Local Anesthesia Techniques in Dentistry and Oral Surgery
Local Anesthesia Techniques in Dentistry and Oral Surgery
Introduction
Pain is an unpleasant sensory and psychological experience resulting from actual or potential tissue damage and is commonly associated with dental treatment.[1] Local anesthesia is a safe and effective way of managing pain. Anesthetic agents work by reversibly binding to sodium channels, preventing the entry of sodium into the cells and thereby inhibiting the propagation of nerve impulses. Consequently, nociceptive impulses associated with painful stimuli do not reach the brain, and the patient does not perceive pain.[2][3]
The maxillary and mandibular branches of the trigeminal nerve provide sensory innervation to the soft and hard tissues of the oral cavity.[4][5] The anesthetic solution must be injected adjacent to the nerve supplying the area where dental treatment will be performed. A thorough understanding of these trigeminal nerve branches and associated anatomical landmarks is essential.[2]
Local anesthesia in dentistry can be given as either infiltration or block anesthesia. Generally, infiltration anesthesia is commonly used in the maxilla, whereas block anesthesia is frequently used in the mandible.[6] In addition, there are supplemental local anesthesia techniques that can be utilized when infiltration and block methods have failed to achieve profound anesthesia. Supplemental techniques include intraligamentary, intraosseous, intrapulpal, and interseptal anesthesia.[7]
This paper will explore the anatomical course of the nerves supplying the oral cavity and the different techniques utilized to anesthetize these nerves prior to delivering dental treatment. The equipment required for dental local anesthesia, including common anesthetic agents and their applications, will be considered. Furthermore, the prevention and management of complications associated with local anesthesia will be discussed.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Infraorbital Nerve
The infraorbital nerve originates from the maxillary division of the trigeminal nerve as it enters the inferior orbital fissure after passing through the pterygopalatine fossa. The nerve travels along the infraorbital groove and infraorbital canal in the orbital floor before entering the face via the infraorbital foramen. The infraorbital nerve delivers sensation to the maxillary teeth via the superior alveolar nerve branches prior to entering the infraorbital foramen. It divides into palpebral, nasal, and superior labial terminal branches on the face. These terminal branches provide sensation to the skin of the lower eyelid, nose, cheek, and upper lip.[4]
Superior Alveolar Nerves
The posterior superior alveolar (PSA) nerve emerges before the maxillary nerve enters the infraorbital groove, and it descends along the maxillary tuberosity, where it innervates the gingiva and buccal mucosa of this region. It then enters the posterior alveolar canal and provides sensory fibers to the maxillary sinus mucosa, the maxilla, maxillary molar teeth, and periodontium.[4]
The middle superior alveolar (MSA) nerve branches off within the infraorbital canal and runs down along the maxillary sinus lateral wall. This nerve innervates the maxillary premolar teeth and periodontium. In some individuals, the MSA nerve is absent, and the premolar teeth are supplied by the PSA nerve instead.[4]
The anterior superior alveolar (ASA) nerve also originates within the infraorbital canal and descends along the anterior wall of the maxillary sinus. This nerve innervates the canine and incisor teeth and their periodontium.[4]
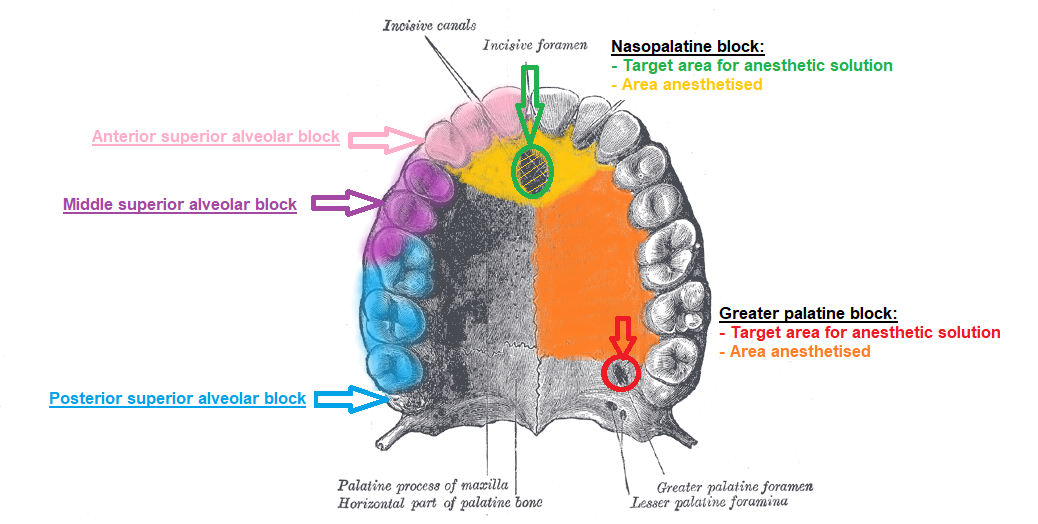
Palatine Nerves
The palatine nerves originate from the pterygopalatine ganglion, which is supplied by the maxillary division of the trigeminal nerve [4].
The greater palatine nerve runs through the greater palatine canal and enters the greater palatine foramen, usually located medial to the third maxillary molars, to innervate the hard palate and palatal gingiva.[4]
The lesser palatine nerve descends through the lesser palatine foramen, which is posteromedial to the greater palatine foramen, to innervate the soft palate, uvula, and tonsils.[4]
The nasopalatine nerve enters the sphenopalatine foramen, running along the nasal cavity and innervating the nasal septum. The nerve then emerges through the incisive foramen of the hard palate to innervate the anterior hard palate and anterior palatal gingiva. The nasopalatine nerve also provides sensory fibers to the maxillary incisors in some patients.[4]
Buccal Nerve
The buccal nerve, also known as the long buccal nerve, stems from the anterior trunk of the mandibular division of the trigeminal nerve.[5] It descends along the lateral pterygoid muscle and perforates the temporalis tendon, where it provides sensory branches to the posterior buccal mucosa and the buccal gingiva of the second and third mandibular molars.
The nerve runs across the buccinator and provides sensory innervation to the skin over the anterior buccinator and the buccal mucosa. The buccal mucosa innervation extends superiorly up to the region opposite the maxillary molars and anteriorly to the lateral aspect of the lips.[8]
Lingual Nerve
The lingual nerve stems from the posterior trunk of the mandibular division of the trigeminal nerve. It descends between the tensor veli palatini, lateral pterygoid, and medial pterygoid muscles to enter the pterygomandibular space.[5] The lingual nerve passes anterior and medial to the inferior alveolar nerve (IAN).[9]
It runs along the lingual body of the mandible, passing medial to the third molar and above the mylohyoid line, generally 2 or 3 mm below the alveolar crest, where it is only covered by gingival mucoperiosteum. The nerve then runs across the extrinsic tongue muscles, mylohyoid muscle, sublingual gland, and submandibular gland—the nerve curves around the submandibular duct before dividing into terminal branches.
