Introduction
Coats disease is an idiopathic ocular condition characterized by retinal telangiectasia, aneurysms, and exudation.[1][2][3] George Coats first described it in 1908 as a unilateral condition with retinal exudation and telangiectasia in male children.[4] Later, Theodor von Leber described a similar case with telangiectatic and aneurysmal vessels without subretinal exudation.[2] This condition was later known as Leber multiple miliary aneurysms.[2] It was identified as an earlier disease process of Coats disease. Subsequently, Shields et al. defined Coats disease as ‘idiopathic retinal telangiectasia associated with exudation and frequent exudative retinal detachment with no signs of retinal or vitreal traction.’[5]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Coats disease is usually sporadic.[4] Considering the unilateral and sporadic nature of the disease, a somatic mutation is more likely.[6] Coats disease is characterized by peripheral retinal avascularity similar to other diseases like Norrie disease, familial exudative vitreoretinopathy (FEVR), facioscapulohumeral muscular dystrophy (FSHD), and osteoporosis pseudoglioma syndrome.[7][8][9][10][11][12][13] All of these conditions are related to abnormalities in the Wnt signaling pathway during retinal angiogenesis.[7][8]
Cremers and colleagues found a mutation in the CRB1 gene in 55% of eyes with retinitis pigmentosa and Coats-like secondary exudative vasculopathy.[14] They suggested that CRB1 could be involved in primary Coats disease as well as other retinal conditions.[14] Several reports have suggested a missense mutation within the Norrie disease pseudoglioma gene, NDP, on chromosome Xp11.2 in the pathogenesis of Coats disease.[15][16][17][18][19] Mutation in the PANK2 gene has also been implicated in Coats disease.[6][20][6]
Epidemiology
Morris et al. conducted a population bases study of Coats disease.[21] The incidence was 0.09 per 100,000 population. All cases were unilateral, and 85% were male.[21] The mean age at presentation was 146 months (median 96 months). Some authors have reported that the disease could be present at birth.[22] In a large series, only 5% of cases were bilateral.[2] The fellow eye was usually without symptoms and had subtle peripheral telangiectatic changes.[2] Adult-onset Coats disease (first diagnosed at a minimum age of 35 years) constituted 7% of the 646 patients with Coats disease in a tertiary eye care center.[23] The mean age at diagnosis of adult-onset Coats disease was 47 years in this series.[23]
Pathophysiology
In Coats disease, the blood-retinal barrier breaks down, which causes plasma leakage into the vessel wall.[24] The blood vessels become thickened and necrosed.[24] This leads to a ‘sausage-like’ shape of the vessel. The abnormal pericytes and endothelial cells in retinal blood vessels subsequently degenerate. These blood vessels form aneurysms and later occlude, leading to ischemia and rarely neovascularization.[25]
Histopathology
Coats studied the histologic features of enucleated eyes.[6] He described the subretinal fibrous tissue masses as tightly adherent to the outer retina. Most of the eyes had associated retinal thickening, degeneration, detachment, hemorrhages, cholesterol crystals, and vascular abnormalities.[6] One eye had evidence of bone formation. Other authors have also described the histopathologic features such as bullous retinal detachment and the presence of subretinal fluid. The outer retina is thickened due to exudation, and the inner retina contains telangiectatic vessels. The retinal vessels have perivascular sheathing and are degenerated. There is capillary dropout with areas of neovascularization.[26][27][28][29][30] Thick PAS (Periodic acid–Schiff)-positive deposits in the wall of retinal vessels and large aneurysms are typically seen in Coats disease.[24] Kase et al. have reported increased vascular endothelial growth factor (VEGF) levels in eyes with vascular abnormalities. They noted VEGF immunoreactivity in retinal macrophages and endothelium of blood vessels.[31]
History and Physical
The presenting symptoms are varied. The patients can present with decreased visual acuity (43%), strabismus (23%), leukocoria/xanthocoria (20%), pain (3%), heterochromia (1%), and nystagmus (1%).[2] Eight percent of patients may be asymptomatic and are detected coincidentally on routine examination.[2]
Visual acuity can range from 20/20 to 20/50 in 12% of cases, 20/60 to 20/100 in 11%, 20/200 to counting fingers in 18%, and hand motions to no light perception in 58%.[2] The main causes of poor vision include subfoveal fluid or lipids, subfoveal fibrosis, macular edema, epiretinal membrane, and optic atrophy.[5] The anterior segment is normal in 90% of cases. Those with findings include cataract, iris neovascularization, shallow anterior chamber, corneal edema due to high intraocular pressure, cholesterol in the anterior chamber, and megalocornea.[32][33]
Retinal findings include telangiectasia, fusiform aneurysms, and intraretinal exudation. There may be sheathing of the vasculature.[5] These findings are generally noted in the inferotemporal quadrant in the peripheral zones between the equator to ora serrata.[5] As the disease progresses, fluid exudation leads to exudative retinal detachment, retinal hemorrhage, vasoproliferative tumor, macular fibrosis, and optic disc neovascularization.[34] Advanced complications such as iridocyclitis, cataract, and secondary neovascular glaucoma can lead to phthisis bulbi.[35][36][37]
Adult-onset Coats disease is characterized by systemic associations (usually hypertension), incidental detection, involvement of less than six clock hours of the retina, a benign natural course of the disease, and usually better visual outcomes compared to childhood-onset Coats disease.[23] Seventy-three percent of patients with the adult-onset disease were male, and 93% of cases had unilateral involvement.[23]
Evaluation
The diagnosis of Coats disease is clinical. Ancillary investigations are done when the diagnosis is in doubt, particularly with bullous retinal detachment with exudation and dilated vessels.
