Anatomy, Bony Pelvis and Lower Limb: Arches of the Foot
Anatomy, Bony Pelvis and Lower Limb: Arches of the Foot
Introduction
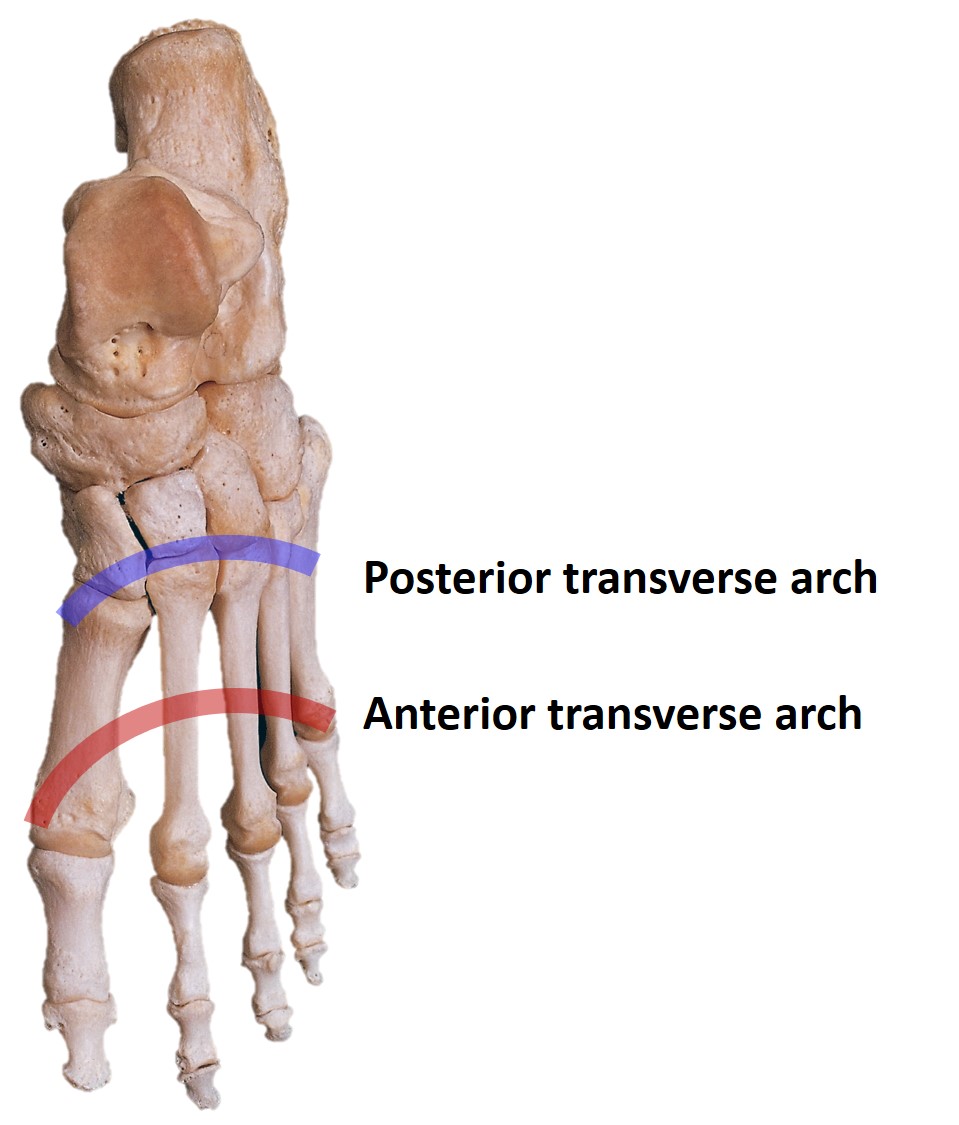
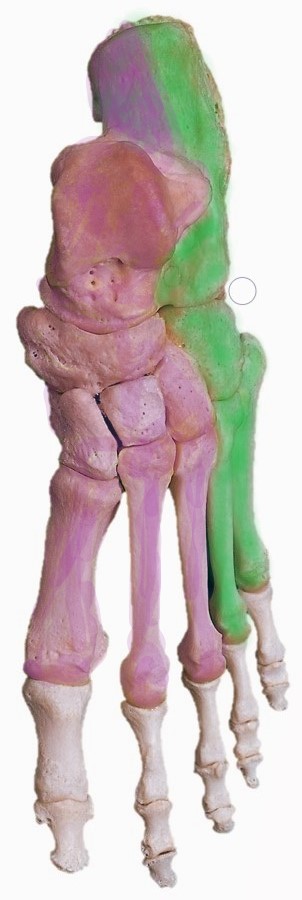
An arched foot is characteristic of humans, distinguishing it from other primates. Arches of the foot help in providing upright posture and weight bearing. The human foot has 2 longitudinal (medial and lateral) and 2 transverse arches (anterior and posterior transverse arches) (see Image. Transverse Arches of the Foot).[1][2] These arches are formed by the shapes of tarsals and metatarsals and are supported by ligaments and extrinsic and intrinsic muscles of the foot. Among the longitudinal arches, the medial arch has more height, while the anterior arch is complete among the transverse arches, while the posterior arch is half dome-shaped and incomplete. These arches make the sole concave so that our footprint is incomplete. It is present since birth but is masked by the presence of the fat pad in children.[3][4]
These arches of the foot provide a flexible platform to support body weight and act as a multisegmented lever for propulsion in walking, running, and jumping. An arched foot can absorb shock and adapt to uneven surfaces. The foot has to suffer from deformities due to congenital anomalies or acquired injury by improper shoewear or high heels.[3][4]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Functions of Arches of the Foot
Arches of the foot are important structural adaptations for function. Various functions of the arches of the foot include:
- Help in proportional body weight distribution to weight-bearing area.
- Act as a segmented lever, which helps propel the body forward in walking, running, and jumping.[1]
- Act as a shock absorber in stepping & jumping movements.[2][4]
- Act as springs board.
- Adapt the foot on an uneven surface.[4]
- Protect plantar vessels and nerves.
- The arched foot is dynamic and pliable.[4][5]
- When the foot is on the ground, the arches flatten somewhat. When the foot is off the ground, arches restore their contour.