The lingual nerve provides somatic sensation to the anterior two-thirds of the tongue, the floor of the mouth, and the lingual gingiva. The lingual nerve also carries fibers from the chorda tympani branch of the facial nerve to provide secretomotor supply to the submandibular and sublingual glands and to carry taste sensation from the anterior two-thirds of the tongue.[5]
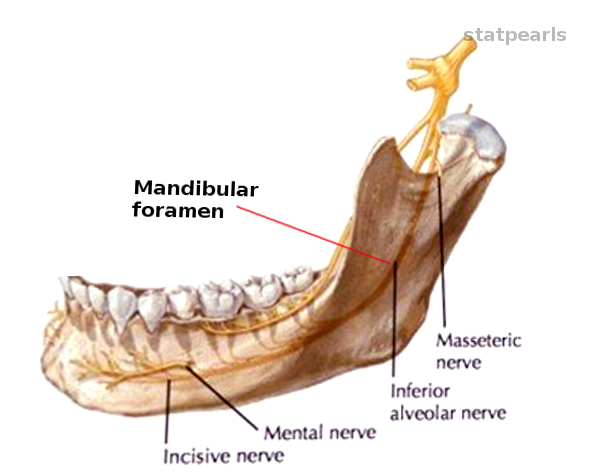
Inferior Alveolar Nerve (IAN)
The IAN stems from the posterior trunk of the mandibular division of the trigeminal nerve.[5] It runs deep to the lateral pterygoid muscle and gives off a mylohyoid nerve branch before descending into the pterygomandibular space and entering the mandibular foramen.[5][9] The IAN runs along the mandibular canal below the teeth apices, giving dental branches innervating the teeth via their apical foramina and interdental branches to innervate the periodontium.
At the mental foramen, located below the premolar apices, the IAN divides into incisive and mental nerves. The incisive nerve continues within the bone via the incisive canal to supply the teeth and buccal gingiva of the first premolar, canine, and incisors. The incisive nerve sometimes extends beyond the midline to provide additional sensation to the contralateral anterior teeth. The mental nerve exits via the mental foramen to supply the lower labial mucosa and the skin of the lower lip and chin.[5]
The mylohyoid nerve originates from the IAN approximately 13.4 to 14.7 mm above the mandibular foramen.[10] It pierces the sphenomandibular ligament and runs along the mylohyoid groove of the lingual surface of the mandible. It provides motor supply to the mylohyoid and anterior belly of digastric muscles.[5]
Despite its primarily motor nature, in some cases, the mylohyoid nerve can provide accessory sensory innervation to the mandibular teeth, associated soft tissues, and submental skin. This can be due to anastomosis with the lingual nerve or anatomical variations. Anatomical variations in the origin, course, communications, and innervations of the mylohyoid nerve can account for the failure to fully anesthetize mandibular teeth and soft tissues.[10]
Pterygomandibular Space
The pterygomandibular space contains the inferior alveolar neurovascular bundle, the lingual nerve, and the sphenomandibular ligament.[9] It is bound by the lateral pterygoid muscle superiorly, the medial pterygoid muscle inferiorly and medially, the mandibular ramus laterally, the parotid gland posteriorly, and the pterygomandibular raphe anteriorly. The pterygomandibular raphe is formed by the junction of the buccinator and superior constrictor muscles.[9][11]
The pterygomandibular space is mainly made up of loose areolar connective tissue.[9] The aim of an IAN block (IANB) is to deliver the anesthetic solution to the vicinity of the IAN in the pterygomandibular space.[11]
The inferior alveolar neurovascular bundle is located in the sulcus colli, a bony depression on the medial aspect of the ramus. The mandibular foramen is positioned at the inferior aspect of the sulcus colli, posterior to the midline of the ramus, and the level of the mandibular occlusal plane.[11]
A crest of thick bone, known as the crista endocoronoidea, forms the anterior border of the sulcus colli, and it should be contacted during IANB administration. Contacting this bony protrusion helps ensure that the anesthetic solution is delivered adjacent to the IAN, without mechanical injury to the nerve and superior to the lingula.[9]
The lingula is a bony projection anterior to the mandibular foramen. It is important to deliver the IANB above the lingula because the sphenomandibular ligament attaches to the lingula, and this fibrous ligament can prevent the effective diffusion of the anesthetic solution.[9][11]
Indications
Local anesthesia is essential for pain management in dentistry. Dental treatments can be associated with mechanical, thermal, or chemical stimuli, eliciting a painful response. Such dental treatments may include oral surgery, periodontal, endodontic, prosthetic, and restorative treatments. Local anesthesia is used to provide temporary sensory loss to allow for the delivery of dental treatment.[11]
Contraindications
A known allergy to a local anesthetic agent or an ingredient of the anesthetic solution contraindicates its use. Allergy is the only absolute contraindication to local anesthesia. However, some anesthetic agents or techniques should be avoided or used with caution in certain individuals.
Furthermore, toxicity and potential interactions need to be considered. Toxicity can result from exceeding the maximum recommended anesthetic dose or from the concomitant use of the anesthetic agent by the patient. Drug interactions with local anesthetics are rare. However, interactions of vasoconstrictors with beta-blockers, tricyclic antidepressants, amphetamines, and volatile anesthetics leading to hypertension and cardiac arrhythmias have been reported.[3]
Caution is Necessary for the Following Circumstances
Hepatic or Renal Impairment
Lower anesthetic doses should be considered for patients with hepatic or renal impairment, as reduced liver or kidney function can affect the metabolism of anesthetic agents. Lidocaine and mepivacaine are almost entirely metabolized in the liver, with a small percentage being excreted unchanged in the urine. Prilocaine is metabolized by kidneys, lungs, and liver. Whereas for articaine, only 10-15% of the drug is metabolized by the liver, and the remaining drug is converted to articainic acid, a non-toxic and inactive form, in the blood.[6]
Cardiovascular Disease
Adrenaline is commonly added to local anesthetic agents, and caution is recommended for patients with cardiovascular disease. A maximum dose of adrenaline of 0.04 mg is advised for patients with cardiovascular disease, compared to 0.2 mg for a healthy adult.[12]
However, there is limited evidence on the effects of the adrenaline found in local anesthesia on patients with cardiovascular disease. Using a low dose of adrenaline does not significantly affect blood pressure or heart rate. Adverse effects can be associated with intravascular injection, injection of a highly vascular area, or exceeding the recommended dose.[13]
Furthermore, intraligamental and intraosseous injection with adrenaline-containing anesthetics is not recommended for patients with cardiovascular disease as the drug rapidly enters the circulation with these techniques.[7]
Elderly Patients
Caution is essential when delivering local anesthesia to the elderly, and lower doses should be considered due to reduced kidney and liver function. Cardiovascular disease is also more common in the elderly, and limiting the use of adrenaline should be considered.[3]
Pregnancy
Lidocaine can be relatively safe, and there is no clear evidence that local anesthesia increases the risk of complications for the mother or fetus. However, any local anesthesia administered can cross the placenta and enter the fetus. Therefore, the operator should weigh the benefits and risks of local anesthesia, considering the health of the mother and fetus, the latest evidence regarding local anesthesia, and the risk of delaying treatment. It is generally recommended that elective dental treatment be deferred in pregnancy’s first and third trimesters.[3][14]
Some clinicians avoid using prilocaine with felypressin in pregnancy as there is a theoretical risk of labor induction with felypressin and fetal methemoglobinemia with prilocaine. Nonetheless, these complications are rare at the low doses utilized in dentistry.[15]
Patients with Bleeding Disorders or Taking Anticoagulants
Local infiltration techniques are preferred over block anesthesia for patients with inherited bleeding disorders. This is because of the risk of intramuscular hematoma with potential airway compromise associated with IAN or PSA nerve blocks in these patients.[16] Although some practitioners may be concerned with block anesthesia in anticoagulated patients, studies suggest that mandibular blocks can be used safely for anticoagulated patients.[17]
Equipment
- Personal protective equipment
- Dental syringe
- A 25, 27, or 30 gauge, short or long dental needle, depending on the anesthetic technique
- Local anesthetic solution
- Topical anesthesia can be considered
Local Anesthetic Agents