Fundus Fluorescein Angiography (FFA)
The typical fluorescein angiographic features are telangiectasia, aneurysms, beading of vessel walls, and peripheral retinal nonperfusion.[38] The anomalous vessels show early leakage, which continues until the late phase.[39] The aneurysms are clearly visible as ‘light bulb’ dilations on the larger blood vessels. In the periphery, areas of capillary drop out and rarely neovascularization can be seen. FFA helps in treatment by identifying the telangiectatic leaking vessels, which can be selectively lasered. It also highlights the areas of nonperfusion which can be treated with photocoagulation in cases of neovascularization or even before the development of neovascularization.[5][40][41] With the development of wide-field angiography machines such as Retcam and Optos, peripheral vascular anomalies can be detected and selectively laser targeted.[42]
Optical Coherence Tomography (OCT)
OCT is helpful in monitoring for macular involvement. It helps in documenting cystoid macular edema, epiretinal membrane, subretinal/intraretinal fluid, subfoveal lipids, central macular thickness, and subfoveal choroidal thickness.[43] In a study, subretinal compact hyperreflectivity (fibrosis) and outer retinal atrophy were associated with worse final visual acuity.[44]
OCT Angiography (OCTA)
OCTA may be used to monitor the disease and response to therapy non-invasively.[45][46] Reported OCTA feature of Coats disease after therapy includes chorioretinal anastomoses, abnormal foveal vascular loops, and flow voids in the choroid.[45] Abnormal foveal avascular zone (FAZ) with retinal vessels traversing the FAZ may be noted in the affected and the fellow eye in cases with unilateral Coats disease.[47]
Ocular Ultrasonography (USG)
It depicts the extent of retinal detachment. It characterizes the subretinal space, which is usually acoustically clear, but sometimes hyperechogenicity can be seen due to the presence of cholesterol deposits. Calcification can occur in advanced Coats disease along the retinal pigmentary epithelium. It is seen as a curvilinear pattern in contrast to retinoblastoma, where it is randomly distributed.[4]
The analysis of subretinal fluid sometimes helps in diagnosis by demonstrating lipid-laden macrophages and cholesterol crystals.[2]
Computed Tomography (CT)
CT is useful to rule out retinoblastoma. The presence of a solid mass with calcification is present in retinoblastoma. This is better delineated in the CT scan. In Coats disease, the scan would be clear of these lesions.[48][49] CT also highlights the intraocular morphology and the subretinal exudation.
Magnetic Resonance Imaging (MRI)
MRI may be useful in diagnosing advanced Coats disease and ruling out retinoblastoma. The exudate in Coats disease is hyperintense on both T1-weighted and T2-weighted MRI images, whereas in retinoblastoma, the T1-weighted image will show a hyperintense mass, but the T2-weighted image shows a hypointense mass.[48][50] Retinoblastoma shows enhancement with gadolinium contrast, a feature not seen in Coats disease.[1]
Treatment / Management
The treatment for Coats disease depends on the stage of the disease. Mild cases with only retinal telangiectasia and no exudation can be observed and followed up at regular intervals. Treatment is needed when exudation develops. In less severe cases of exudation, laser photocoagulation to telangiectatic vessels is done.[51][52][53] (B2)
FFA helps in detecting the leaking vessels.[42] These are directly treated with moderate intensity burns. Laser therapy causes inflammation and leads to a transient increase in exudation. So, multiple sessions of laser are needed at intervals of 2 to 3 months. But the laser is ineffective in cases of extensive subretinal exudation and retinal detachment. Cryotherapy is useful in such cases. It is done by a double freeze-thaw technique over the affected retina. Cryotherapy is associated with more inflammation, pain, and sometimes exudative retinal detachment, so therapy should be limited per session and divided into multiple sessions.(B3)
Advanced cases with bullous exudative detachment abutting the lens might benefit from surgery. The subretinal fluid is drained either trans-sclerally or internally. The detached retina gets approximated. Pan retinal photocoagulation or cryotherapy is then done. In cases with the rhegmatogenous or tractional component, pars plana vitrectomy is done with or without tamponade. Surgery primarily aims to prevent a painful blind eye and avoid enucleation rather than vision restoration.
Enucleation is done in endstage disease with neovascularization or angle-closure glaucoma.[5][54] Alternatively, transscleral diode laser cyclophotocoagulation can be tried in eyes with neovascular glaucoma.[55] (B2)
Intravitreal corticosteroids and anti-VEGF agents may effectively reduce macular edema and subretinal fluid.[56][57][58][59][60][61][62][63][64] They are employed as adjunctive agents. They can also be given before laser and cryotherapy to reduce the reactive exudation associated with them.[65](B2)
Differential Diagnosis
Diseases that produce leukocoria[66] and strabismus can simulate Coats disease.[66] The differential diagnosis includes retinoblastoma, FEVR, retinal detachment, Noorie disease, persistent hyperplastic primary vitreous (PHPV), retinopathy of prematurity (ROP), congenital cataract, retinal hemorrhage, hemangioblastoma, toxocariasis, choroidal hemangioma, coloboma, endophthalmitis, cytomegalovirus retinitis, and toxoplasmosis.[67][68][67] The most important differential is retinoblastoma. Retinoblastoma is the most common intraocular malignancy in children and is fatal if left untreated. Coats disease is the most common cause of erroneous enucleation reported.[2]
Retinoblastoma can present in a younger child below one year; Coats disease is not as common in this age group and generally presents after 2 or 3 years. The large vessels in retinoblastoma go subretinally within the tumor, whereas in Coats disease, the telangiectatic vessels are always noted in the retinal surface. Bilaterality is common in retinoblastoma but very rare in Coats disease. Retinoblastoma often has a family history, but family history is usually not present in Coats disease. Retinoblastoma presents with leukocoria, and Coats disease has xanthocoria. On USG, retinoblastoma presents as a solid mass and calcification with shadowing. This feature is absent in Coats. The calcification in retinoblastoma is randomly distributed. Calcification in Coats is rare but, if present, is curvilinearly distributed along the retinal pigment epithelium.