Classification of the Arches of the Foot
- Longitudinal arch (see Image. Longitudinal Arch [Lateral])
- Medial longitudinal arch
- Lateral longitudinal arch
- Transverse arch
- Anterior transverse arch
- Posterior transverse arch
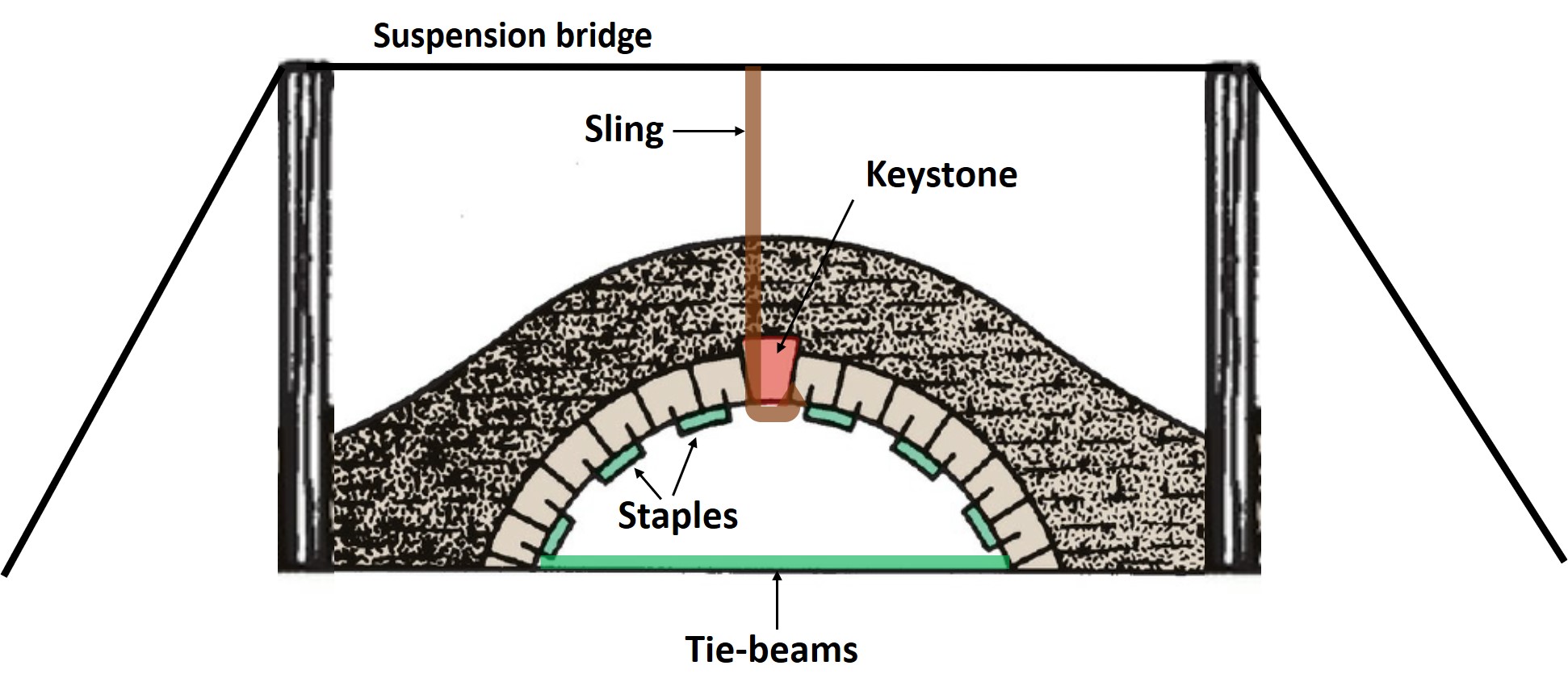
The formation of arches of the foot is compared with the stone bridge having two ends, pillars, a summit, and a keystone, and their support mechanism is also compared with the same as in the stone bridge, eg, intersegmental ties (staples), tie-beams, and slings (see Image. Factors Maintaining Stone Bridge Arch).
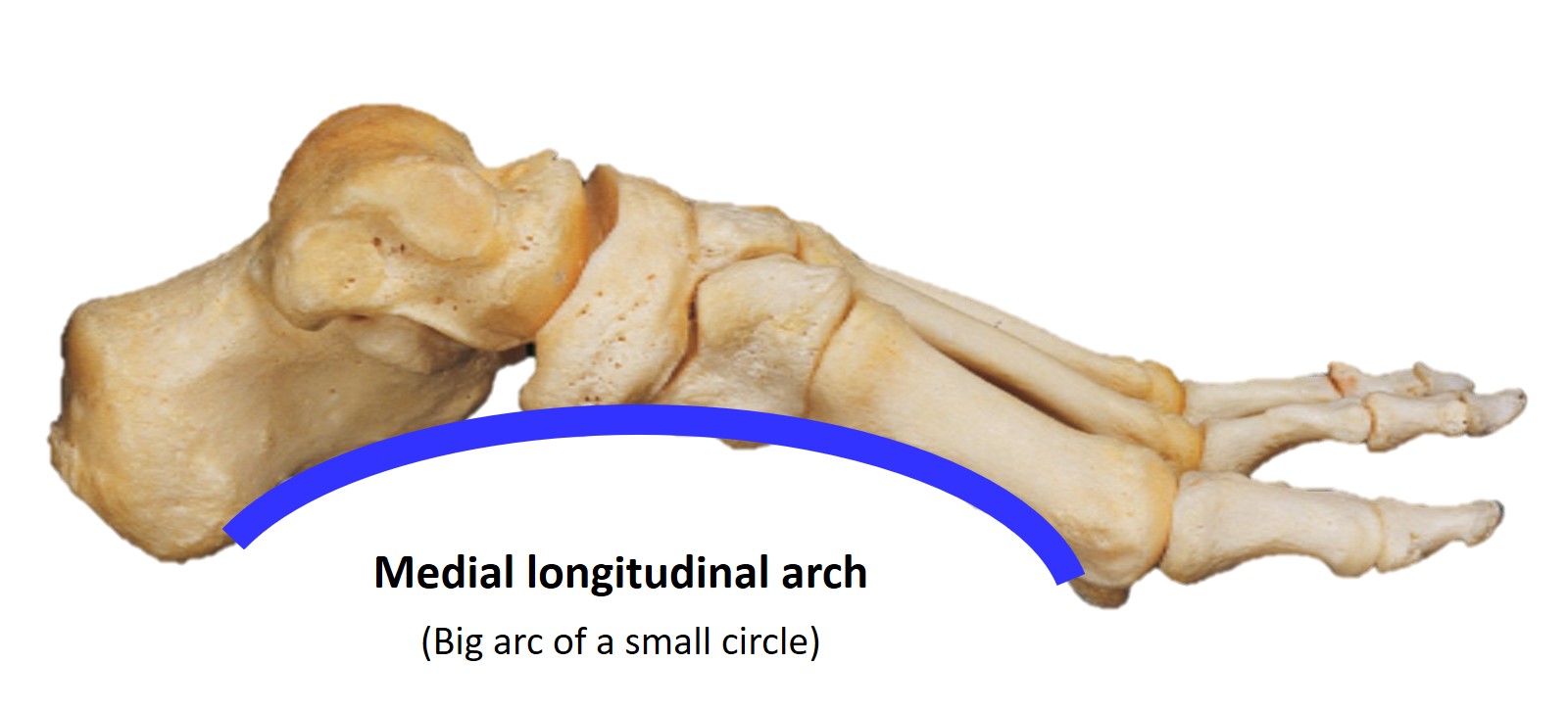
Medial Longitudinal Arch
- Bones forming medial longitudinal arch include the following:
- Characteristics of the medial longitudinal arch
- It is higher and represents a big arc of a small circle
- Having more bones and more joints, so more mobile.
- Have the property of resiliency and shock absorber.[5]
- Two ends of the medial longitudinal arch
- Anterior end
- Heads of first, second, and third metatarsals
- Phalanges do not take part in the formation of the arch.
- Posterior end
- Medial tubercle of calcaneum
- Anterior end
- Pillars of the medial longitudinal arch
- Anterior pillar
- It is long and weak.
- Formed by the talus, navicular, three cuneiforms, first, second and third metatarsals
- Posterior pillar
- It is short & strong.
- It is formed by the medial half of the calcaneum.
- The Summit of the medial longitudinal arch
- It lies at a higher level than the lateral arch.
- It lies at the level of the superior trochlear articular surface of the talus.
- The main joint of the medial longitudinal arch
- The most vulnerable part of the medial longitudinal arch
- Head of the talus, which acts as a keystone.[4] See Image. Medial Longitudinal Arch of the Foot.
Factors Maintaining the Medial Longitudinal Arch
- Shape of bone
- Wedge-shaped bone, their edge forms plantar surface
- Head of the talus act as a keystone.[4]
- Intersegmental ties (staples)
- Plantar ligaments & spring ligaments; are further supported by slips of the tibialis posterior tendon.
- Tie-beams
- Plantar aponeurosis
- Abductor hallucis
- Medial part of flexor digitorum brevis
- Medial part of flexor digitorum longus
- Tendon of flexor hallucis longus.[6]
- Suspending factors
- In standing position: Plantar ligaments and plantar aponeurosis provide support.
- During locomotion: Muscles become an active part of the maintenance of arches.
- The plantar aponeurosis act as a “windlass mechanism” to maintain the arch of the foot.[4][5]
- Failure of arch support depends on the duration of stress and not on the severity of stress foot bears.
