Introduction
Angiographic results alone can guide the decision to perform a percutaneous coronary intervention (PCI). Angiography is used to visually assess the coronary anatomy and determine the degree of stenosis, plaque, or blockage in the coronary artery. The blockage creates visual irregularities of the inner diameter of coronary vessels on angiography, and those irregularities are quantified using a percentage. This percentage correlates with the degree of blockage of the artery. The degree of blockage is usually quantified with a percentage and categorized into mild, moderate/intermediate, or severe.[1][2][3][4]
The assessment of intermediate blockages in coronary artery disease has long been a challenge for interventional cardiologists to determine the appropriate use of angioplasty and stenting. Fractional Flow Reserve (FFR) offers yet another tool to assist in identifying those intermediate blockages. The goal of angioplasty and stenting in the coronary arteries is to increase blood flow to the heart and relieve chest pain. However, studies have shown that if a functional measurement, such as FFR, shows that the flow is not significantly blocked, the blockage or lesion does not need to be revascularized (angioplasty/stenting), and a physician can treat the patient with medical therapy safely. FFR is a guide wire-based procedure that accurately measures blood pressure and flow through an isolated coronary artery segment. A physician can do FFR through a standard diagnostic catheter during a coronary angiogram or cardiac catheterization. FFR has been demonstrated to be useful in assessing “intermediate” blockages (coronary artery disease) to determine the need for angioplasty or stenting (See Image. Fractional Flow Reserve Procedure).[5][6][7][8]
Technique or Treatment
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Technique or Treatment
FFR is obtained as part of diagnostic cardiac catheterization. A guide catheter is utilized to advance the FFR-specific guide wire to the coronary artery orifice. A coronary artery pressure proximal to the stenotic lesion (or Pa) is obtained. The operator (or interventional cardiologist) then advances the FFR-specific guide wire and crosses the intermediate stenotic lesion, allowing coronary artery pressure distal to the stenosis (or Pd) to be obtained. The operator can visualize the pressure sensor angiographically to help ensure proper placement.
FFR measurements must be obtained during maximal blood flow or maximal hyperemia. To achieve maximal hyperemia, a hyperemic stimulus is administered intravenously or intracoronary through the guide catheter, and FFR is monitored for 3 to 4 minutes. Intravenous (IV) adenosine is the most widely used method to induce maximal hyperemia.[9][10]
Equation
FFR is the ratio of the maximum achievable blood flow through a blockage (area of stenosis) to the maximum achievable blood flow in the same vessel in the hypothetical absence of the blockage. It is calculated using a pressure ratio measured distal to the blockage (Pd) and pressure proximal to the blockage (Pa).
The ‘‘normal’’ ratio is expected to be 1. For example, an FFR value of 0.80 means that the maximum blood flow in the coronary artery being measured is 80% of what it would be if the artery were completely normal.
FFR = Pd / Pa
- Pd = pressure distal to the lesion (blockage)
- Pa = pressure proximal to the lesion (blockage)
Interpretation
In utilizing FFR, coronary stenosis can be classified into 3 groups based on physiologic assessment during coronary angiography:
- Ischemia-producing stenosis (FFR less than 0.75)/Revascularization
- Non–ischemia-producing stenosis (FFR greater than 0.80)/Medical Therapy
- Gray zone (FFR 0.75 to 0.80)/Revascularization versus Medical therapy
Clinical Significance
Coronary artery disease (CAD) is 1 of the leading causes of death in the United States, accounting for 1 out of every 4 deaths annually. Coronary revascularization has long been a definitive treatment for reducing symptoms, myocardial infarction, and death in acute coronary syndromes (ACS). However, coronary revascularization is not as clear in stable CAD.