FEVR and Noorie disease can be differentiated based on bilaterality, a positive family history, and the presence of retinal dragging, all of which are rare in Coats disease. Retinopathy of prematurity (ROP) is seen in preterm low birth-weight babies. Proliferative retinopathy due to chronic rhegmatogenous retinal detachment and pars planitis is another differential.
The classical finding in Coats is dilated telangiectatic vessels, aneurysms, hard exudates, peripheral avascularity, and exudative retinal detachment.
Sometimes a mass forms which might simulate
- Melanoma,
- Papillary or retinal capillary hemangioblastoma,
- Choroidal granuloma (sarcoidosis, tuberculosis), and
- Vasoproliferative tumor.
Other differential diagnoses of diseases with extensive hard exudates include
- Branch retinal venous occlusion,
- Vasoproliferative tumor,
- Capillary hemangioma,
- Chronic retinal detachment,
- Trauma, and
- Inflammation.
A Coats-like response (retinal telangiectasia, aneurysm, and hard exudates) may also be noted in
- Retinitis pigmentosa[69]
- Healed choroiditis[70]
- Tubercular subretinal abscess[71]
- Retinal vasculitis,[72]
- Pars planitis[73][74][75]
- Leber Congenital amaurosis[76]
- Facioscapulohumeral muscular dystrophy and deafness,
- Progressive facial hemiatrophy or Parry-Romberg syndrome or progressive hemifacial atrophy or hemifacial atrophy[77]
- Isolated hemihyperplasia
- Tuberous sclerosis
- Alport's syndrome
- X-linked retinoschisis and regressed retinopathy of prematurity[78]
- 'Blood-filled senile retinoschisis'[79]
- Linear Scleroderma[80]
- En coup de sabre scleroderma[81]
- Epidermal nevus syndrome
As described by Gass and Blodi, type I macular telangiectasia is characterized by nonfamilial and usually unilateral disease with retinal telangiectasia and hard exudates.[82] This disease is thought to lie in the spectrum of Coats disease.[83] The peripheral retinal yellow hard exudates in retinitis pigmentosa with a Coats-like response may be misdiagnosed as acute retinal necrosis.[84][85] Coats-like disease in FSHD is seen in around 75% of patients angiographically.[86] The retinal involvement is usually bilateral.[86] The posterior pole is usually not involved, and the disease usually has milder severity.[86] Visual loss is rarely (1%) noted.[86] Such bilateral Coats-like response in FSHD may affect females.[87]
Staging
Shields et al. introduced the staging of Coats disease in 2000, which is most widely used:
- Stage 1 is characterized by retinal telangiectasia
- Stage 2 has telangiectasia and intraretinal exudation
- Stage 2A: extrafoveal exudation
- Stage 2B: foveal involvement
- Stage 3 denotes exudative retinal detachment
- 3A is a subtotal detachment
- 3A1: extrafoveal
- 3A2: foveal involvement
- 3B is a total retinal detachment
- 3A is a subtotal detachment
- Stage 4 has a total retinal detachment plus increased intraocular pressure
- Stage 5 is an endstage disease, occasionally with phthisis bulbi[5][88]
Prognosis
Shields et al. reported the visual outcome of 160 patients with Coats disease.[89] This study found that the advanced stage of the disease was associated with poor visual acuity after treatment. The advanced disease showed less frequent resolution of disease, subretinal fluid, and exudation. The enucleation rate was higher in Stages 4 and 5. Poor visual acuity in advanced stages was mainly due to persistent retinal detachment and macular fibrosis. For stages 1 and 2, telangiectatic vessels resolved completely (47%) or partially (53%) over a mean interval of 15 months following treatment.[5]
Overall most cases (76%) stabilized or improved anatomically following treatment. A minority (8%) of patients progressively worsened.[5] Approximately 20% required enucleation for neovascular glaucoma or painful phthisis bulbi. The risk of recurrence of disease persists even after the resolution of the disease. Patients should be followed lifelong for recurrence.[3][90][91] Lack of visual rehabilitation and subretinal fibrotic nodule indicate poor visual prognosis.[92] In a series of 67 patients, the identified poor prognostic factors for globe salvage included cataract, diffuse involvement, advanced presentation (stage 3B or worse), anterior hyaloid proliferation, vitreous hemorrhage, preretinal or subretinal fibrosis, and combined or tractional retinal detachment.[92]
Complications
The clinical course of Coats disease is progressive. Acute exacerbations of the disease infrequently occur, followed by a quiescent state. Spontaneous remissions are rare. In untreated eyes, secondary complications can develop, including:
Deterrence and Patient Education
As Coats disease is idiopathic and sporadic, there are no preventative measures that can be taken by the patients' families. The patients' family members should be appropriately counseled regarding the prognosis of Coats disease and the importance of long-term follow-up.
Enhancing Healthcare Team Outcomes
Any patient presenting with Coats disease should not only receive treatment by an ophthalmologist as it requires an interprofessional team evaluation by pediatricians and oncologists. Interprofessional team communication can lead to better patient management. The patient will most often present to the primary clinician, and these professionals should be aware of the condition as it is treatable. Prompt referral to an ophthalmologist is necessary. These patients can then be followed by their primary clinicians and ensure compliance with treatment. The nursing staff will be the first to the department to come in contact with patients on follow-up and can assess treatment progress as well as evaluate compliance with therapy and report any issues to the primary care clinician. This collaborative, interprofessional approach to care can ensure optimal patient outcomes.