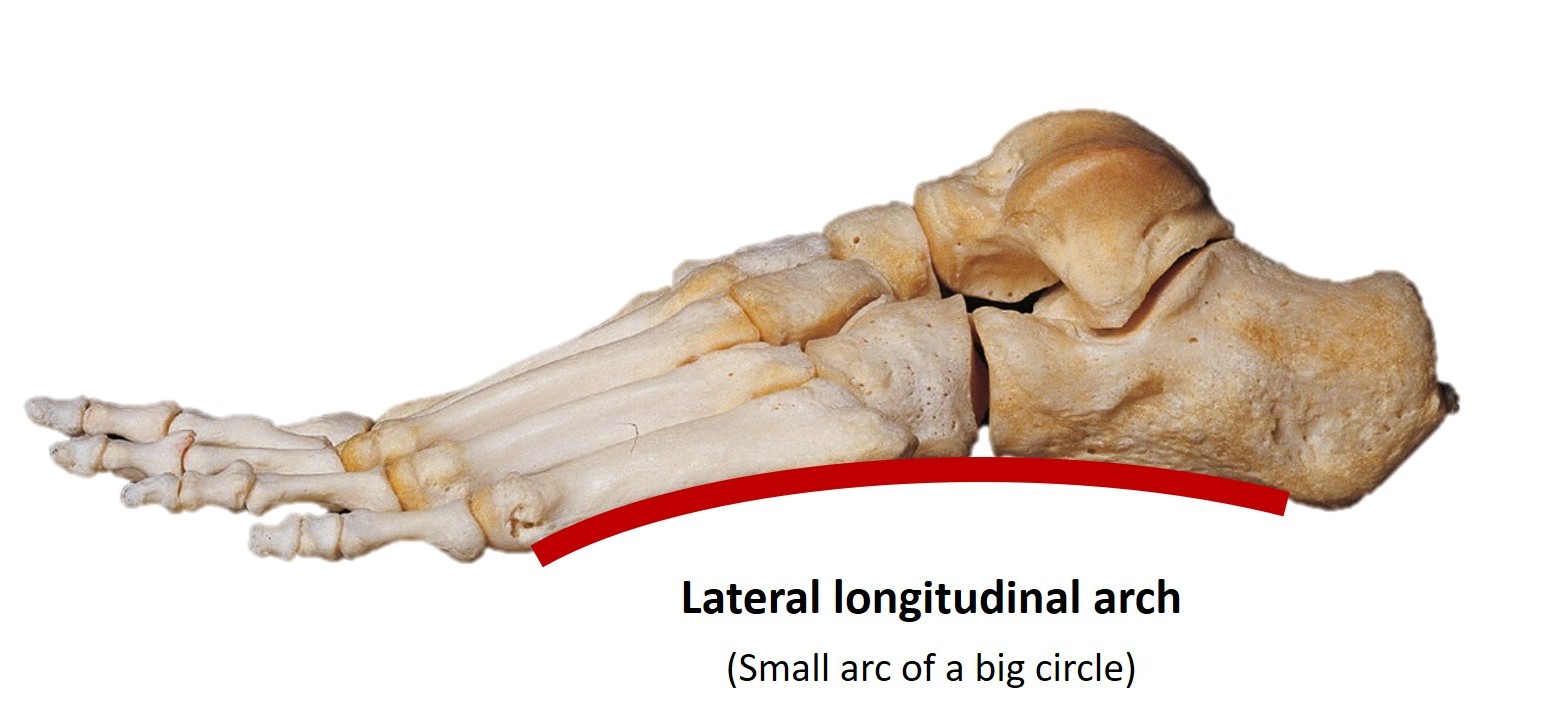
Lateral Longitudinal Arch
- Bones forming the lateral longitudinal arch include the following:
- Lateral part of the calcaneum
- Cuboid
- Fourth and fifth metatarsals.[4]
- Characteristics of the lateral longitudinal arch are as follows:
- Two ends of the lateral longitudinal arch:
- Anterior end
- Heads of the fourth and fifth metatarsals
- Posterior end
- Lateral tubercle of calcaneum.
- Anterior end
- Pillars of the lateral longitudinal arch:
- Anterior pillar
- Long and weak
- It is formed by the cuboid, fourth and fifth metatarsals.
- Posterior pillar
- Short and strong
- Formed by the lateral half of calcaneum
- Anterior pillar
- Summit of the lateral longitudinal arch
- The main joint of the lateral longitudinal arch
- Calcaneo-cuboid joint[3]
- The most vulnerable part of the lateral longitudinal arch
- Calcaneo-cuboid joint
Factors Maintaining the Lateral Longitudinal Arch
- Shape of bone
- Calcanean angle of the cuboid, which maintains the upward tilt of the long axis of the calcaneum
- Intersegmental ties (staples)
- Long plantar ligament
- Short plantar ligament
- Dorsal metatarsocuboid ligament
- Dorsal calcaneocuboid ligament
- Tie-beams
- Plantar aponeurosis
- Abductor digiti minimi
- Lateral part of flexor digitorum brevis
- Lateral part of flexor digitorum longus
- Tendon of flexor digiti minimi brevis.[6]
- Suspending factors
Summary of Longitudinal Arches of the Foot
| Characteristics | Medial longitudinal arch | Lateral longitudinal arch |
| Features | Higher, more mobile, resilient, and shock absorber | Lower, less mobile, transmits weight, rigid |
| Anterior end | Heads of first, second, and third metatarsals | Heads of the fourth and fifth metatarsals |
| Posterior end | Medial tubercle of the calcaneum | Lateral tubercle of the calcaneum |
| Summit | The superior articular surface of the talus | The articular surface on the superior surface of calcaneum at the level of the subtalar joint |
| Anterior pillar | Talus, navicular, three cuneiforms, and first to third metatarsals | Cuboid, fourth and fifth metatarsals |
| Posterior pillar | The medial half of the calcaneum | The lateral half of the calcaneum |
| Main joint | Talocalcaneonavicular joint | Calcaneocuboid joint |
| Bony factor | The head of the talus is the keystone. | A cuboid is a keystone. |
| Intersegmental ties | Spring ligament | Long plantar ligament and short plantar ligament |
| Tie beams | Medial part of the plantar aponeurosis, abductor hallucis, medial part of the flexor digitorum brevis | Lateral part of the plantar aponeurosis, Abductor digiti minimi, lateral part of the flexor digitorum brevis |
| Slings | Tibialis anterior (action from above), tibialis posterior (action from below) | Peroneus brevis and peroneus tertius (action from above) |
Transverse Arches of the Foot
For modulating the elasticity and rigidity of the foot, the midfoot plays an important role. Transverse arch act as a stiff spring lever that stores the energies and will be utilized during the propulsion of the foot. The transverse arch modulates the biomechanics of the longitudinal arch according to the need.[4]
During the stance phase, three points that touch the ground are the head of the first and fifth metatarsals, and the heel or calcaneum suggests that the foot is elevated at the second to fourth metatarsals indicating a transverse arch.[9]
Transverse arches of the foot are of two types, anterior and posterior transverse arches.
Anterior Transverse Arch
- It is a complete arch because both ends touch the ground.
- Formed by the head of the first to fifth metatarsals.[2][4]
Posterior Transverse Arch
- Only the lateral end touches the ground, making it an incomplete arch.
