical safety modifications within the dwelling, such as grab rails, night lights, and reduction of clutter on the floor, as well as exercises focused on improving balance and coordination and optimization of medications to reduce confusion, vertigo, and syncope.[49] Patients with improved overall health and strength are less likely to fall and sustain serious injuries.[50]
Enhancing Healthcare Team Outcomes
Le Fort fractures are not common, but when they present, they are typically in the emergency department and often in the setting of other concomitant injuries. Patients with polytrauma may arrive with vital sign instability or shock, necessitating evaluation by a trauma surgeon, who may need to address injuries more immediately life-threatening than the facial fractures by the ATLS algorithm. However, Le Fort fractures are also best managed by a team that may include oral surgeons, otolaryngologists, plastic surgeons, ophthalmologists, and neurosurgeons for higher-grade fractures. Beyond the surgical team, the patient will require care from specialist nurses and potential nutrition support if the fractures require MMF repair. Last, radiology services are indispensable for both diagnosis and surgical planning.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
Horizontal Butresses of the Face. The horizontal buttresses of the face provide structural support and determine the width of the face: grey, frontal bar; yellow, inferior orbital rims and zygomatic arches; pink, superior alveolar ridge; and brown, mandibular body.
Contributed by MH Hohman, MD, FACS
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
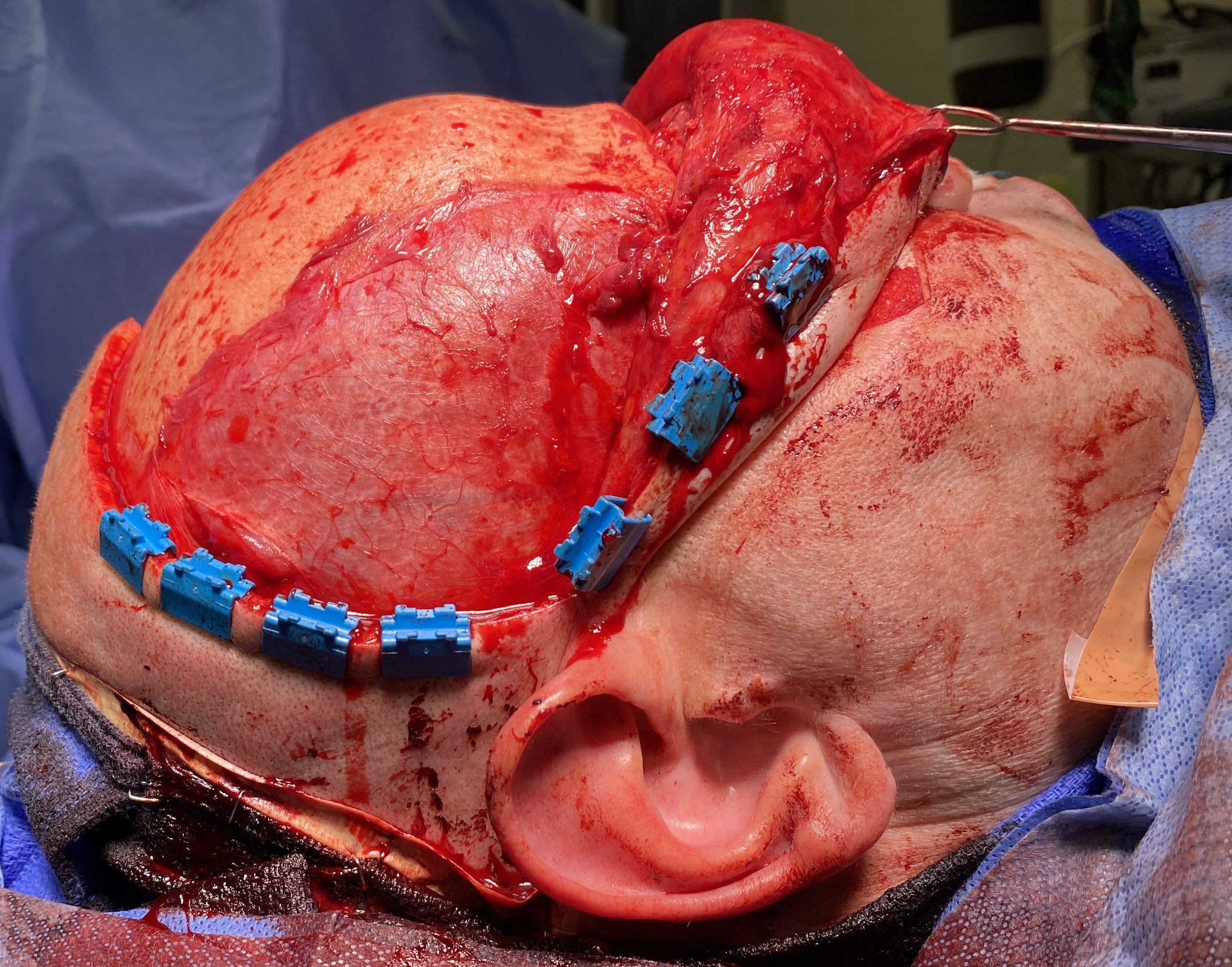
Coronal Approach to the Craniofacial Skeleton. This surgical exposure grants access to the frontal sinus, naso-orbito-ethmoid region, zygomatic arches, orbital roofs, and anterior skull base. Structures at risk include the frontal branches of the facial nerve and the supraorbital and supratrochlear nerves.