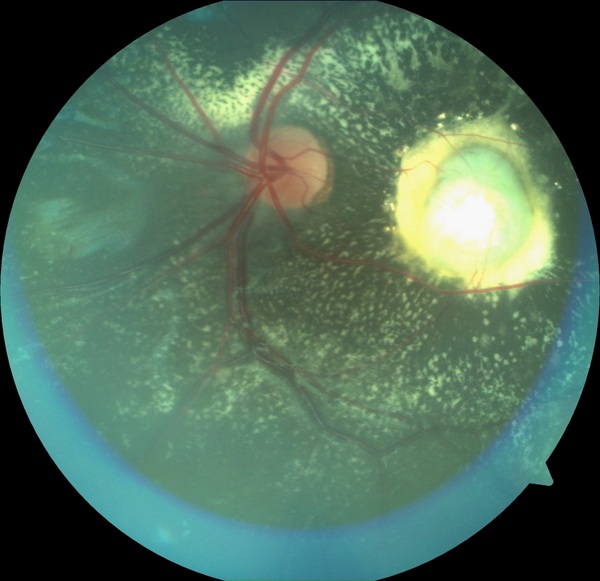
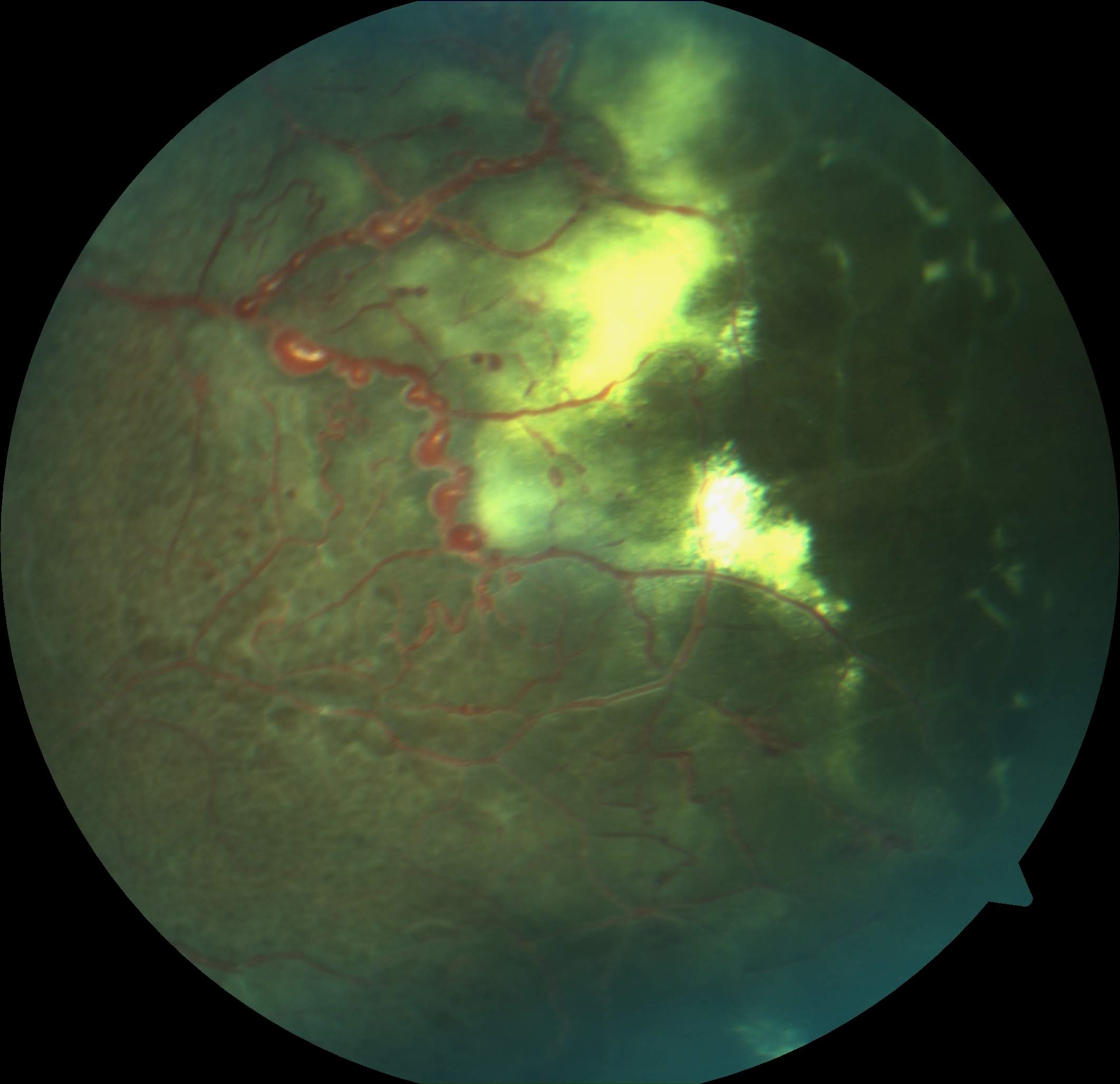
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Jones JH,Kroll AJ,Lou PL,Ryan EA, Coats' disease. International ophthalmology clinics. 2001 Fall; [PubMed PMID: 11698747]
Shields JA, Shields CL, Honavar SG, Demirci H. Clinical variations and complications of Coats disease in 150 cases: the 2000 Sanford Gifford Memorial Lecture. American journal of ophthalmology. 2001 May:131(5):561-71 [PubMed PMID: 11336930]
Level 2 (mid-level) evidenceShienbaum G,Tasman WS, Coats disease: a lifetime disease. Retina (Philadelphia, Pa.). 2006 Apr; [PubMed PMID: 16603961]
Level 2 (mid-level) evidenceSen M, Shields CL, Honavar SG, Shields JA. Coats disease: An overview of classification, management and outcomes. Indian journal of ophthalmology. 2019 Jun:67(6):763-771. doi: 10.4103/ijo.IJO_841_19. Epub [PubMed PMID: 31124484]
Level 3 (low-level) evidenceShields JA,Shields CL,Honavar SG,Demirci H,Cater J, Classification and management of Coats disease: the 2000 Proctor Lecture. American journal of ophthalmology. 2001 May; [PubMed PMID: 11336931]
Level 2 (mid-level) evidenceSigler EJ,Randolph JC,Calzada JI,Wilson MW,Haik BG, Current management of Coats disease. Survey of ophthalmology. 2014 Jan-Feb [PubMed PMID: 24138893]
Level 3 (low-level) evidenceYe X,Wang Y,Cahill H,Yu M,Badea TC,Smallwood PM,Peachey NS,Nathans J, Norrin, frizzled-4, and Lrp5 signaling in endothelial cells controls a genetic program for retinal vascularization. Cell. 2009 Oct 16; [PubMed PMID: 19837032]
Level 3 (low-level) evidenceClevers H, Eyeing up new Wnt pathway players. Cell. 2009 Oct 16; [PubMed PMID: 19837026]
Level 3 (low-level) evidenceDickinson JL,Sale MM,Passmore A,FitzGerald LM,Wheatley CM,Burdon KP,Craig JE,Tengtrisorn S,Carden SM,Maclean H,Mackey DA, Mutations in the NDP gene: contribution to Norrie disease, familial exudative vitreoretinopathy and retinopathy of prematurity. Clinical [PubMed PMID: 16970763]
Warden SM,Andreoli CM,Mukai S, The Wnt signaling pathway in familial exudative vitreoretinopathy and Norrie disease. Seminars in ophthalmology. 2007 Oct-Dec; [PubMed PMID: 18097984]
Qin M,Hayashi H,Oshima K,Tahira T,Hayashi K,Kondo H, Complexity of the genotype-phenotype correlation in familial exudative vitreoretinopathy with mutations in the LRP5 and/or FZD4 genes. Human mutation. 2005 Aug; [PubMed PMID: 15981244]
Level 2 (mid-level) evidenceJiao X,Ventruto V,Trese MT,Shastry BS,Hejtmancik JF, Autosomal recessive familial exudative vitreoretinopathy is associated with mutations in LRP5. American journal of human genetics. 2004 Nov; [PubMed PMID: 15346351]
Chen ZY,Battinelli EM,Fielder A,Bundey S,Sims K,Breakefield XO,Craig IW, A mutation in the Norrie disease gene (NDP) associated with X-linked familial exudative vitreoretinopathy. Nature genetics. 1993 Oct; [PubMed PMID: 8252044]
Cremers FP,Maugeri A,den Hollander AI,Hoyng CB, The expanding roles of ABCA4 and CRB1 in inherited blindness. Novartis Foundation symposium. 2004; [PubMed PMID: 14750597]
Black GC,Perveen R,Bonshek R,Cahill M,Clayton-Smith J,Lloyd IC,McLeod D, Coats' disease of the retina (unilateral retinal telangiectasis) caused by somatic mutation in the NDP gene: a role for norrin in retinal angiogenesis. Human molecular genetics. 1999 Oct; [PubMed PMID: 10484772]
Level 3 (low-level) evidenceShastry BS,Trese MT, Overproduction and partial purification of the Norrie disease gene product, norrin, from a recombinant baculovirus. Biochemical and biophysical research communications. 2003 Dec 5; [PubMed PMID: 14630047]
Berger W,van de Pol D,Bächner D,Oerlemans F,Winkens H,Hameister H,Wieringa B,Hendriks W,Ropers HH, An animal model for Norrie disease (ND): gene targeting of the mouse ND gene. Human molecular genetics. 1996 Jan; [PubMed PMID: 8789439]