Local anesthetics are divided into two classes: amides and esters. Amide anesthetics are common in dentistry, including lidocaine, prilocaine, mepivacaine, and bupivacaine. Articaine is an amide anesthetic with an ester linkage. Ester anesthetics are less frequently utilized in dentistry, but drugs such as benzocaine may be used for topical anesthesia.[3]
The gold standard and most widely used local anesthetic in dentistry is lidocaine due to its safety and effectiveness. Adrenaline is added to lidocaine to counteract its vasodilating properties and delay drug absorption, which prolongs the duration of anesthesia and reduces the toxicity risk.[6]
Articaine with adrenaline, while not as frequently utilized as lidocaine, is heavily relied upon as a result of its superior solubility. Articaine has a high lipid solubility due to its thiophene ring and can diffuse across the maxillary and mandibular bone more readily than other anesthetics. Articaine buccal infiltrations are particularly useful in the posterior mandible as, unlike other agents, articaine can penetrate the dense cortical bone to anesthetize the IAN. It must be noted that articaine is not recommended for IANB due to a greater risk of nerve damage.[6]
Comparatively, prilocaine and mepivacaine have weak vasodilation properties and can be used without adrenaline. Both are short-acting anesthetics and good options for children, the elderly, and patients with contraindications to adrenaline.[6]
Children are more prone to soft tissue injury by inadvertently biting soft tissues when anesthetized; therefore, a short-acting anesthetic can be advantageous.[3]
Mepivacaine is the anesthetic of choice for patients with cardiovascular disease. Furthermore, studies suggest that mepivacaine can be more successful than other agents in anesthetizing teeth with irreversible pulpitis [6]. Bupivacaine is a long-acting anesthetic with effects lasting up to eight hours, meaning it is less commonly used in dentistry, where prolonged anesthesia is not often required.[6]
Personnel
Local anesthesia is generally administered by dentists, dental hygienists, or dental therapists with the support of a dental assistant. The dental assistant ensures that the necessary equipment and materials are available. The operator or assistant can assemble the dental syringe. The operator administers the local anesthesia and appropriately disposes of the sharp instruments. The dental assistant is then responsible for sterilizing or disposing of the remaining equipment. Either the operator or the assistant can give the patient post-operative instructions concerning the local anesthesia following the procedure.
Preparation
The patient’s medical history, including any medical conditions, medications, and allergies, should be reviewed as this can affect the choice of the anesthetic agent. The patient’s weight should be known to avoid exceeding the safe dose of anesthetic solution. The dental syringe is assembled by the operator or dental assistant, confirming the anesthetic agent to be utilized and its expiry date. Under good lighting, local anesthesia is administered with the patient in the dental chair in a supine or semi-supine position. Anatomical landmarks are observed before administering the local anesthesia. Furthermore, the application of topical anesthesia or freezing can be considered before injection to reduce discomfort.[6]
Technique or Treatment
Infiltration Anesthesia
Buccal Infiltration
The needle is inserted 2 or 3 mm into the buccal sulcus adjacent to the tooth to be treated. The solution diffuses across the periosteum and alveolar bone to anesthetize the nerves supplying sensation to the tooth, periodontium, and buccal gingiva.[16]
Infiltration anesthesia is commonly reserved for the maxilla because the maxilla’s porous structure allows the anesthetic solution to easily penetrate the bone.[6] However, the introduction of articaine has facilitated mandibular buccal infiltrations. Articaine has a high lipid solubility and can be used for buccal infiltrations in the posterior mandible as an alternative to or to supplement an IANB. Success rates of 84 to 94% have been reported for the ability of articaine buccal infiltrations to anesthetize the mandibular molars.[11][16]
In addition, studies have suggested that palatal anesthesia can be achieved following a maxillary buccal infiltration with articaine, negating the need for a separate palatal infiltration.[18]
Palatal Infiltration
A palatal infiltration can be administered to anesthetize the nasopalatine or greater palatine nerve endings, thus providing anesthesia to the palatal gingiva. This injection is often described as painful due to the separation of the tightly-bound mucoperiosteum from the underlying hard palate bone. Methods to reduce discomfort may include topical anesthesia, cooling, applying pressure with a mirror handle, or slightly retracting the needle before injection.[1]
Intrapapillary Infiltration
Intrapapillary (also known as transpapillary) infiltration can sometimes be used to avoid the need for a palatal infiltration. Following a buccal infiltration, the needle is inserted across the buccal interdental papilla and advanced above the alveolar bone to reach the palatal papilla. This technique anesthetizes the palatal interdental papilla and palatal free gingiva. Intrapapillary infiltration is commonly used for primary teeth.[1]
Maxillary Blocks
The posterior superior alveolar block is used to anesthetize the maxillary molars, excluding the mesiobuccal root of the first molar. It also anesthetizes their periodontium and the adjacent buccal soft tissues. The needle is inserted 15 mm into the buccal vestibule distal to the malar at 45 degrees to the occlusal plane, and 1 ml of anesthetic solution is injected.[2]
The middle superior alveolar block anesthetizes the maxillary premolars, the mesiobuccal root of the first molar, their periodontium, and adjacent buccal soft tissues. The needle is inserted 5 mm into the buccal vestibule adjacent to the maxillary second premolar, and 1 ml of anesthetic solution is given.[2]
The anterior superior alveolar block anesthetizes the maxillary incisor and canine teeth, periodontium, and buccal soft tissues. The needle is inserted 5 mm into the buccal vestibule of the maxillary canine, and 1 ml of anesthetic solution is given.[2]
The infraorbital block serves to anesthetize the ipsilateral maxillary teeth, periodontium, buccal soft tissues, maxillary tuberosity, and the skin of the lower eyelid, nose, cheek, and upper lip.[4] The needle is parallel to the second premolar and inserted into the mucosa above this tooth. The operator’s fingers of the non-dominant hand are placed over the infraorbital rim, and the needle is inserted until palpated in the vicinity of the infraorbital foramen. Alternatively, an extraoral approach can be used by inserting the needle through the skin and muscle in the mid-pupillary line after locating the inferior border of the infraorbital rim.[19]
The greater palatine block anesthetizes the ipsilateral hard palate posterior to the canine tooth. The needle is inserted at the entrance of the greater palatine foramen to a depth of less than 5 mm until the bone is contacted and 0.5 ml of anesthetic solution is injected. The greater palatine foramen is a palpable depression or soft area on the hard palate, usually at the third maxillary molar level or 5 mm anterior to the hard and soft palate junction and halfway between the gingiva and palate midline.[2][4]
The nasopalatine block anesthetizes the palatal premaxilla bilaterally. In some patients, it further provides some anesthesia to the maxillary incisors. Following buccal and intrapapillary infiltrations, the needle is inserted into the blanched incisive papilla to a depth of less than 5 mm until the bone is contacted and the tip contacts the lateral soft tissue of the incisive papilla. 0.25 ml of anesthetic solution is usually sufficient.[2]
Mandibular Blocks
Inferior Alveolar Nerve Block (IANB)
The IANB anesthetizes the ipsilateral mandibular teeth, periosteum, lower lip, chin, and the buccal soft tissues from the premolars to the midline.[2] The lingual nerve is generally anesthetized simultaneously, providing anesthesia to the ipsilateral lingual soft tissues, tongue, and floor of the mouth. For this technique, it is essential that the patient fully opens their mouth; otherwise, the IAN relaxes away from the lingula tip, and anesthesia may not be achieved.[11]