Contributed by MH Hohman, MD, FACS
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
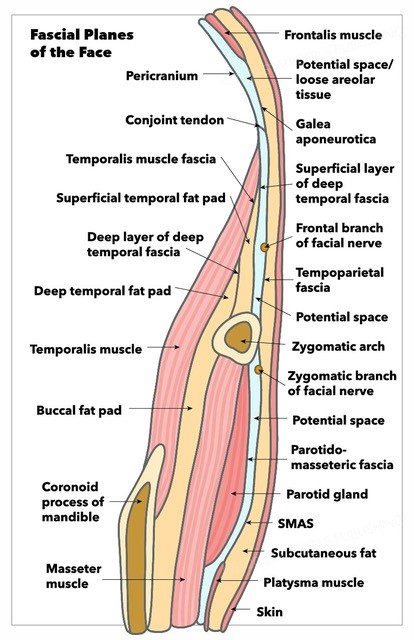
Fascial Planes of the Face and Musculature. This illustration depicts the fascial planes of the face, highlighting the continuity of the frontalis muscle, galea aponeurotica, temporoparietal fascia, superficial musculoaponeurotic system, platysma, and the location of the facial nerve.
Contributed by K Humphreys and MH Hohman, MD, FACS
References
Tessier P. The classic reprint. Experimental study of fractures of the upper jaw. I and II. René Le Fort, M.D. Plastic and reconstructive surgery. 1972 Nov:50(5):497-506 contd [PubMed PMID: 4563382]
Tessier P. The classic reprint: experimental study of fractures of the upper jaw. 3. René Le Fort, M.D., Lille, France. Plastic and reconstructive surgery. 1972 Dec:50(6):600-7 [PubMed PMID: 4564611]
Phillips BJ, Turco LM. Le Fort Fractures: A Collective Review. Bulletin of emergency and trauma. 2017 Oct:5(4):221-230. doi: 10.18869/acadpub.beat.5.4.499.. Epub [PubMed PMID: 29177168]
Salonen EM, Koivikko MP, Koskinen SK. Violence-related facial trauma: analysis of multidetector computed tomography findings of 727 patients. Dento maxillo facial radiology. 2010 Feb:39(2):107-12. doi: 10.1259/dmfr/67015359. Epub [PubMed PMID: 20100923]
Lee KH. Interpersonal violence and facial fractures. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2009 Sep:67(9):1878-83. doi: 10.1016/j.joms.2009.04.117. Epub [PubMed PMID: 19686924]
Maladière E, Bado F, Meningaud JP, Guilbert F, Bertrand JC. Aetiology and incidence of facial fractures sustained during sports: a prospective study of 140 patients. International journal of oral and maxillofacial surgery. 2001 Aug:30(4):291-5 [PubMed PMID: 11518350]
Bagheri SC, Holmgren E, Kademani D, Hommer L, Bell RB, Potter BE, Dierks EJ. Comparison of the severity of bilateral Le Fort injuries in isolated midface trauma. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2005 Aug:63(8):1123-9 [PubMed PMID: 16094579]
Xiao-Dong L, Qiu-Xu W, Wei-Xian L. Epidemiological pattern of maxillofacial fractures in northern China: A retrospective study of 829 cases. Medicine. 2020 Feb:99(9):e19299. doi: 10.1097/MD.0000000000019299. Epub [PubMed PMID: 32118746]
Level 2 (mid-level) evidenceGirotto JA, MacKenzie E, Fowler C, Redett R, Robertson B, Manson PN. Long-term physical impairment and functional outcomes after complex facial fractures. Plastic and reconstructive surgery. 2001 Aug:108(2):312-27 [PubMed PMID: 11496168]
Level 2 (mid-level) evidencePatil RS, Kale TP, Kotrashetti SM, Baliga SD, Prabhu N, Issrani R. Assessment of changing patterns of Le fort fracture lines using computed tomography scan: an observational study. Acta odontologica Scandinavica. 2014 Nov:72(8):984-8. doi: 10.3109/00016357.2014.933252. Epub 2014 Sep 17 [PubMed PMID: 25227590]
Level 2 (mid-level) evidenceJuncar M, Tent PA, Juncar RI, Harangus A, Mircea R. An epidemiological analysis of maxillofacial fractures: a 10-year cross-sectional cohort retrospective study of 1007 patients. BMC oral health. 2021 Mar 17:21(1):128. doi: 10.1186/s12903-021-01503-5. Epub 2021 Mar 17 [PubMed PMID: 33731083]