Level 3 (low-level) evidenceLuhmann UF,Lin J,Acar N,Lammel S,Feil S,Grimm C,Seeliger MW,Hammes HP,Berger W, Role of the Norrie disease pseudoglioma gene in sprouting angiogenesis during development of the retinal vasculature. Investigative ophthalmology [PubMed PMID: 16123442]
Level 3 (low-level) evidenceOhlmann A,Scholz M,Goldwich A,Chauhan BK,Hudl K,Ohlmann AV,Zrenner E,Berger W,Cvekl A,Seeliger MW,Tamm ER, Ectopic norrin induces growth of ocular capillaries and restores normal retinal angiogenesis in Norrie disease mutant mice. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2005 Feb 16; [PubMed PMID: 15716406]
Level 3 (low-level) evidenceSohn EH,Michaelides M,Bird AC,Roberts CJ,Moore AT,Smyth D,Brady AF,Hungerford JL, Novel mutation in PANK2 associated with retinal telangiectasis. The British journal of ophthalmology. 2011 Jan [PubMed PMID: 20974629]
Level 3 (low-level) evidenceMorris B,Foot B,Mulvihill A, A population-based study of Coats disease in the United Kingdom I: epidemiology and clinical features at diagnosis. Eye (London, England). 2010 Dec; [PubMed PMID: 20865031]
Campbell FP, Coats' disease and congenital vascular retinopathy. Transactions of the American Ophthalmological Society. 1976; [PubMed PMID: 325857]
Level 3 (low-level) evidenceRishi E,Rishi P,Appukuttan B,Uparkar M,Sharma T,Gopal L, Coats' disease of adult-onset in 48 eyes. Indian journal of ophthalmology. 2016 Jul [PubMed PMID: 27609165]
Egbert PR,Chan CC,Winter FC, Flat preparations of the retinal vessels in Coats' disease. Journal of pediatric ophthalmology. 1976 Nov-Dec; [PubMed PMID: 798026]
Fernandes BF,Odashiro AN,Maloney S,Zajdenweber ME,Lopes AG,Burnier MN Jr, Clinical-histopathological correlation in a case of Coats' disease. Diagnostic pathology. 2006 Aug 30; [PubMed PMID: 16942617]
Level 3 (low-level) evidenceTripathi R,Ashton N, Electron microscopical study of Coat's disease. The British journal of ophthalmology. 1971 May; [PubMed PMID: 4102954]
DUKE JR,WOODS AC, COATS'S DISEASE. II. STUDIES ON THE IDENTITY OF THE LIPIDS CONCERNED, AND THE PROBABLE ROLE OF MUCOPOLYSACCHARIDES IN ITS PATHOGENESIS. The British journal of ophthalmology. 1963 Jul; [PubMed PMID: 14189711]
Chang MM,McLean IW,Merritt JC, Coats' disease: a study of 62 histologically confirmed cases. Journal of pediatric ophthalmology and strabismus. 1984 Sep-Oct; [PubMed PMID: 6502405]
Level 3 (low-level) evidenceFarkas TG,Potts AM,Boone C, Some pathologic and biochemical aspects of Coats' disease. American journal of ophthalmology. 1973 Feb; [PubMed PMID: 4348894]
Takei Y, Origin of ghost cell in Coats' disease. Investigative ophthalmology. 1976 Aug; [PubMed PMID: 955836]
Level 3 (low-level) evidenceKase S,Rao NA,Yoshikawa H,Fukuhara J,Noda K,Kanda A,Ishida S, Expression of vascular endothelial growth factor in eyes with Coats' disease. Investigative ophthalmology [PubMed PMID: 23221067]
Gupta N,Beri S,D'souza P, Cholesterolosis Bulbi of the Anterior Chamber in Coats Disease. Journal of pediatric ophthalmology and strabismus. 2009 Jun 25; [PubMed PMID: 19645389]
Shields JA,Eagle RC Jr,Fammartino J,Shields CL,De Potter P, Coats' disease as a cause of anterior chamber cholesterolosis. Archives of ophthalmology (Chicago, Ill. : 1960). 1995 Aug; [PubMed PMID: 7639669]
Level 3 (low-level) evidenceReichstein DA,Recchia FM, Coats disease and exudative retinopathy. International ophthalmology clinics. 2011 Winter; [PubMed PMID: 21139479]
Friedenwald H,Friedenwald JS, Terminal Stage in a Case of Retinitis with Massive Exudation. Transactions of the American Ophthalmological Society. 1929; [PubMed PMID: 16692828]
Level 3 (low-level) evidenceNaumann GD,Portwich E, [Etiology and final clinical cause for 1000 enucleations. (A clinico-pathologic study) (author's transl)]. Klinische Monatsblatter fur Augenheilkunde. 1976 May; [PubMed PMID: 957559]