The dental syringe is positioned above the contralateral premolars. A long needle is inserted 1 to 1.5 cm superior to the mandibular occlusal plane into the pterygotemporal depression to reach the pterygomandibular space.[2][9][11]
The pterygotemporal depression is located between the pterygomandibular raphe and the coronoid notch of the mandibular ramus. The coronoid notch is the most concave point on the anterior ramus, and it can be palpated with the non-dominant hand before the injection. The needle is inserted 20 to 25 mm until the bone of the crista endocoronoidea is contacted.[11]
The needle is then withdrawn 1 to 2 mm, aspiration is performed to prevent intravascular injection, and 1.5 ml of anesthetic solution is delivered. The needle is then withdrawn halfway, and the remaining solution is given to anesthetize the lingual nerve. Nonetheless, an IANB usually anesthetizes the lingual nerve even if this last step is omitted.[2] Anesthesia onset is generally three to five minutes.[11]
Gow-Gates Technique
The Gow-Gates technique blocks the mandibular nerve adjacent to its division into auriculotemporal, inferior alveolar, mylohyoid, lingual, and buccal nerves [2]. Therefore anesthetizing all these nerves and providing anesthesia to the ipsilateral mandibular hard and soft tissues, anterior two-thirds of the tongue, the floor of the mouth, buccal mucosa, and the skin of the zygoma and temple.[12]
The patient should open their mouth fully to allow the condyle to rotate and translate forwards. The operator palpates the condyle and retracts the cheek with their non-dominant hand. The syringe is placed at the level of the contralateral mandibular canine, and a long needle is inserted at the level of the upper second molar and just below the lateral pterygoid muscle insertion.[2] The needle is advanced 25 mm to contact the bone of the condylar neck.[11]
The needle is then withdrawn 1 mm and the solution injected following aspiration.[2] The patient should be asked to maintain their mouth open for 20 seconds following the injection.[11]
For experienced clinicians, the Gow-Gates approach is associated with a higher success rate and a lower risk of positive aspiration than the conventional IANB.[2][11] The higher success rate may be attributed to anesthetizing nerves that provide accessory innervation, such as the mylohyoid nerve. However, it has a slower onset of anesthesia of 5 to 25 minutes, and, in inexperienced clinicians, it can be associated with higher rates of complications and failure.[11]
Vazirani-Akinosi Technique
The Vazirani-Akinosi technique, also known as the closed-mouth block, is helpful for patients with trismus or when the landmarks used for a conventional IANB are not clearly defined. This technique anesthetizes the inferior alveolar, mylohyoid, lingual, and buccal nerves in 5 to 7 minutes.[11]
The patient’s mouth remains closed with the muscles of mastication relaxed, and the operator palpates the coronoid process before the injection. A long needle parallel to the maxillary occlusal plane is inserted between the coronoid process and the maxillary tuberosity at the level of the maxillary posterior teeth mucogingival junction.[11]
The bevel of the needle should point away from the ramus to ensure deflection occurs towards the ramus. The needle is advanced to a depth of half the anteroposterior width of the ramus. For most adults, this depth is 25 mm from the maxillary tuberosity, and the hub of the needle sits above the mesial aspect of the upper second molar.[2] The anesthetic solution is injected following aspiration. In this technique, the bone should not be contacted; bone contact means that the needle was inserted too laterally.[11]
Mental and Incisive Blocks
Although the mental and incisive nerves are anesthetized by an IANB, mental and incisive blocks are useful when bilateral anesthesia is desired on or anterior to the mandibular premolars.[2]
A short needle is inserted in the buccal sulcus next to the mental foramen, usually located between the premolar apices. The needle is inserted 5 to 6 mm with the bevel facing the bone, and the anesthetic solution is administered following aspiration. Gentle pressure and massaging at the injection site for two minutes allow the anesthetic solution to enter the mental foramen to anesthetize the incisive nerve. The mental and incisive blocks provide anesthesia to the premolar, canine, incisor teeth and their periodontium, buccal soft tissues, the lower lip, and the chin. However, anesthesia of the lingual tissues is not provided.[2]
Buccal Nerve Block
The buccal nerve block is administered when anesthesia of the buccal mucosa or the buccal gingiva of the mandibular molars is required. The needle is advanced 1 to 3 mm into the buccal vestibule distal to the second or third molar until the bone is contacted. The point of insertion is medial to the coronoid notch. A small amount of anesthetic solution, usually 0.25 ml, tends to suffice.[2]
Modified IANB Techniques
Table 1 outlines examples of modified IANB techniques described in the literature
| Modified IANB by Thangavelu et al. |
The syringe is placed at the contralateral canine or premolar teeth and inserted 6 to 8 mm superior to the halfway point between the upper and lower occlusal planes and 8 to 10 mm posterior to the anterior aspect of the ramus. The needle is advanced 21 to 24 mm, with continuous bone contact. Anesthetic solution is delivered following aspiration. This technique has shown a high success rate of 95% and a lower risk of complications such as positive aspiration, hematoma, nerve damage, trismus, and needle breakage. However, it traumatizes the periosteum of the medial ramus.[11] |
| Arched needle technique |
The needle is bent and inserted at an angle of almost 90 degrees to the ramus. The rationale for this technique is that it helps overcome the risk of inserting the needle too posteriorly, which can lead to complications, including transient facial paralysis and failure of anesthesia.[11] |
|
Modified IANB by Palti et al |
Two wires are used to estimate the location of the mandibular foramen. The first wire approaches from the contralateral first permanent molar or second primary molar, along their mesiobuccal groove and distolingual cusp. The second wire is parallel to the ipsilateral occlusal plane. The wires intersect at the mandibular foramen, and this is the point where the anesthetic is injected. A higher success rate has been reported in children than adults, but further evidence is required.[11] |
|
Mandibular foramen anterior technique by Takusugi et al |
The needle is inserted anterior to the mandibular foramen to reduce the risk of vascular and nerve injury. The syringe barrel is positioned above the contralateral first molar, and the needle is inserted 1 cm superior to the occlusal plane and at a depth of 1 cm. A success rate of 75% has been suggested for this technique.[12] |
| Indirect IANB or Fischer 1-2-3 technique | This is a three-step technique with the anesthetic solution delivered using three different needle positions. First, the operator palpates the external oblique ridge with the thumb of the non-dominant hand, and the syringe barrel is placed on the contralateral premolars. The needle is inserted on the midpoint of the thumbnail to a depth of 6 mm. The needle is then withdrawn, and the syringe repositioned to be parallel with the ipsilateral occlusal plane. This allows the needle to slip onto the internal oblique ridge. In this second position, the needle is inserted 8 mm. Finally, the syringe is moved back to the contralateral first premolar. The needle is inserted 12 to 15 mm until it contacts the bone. The anesthetic solution is injected following aspiration at these three locations.[12] |
|
Modified IANB by Boonsiriseth et al |
The syringe is placed parallel to the ipsilateral mandibular occlusal plane. A long needle with a rubber stop at 20 mm is inserted in the pterygotemporal depression to a depth of 20 mm as measured by the rubber stop. The bone is not contacted, and there is a lower risk of pain, positive aspiration, nerve injury, and vascular injury.[12] |
Supplemental Anesthesia Techniques
Supplemental techniques can be useful when conventional block and infiltration methods have failed to provide adequate anesthesia.