- It only forms a “half dome.” This arch completes by a similar half dome of the opposite side arch.[2]
- It is formed by the base of the metatarsals, tarsals, and metatarsals.[2][4]
Factors Maintaining the Transverse Arc
- Shape of bone
- Wedge-shaped 3 cuneiforms and base of middle three metatarsals
- Intersegmental ties
- Deep transverse ligament and intrinsic plantar ligament
- Dorsal interossei and adductor hallucis[6]
- Tie-beams
- Tendon of peroneus longus and tendon of tibialis posterior
- Suspending factors
- Peroneus tertius, peroneus brevis, and tibialis anterior.[8]
Summary of the Transverse Arches of the Foot
| Characteristics | Anterior Transverse Arch | Posterior Transverse Arch |
| Formation | Heads of first to fifth metatarsals | Navicular, three cuneiforms, bases, and shafts of metatarsals |
| Features | complete arch | Incomplete. The arch is half dome-shaped. Raised medially. |
| Bony factor | Round shaped | Wedge-shaped |
| Intersegmental ties | Dorsal interossei muscles | Dorsal interossei muscles |
| Tie beams | Adductor hallucis, deep transverse metatarsal ligaments | Flexor hallucis brevis, intertarsal ligaments, and tarsometatarsal ligaments |
| Slings | peroneus longus, tibialis posterior | peroneus longus, tibialis posterior |
Carpopedal unit is a complementary concept to the common longitudinal division of the foot (lateral and medial longitudinal arch) or transverse division of the foot (forefoot, midfoot, hindfoot). The carpopedal unit is formed by the forefoot, midfoot, and calcaneus, bounded to each other by the spring ligament, bifurcate ligament, and calcaneocuboid ligament.[3] It articulates with the talus by talonavicular, anterior, middle, and posterior subtalar joints. The talus and the tibia, and the fibula form the same functional unit as the talo-tibiofibular complex.[3]
Embryology
The hind limb bud develops as bulging on the ventrolateral surface in the 4th week of the embryo by the proliferation of the somatopleuric layer of lateral plate mesoderm opposite to L3 to L5 somites covered by ectoderm. The limb bud grows from the proximal to the distal, and a primitive footplate is formed at 4.5 weeks.[6][10]
Following interactions between epithelium and mesenchyme, an apical ectodermal ridge (AER) is formed from ectoderm. Mesenchyme will condense to form ligaments and the skeleton of the hindlimb, While ectoderm forms the skin and its appendages. AER has a role in the development of skeletal elements by releasing various signals. Limb development may be hampered if AER is affected or removed.[11][12]
Around the 6th week cartilaginous skeleton forms by chondrification. Ossification of cartilaginous models begins at the 10th week, which may continue after birth till puberty to complete the secondary ossification process. In some tarsal bones, endochondral ossification starts after birth.[12]
The Human pentadactylous hind limb has been differentiated into three segments.
- Stylopodium, or proximal segment, gives rise to the femur.
- Zeugopodium or intermediate segment gives rise to two skeletal elements - tibia and fibula.[11]
- Autopodium gives rise to skeletal elements of the foot (metatarsals and phalanges). Mesopodium considers a segment between autopodium and zeugopodium, giving rise to tarsals.[13] Autopodium forms a digital plate demarcated into digital rays, which form digits, and interdigital tissue between digital rays disintegrates by apoptosis. As per the position, digits are given numbers.[13]
During 6th week, the paddle-shaped foot lies inverted and equinus in position. During the 8th week, the forefoot is adducted, and notches between the toes are visible. During the 9th week, all digits are formed, heads of the first and fifth metatarsals drop downward, and the transverse arch of the foot form.[14]
Around the 12th week, the foot rotates and comes to lie in the supine position. Between the 13 to 16th week, the size of the limb increases, the equinus level of the foot decreases, and the foot lie right angle to the lower part of the leg.
At the time of birth, due to the presence of a fatty pad in the sole, arch of the foot is not visible. This fatty pad protects the arch and prevents compressions of the nerves and blood vessels of the sole. At around 5 to 6 years, normal arches become apparent in children. During weight-bearing, arches disappear as flexible pes planus.[15]
Blood Supply and Lymphatics
The foot is supplied by branches from the anterior and posterior tibial arteries. The anterior tibial artery continues as the dorsalis pedis artery when it passes between the line joining two malleoli and enters into the foot. The dorsalis pedis artery provides branches like medial malleolar, lateral malleolar, medial tarsal, lateral tarsal, arcuate, and first dorsal metatarsal arteries, which supply the dorsum of the foot.[16]
It then runs toward the first web space and passes between two heads of the dorsal interossei, and enters into the sole to join the plantar arch. Dorsal metatarsal arteries, except the first one, arise from the arcuate artery, which further divides into dorsal digital arteries to supply the adjacent side of the toes. Perforating arteries connect the dorsal and plantar arteries.[17]
The plantar aspect of the foot is supplied by medial calcaneal, medial plantar, and lateral plantar arteries (branches of the posterior tibial artery). The medial plantar run along the medial border of the sole, while the lateral plantar artery runs along the lateral side of the sole.[16] The lateral plantar artery gives rise to the superficial branch and deep branch, among which the deep branch continues as a deep plantar arch that joins with the dorsalis pedis artery. The deep arch further divides and provides plantar metatarsal and plantar digital arteries.
The heel of the foot is supplied by anastomosis of the lateral calcaneal (branch of peroneal artery) and medial calcaneal arteries.[16][17]
In the foot, digital veins join to form dorsal and plantar venous arches on the dorsal and ventral surfaces of the foot, respectively. Digital veins run in the interdigital cleft and drain blood from the adjacent side of the toes.[18] The plantar venous arch continues as the medial and lateral plantar vein accompanies the respective arteries, and they join to form a posterior tibial vein. In the dorsum of the foot lateral marginal vein joins the dorsal venous arch laterally to form a small saphenous vein. In contrast, the medial marginal vein joins the dorsal venous arch medially to form a great saphenous vein. The femoral vein receives blood from the great saphenous vein, while the popliteal vein receives blood from the small saphenous vein and the posterior tibial vein.[18][19]
Superficial lymphatics of the foot converge on the medial and lateral sides. Superficial lymphatics from the medial side pass along with the great saphenous vein to drain into the superficial inguinal group of lymph nodes. In contrast, superficial lymphatic from the lateral side runs along with a small saphenous vein and drains into the popliteal group of lymph nodes, Which also receives deep lymphatics of the foot and leg. The Popliteal group ultimately drains into the deep inguinal group of lymph nodes.[20][21]
Nerves
The foot is innervated by branches from the medial plantar nerve, lateral plantar nerve, medial calcaneal, inferior calcaneal, superficial peroneal, deep peroneal, saphenous, and sural nerves.[22]
Common peroneal nerve wind around the neck of the fibula and divides into superficial and deep peroneal nerves.[23] Superficial peroneal nerve supplies evertors of the foot (peroneus longus and peroneus brevis) and, in the lower part of the leg, becomes cutaneous, carries sensory information from the anterolateral aspect of the leg, and divides into lateral and medial branches to supply most of the dorsum of the foot except first web space, medial and lateral borders.[22]
The deep peroneal nerve passes in front of the interosseous membrane. It lies lateral to the anterior tibial artery in the upper and lower part of the leg while it lies anteriorly in the middle part giving rise to its name, nervi hesitant. It supplies muscles of the anterior aspects of the leg responsible for dorsiflexion of the ankle and toes and invertors of the foot (tibialis anterior, extensor hallucis longus, extensor digitorum longus, and peroneus tertius).[24] In the foot, its lateral branch passes deep to the extensor digitorum brevis and supplies it through the pseudoganglion. The deep peroneal nerve also provides sensory innervation to the dorsal aspect of the first web space.[24][23]
The posterior division of the femoral nerve gives rise to the cutaneous branch, the saphenous nerve, which pierces the roof of the adductor canal and runs along with great saphenous vein in the leg and supplies skin of the medial side of the ankle and foot up to the ball of the great toe.[23]
The tibial nerve gives rise to the sural nerve, which joins with the sural communicating nerve that arises from the common peroneal nerve. It passes between the medial and lateral heads of the gastrocnemius muscle and then runs subcutaneously along with a small saphenous vein. It provides sensory branches to the lower part of the lateral side of the back of the leg and the lateral border of the foot up to the tip of the little toe.[22][23]
The heel region of the foot is supplied by medial and inferior calcaneal nerves. Proximal to the tarsal tunnel, the tibial nerve gives rise to the medial calcaneal nerve, which pierces the flexor retinaculum and then provides sensory supply to the posteromedial aspect of the heel. The lateral plantar nerve gives its first branch inferior calcaneal nerve, which provides motor fibers to the abductor digiti minimi muscle and sensory supply to the anterior part of the calcaneus.[23][25]
The tibial nerve divides into two terminal branches, lateral and medial plantar nerves deep to the flexor retinaculum. The medial plantar nerve passes beneath the abductor hallucis and flexor hallucis longus muscles to enter the sole. It will provide motor branches to the abductor hallucis, flexor digitorum brevis, first lumbrical, and flexor hallucis brevis muscle.[23] Medial plantar divides into the common plantar nerves, which further branch into proper digital nerves to provide sensory supply to the medial side of the foot, the whole medial three digits, and the lateral side of the fourth digit.[23]
The lateral plantar nerve runs obliquely beneath the flexor digitorum brevis muscle. The main trunk of the lateral plantar nerve provides motor supplies to abductor digiti minimi and flexor digitorum accessorius and sensory to the lateral part of the sole. It further divides into superficial and deep branches.[24] The superficial branch of the lateral plantar nerve gives motor innervations to flexor digiti minimi brevis, third plantar, and fourth dorsal interossei muscles while providing sensory supply to lateral one and half digits.[26]
The deep branch of the lateral plantar nerve innervates all lumbricals except first, all plantar and dorsal interossei except the fourth web space, adductor hallucis muscles. In the third web space, there is communication occurs between lateral and medial plantar nerves, which is the most common site for Morton neuroma.[24][23][26]
Muscles
The following extrinsic and intrinsic muscles provide support and help in the maintenance of the arches of the foot. In the standing position, plantar ligaments and aponeurosis provide support, while during locomotion, especially in the stance phase, for shock absorption and weight transmission, muscles play a key role.