Tripathy K,Chawla R,Temkar S,Sagar P,Kashyap S,Pushker N,Sharma YR, Phthisis Bulbi-a Clinicopathological Perspective. Seminars in ophthalmology. 2018 [PubMed PMID: 29902388]
Level 3 (low-level) evidenceRuia S, Tripathy K. Fluorescein Angiography. StatPearls. 2024 Jan:(): [PubMed PMID: 35015403]
Cunha-Vaz JG, The blood-retinal barriers. Documenta ophthalmologica. Advances in ophthalmology. 1976 Oct 15; [PubMed PMID: 1009819]
Level 3 (low-level) evidenceRidley ME,Shields JA,Brown GC,Tasman W, Coats' disease. Evaluation of management. Ophthalmology. 1982 Dec; [PubMed PMID: 6891766]
Tarkkanen A,Laatikainen L, Coat's disease: clinical, angiographic, histopathological findings and clinical management. The British journal of ophthalmology. 1983 Nov; [PubMed PMID: 6685529]
Kang KB,Wessel MM,Tong J,D'Amico DJ,Chan RV, Ultra-widefield imaging for the management of pediatric retinal diseases. Journal of pediatric ophthalmology and strabismus. 2013 Sep-Oct; [PubMed PMID: 23739460]
Level 3 (low-level) evidenceShields CL,Udyaver S,Dalvin LA,Lim LS,Atalay HT,L Khoo CT,Mazloumi M,Shields JA, Coats disease in 351 eyes: Analysis of features and outcomes over 45 years (by decade) at a single center. Indian journal of ophthalmology. 2019 Jun; [PubMed PMID: 31124485]
Ong SS,Mruthyunjaya P,Stinnett S,Vajzovic L,Toth CA, Macular Features on Spectral-Domain Optical Coherence Tomography Imaging Associated With Visual Acuity in Coats' Disease. Investigative ophthalmology & visual science. 2018 Jun 1 [PubMed PMID: 30025132]
Ashkenazy N,Acon D,Kalavar M,Berrocal AM, Optical coherence tomography angiography and multimodal imaging in the management of coats' disease. American journal of ophthalmology case reports. 2021 Sep [PubMed PMID: 34381924]
Level 3 (low-level) evidenceHautz W, Gołębiewska J, Kocyła-Karczmarewicz B. Optical Coherence Tomography and Optical Coherence Tomography Angiography in Monitoring Coats' Disease. Journal of ophthalmology. 2017:2017():7849243. doi: 10.1155/2017/7849243. Epub 2017 Mar 9 [PubMed PMID: 28377823]
Muakkassa NW,de Carlo TE,Choudhry N,Duker JS,Baumal CR, Optical Coherence Tomography Angiography Findings in Coats' Disease. Ophthalmic surgery, lasers & imaging retina. 2016 Jul 1 [PubMed PMID: 27434894]
Eisenberg L,Castillo M,Kwock L,Mukherji SK,Wallace DK, Proton MR spectroscopy in Coats disease. AJNR. American journal of neuroradiology. 1997 Apr; [PubMed PMID: 9127038]
Level 3 (low-level) evidencePotter PD,Shields CL,Shields JA,Flanders AE, The role of magnetic resonance imaging in children with intraocular tumors and simulating lesions. Ophthalmology. 1996 Nov; [PubMed PMID: 8942869]
Senft SH,Hidayat AA,Cavender JC, Atypical presentation of Coats disease. Retina (Philadelphia, Pa.). 1994; [PubMed PMID: 8016459]
Level 3 (low-level) evidenceSchefler AC,Berrocal AM,Murray TG, Advanced Coats' disease. Management with repetitive aggressive laser ablation therapy. Retina (Philadelphia, Pa.). 2008 Mar; [PubMed PMID: 18317343]
Level 2 (mid-level) evidenceSpitznas M,Joussen F,Wessing A, Treatment of Coats' disease with photocoagulation. Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. Albrecht von Graefe's archive for clinical and experimental ophthalmology. 1976 Apr 1; [PubMed PMID: 1083682]
Shapiro MJ,Chow CC,Karth PA,Kiernan DF,Blair MP, Effects of green diode laser in the treatment of pediatric Coats disease. American journal of ophthalmology. 2011 Apr; [PubMed PMID: 21257148]
Level 2 (mid-level) evidenceShields JA,Shields CL, Review: coats disease: the 2001 LuEsther T. Mertz lecture. Retina (Philadelphia, Pa.). 2002 Feb; [PubMed PMID: 11884883]
Harris GS, Coats' disease, diagnosis and treatment. Canadian journal of ophthalmology. Journal canadien d'ophtalmologie. 1970 Oct; [PubMed PMID: 5481542]