Intraligamentary Anesthesia
A conventional dental syringe with a short needle or a specialized intraligamental syringe can be used.[7] The needle is inserted into the gingival sulcus at 30 degrees to the tooth’s long axis to reach the periodontal ligament (PDL) space, and it is advanced as far apically as possible.[2][7] The injection is given slowly mesially and then repeated distally.[2]
The anesthetic solution diffuses from the PDL to the adjacent cancellous bone under the high pressure of the injection. Anesthesia onset is rapid, usually within 30 seconds. However, the duration of anesthesia is short, generally lasting 10 to 45 minutes.[7][11]
Reported complications for intraligamentary injections include cartridge fracture due to high pressure; damage to unerupted teeth; damage to the PDL; tooth extrusion; discomfort; and bacteriemia with a potential risk of endocarditis for high-risk patients. The risks of cartridge fracture and discomfort can be mitigated by injecting slowly.[7] Generally, 0.2 ml of the solution is administered over 20 seconds.[2]
The intraligamentary technique is commonly utilized following a failed IANB and appears to be more successful for exodontia than endodontic treatment.[7][11] Intraligamentary injection should be avoided in the infected or inflamed periodontium. It should also be avoided in primary teeth as enamel hypomineralisation or hypoplasia of the developing permanent teeth has been described.[11]
Intraosseous Anesthesia
Specialized intraosseous injection devices are used to drill a small hole through the cortical plate to reach the cancellous bone, and the anesthetic solution is injected slowly through this hole.[2] A small amount of anesthesia is given via local infiltration to the adjacent gingiva prior to perforation to reduce discomfort.[11]
The perforation is made through the attached gingiva at a point 2 mm apical to the junction of two imaginary lines. These lines run horizontally across the buccal gingival margins and vertically to bisect the interdental papilla distal to the tooth to be anesthetized.[7]
Anesthesia onset is rapid, often immediate, and anesthesia usually lasts 15 to 60 minutes, depending on the use of a vasoconstrictor.[11] Intraosseous injection should be avoided near the mental foramen and at sites of periapical infection or periodontal disease.[2][11]
Intrapulpal Anesthesia
A short needle is inserted into the pulp chamber or root canal to a point where there is a tight fit, and 0.2 to 0.3 ml of anesthetic solution is delivered under pressure.[2][7] Anesthesia is achieved due to the pressure rather than the anesthetic solution, and similar results have been observed when using saline solution instead of an anesthetic agent.[11]
Injecting all canals in multirooted teeth has been recommended. In addition, an alternative technique described is allowing the pulp chamber to bathe in the anesthetic solution for 30 seconds.[7]
Intraseptal Anesthesia
A short needle is inserted at 90 degrees into the interdental papilla, 2 mm apical to the gingival margin. A small amount of anesthetic solution is administered when the needle enters the gingiva. The needle is then advanced until the bone is contacted and pushed a further 1 to 2 mm into the interdental septum by applying gentle pressure. Then, 0.2 to 0.4 ml of anesthetic solution is injected over at least 20 seconds. Intraseptal injection should be avoided at sites of infection.[2]
Complications
Allergic Reactions
Allergy to amide local anesthetics is very rare, and an incidence of 0.1 to 1% has been reported. Some patients may have an allergic reaction to the sodium metabisulfite preservative found in many local anesthetics. Allergy to ester anesthetics, such as topical benzocaine, is more common. Allergic reactions can range from aphthous ulceration to anaphylaxis. Clinicians must be able to identify and manage such reactions.[3]
Failure to Achieve Anesthesia
Causes for anesthetic failure include anatomical variations, inadequate technique, patient anxiety, and local infection or inflammation.[9] Anesthetic failure is more commonly associated with the conventional IANB method. The reported success rate of IANB is 80 to 85%. However, lower success rates ranging from 19 to 70% have been described for mandibular molars with irreversible pulpitis.[11]
Accessory innervation is a common cause of anesthetic failure and should be suspected when an IANB provides anesthesia for the lower lip but not the dentition.[11] The mylohyoid nerve can provide accessory innervation to mandibular teeth, and an IANB generally fails to anesthetize the mylohyoid nerve as this nerve branches off superior to the point of injection. Furthermore, the sphenomandibular ligament provides a physical barrier to the diffusion of the anesthetic solution to the mylohyoid nerve, and the mylohyoid nerve sometimes travels within the bone.