Intrinsic Muscles of the Foot
Abductor hallucis: It is the muscle of the first layer of the sole, causing abduction of the great toe. Support the medial longitudinal arch of the foot as a tie beam.[6]
Flexor digitorum brevis: It also lies in the first layer of the sole, causing flexion at the proximal interphalangeal and metatarsophalangeal joints. It acts as a tie beam and supports both longitudinal arches of the foot.[6]
Abductor digiti minimi: The first layer of muscle of the sole lies on the lateral side, causing abduction of the little toe. Support the lateral longitudinal arch of the foot as a tie beam.
Lumbricals: It arises from tendons of flexor digitorum longus, so they do not have a bony origin. It prevents buckling of the toes and supports the arches of the foot.
Flexor hallucis brevis: It causes flexion of the great toe and supports the medial longitudinal arch.[6]
Adductor hallucis: Muscle of the third layer of the sole, having two heads of origin, act as intersegmental ties as well as tie-beam for the transverse arch of the foot. Its unopposed action may predispose to hallux valgus.
Flexor digiti minimi brevis: It causes flexion of the little toe and supports the lateral longitudinal arch of the foot as a tie beam.[6]
Dorsal Interossei: They lie in the fourth layer of the sole, causing abduction of the toes and assisting extensor tendons in the dorsiflexion of the toes. Four dorsal interossei originate from the adjacent side of the metatarsals, so they act as intersegmental ties or staples for the transverse arch of the foot.
Extrinsic Muscles Act on the Foot
Tibialis posterior: Its slips of insertion on the plantar surface of the foot supports the longitudinal and transverse arches of the foot from below as sustentacular action and also act as intersegmental ties or staples. Also, help the foot to adjust to the uneven surface by causing inversion.[7]
Flexor digitorum longus: It enters into the sole by passing through the tarsal tunnel and runs in the second layer of the sole, causing flexion at the distal interphalangeal joint and assisting for flexion of the proximal joint, including plantar flexion at the ankle joint. It also supports the longitudinal arch as a tie beam.
Flexor hallucis longus: A muscle of the back of the leg enters into the sole and causes flexion of the interphalangeal joint of the great toe. It also assists in supporting the medial longitudinal arch of the foot as a tie beam.[7]
Tibialis anterior: It helps the foot to adjust on uneven surfaces by causing inversion. It acts as slings to pull the medial longitudinal arch of the foot upwards. Also, along with peroneus longus, it supports the longitudinal arch of the foot by elevation.[1][4]
Peroneus longus: Muscle of the lateral compartment of the leg, also enter into the sole by passing through a cuboidal groove and inserts into the medial cuneiform and base of the first metatarsal. It supports the longitudinal arch as sustentacular action and slings along with the tibialis anterior to pull the longitudinal arch upwards and also acts as a tie beam for the transverse arch.[8]
Peroneus brevis: It is also the muscle of the lateral compartment of the leg and maintains the lateral longitudinal arch as sling action.[8]
Peroneus tertius: It also assists the peroneus brevis in maintaining the lateral longitudinal arch of the foot. Peroneus longus, brevis, and tertius muscles cause eversion of the foot, so they help adjust the foot on an uneven surface.[1][4]
Physiologic Variants
Depending upon the variation in the height range and the morphology of the longitudinal and transverse arches of the foot, the physiological variant may include pes rectus, pes planus, and pes cavus.
Pes Rectus
The height of the arches of the foot lies within normal range, and when we bisect the posterior surface of the calcaneum, it passes perpendicularly with respect to the ground.[27][2]
Pes Planus / Flatfoot
In children, flatfoot is seen as an asymptomatic physiological deviation. The height of the arches of the foot lies below the normal range and is associated with an everted calcaneus. Due to the presence of a fatty pad in the sole, the foot touches the ground nearly completely. Later on, because of the further growth of the skeleton, the arches of the foot can be visible.[27]
Pes Cavus
The height of the arches of the foot lies above the normal range and is associated with an inverted calcaneus.[2]
Every child has an individual timeline for developing arches of the foot, which can also be influenced by gender and obesity-like risk factors.[27]
Gait Cycle
Everybody has different gait cycles, which consist of two phases, e.g., the stance phase and the swing phase. The majority (60%) of the gait cycle consists of the stance phase, while the swing phase makes up 40%. The stance phase ranges from heel strike to toe-off, whereas toe-off to heel strike is the swing phase.[28] The swing phase is further divided into three rockers as following
- The momentarily occurring transition from heel strike to the flat foot is known as the initial rocker. On heel strike, ground reaction forces act posterior to the ankle joint, which leads to ankle plantarflexion. In this controlled movement, eccentric contraction of the tibialis anterior plays a key role in the first rocker of the stance phase.
- The period between a flat foot to heel off marks the second or ankle rocker. The whole body moves over the foot in this phase leading to ankle dorsiflexion of 10 degrees. The eccentric contraction of the gastrocnemius and soleus muscle control this ankle dorsiflexion
- The third rocker, also known as the forefoot rocker, begins with the heel-off and concludes with the toe-off. The ankle moves from dorsiflexion to abrupt plantar flexion, which requires concentric contraction of the triceps surae. The point of ground reaction forces stays anterior to the ankle joint in both the second and third rocker phases.
Ankle dorsiflexion is required in the swing phase to clear the ground. However, ground reaction forces have no role in this phase as the foot is off the ground.[29][30]
Applied Anatomy
Ankle dorsiflexion of 10 degrees and plantarflexion of 15 degrees are necessary for normal walking. The talus is a wedge-shaped bone with a broad anterior articulating surface and has a longer lateral wall than the medial aspect. In ankle dorsiflexion, prolonged movement on the lateral aspect of the talus results in the talus external rotation. In addition to that, ankle dorsiflexion is linked with subtalar eversion. The wide joint contact area during dorsiflexion is inversely proportional to joint stress forces. Plantarflexion is coupled with subtalar inversion, talar internal rotation, and high joint reaction forces. When loaded, the fibula displaces 1 to 3 mm distally and rotates internally.[31][32]
In the first and second rockers, the foot acts as a shock absorber and movable adaptor, while in the third rocker, it serves as a rigid lever. When the ankle joint's plantar flexion drives the foot to the ground, the soft forefoot pad absorbs energy. The eversion of subtalar joints makes transverse tarsal joints parallel to each other, resulting in a flexible and adaptable foot in the second rocker. The plantarflexion of the ankle in the third rocker leads to an inversion of the ankle and subtalar joints. The transverse tarsal joints (talonavicular and calcaneocuboid articulations) are rotated by the subtalar inversion into a non-parallel alignment, creating a stiff foot that aids in the body's forward propulsion. The windlass effect is created by toe dorsiflexion and tightening of the plantar fascia, which provides a stiff high arched foot.[33][34]
Surgical Considerations
Abnormalities of the arches of the foot lead to various clinical consequences.