Othman IS,Moussa M,Bouhaimed M, Management of lipid exudates in Coats disease by adjuvant intravitreal triamcinolone: effects and complications. The British journal of ophthalmology. 2010 May; [PubMed PMID: 19955197]
Level 2 (mid-level) evidenceJarin RR,Teoh SC,Lim TH, Resolution of severe macular oedema in adult Coat's syndrome with high-dose intravitreal triamcinolone acetonide. Eye (London, England). 2006 Feb; [PubMed PMID: 15723038]
Level 3 (low-level) evidenceLei S,Lam WC, Efficacy and safety of dexamethasone intravitreal implant for refractory macular edema in children. Canadian journal of ophthalmology. Journal canadien d'ophtalmologie. 2015 Jun; [PubMed PMID: 26040225]
Ghazi NG,Al Shamsi H,Larsson J,Abboud E, Intravitreal triamcinolone in Coats' disease. Ophthalmology. 2012 Mar; [PubMed PMID: 22385486]
Level 3 (low-level) evidenceEntezari M,Ramezani A,Safavizadeh L,Bassirnia N, Resolution of macular edema in Coats' disease with intravitreal bevacizumab. Indian journal of ophthalmology. 2010 Jan-Feb; [PubMed PMID: 20029156]
Level 3 (low-level) evidenceAlvarez-Rivera LG,Abraham-Marín ML,Flores-Orta HJ,Mayorquín-Ruiz M,Cortés-Luna CF, [Coat's disease treated with bevacizumab (Avastin)]. Archivos de la Sociedad Espanola de Oftalmologia. 2008 May; [PubMed PMID: 18464184]
Level 3 (low-level) evidenceLin CJ,Hwang JF,Chen YT,Chen SN, The effect of intravitreal bevacizumab in the treatment of Coats disease in children. Retina (Philadelphia, Pa.). 2010 Apr; [PubMed PMID: 19996822]
Level 3 (low-level) evidenceGaillard MC,Mataftsi A,Balmer A,Houghton S,Munier FL, ranibizumab in the management of advanced Coats disease Stages 3B and 4: long-term outcomes. Retina (Philadelphia, Pa.). 2014 Nov; [PubMed PMID: 25075562]
Level 2 (mid-level) evidenceZheng XX,Jiang YR, The effect of intravitreal bevacizumab injection as the initial treatment for Coats' disease. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2014 Jan; [PubMed PMID: 23873253]
Level 2 (mid-level) evidenceLi S,Deng G,Liu J,Ma Y,Lu H, The effects of a treatment combination of anti-VEGF injections, laser coagulation and cryotherapy on patients with type 3 Coat's disease. BMC ophthalmology. 2017 May 22 [PubMed PMID: 28532448]
Kanukollu VM, Tripathy K. Leukocoria. StatPearls. 2022 Jan:(): [PubMed PMID: 32809629]
Gupta A,Tripathy K, Ocular Toxocariasis StatPearls. 2022 Jan [PubMed PMID: 35015409]
Simakurthy S,Tripathy K, Endophthalmitis StatPearls. 2021 Jan; [PubMed PMID: 32644505]
Jiang Y,Lim J,Janowicz M, Cholesterol Crystals Secondary to Coats-Like Response With Retinitis Pigmentosa. JAMA ophthalmology. 2017 Oct 12 [PubMed PMID: 29049676]
Verma S,Bhatia I,Banerjee M,Kumar V, Coats like response in healed choroiditis. Ocular immunology and inflammation. 2021 Apr 2 [PubMed PMID: 33797302]
Nair N,Kummamuri S,Sudharshan S,Khetan V, Coats-like response in tubercular subretinal abscess masquerading as melanoma as the initial manifestation of miliary tuberculosis. Indian journal of ophthalmology. 2020 Sep [PubMed PMID: 32823473]
Chaudhary P,Varshney A,Videkar C, Secondary Coats' response to retinal vasculitis managed with bevacizumab. Indian journal of ophthalmology. 2018 Sep [PubMed PMID: 30127171]
Suh DW,Pulido JS,Jampol LM,Chong LP,Thomas M, Coats'-like response in pars planitis. Retina (Philadelphia, Pa.). 1999; [PubMed PMID: 10048380]
Level 3 (low-level) evidenceChauhan K, Tripathy K. Pars Planitis. StatPearls. 2024 Jan:(): [PubMed PMID: 28613790]
Chen PP,Chong LP, Coats'-like response in a patient with pars planitis. The British journal of ophthalmology. 1996 Jul [PubMed PMID: 8795387]