The Gow-Gates, Vazirani-Akinosi, or supplemental techniques can help address the mylohyoid accessory innervation. These techniques can also help overcome failure resulting from bifid mandibular canals, a variation that has been described in 0.35 to 1% of the population.[9]
In addition, the buccal and great auricular nerves can provide accessory innervation to mandibular teeth via the retromolar foramen when present.[11] Injecting a small amount of anesthetic into the retromolar area can help anesthetize any accessory nerves entering the retromolar foramina. Furthermore, contralateral incisive nerve innervation is common, and when profound anesthesia in anterior teeth is not achieved, a contralateral incisive nerve block may be required.[5]
There is also a link between skeletal pattern and IANB failure, with a greater risk of IANB failure in patients with retrognathic mandibles. One study found a failure rate of 14.5% for patients with retrognathic mandibles compared to 7.3 % for patients with class I skeletal patterns. This can be explained by the higher position of the mandibular foramen and a smaller mouth opening in retrognathic mandibles, both due to short condyles. Injecting the IANB at a higher point than usual, or using alternative techniques such as Gow-Gates and Vazirani-Akinosi methods, have been proposed to improve anesthetic success in retrognathic mandibles.[20]
Furthermore, infection lowers the pH of the environment, and this acidity can affect the efficacy of local anesthesia. It is recommended that the anesthetic solution is injected as far as possible from the area of infection.[5]
The pH of the anesthetic solution also plays a role. Local anesthesia is generally acidic, with the commonly used lidocaine with adrenaline having a pH of 3.5. Studies have shown that increasing the pH of local anesthetic, for example, by buffering with sodium bicarbonate, can shorten the speed of anesthesia onset and reduce patient discomfort during injection.[10]
Hematoma
Occasionally, blood can extravasate and accumulate to form a hematoma when the needle punctures a blood vessel. A hematoma can cause soreness, facial swelling, and trismus. If a hematoma is suspected, the clinician should apply pressure to help stop the bleeding and ensure hemostasis has been achieved before the patient’s departure.[3]
In addition, there are reported cases of patients where a maxillary artery puncture has led to a hematoma in the infratemporal fossa resulting in pressure in the IAN and lingual nerve, with sensory disturbances such as hyperalgesia, allodynia, and facial pain as a consequence [5]. Due to the higher needle insertion point, there is a greater risk of a maxillary artery or pterygoid plexus injury with the Gow-Gates and Vazirani-Akinosi techniques.[10]
Intravascular Injection
Intravascular injection of local anesthesia can lead to palpations, visual disturbances, headaches, and vertigo. The patient should be monitored and reassured that the symptoms should be transient and self-limiting. An intravascular injection can be prevented by aspirating before injection. The negative pressure of aspiration withdraws blood into the cartridge if the needle tip is inside a blood vessel, warning the operator not to inject the anesthetic solution at this location.[3]
The conventional IANB technique has the highest risk of positive aspiration.[2] The inferior alveolar vessels run posterior to the IAN and can be exposed to trauma from the needle during IANB. In an IANB, the needle must be retracted 1 to 2 mm before aspiration as the inferior alveolar vein may be pinned to the bone, resulting in a false negative result of aspiration.[11]
Methemoglobinemia
Exceeding the maximum dose of ester anesthetics or prilocaine can lead to methemoglobinemia. Methemoglobinemia is when the iron in hemoglobin is changed from a ferrous to a ferric state, creating methemoglobin. The ferric hemoglobin has a high affinity for oxygen, preventing oxygen from dissociating and depriving tissues and organs of oxygen. This can lead to hypoxemia, with symptoms such as shortness of breath and cyanosis. It is a medical emergency, oxygen must be administered, and emergency services contacted. This condition is treated with intravenous methylene blue.[3]
Needle Fracture
Needle fracture is a rare complication of local anesthesia with modern needles. The most common cause of breakage is sudden movement. This usually involves patient movement, but cases of dentist movement, change in needle direction, and sudden swallowing have been reported. Patients may develop symptoms such as pain, trismus, swelling, and dysphagia. A few patients may remain asymptomatic.[21]
Needle breakage is most likely with mandibular nerve blocks and if a needle with a small diameter is used. Therefore, a 27 gauge or less needle should be used for mandibular blocks. A long needle must be used so that at least 5 mm of the needle is outside the mucosa to allow retrieval in the case of breakage. The mandible should be held firmly, and the patient should be advised against sudden movements. Furthermore, forceful or repeated pre-bending of the needle should be avoided, and the needle should be changed if repeated injections are required.
If a needle breaks, the broken fragment should be removed as soon as possible. Broken needle fragments following a mandibular block most commonly sit within the pterygomandibular region. However, migration to the external auditory canal, superficial post-auricular region, and base of the skull has been reported.[21]
Nerve Injury and Altered Sensation
Nerve injury may result from direct injury by the needle, damage to intraneural blood supply leading to a hematoma compressing the nerve, or neurotoxicity of the anesthetic solution. Neurotoxicity is believed to be greater for articaine and prilocaine than lidocaine.[22]
Nerve injury can lead to temporary or permanent loss of sensation. Following an IANB, the reported incidence of temporary IAN and lingual nerve impaired sensation ranges from 0.15 to 0.54%, while permanent sensory loss ranges from 0.0001 to 0.01%.[23]
The nerve at most significant risk of injury during an IANB is the lingual nerve, as it sits close to the mucosa without the bony protection of the lingula or sulcus colli bone.[9][22] Nerve injury with maxillary infiltration is very rare.[22]
When a patient presents with sensory loss following local anesthesia, careful examination of the distribution of sensory loss should be performed. The patient is followed up regularly until resolution, and referral to a specialist should be considered.[22]
Ocular Complications
Ocular symptoms have been described as complications following intravascular injection into the maxillary artery. Retrograde flow of the anesthetic solution to the lacrimal and optic arteries can lead to anesthesia of the oculomotor, trochlear, and abducens nerves. Symptoms may include diplopia, ptosis, ophthalmoplegia, amaurosis, mydriasis, transient vision loss, and periorbital skin blanching. These are generally self-resolving.[3][5]
Psychogenic Reactions
Patient anxiety regarding the administration of anesthesia or the dental treatment itself can lead to increased heart rate, changes in blood pressure, dyspnea, pallor, nausea, vomiting, and syncope.[3]
Soft Tissue Trauma
Patients should be warned that soft tissues such as lips, cheeks, and tongue can still be numb following dental treatment, and care must be taken until the anesthesia fully wears off. There is a risk of patients biting these soft tissues due to poor sensory feedback, leading to soft tissue trauma.[3]
Systemic Toxicity
Toxicity can occur if the maximum safe dose of local anesthesia is exceeded and can lead to neurological and cardiac adverse effects. Excitatory neurological symptoms manifest initially. These may include visual disturbances, sensory disturbances, and seizures. This is followed by depressive symptoms, such as decreased consciousness which could lead to coma and respiratory arrest. Cardiac manifestations can range from tachyarrhythmia to bradyarrhythmia to cardiac arrest. Dental practitioners must be able to recognize and manage symptoms of toxicity.[3]
Toxicity can be avoided by not exceeding the maximum anesthetic dose based on the patient’s weight. Table 2 outlines the maximum dosage for common anesthetic solutions used in dentistry. The percentage of anesthetic solution signifies the grams per 100 ml. For example, a 2% solution has 2 grams in 100 ml, therefore 20 mg/ml.