One of the major setbacks with coronary revascularization has been the dependence on angiographic (or visual estimation) analysis of lesions. Many factors are considered during angiography, which ultimately dictates the best treatment course. These include the patient’s symptoms, clinical characteristics, an angiographic appearance of the coronary anatomy, and alternative options, which may include CABG. This leaves a large area of operator variability concerning interpretation and treatment. This lack of clarity has led to inappropriate stenting cases, which have been well publicized. This focus has drawn the attention of media, providers, clinicians, and payors to develop criteria and guidelines that standardize the process of coronary revascularization.
Some trials have been published, helping to establish the Appropriate Use Criteria (AUC) for coronary revascularization. The AUC is the good intent to ensure that the right procedure is performed on the right patient at the right time for the right reasons to achieve the best possible outcome. Reliance on clinical trials, guidelines, and AUC is the framework for coronary revascularization.
The development of FFR arose in the early 1990s to select physiologically significant lesions. The DEFER (2001) trial was the first major landmark trial, showcasing FFR and demonstrating coronary revascularization could be safely deferred when lesions had an FFR greater than 0.75. However, FFR was not widely used in subsequent years for various reasons.
The Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE, 2007) studied PCI in patients with stable CAD and high-grade coronary stenosis, randomizing patients to PCI versus optimal medical therapy. The COURAGE trial failed to demonstrate the benefit of routine revascularization of coronary lesions when compared to optimal medical therapy alone. This landmark trial, inappropriate stenting, and further establishment of AUC and guidelines brought FFR back to the forefront.
Enhancing Healthcare Team Outcomes
The Fractional Flow Reserve versus Angiography for Multivessel Evaluation (FAME, 2009) compared patients undergoing routine PCI for stable multivessel CAD to FFR-guided or angiography-guided PCI, with both groups on OMT. FAME (2009) demonstrated that FFR was superior to traditional angiography-guided PCI among patients with stable multivessel CAD, demonstrating lower 1-year adverse events and reduced costs. This trial paved the way for continued study and evaluation of FFR capability compared to OMT, as demonstrated in the COURAGE (2007) trial. Fractional Flow Reserve versus Angiography for Multivessel Evaluation 2 (FAME 2, 2011) studied the role of PCI among patients with stable single or multivessel CAD with physiologically significant coronary lesions. In contrast to FAME, FAME 2 focused on patients with FFR less than or equal to 0.80, comparing PCI to OMT alone. Among patients with stable CAD with FFR less than or equal to 0.80, PCI demonstrated overall better outcomes concerning death, nonfatal MI, and urgent revascularization. The preponderance of clinical trial evidence for FFR-driven revascularization prompted the incorporation of FFR into the 2011 American College of Cardiology (ACC)/American Heart Association (AHA) and 2014 European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Guidelines.
Media
(Click Image to Enlarge)
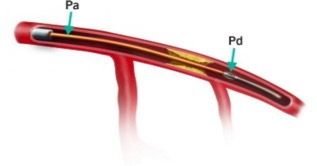
Fractional Flow Reserve Procedure. The assessment of intermediate blockages in coronary artery disease has been a challenge for interventional cardiologists to determine the appropriate use of angioplasty and stenting. FFR is another tool to assist in the identification of intermediate blockages.