Pes Planus / Flat Foot
Decrease or absent longitudinal arch of the foot so that the whole foot touches the ground. When weight bearing arch disappears, and while the foot is not bearing weight, it reappears as the normal arch is referred to as flexible pes planus. Flexible flat feet can be differentiated by toe raise/ jack test.[1][15]
The forefoot is supinated, while the midfoot is in neutral or abduction. The hind foot is usually valgus/everted, with the Ankle in plantar flexion. The fundamental anomaly in flexible flatfoot (FFF) is excessive ligamentous laxity, while bone abnormalities constitute a secondary abnormality. Conditions that look like flat feet, like a bulky fat pad in pediatric patients, foot edema, or any benign or malignant neoplasm of the foot; should be excluded.[15]
It may occur secondary to dysfunction of the posterior tibial tendon, trauma to the hindfoot or midfoot, midtarsal joint dislocation or subluxation, injury to ligaments like spring ligament/long and short plantar ligaments, or plantar fascia. Usually, rest, proper footwear, and NSAIDs are sufficient for management. Surgery can be considered in resistant cases.[1][15]
The weight-bearing anteroposterior (AP), lateral, and oblique radiographs are required for the planning and diagnosis of this pathological entity. The center of rotation of angulation (CORA) is measured to determine the apex of deformity via the talo-first metatarsal angle, as shown in the illustration. The collapsed medial arch is measured by a calcaneal pitch, and the increased talocalcaneal angle depicts hind foot vagus deformity.[35]
Pes Cavus / High-arched Foot
In this deformity, there is an abnormally increased height of the longitudinal arch of the foot. The higher arch decreases shock absorbing ability, so more pressure is exerted on the ball of the great toe and heel. The most common causes of pes cavus include neurological disorders, injury, neglected clubfoot, or idiopathy.[36]
In pes cavus, weakness of intrinsic foot muscles and overpowering of sling muscle peroneus longus and tibialis posterior muscle causes elevation of the arch of the foot. Surgical intervention should be done as early as possible as deformities may worsen and lead to muscle imbalance, and joints may undergo degeneration or arthritic changes. Surgical measures may include various tendon transfers.[1][36]
Plantar Fasciitis
It is also known as plantar fasciopathy or fasciosis. It commonly affects athletes, especially runners.[37] Although its name has the suffix “itis,” it is more of the degenerative condition of the plantar fascia rather than an inflammation. The plantar fascia is an important structure to support and maintains the arch and provides shock absorption. It is presented as sharp pain localized at the medial heel, which can be aggravated by weight bearing and may be associated with calcaneal spur.[38]
Overuse injury caused by repetitive strain leads to microtears in the plantar fascia. Predisposing factors for this condition are pes cavus, pes planus, and excessive supination or pronation.[38][37]
It is primarily managed by conservative methods like NSAID, stretching, weight reduction, and shoe modification, but if not responded to, invasive measures like shock wave therapy, ultrasound-guided various injections of autologous platelet-rich plasma, steroid, or prolotherapy. Surgical measures (fasciotomy, open surgical release, endoscopic release, nerve decompression, or calcaneal drilling) are considered as last resort for managing plantar fasciitis when not responding to other measures.[38][37][39]
Clinical Significance
Foot deformities of congenital origin are prefixed as talipes, while that of acquired origin are referred to as pes.[40]
A few terminologies related to foot deformities are as follows.
Equinus: Foot is fixed in plantar flexion.
Calcaneus: Foot is fixed in dorsiflexion, so having a prominent heel.
Varus: Foot is fixed in an inverted position, and the forefoot is adducted.[40]
Valgus: Foot is fixed in everted position, and forefoot is abducted.[40]
Cavus: Increase the height of the longitudinal arch of the foot.
Planus: Flattened / Decreased height of the longitudinal arch of the foot.[40]
Talipes equinus: Congenital deformity of the foot in which the foot is plantar flexed, so the patient walks on toes with the heel raised.
Talipes calcaneus: Congenital deformity of the foot in which the foot is dorsiflexed, so the patient walks on heels with the forefoot raised.[40]
Talipes varus: Congenital deformity of the foot in which the foot is inverted and abducted, so the patient walks on the outer border of the foot.[40]
Talipes valgus: Congenital deformity of the foot in which the foot is everted and abducted, so the patient walks on the inner border of the foot. [40]
Talipes equino-varus / Club Foot
It is one of the commonest musculoskeletal congenital anomalies. It includes four components equinus hindfoot, varus calcaneus, cavus midfoot, and adduction of the forefoot.[41][42] These structural deformities may be caused by subluxation or dislocation of the talus at the talocalcaneonavicular joint, abnormalities of calf muscles or peroneus muscles, and tightness of ligaments of the medial side of the foot.[14][41][42] The risk of clubfoot increases with positive family history and smoking during pregnancy. Based on causes, it can be classified into four types, postural, idiopathic, neurogenic, and syndromic.
Conservative treatment is considered the best choice for managing clubfoot, including serial manipulation, casting, and bracing following the Ponseti method. While surgical methods may include soft tissue release, osteotomies, or arthrodesis. Ultimately, all treatment methods aim to obtain a pain-free, plantigrade, functional foot with no mobility issues.[41][42][43][44]
Other Issues
Many foot disorders affecting the arches are caused by improper shoe size, high heel shoes, arthropathy of the foot, or altered foot alignment.[45]
Hammertoe
Hammertoe refers to hyperextension at the metatarsophalangeal joint and hyperflexion at the proximal interphalangeal joints. While in claw toe, there is hyperextension at the metatarsophalangeal joint and hyperflexion at the proximal and distal interphalangeal joints. They are usually associated with improper size or high heel shoes or hallux valgus. It occurs due to muscular imbalance between extrinsic and intrinsic muscles, commonly involving extensor hallucis longus, flexor hallucis longus, and the peroneus longus.[45][46][47]
Hallux Valgus / Bunion
Hallux valgus or bunion is characterized by lateral deviation of the great toe and medial deviation of the head of the first metatarsal, which leads to prominence on the medial side of the base of the great toe. It is frequently seen in women and is associated with high heels or tight shoes. Hallux valgus deformity complex includes metatarsus primus varus, hallux valgus, and metatarsosesamoid dissociation.[45][48][49]
It occurs due to muscular imbalance and laxity of ligaments around the first metatarsophalangeal joint. Alignment of the first metatarsal is maintained by medially abductor hallucis and laterally by peroneus longus, assisted by collateral ligaments. These are also important factors in maintaining the arches of the foot.[47] Increased pressure on the first metatarsal lead to an increased hallux angle causing strain on medial structures. Adductor hallucis and capsule of the lateral side exaggerate this deformity. It is associated with Achilles tendon contracture and pes planus.[47][48]
Hallux Varus
Medial deviation of the great toe at the first metatarsophalangeal joint is called hallux varus.[50]
Hallux Limitus/Rigidus
A limited or absent range of motion occurs at the first metatarsophalangeal joint refers to hallux limitus or rigidus.[45]
Tailor Bunion / Bunionette
Bunionette refers to prominence on the lateral side of the head of the fifth metatarsal, which leads to medial deviation of the little toe. Because the tailor uses the cross-legged position, which predisposes to this condition, it is also known as a tailor bunion.[51]
Tailor bunion is of three types. In type 1, thickened and enlarged head of the fifth metatarsal on the lateral surface; in type 2, increased curvature on the lateral side and normal intermetatarsal angle between the fourth and fifth metatarsal. In contrast, in type 3, an increase in the same intermetatarsal angle. Due to continuous irritation, a bursa can form, which may ulcerate later on.[51][52]
March Fracture / Stress Fracture
The March fracture caused by repetitive stress due to abnormal load on healthy bone leads to microdamage and fracture later. It commonly occurs in sports persons or army soldiers due to increased physical activity after rest. It usually involves the neck of the second metatarsal because it is more fixed in position.[53][54]
Skew-foot
Skew-foot manifested clinically as dorsolateral swelling or bump on the lateral and intermediate cuneiform bones and is associated with subluxation of the first tarsometatarsal joint. It is associated with angular medial concavity and convexity on the lateral side, giving rise to z-shape alignment.