To calculate the amount of anesthetic agent in a cartridge, the mg/ml figure is multiplied by the total solution in the cartridge, usually 1.8 ml or 2.2 ml. Table 3 illustrates an example of the calculation.[3]
Toxicity is an emergency and, therefore, emergency medical service must be contacted. Management involves supplemental oxygen and intravenous medication, including Intralipid, midazolam if the patient has seizures, and vasopressor if the patient has hypotension or bradycardia. The patient should be monitored for ventricular tachycardia, ventricular fibrillation, acidosis, hyperkalemia, and hypercarbia, and these should be treated accordingly.[3]
Table 2: Maximum dosage for anesthetic solutions commonly used in dentistry
| Anesthetic | Maximum dose |
| Lidocaine with vasoconstrictor | 7 mg/kg (up to 500 mg) |
| Articaine with vasoconstrictor | 7 mg/kg (up to 500 mg) |
| Mepivacaine with or without vasoconstrictor | 6.6 mg/kg (up to 400 mg) |
| Prilocaine with or without vasoconstrictor | 8 mg/kg (up to 500 mg) |
| Bupivacaine with vasoconstrictor | 2 mg/kg (up to 200 mg) |
Table 3: Example of maximum dose calculation
|
A 2.2ml cartridge of 2% lidocaine with vasoconstrictor has 44 mg of lidocaine (20 mg/ml x 2.2 ml = 44 mg). A 70 kg adult can have a maximum of 490 mg of lidocaine with vasoconstrictor (7 mg/kg x 70 kg = 490 mg) 490 mg / 44 mg = 11.1 cartridges Therefore, a 70 kg adult can have a maximum of 11 cartridges of 2.2ml 2% lidocaine with a vasoconstrictor. |
Transient Facial Nerve Palsy
Transient facial palsy is a rare complication and can be immediate or delayed. Immediate palsy can occur due to direct anesthesia of the facial nerve after injection into the parotid gland when an IANB is given too posteriorly. Facial weakness occurs within minutes of the injection and resolves within 3 hours.[24]
Delayed palsy occurs several hours or days after the local anesthetic administration, and recovery can take 24 hours to many months. The mechanism is more complicated, and postulated theories include: the anesthetic agent or mechanical injury from the needle leading to a sympathetic vascular reflex and ischemic neuritis; mechanical trauma leading to the activation of a latent herpes simplex or varicella-zoster virus, and these viral infections leading to neural sheath inflammation and facial palsy; nerve damage due to breakdown products of the local anesthetic; prolonged mouth opening stretching the facial nerve; and intravascular injection. It is important to protect the eye with an eye patch when a patient develops transient facial palsy. Artificial tears and sunglasses are also recommended.[24]
Trismus
Trismus can result from muscle spasticity if the needle pierces through a muscle of mastication or from a hematoma preventing mandible movements. Trismus is usually managed conservatively with a soft diet, analgesia, and physiotherapy.[3]
Clinical Significance
Profound anesthesia is a prerequisite for most dental treatments as it allows the patient to be comfortable and the clinician to deliver treatment.[6][22] Furthermore, given that dental anxiety frequently stems from painful experiences, effective pain management through local anesthesia can be key in preventing and mitigating dental anxiety.[6]
The selection of local anesthetic agents and delivery techniques can influence the efficacy of anesthesia.[6] Subsequently, dental practitioners must have a robust knowledge of the local anesthetic agents and techniques utilized in dentistry, including their indications and contraindications.
Although local anesthesia is rarely associated with serious adverse effects, clinicians must additionally understand the potential complications to ensure patient safety. This must also extend to understanding how best to manage or prevent these complications.
Furthermore, understanding the nerve supply to the dentition and surrounding tissues is essential to ensure that the anesthetic solution is deposited near the nerves supplying the area of interest. In addition, an awareness of possible anatomical variations allows the clinician to understand why anesthesia might fail and what methods can be utilized to overcome failure.
Failure to achieve anesthesia can delay treatment and cause the patient to lose confidence in the clinician and dentistry. Clinicians must understand why anesthesia can fail and be able to utilize alternative techniques where conventional methods have failed.
Enhancing Healthcare Team Outcomes
All members of the dental team have a responsibility to ensure patient safety. The operator and dental assistant should ensure that the anesthetic solution has not expired and the maximum dose is not exceeded.
The dental team members must be aware of the risk of toxicity and understand how to prevent, identify, and manage toxicity. All team members must also be able to recognize and address any medical emergencies that may occur during or after the administration of local anesthesia. Dental assistants can also play a key role in patient care, for example, by providing reassurance to anxious patients. All team members must work together to deliver patient-centered care to ensure good patient outcomes.
Media
(Click Image to Enlarge)
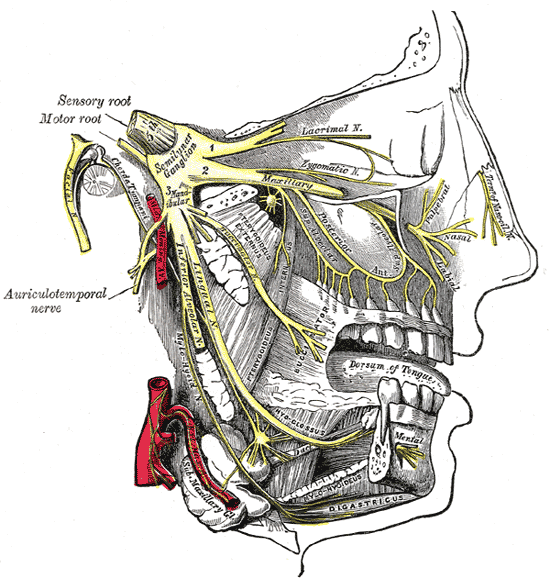
Trigeminal Nerve Divisions. This illustration shows the distribution of the 3 trigeminal nerve divisions. The ophthalmic division gives rise to the lacrimal nerve and supplies the superior third of the face and skull. The maxillary division supplies the midfacial region. The mandibular division innervates the muscles of mastication and gathers sensory information from the lower third of the face. The trigeminal nerve's semilunar ganglion and sensory and motor roots are also shown.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
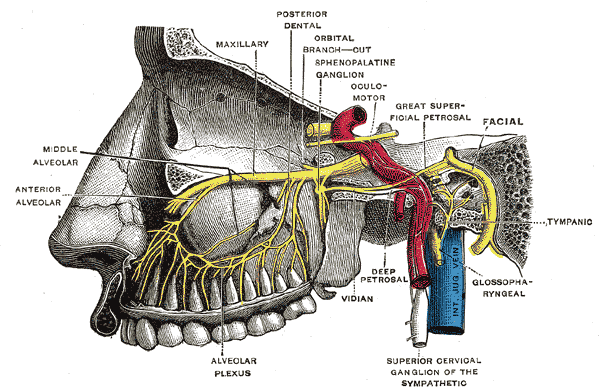