Contributed by St Jude Medical
References
Demir OM, Mitomo S, Mangieri A, Ancona MB, Regazzoli D, Lanzillo G, Giannini F, Testa L, Wijns W, Colombo A, Latib A. Diagnostic Accuracy of Microcatheter Derived Fractional Flow Reserve. The American journal of cardiology. 2019 Jul 15:124(2):183-189. doi: 10.1016/j.amjcard.2019.04.038. Epub 2019 Apr 25 [PubMed PMID: 31104777]
Leipsic J, Anastasius M, Blanke P. Plaque, Pressure, and Risk: The Story Unfolds. Journal of the American College of Cardiology. 2019 May 21:73(19):2425-2426. doi: 10.1016/j.jacc.2019.03.465. Epub [PubMed PMID: 31097162]
Villines TC. Computed Tomography-Derived Fractional Flow Reserve: A Needed ADVANCE or Expensive Nicety? JACC. Cardiovascular imaging. 2020 Jan:13(1 Pt 1):106-108. doi: 10.1016/j.jcmg.2019.04.005. Epub 2019 May 15 [PubMed PMID: 31103582]
Lee JM, Choi KH, Koo BK, Park J, Kim J, Hwang D, Rhee TM, Kim HY, Jung HW, Kim KJ, Yoshiaki K, Shin ES, Doh JH, Chang HJ, Cho YK, Yoon HJ, Nam CW, Hur SH, Wang J, Chen S, Kuramitsu S, Tanaka N, Matsuo H, Akasaka T. Prognostic Implications of Plaque Characteristics and Stenosis Severity in Patients With Coronary Artery Disease. Journal of the American College of Cardiology. 2019 May 21:73(19):2413-2424. doi: 10.1016/j.jacc.2019.02.060. Epub [PubMed PMID: 31097161]
Neupane S, Singh H, Edla S, Altujjar M, Yamsaki H, Lalonde T, Rosman HS, Eggebrecht H, Mehta RH. Meta-analysis of fractional flow reserve guided complete revascularization versus infarct related artery only revascularization in patients with ST-elevation myocardial infarction and multivessel coronary artery disease. Coronary artery disease. 2019 Sep:30(6):393-397. doi: 10.1097/MCA.0000000000000740. Epub [PubMed PMID: 31094897]
Level 1 (high-level) evidenceMasdjedi K, van Zandvoort LJC, Balbi MM, Gijsen FJH, Ligthart JMR, Rutten MCM, Lemmert ME, Wilschut JM, Diletti R, de Jaegere P, Zijlstra F, Van Mieghem NM, Daemen J. Validation of a three-dimensional quantitative coronary angiography-based software to calculate fractional flow reserve: the FAST study. EuroIntervention : journal of EuroPCR in collaboration with the Working Group on Interventional Cardiology of the European Society of Cardiology. 2020 Sep 18:16(7):591-599. doi: 10.4244/EIJ-D-19-00466. Epub [PubMed PMID: 31085504]
Level 1 (high-level) evidenceFournier S, Toth GG, Colaiori I, De Bruyne B, Barbato E. Long-Term Patency of Coronary Artery Bypass Grafts After Fractional Flow Reserve-Guided Implantation. Circulation. Cardiovascular interventions. 2019 May:12(5):e007712. doi: 10.1161/CIRCINTERVENTIONS.118.007712. Epub [PubMed PMID: 31084238]
Whayne TF Jr, Sousa MJ, Abdel-Latif A. Use and Value of Fractional Flow Reserve in Coronary Arteriography. Angiology. 2020 Jan:71(1):5-9. doi: 10.1177/0003319719848559. Epub 2019 May 13 [PubMed PMID: 31084188]
Abo-Aly M, Lolay G, Adams C, Ahmed AE, Abdel-Latif A, Ziada KM. Comparison of intracoronary versus intravenous adenosine-induced maximal hyperemia for fractional flow reserve measurement: A systematic review and meta-analysis. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography & Interventions. 2019 Nov 1:94(5):714-721. doi: 10.1002/ccd.28317. Epub 2019 May 9 [PubMed PMID: 31074100]
Level 1 (high-level) evidencePatel AR, Maffessanti F, Patel MB, Kebed K, Narang A, Singh A, Medvedofsky D, Zaidi SJ, Mediratta A, Goyal N, Kachenoura N, Lang RM, Mor-Avi V. Hemodynamic impact of coronary stenosis using computed tomography: comparison between noninvasive fractional flow reserve and 3D fusion of coronary angiography with stress myocardial perfusion. The international journal of cardiovascular imaging. 2019 Sep:35(9):1733-1743. doi: 10.1007/s10554-019-01618-5. Epub 2019 May 9 [PubMed PMID: 31073698]