Metatarsus Adductus
In this condition, metatarsals are adducted at the tarsometatarsal joint. Thus the fifth metatarsal near the base is prominent, and convexity is seen on the lateral side, while medial side concavity is seen without any dorsolateral bump. It is described as transverse foot deformity.[50]
Metatarsalgia
Pain along the region of the head of the metatarsal is called metatarsalgia. It is of three types, iatrogenic, primary, and secondary. Primary metatarsalgia occurs because of anatomical abnormalities of the metatarsals associated with pes cavus or hallux valgus. Secondary metatarsalgia is caused by indirect pressure or load on the anterior part of the foot. While iatrogenic one occurs as a consequence of foot surgery, e.g., osteotomy of the metatarsal may follow malunion or avascular necrosis, leading to metatarsalgia.[45]
Morton (interdigital) Neuroma
Entrapment of plantar digital nerves with perineural fibrosis is seen in Morton neuroma. It commonly affects women and predominantly involves third web space digital nerve. Entrapment occurs between the intermetatarsal ligaments.[45] It presents with burning pain and a tingling sensation felt on the anterior part of the foot, which is aggravated by applying pressure in the third web space proximal to the head of the metatarsal.[45]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Babu D, Bordoni B. Anatomy, Bony Pelvis and Lower Limb: Medial Longitudinal Arch of the Foot. StatPearls. 2025 Jan:(): [PubMed PMID: 32965960]
Gwani AS, Asari MA, Mohd Ismail ZI. How the three arches of the foot intercorrelate. Folia morphologica. 2017:76(4):682-688. doi: 10.5603/FM.a2017.0049. Epub 2017 May 29 [PubMed PMID: 28553850]
Ghanem I, Massaad A, Assi A, Rizkallah M, Bizdikian AJ, El Abiad R, Seringe R, Mosca V, Wicart P. Understanding the foot's functional anatomy in physiological and pathological conditions: the calcaneopedal unit concept. Journal of children's orthopaedics. 2019 Apr 1:13(2):134-146. doi: 10.1302/1863-2548.13.180022. Epub [PubMed PMID: 30996737]
Level 3 (low-level) evidenceAsghar A, Naaz S. The transverse arch in the human feet: A narrative review of its evolution, anatomy, biomechanics and clinical implications. Morphologie : bulletin de l'Association des anatomistes. 2022 Dec:106(355):225-234. doi: 10.1016/j.morpho.2021.07.005. Epub 2021 Aug 19 [PubMed PMID: 34419345]
Level 3 (low-level) evidenceVenkadesan M, Yawar A, Eng CM, Dias MA, Singh DK, Tommasini SM, Haims AH, Bandi MM, Mandre S. Stiffness of the human foot and evolution of the transverse arch. Nature. 2020 Mar:579(7797):97-100. doi: 10.1038/s41586-020-2053-y. Epub 2020 Feb 26 [PubMed PMID: 32103182]
Card RK, Bordoni B. Anatomy, Bony Pelvis and Lower Limb, Foot Muscles. StatPearls. 2025 Jan:(): [PubMed PMID: 30969527]
Mostafa E, Graefe SB, Varacallo MA. Anatomy, Bony Pelvis and Lower Limb: Leg Posterior Compartment. StatPearls. 2025 Jan:(): [PubMed PMID: 30726025]
Khan IA, Mahabadi N, D’Abarno A, Varacallo MA. Anatomy, Bony Pelvis and Lower Limb: Leg Lateral Compartment. StatPearls. 2025 Jan:(): [PubMed PMID: 30137811]
Kanatli U, Yetkin H, Bolukbasi S. Evaluation of the transverse metatarsal arch of the foot with gait analysis. Archives of orthopaedic and trauma surgery. 2003 May:123(4):148-50 [PubMed PMID: 12734711]
Level 2 (mid-level) evidenceAnderson BW, Ekblad J, Black AC, Bordoni B. Anatomy, Appendicular Skeleton. StatPearls. 2025 Jan:(): [PubMed PMID: 30571018]
Marín-Llera JC, Garciadiego-Cázares D, Chimal-Monroy J. Understanding the Cellular and Molecular Mechanisms That Control Early Cell Fate Decisions During Appendicular Skeletogenesis. Frontiers in genetics. 2019:10():977. doi: 10.3389/fgene.2019.00977. Epub 2019 Oct 11 [PubMed PMID: 31681419]
Level 3 (low-level) evidenceKlaassen Z, Shoja MM, Tubbs RS, Loukas M. Supernumerary and absent limbs and digits of the lower limb: a review of the literature. Clinical anatomy (New York, N.Y.). 2011 Jul:24(5):570-5. doi: 10.1002/ca.21102. Epub 2011 Jan 3 [PubMed PMID: 21647959]
Talamillo A, Bastida MF, Fernandez-Teran M, Ros MA. The developing limb and the control of the number of digits. Clinical genetics. 2005 Feb:67(2):143-53 [PubMed PMID: 15679824]
Balasankar G, Luximon A, Al-Jumaily A. Current conservative management and classification of club foot: A review. Journal of pediatric rehabilitation medicine. 2016 Nov 30:9(4):257-264 [PubMed PMID: 27935562]
Raj MA, Tafti D, Kiel J. Pes Planus. StatPearls. 2025 Jan:(): [PubMed PMID: 28613553]
Guillot C, Smith T. Anatomy, Bony Pelvis and Lower Limb: Foot Arteries. StatPearls. 2025 Jan:(): [PubMed PMID: 32809747]
Takahashi LA, França GJ, Valle CED, Ferreira LRC. Assessment of the pedal arteries with Duplex Scanning. Jornal vascular brasileiro. 2020 Nov 11:19():e20200068. doi: 10.1590/1677-5449.200068. Epub 2020 Nov 11 [PubMed PMID: 34211519]
Lezak B, Varacallo MA. Anatomy, Bony Pelvis and Lower Limb, Foot Veins. StatPearls. 2025 Jan:(): [PubMed PMID: 31194435]
Karip B, Ertaş A. Abnormal vein patterns on the feet: two case reports. Folia morphologica. 2023:82(3):732-734. doi: 10.5603/FM.a2022.0053. Epub 2022 May 24 [PubMed PMID: 35607869]
Level 3 (low-level) evidenceShinaoka A, Koshimune S, Suami H, Yamada K, Kumagishi K, Boyages J, Kimata Y, Ohtsuka A. Lower-Limb Lymphatic Drainage Pathways and Lymph Nodes: A CT Lymphangiography Cadaver Study. Radiology. 2020 Jan:294(1):223-229. doi: 10.1148/radiol.2019191169. Epub 2019 Nov 19 [PubMed PMID: 31746690]
Suami H. Lymphosome concept: Anatomical study of the lymphatic system. Journal of surgical oncology. 2017 Jan:115(1):13-17. doi: 10.1002/jso.24332. Epub 2016 Jun 22 [PubMed PMID: 27334241]
Ficke J, Byerly DW. Anatomy, Bony Pelvis and Lower Limb: Foot. StatPearls. 2025 Jan:(): [PubMed PMID: 31536304]