Level 2 (mid-level) evidenceSimon LV, Newton EJ. Basilar Skull Fractures. StatPearls. 2024 Jan:(): [PubMed PMID: 29261908]
Andreu-Arasa VC, Chapman MN, Kuno H, Fujita A, Sakai O. Craniofacial Manifestations of Systemic Disorders: CT and MR Imaging Findings and Imaging Approach. Radiographics : a review publication of the Radiological Society of North America, Inc. 2018 May-Jun:38(3):890-911. doi: 10.1148/rg.2018170145. Epub 2018 Apr 6 [PubMed PMID: 29624481]
Reddy M, Baugnon K. Imaging of Cerebrospinal Fluid Rhinorrhea and Otorrhea. Radiologic clinics of North America. 2017 Jan:55(1):167-187. doi: 10.1016/j.rcl.2016.08.005. Epub [PubMed PMID: 27890184]
Goodmaker C, Hohman MH, De Jesus O. Naso-Orbito-Ethmoid Fractures. StatPearls. 2024 Jan:(): [PubMed PMID: 32491400]
Marchiori E, Hochhegger B, Zanetti G. The halo sign. Jornal brasileiro de pneumologia : publicacao oficial da Sociedade Brasileira de Pneumologia e Tisilogia. 2017 Jan-Feb:43(1):4. doi: 10.1590/S1806-37562016000000354. Epub [PubMed PMID: 28380182]
Béogo R, Bouletreau P, Konsem T, Traoré I, Coulibaly AT, Ouédraogo D. Wire internal fixation: an obsolete, yet valuable method for surgical management of facial fractures. The Pan African medical journal. 2014:17():219. doi: 10.11604/pamj.2014.17.219.3398. Epub 2014 Mar 19 [PubMed PMID: 25237416]
Becker A, Metheny H, Trotter B. Battle Sign. StatPearls. 2024 Jan:(): [PubMed PMID: 30725789]
Kommaraju K, Haynes JH, Ritter AM. Evaluating the Role of a Neurosurgery Consultation in Management of Pediatric Isolated Linear Skull Fractures. Pediatric neurosurgery. 2019:54(1):21-27. doi: 10.1159/000495792. Epub 2019 Jan 23 [PubMed PMID: 30673671]
Patel A, Lofgren DH, Varacallo M. Temporal Fracture. StatPearls. 2024 Jan:(): [PubMed PMID: 30571012]
Reuben AD, Watt-Smith SR, Dobson D, Golding SJ. A comparative study of evaluation of radiographs, CT and 3D reformatted CT in facial trauma: what is the role of 3D? The British journal of radiology. 2005 Mar:78(927):198-201 [PubMed PMID: 15730983]
Level 2 (mid-level) evidenceMyga-Porosiło J, Skrzelewski S, Sraga W, Borowiak H, Jackowska Z, Kluczewska E. CT Imaging of facial trauma. The role of different types of reconstruction. Part II - soft tissues. Polish journal of radiology. 2011 Jan:76(1):52-8 [PubMed PMID: 22802816]
Valsa A, Kumar L, Sumir G, Williams A, Singh M, Victor JV. Submental intubation for airway management of patients with complex caniomaxillofacial injuries: Our experience. Anesthesia, essays and researches. 2012 Jul-Dec:6(2):161-6. doi: 10.4103/0259-1162.108301. Epub [PubMed PMID: 25885610]
Goormans F, Coropciuc R, Vercruysse M, Spriet I, Willaert R, Politis C. Systemic Antibiotic Prophylaxis in Maxillofacial Trauma: A Scoping Review and Critical Appraisal. Antibiotics (Basel, Switzerland). 2022 Apr 5:11(4):. doi: 10.3390/antibiotics11040483. Epub 2022 Apr 5 [PubMed PMID: 35453234]
Level 2 (mid-level) evidenceMundinger GS, Borsuk DE, Okhah Z, Christy MR, Bojovic B, Dorafshar AH, Rodriguez ED. Antibiotics and facial fractures: evidence-based recommendations compared with experience-based practice. Craniomaxillofacial trauma & reconstruction. 2015 Mar:8(1):64-78. doi: 10.1055/s-0034-1378187. Epub 2014 Sep 17 [PubMed PMID: 25709755]