Level 3 (low-level) evidenceKumar V,Tewari R,Chandra P,Kumar A, Ultra wide field imaging of coats like response in Leber's congenital amaurosis. Saudi journal of ophthalmology : official journal of the Saudi Ophthalmological Society. 2017 Apr-Jun [PubMed PMID: 28559726]
Agarwal A,Pilania RK,Anjani G,Choudhary H,Gupta A,Gupta V, Retinal Vasculitis With Coats-Like Response in a Young Girl With Parry-Romberg Syndrome. Journal of clinical rheumatology : practical reports on rheumatic & musculoskeletal diseases. 2021 Dec 1 [PubMed PMID: 31124919]
Fan KC,McAllister MA,Yannuzzi NA,Patel NA,Prakhunhungsit S,Negron CI,Capó H,Berrocal AM, X-Linked Retinoschisis and a Coats-Like Response in the Setting of Retinopathy of Prematurity. Journal of vitreoretinal diseases. 2020 Nov 1; [PubMed PMID: 34622118]
Gelisken F,Sherif Adel S,Inhoffen W,Bartz-Schmidt KU, Coats'-like response in blood-filled senile retinoschisis. Ophthalmologica. Journal international d'ophtalmologie. International journal of ophthalmology. Zeitschrift fur Augenheilkunde. 2002 Sep-Oct; [PubMed PMID: 12424408]
Level 3 (low-level) evidenceBehboudi H,Zayeni H,Haji-Abbasi A,Moravvej Z,Azaripour E,Alizadeh Y,Soltani-Moghadam R, Coats'-like Response Associated with Linear Scleroderma. Journal of ophthalmic & vision research. 2022 Jan-Mar [PubMed PMID: 35194504]
George MK,Bernardino CR,Huang JJ, Coats-like response in linear en coup de sabre scleroderma. Retinal cases & brief reports. 2011 Fall [PubMed PMID: 25390412]
Level 3 (low-level) evidenceGass JD,Blodi BA, Idiopathic juxtafoveolar retinal telangiectasis. Update of classification and follow-up study. Ophthalmology. 1993 Oct [PubMed PMID: 8414413]
Yannuzzi LA,Bardal AM,Freund KB,Chen KJ,Eandi CM,Blodi B, Idiopathic macular telangiectasia. Archives of ophthalmology (Chicago, Ill. : 1960). 2006 Apr [PubMed PMID: 16606869]
Level 2 (mid-level) evidenceTran L,Papasavvas I,Fleischhauer J,Herbort CP Jr, Peripheral Inflammatory Yellow Exudative Retinal Coats-Like Vitreoretinopathy Misdiagnosed as Acute Retinal Necrosis in a Retinitis Pigmentosa Patient after Cataract Surgery. Case reports in ophthalmology. 2021 May-Aug [PubMed PMID: 34248592]
Level 3 (low-level) evidenceBergstrom R, Tripathy K. Acute Retinal Necrosis. StatPearls. 2024 Jan:(): [PubMed PMID: 29262034]
Fitzsimons RB,Gurwin EB,Bird AC, Retinal vascular abnormalities in facioscapulohumeral muscular dystrophy. A general association with genetic and therapeutic implications. Brain : a journal of neurology. 1987 Jun [PubMed PMID: 3580827]
Vance SK,Wald KJ,Sherman J,Freund KB, Subclinical facioscapulohumeral muscular dystrophy masquerading as bilateral Coats disease in a woman. Archives of ophthalmology (Chicago, Ill. : 1960). 2011 Jun [PubMed PMID: 21670353]
Level 3 (low-level) evidenceCahill M,O'Keefe M,Acheson R,Mulvihill A,Wallace D,Mooney D, Classification of the spectrum of Coats' disease as subtypes of idiopathic retinal telangiectasis with exudation. Acta ophthalmologica Scandinavica. 2001 Dec; [PubMed PMID: 11782226]
Level 2 (mid-level) evidenceShields CL,Udyaver S,Dalvin LA,Lim LS,Atalay HT,Khoo C,Mazloumi M,Shields JA, Visual acuity outcomes in Coats disease by classification stage in 160 patients. The British journal of ophthalmology. 2020 Mar; [PubMed PMID: 31177186]
Egerer I,Tasman W,Tomer TT, Coats disease. Archives of ophthalmology (Chicago, Ill. : 1960). 1974 Aug; [PubMed PMID: 4847500]
Tasman W, Coats' disease. American family physician. 1977 Apr; [PubMed PMID: 848416]
Shanmugam MP,Shah PN,Sagar P,Ramanjulu R,Mishra DK, Coats' disease - Prognostic factors for globe and vision salvage in children, a long-term experience. Indian journal of ophthalmology. 2022 Feb [PubMed PMID: 35086222]
Judisch GF,Apple DJ, Orbital cellulitis in an infant secondary to Coats' disease. Archives of ophthalmology (Chicago, Ill. : 1960). 1980 Nov [PubMed PMID: 7436836]
Level 3 (low-level) evidence