Tang A, Bordoni B. Anatomy, Bony Pelvis and Lower Limb, Foot Nerves. StatPearls. 2025 Jan:(): [PubMed PMID: 30725977]
Lezak B, Massel DH, Varacallo MA. Peroneal Nerve Injury. StatPearls. 2025 Jan:(): [PubMed PMID: 31751049]
Kiel J, Kaiser K. Tarsal Tunnel Syndrome. StatPearls. 2025 Jan:(): [PubMed PMID: 30020645]
Desai SS, Cohen-Levy WB. Anatomy, Bony Pelvis and Lower Limb: Tibial Nerve. StatPearls. 2025 Jan:(): [PubMed PMID: 30725713]
Chang CH, Yang WT, Wu CP, Chang LW. Would foot arch development in children characterize a body maturation process? A prospective longitudinal study. Biomedical journal. 2022 Oct:45(5):828-837. doi: 10.1016/j.bj.2021.10.012. Epub 2021 Nov 2 [PubMed PMID: 34737119]
Farzadi M, Safaeepour Z, Nabavi H, Cham MB, Mousavi ME. Effect of Different Placement of Heel Rockers on Lower-Limb Joint Biomechanics in Healthy Individuals. Journal of the American Podiatric Medical Association. 2018 May:108(3):231-235. doi: 10.7547/16-052. Epub [PubMed PMID: 29932758]
Umberger BR. Stance and swing phase costs in human walking. Journal of the Royal Society, Interface. 2010 Sep 6:7(50):1329-40. doi: 10.1098/rsif.2010.0084. Epub 2010 Mar 31 [PubMed PMID: 20356877]
Geng X, Yang P, Wang X, Geng Y, Han Y. [Recognition of walking stance phase and swing phase based on moving window]. Sheng wu yi xue gong cheng xue za zhi = Journal of biomedical engineering = Shengwu yixue gongchengxue zazhi. 2014 Apr:31(2):273-8 [PubMed PMID: 25039126]
Brockett CL, Chapman GJ. Biomechanics of the ankle. Orthopaedics and trauma. 2016 Jun:30(3):232-238 [PubMed PMID: 27594929]
Leardini A, Stagni R, O'Connor JJ. Mobility of the subtalar joint in the intact ankle complex. Journal of biomechanics. 2001 Jun:34(6):805-9 [PubMed PMID: 11470119]
Welte L, Kelly LA, Lichtwark GA, Rainbow MJ. Influence of the windlass mechanism on arch-spring mechanics during dynamic foot arch deformation. Journal of the Royal Society, Interface. 2018 Aug:15(145):. doi: 10.1098/rsif.2018.0270. Epub [PubMed PMID: 30111662]
Blackwood CB, Yuen TJ, Sangeorzan BJ, Ledoux WR. The midtarsal joint locking mechanism. Foot & ankle international. 2005 Dec:26(12):1074-80 [PubMed PMID: 16390642]
Isikan UE. The values of talonavicular angles in patients with pes planus. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 1993 Sep-Oct:32(5):514-6 [PubMed PMID: 8252011]
Seaman TJ, Ball TA. Pes Cavus. StatPearls. 2025 Jan:(): [PubMed PMID: 32310476]
Rhim HC, Kwon J, Park J, Borg-Stein J, Tenforde AS. A Systematic Review of Systematic Reviews on the Epidemiology, Evaluation, and Treatment of Plantar Fasciitis. Life (Basel, Switzerland). 2021 Nov 24:11(12):. doi: 10.3390/life11121287. Epub 2021 Nov 24 [PubMed PMID: 34947818]
Level 1 (high-level) evidenceBuchanan BK, Sina RE, Kushner D. Plantar Fasciitis. StatPearls. 2025 Jan:(): [PubMed PMID: 28613727]
Allam AE, Chang KV. Plantar Heel Pain. StatPearls. 2025 Jan:(): [PubMed PMID: 29763043]
RITCHIE GW, KEIM HA. A RADIOGRAPHIC ANALYSIS OF MAJOR FOOT DEFORMITIES. Canadian Medical Association journal. 1964 Oct 17:91(16):840-4 [PubMed PMID: 14217246]
Barnes CJ, Dydyk AM. Talipes Equinovarus. StatPearls. 2025 Jan:(): [PubMed PMID: 32491773]
Rieger MA, Dobbs MB. Clubfoot. Clinics in podiatric medicine and surgery. 2022 Jan:39(1):1-14. doi: 10.1016/j.cpm.2021.08.006. Epub [PubMed PMID: 34809788]
Barrie A, Varacallo MA. Clubfoot. StatPearls. 2025 Jan:(): [PubMed PMID: 31855401]
Mustari MN, Faruk M, Bausat A, Fikry A. Congenital talipes equinovarus: A literature review. Annals of medicine and surgery (2012). 2022 Sep:81():104394. doi: 10.1016/j.amsu.2022.104394. Epub 2022 Aug 18 [PubMed PMID: 36147065]
Park CH, Chang MC. Forefoot disorders and conservative treatment. Yeungnam University journal of medicine. 2019 May:36(2):92-98. doi: 10.12701/yujm.2019.00185. Epub 2019 May 14 [PubMed PMID: 31620619]
Abousayed M, Kwon JY. Hallux claw toe. Foot and ankle clinics. 2014 Mar:19(1):59-63. doi: 10.1016/j.fcl.2013.11.001. Epub 2013 Dec 19 [PubMed PMID: 24548509]
Ray JJ, Friedmann AJ, Hanselman AE, Vaida J, Dayton PD, Hatch DJ, Smith B, Santrock RD. Hallux Valgus. Foot & ankle orthopaedics. 2019 Apr:4(2):2473011419838500. doi: 10.1177/2473011419838500. Epub 2019 May 7 [PubMed PMID: 35097321]
Kuhn J, Alvi F. Hallux Valgus. StatPearls. 2025 Jan:(): [PubMed PMID: 31971732]
Wu DY, Lam KF. Osteodesis for hallux valgus correction: is it effective? Clinical orthopaedics and related research. 2015 Jan:473(1):328-36. doi: 10.1007/s11999-014-3938-6. Epub 2014 Oct 28 [PubMed PMID: 25349035]
Level 2 (mid-level) evidenceRampal V, Giuliano F. Forefoot malformations, deformities and other congenital defects in children. Orthopaedics & traumatology, surgery & research : OTSR. 2020 Feb:106(1S):S115-S123. doi: 10.1016/j.otsr.2019.03.021. Epub 2019 Oct 21 [PubMed PMID: 31648997]
DiDomenico L, Baze E, Gatalyak N. Revisiting the tailor's bunion and adductovarus deformity of the fifth digit. Clinics in podiatric medicine and surgery. 2013 Jul:30(3):397-422. doi: 10.1016/j.cpm.2013.04.004. Epub [PubMed PMID: 23827493]
Mazoteras-Pardo V, Becerro-de-Bengoa-Vallejo R, Losa-Iglesias M, Palomo-López P, López-López D, Calvo-Lobo C, Romero-Morales C, Casado-Hernández I. Degree of Impact of Tailor's Bunion on Quality of Life: A Case-Control Study. International journal of environmental research and public health. 2021 Jan 16:18(2):. doi: 10.3390/ijerph18020736. Epub 2021 Jan 16 [PubMed PMID: 33467061]
Level 2 (mid-level) evidenceSaunier J, Chapurlat R. Stress fracture in athletes. Joint bone spine. 2018 May:85(3):307-310. doi: 10.1016/j.jbspin.2017.04.013. Epub 2017 May 13 [PubMed PMID: 28512006]
Koo AY, Tolson DR. March Fracture (Metatarsal Stress Fractures)(Archived). StatPearls. 2025 Jan:(): [PubMed PMID: 30335322]