Appelbaum RD, Farrell MS, Gelbard RB, Hoth JJ, Jawa RS, Kirsch JM, Mandell S, Nohra EA, Rinderknecht T, Rowell S, Cuschieri J, Stein DM. Antibiotic prophylaxis in injury: an American Association for the Surgery of Trauma Critical Care Committee clinical consensus document. Trauma surgery & acute care open. 2024:9(1):e001304. doi: 10.1136/tsaco-2023-001304. Epub 2024 Jun 3 [PubMed PMID: 38835634]
Level 3 (low-level) evidenceSingh AK, Dhungel S, Bhattarai K, Roychoudhury A. Do the Benefits of Systemic Corticosteroids Outweigh Adverse Effects During Maxillofacial Trauma Surgery? A Systematic Review and Meta-Analysis. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2021 Jul:79(7):1530.e1-1530.e21. doi: 10.1016/j.joms.2021.02.003. Epub 2021 Feb 9 [PubMed PMID: 33745861]
Level 1 (high-level) evidenceDakir A, Ramalingam B, Ebenezer V, Dhanavelu P. Efficacy of Tranexamic Acid in Reducing Blood Loss during Maxillofacial Trauma Surgery-A Pilot Study. Journal of clinical and diagnostic research : JCDR. 2014 May:8(5):ZC06-8. doi: 10.7860/JCDR/2014/8680.4313. Epub 2014 May 15 [PubMed PMID: 24995234]
Level 3 (low-level) evidenceHassanpour SE, Zirakzadeh H, Aghajani Y. The Effect of Subcutaneous Epinephrine Dosage on Blood Loss in Surgical Incisions. World journal of plastic surgery. 2020 Sep:9(3):309-312. doi: 10.29252/wjps.9.3.309. Epub [PubMed PMID: 33330008]
Pawloski KR, Sevilimedu V, Twersky R, Tadros AB, Kirstein LJ, Cody HS 3rd, Morrow M, Moo TA. Association Between Local Anesthetic Dosing, Postoperative Opioid Requirement, and Pain Scores After Lumpectomy and Sentinel Lymph Node Biopsy with Multimodal Analgesia. Annals of surgical oncology. 2022 Mar:29(3):1737-1745. doi: 10.1245/s10434-021-10981-4. Epub 2021 Oct 25 [PubMed PMID: 34694521]
Kumar K, Kirksey MA, Duong S, Wu CL. A Review of Opioid-Sparing Modalities in Perioperative Pain Management: Methods to Decrease Opioid Use Postoperatively. Anesthesia and analgesia. 2017 Nov:125(5):1749-1760. doi: 10.1213/ANE.0000000000002497. Epub [PubMed PMID: 29049119]
Phang SY, Whitehouse K, Lee L, Khalil H, McArdle P, Whitfield PC. Management of CSF leak in base of skull fractures in adults. British journal of neurosurgery. 2016 Dec:30(6):596-604 [PubMed PMID: 27666293]
Dahlin BC, Waldau B. Surgical and Nonsurgical Treatment of Vascular Skull Base Trauma. Journal of neurological surgery. Part B, Skull base. 2016 Oct:77(5):396-403. doi: 10.1055/s-0036-1583539. Epub 2016 May 24 [PubMed PMID: 27648396]
Kühnel TS, Reichert TE. Trauma of the midface. GMS current topics in otorhinolaryngology, head and neck surgery. 2015:14():Doc06. doi: 10.3205/cto000121. Epub 2015 Dec 22 [PubMed PMID: 26770280]
Brown R, Lozada K, Kadakia S, Gordin E, Ducic Y. Prophylactic Midface Lift in Midfacial Trauma. Facial plastic surgery : FPS. 2017 Jun:33(3):347-351. doi: 10.1055/s-0037-1602165. Epub 2017 Jun 1 [PubMed PMID: 28571074]
Shim HS, Seo BF, Rha EY, Byeon JH. Endotine Midface for Soft Tissue Suspension in Zygoma Fracture. The Journal of craniofacial surgery. 2015 Sep:26(6):e496-500. doi: 10.1097/SCS.0000000000002010. Epub [PubMed PMID: 26267573]