Facial and Trigeminal Nerve Interactions in Lacrimal Gland Function. This illustration shows the facial and trigeminal branches contributing to lacrimal gland function and includes the maxillary, great superficial petrosal, facial, deep petrosal, and Vidian nerves. Other labeled nerves include the anterior and middle alveolar, posterior dental, orbital, glossopharyngeal, and oculomotor nerves, as well as the alveolar plexus. Ganglia in this section include the sphenopalatine and superior cervical ganglia. Blood vessels include the internal carotid artery and internal jugular vein.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
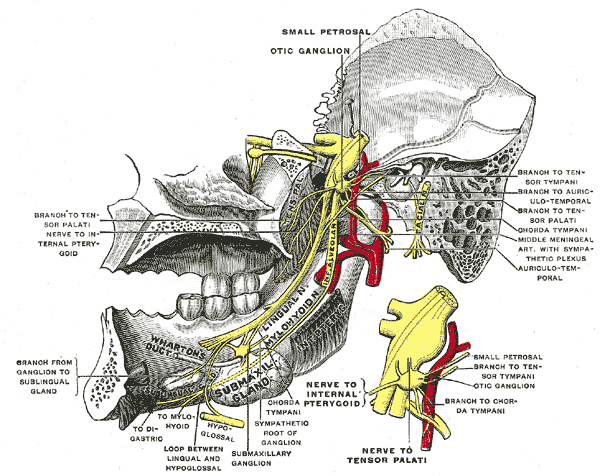
Trigeminal Nerve. The image shows the mandibular division of the trigeminal nerve from the midline. The small figure provides an enlarged view of the otic ganglion.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
References
Sruthi MA,Ramakrishnan M, Transpapillary Injection Technique as a Substitute for Palatal Infiltration: A Split-mouth Randomized Clinical Trial. International journal of clinical pediatric dentistry. 2021 Sep-Oct; [PubMed PMID: 34934275]
Level 1 (high-level) evidenceReed KL,Malamed SF,Fonner AM, Local anesthesia part 2: technical considerations. Anesthesia progress. 2012 Fall; [PubMed PMID: 23050753]
Decloux D,Ouanounou A, Local anaesthesia in dentistry: a review. International dental journal. 2020 Sep 17; [PubMed PMID: 32944974]
Tomaszewska IM,Zwinczewska H,Gładysz T,Walocha JA, Anatomy and clinical significance of the maxillary nerve: a literature review. Folia morphologica. 2015; [PubMed PMID: 26050800]
Somayaji SK,Acharya SR,Mohandas KG,Venkataramana V, Anatomy and clinical applications of the mandibular nerve. Bratislavske lekarske listy. 2012; [PubMed PMID: 22794519]
Wang YH,Wang DR,Liu JY,Pan J, Local anesthesia in oral and maxillofacial surgery: A review of current opinion. Journal of dental sciences. 2021 Oct; [PubMed PMID: 34484571]
Level 3 (low-level) evidenceMeechan JG, Supplementary routes to local anaesthesia. International endodontic journal. 2002 Nov; [PubMed PMID: 12453016]
Takezawa K,Ghabriel M,Townsend G, The course and distribution of the buccal nerve: clinical relevance in dentistry. Australian dental journal. 2018 Mar; [PubMed PMID: 28646596]
Khoury JN,Mihailidis S,Ghabriel M,Townsend G, Applied anatomy of the pterygomandibular space: improving the success of inferior alveolar nerve blocks. Australian dental journal. 2011 Jun; [PubMed PMID: 21623801]
Kini S,Somayaji K,Acharya S,Sampath S, Anomalies and Clinical Significance of Mylohyoid Nerve: A Review. Clinical, cosmetic and investigational dentistry. 2020; [PubMed PMID: 33116912]
Lee CR,Yang HJ, Alternative techniques for failure of conventional inferior alveolar nerve block. Journal of dental anesthesia and pain medicine. 2019 Jun; [PubMed PMID: 31338418]
Kim C,Hwang KG,Park CJ, Local anesthesia for mandibular third molar extraction. Journal of dental anesthesia and pain medicine. 2018 Oct; [PubMed PMID: 30402548]
Guimaraes CC,Lopes LC,Bergamaschi CC,Ramacciato JC,Silva MT,Araújo JO,de Andrade NK,Motta RHL, Local anaesthetics combined with vasoconstrictors in patients with cardiovascular disease undergoing dental procedures: systematic review and meta-analysis. BMJ open. 2021 Jul 15; [PubMed PMID: 34266837]
Level 1 (high-level) evidenceLee JM,Shin TJ, Use of local anesthetics for dental treatment during pregnancy; safety for parturient. Journal of dental anesthesia and pain medicine. 2017 Jun; [PubMed PMID: 28879335]
Corbett IP,Ramacciato JC,Groppo FC,Meechan JG, A survey of local anaesthetic use among general dental practitioners in the UK attending postgraduate courses on pain control. British dental journal. 2005 Dec 24; [PubMed PMID: 16395370]
Level 3 (low-level) evidenceDougall A,Apperley O,Smith G,Madden L,Parkinson L,Daly B, Safety of buccal infiltration local anaesthesia for dental procedures. Haemophilia : the official journal of the World Federation of Hemophilia. 2019 Mar; [PubMed PMID: 30817070]
Wahl MJ,Miller CS,Rhodus NL,Kämmerer P,Dinkova A,Lalla RV,Bajkin BV, Anticoagulants are dental friendly. Oral surgery, oral medicine, oral pathology and oral radiology. 2018 Feb; [PubMed PMID: 29249522]
Chandrasekaran D,Chinnaswami R,Shanthi K,Dhiravia Sargunam AE,Kumar KS,Satheesh T, A Prospective Study to Assess the Efficacy of 4% Articaine, 0.5% Bupivacaine and 2% Lignocaine using a Single Buccal Supraperiosteal Injection for Maxillary Tooth Extraction. Journal of pharmacy [PubMed PMID: 34447189]
Fitzpatrick TH,Downs BW, Anatomy, Head and Neck, Nasopalatine Nerve StatPearls. 2022 Jan; [PubMed PMID: 30860693]
You TM,Kim KD,Huh J,Woo EJ,Park W, The influence of mandibular skeletal characteristics on inferior alveolar nerve block anesthesia. Journal of dental anesthesia and pain medicine. 2015 Sep; [PubMed PMID: 28879267]
Acham S,Truschnegg A,Rugani P,Kirnbauer B,Reinbacher KE,Zemann W,Kqiku L,Jakse N, Needle fracture as a complication of dental local anesthesia: recommendations for prevention and a comprehensive treatment algorithm based on literature from the past four decades. Clinical oral investigations. 2019 Mar; [PubMed PMID: 29959599]
Level 2 (mid-level) evidenceSambrook PJ,Goss AN, Severe adverse reactions to dental local anaesthetics: prolonged mandibular and lingual nerve anaesthesia. Australian dental journal. 2011 Jun; [PubMed PMID: 21623806]
Carter E,Yilmaz Z,Devine M,Renton T, An update on the causes, assessment and management of third division sensory trigeminal neuropathies. British dental journal. 2016 Jun 24; [PubMed PMID: 27338902]
Tzermpos FH,Cocos A,Kleftogiannis M,Zarakas M,Iatrou I, Transient delayed facial nerve palsy after inferior alveolar nerve block anesthesia. Anesthesia progress. 2012 Spring; [PubMed PMID: 22428971]
Level 3 (low-level) evidence