Muradin MS, Seubring K, Stoelinga PJ, vd Bilt A, Koole R, Rosenberg AJ. A prospective study on the effect of modified alar cinch sutures and V-Y closure versus simple closing sutures on nasolabial changes after Le Fort I intrusion and advancement osteotomies. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2011 Mar:69(3):870-6. doi: 10.1016/j.joms.2010.03.008. Epub 2010 Aug 19 [PubMed PMID: 20727648]
Chandra L, Sapru BL, Rai KK, Bhagwath S, Dagur R, Chandra S. Efficacy of v-y closure of upper lip after le fort I osteotomy advancement and superior repositioning on facial esthetics in comparison to simple continuous closure: a statistical analysis. Journal of maxillofacial and oral surgery. 2013 Dec:12(4):366-71. doi: 10.1007/s12663-012-0439-6. Epub 2012 Sep 25 [PubMed PMID: 24431872]
Yuen HW, Hohman MH, Mazzoni T. Mandible Fracture. StatPearls. 2024 Jan:(): [PubMed PMID: 29939527]
Cunningham RM, Maio RF, Hill EM, Zink BJ. The effects of alcohol on head injury in the motor vehicle crash victim. Alcohol and alcoholism (Oxford, Oxfordshire). 2002 May-Jun:37(3):236-40 [PubMed PMID: 12003910]
Murdoch D, Pihl RO, Ross D. Alcohol and crimes of violence: present issues. The International journal of the addictions. 1990 Sep:25(9):1065-81 [PubMed PMID: 2090635]
Johnston JJ, McGovern SJ. Alcohol related falls: an interesting pattern of injuries. Emergency medicine journal : EMJ. 2004 Mar:21(2):185-8 [PubMed PMID: 14988344]
Perkins CS, Layton SA. The aetiology of maxillofacial injuries and the seat belt law. The British journal of oral & maxillofacial surgery. 1988 Oct:26(5):353-63 [PubMed PMID: 3191086]
Hwang K, Kim JH. Effect of Restraining Devices on Facial Fractures in Motor Vehicle Collisions. The Journal of craniofacial surgery. 2015 Sep:26(6):e525-7. doi: 10.1097/SCS.0000000000002030. Epub [PubMed PMID: 26267585]
Cox D, Vincent DG, McGwin G, MacLennan PA, Holmes JD, Rue LW 3rd. Effect of restraint systems on maxillofacial injury in frontal motor vehicle collisions. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2004 May:62(5):571-5 [PubMed PMID: 15122562]
Simoni P, Ostendorf R, Cox AJ 3rd. Effect of air bags and restraining devices on the pattern of facial fractures in motor vehicle crashes. Archives of facial plastic surgery. 2003 Jan-Feb:5(1):113-5 [PubMed PMID: 12533153]
Menon S, Sham ME, Kumar V, Archana S, Nath P, Shivakotee S, Hoda M. Maxillofacial Fracture Patterns in Road Traffic Accidents. Annals of maxillofacial surgery. 2019 Jul-Dec:9(2):345-348. doi: 10.4103/ams.ams_136_19. Epub [PubMed PMID: 31909013]
Aires CCG, Araújo HT, Souza RRL, Santos AJFD, Vasconcellos RJH, Vasconcelos BCDE. Relationship between the use and types of helmets with facial injuries - a prospective study. Revista do Colegio Brasileiro de Cirurgioes. 2023:49():e20223387. doi: 10.1590/0100-6991e-20223387-en. Epub 2023 Jan 6 [PubMed PMID: 36629720]
Clyburn TA, Heydemann JA. Fall prevention in the elderly: analysis and comprehensive review of methods used in the hospital and in the home. The Journal of the American Academy of Orthopaedic Surgeons. 2011 Jul:19(7):402-9 [PubMed PMID: 21724919]
Rubenstein LZ, Josephson KR, Osterweil D. Falls and fall prevention in the nursing home. Clinics in geriatric medicine. 1996 Nov:12(4):881-902 [PubMed PMID: 8890121]