Introduction
An avulsion fracture is a failure of bone in which a bone fragment is pulled away from its main body by soft tissue that is attached to it.[1][2] Avulsion fractures can occur in any area where soft tissue is attached to bone. The failure of bone most commonly results from an acute event with the application of usually sudden, tensile force to the bone through the soft tissue, or when chronic repetitive avulsive stresses lead to a piece of bone being pulled away by the soft tissue.[3][4][5][6] Less commonly, avulsion fractures can also be a complication from a surgical procedure, or the result of a pathologic condition such as a genetic defect, infection, or neoplasm.[1][7][8][9]
Soft tissue attachments to bone can include ligaments, tendons, sub tendon sheaths, joint capsule, labrum, retinaculum, meniscus, or syndesmosis.[10][7][11][12][13][14][15]
Avulsion fractures, as a topic, is very broad, with diverse mechanisms, clinical scenarios, presentations, and a wide range of appropriate management depending on where it occurs. They can represent small or large fractures.[16][5][11][14][17] Clinical significance can be benign or extremely clinically relevant.[18][19][20][21][22][23][5][14] Although size is a consideration, and often significant, size does not necessarily correlate with clinical significance in every injury.[16][17][16][18][11][22][24][11]
Avulsion fractures often happen near joints due to large numbers of supporting osseous, tendinous, and capsuloligamentous structures in a relatively close anatomic space, or at apophyseal myotendinous attachment sites.[10][23][9][5][11][25][26][9] Some areas of the body incorporate many individual joints in very close approximation like the wrist and hand; while other joints like the knee, have multiple articulating surfaces within the joint itself, each with a complex, sometimes overlapping network of muscles, tendons, ligaments, meniscus and capsular attachments that all play a role in both function and stability of the joint.[27][28]
Some types of avulsion fractures are quite common, and many others are very rare, but may remain clinically significant.[29][14]
These injuries are important to recognize because they are frequently associated with other concomitant soft tissue, or osteocartilaginous injuries, or can indicate joint instability.[22][16][4][23][18][11][27][29][14]
Fracture patterns, along with information such as patient age, can provide information for the injury mechanism as well as predict stability and predict associated soft tissue injuries.[10][23][18][30][5][3][31][32][33][25][27][12][29][13][14][34] The addition of an avulsion fracture to an intra-articular soft tissue injury may indicate more significant instability than what is normally seen.[35] Certain avulsion fracture patterns are so reliable that the presence of the avulsion fracture itself is pathognomonic for specific associated injuries or pathologies.[8][1][7][32][33][11][25][35]
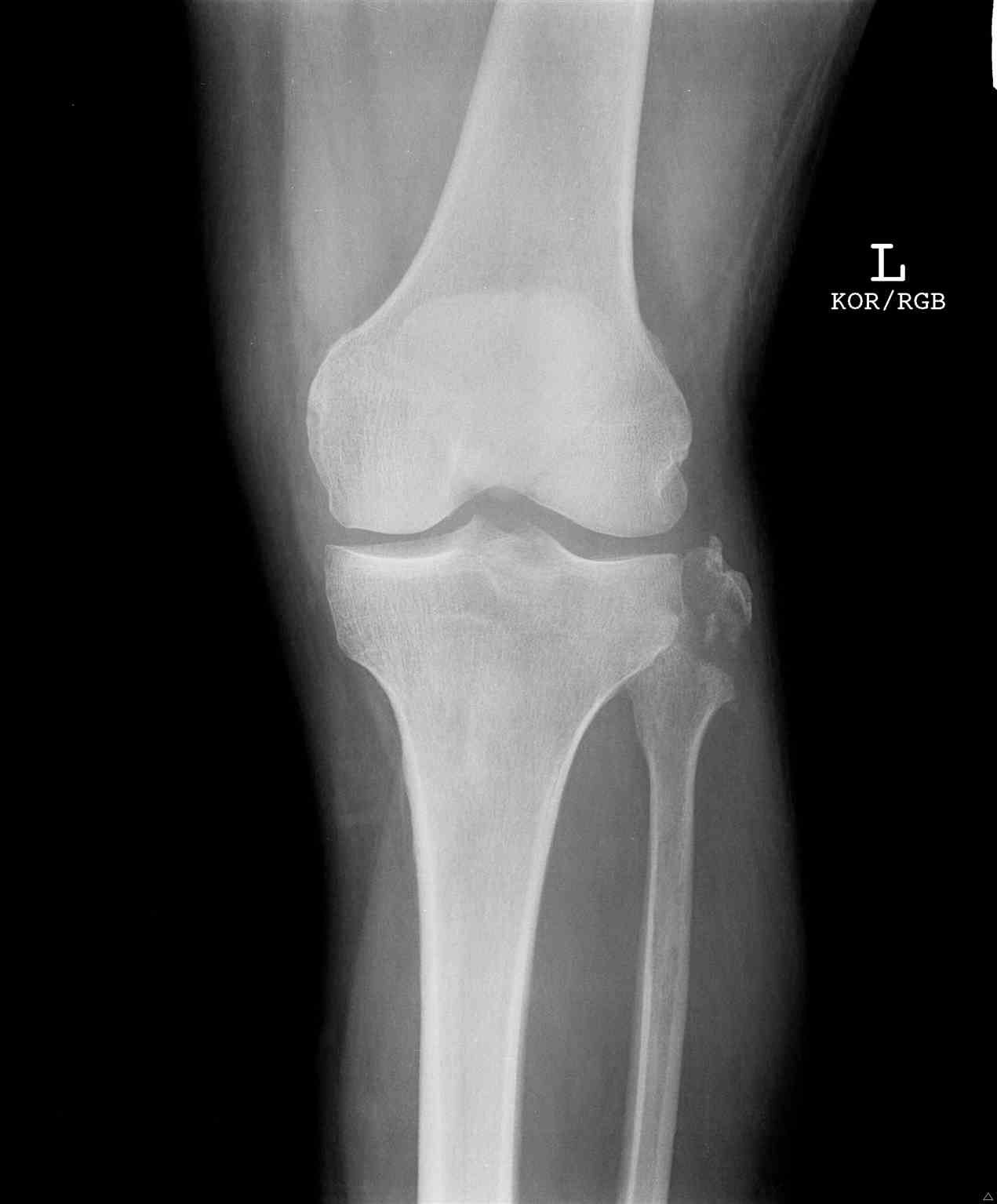
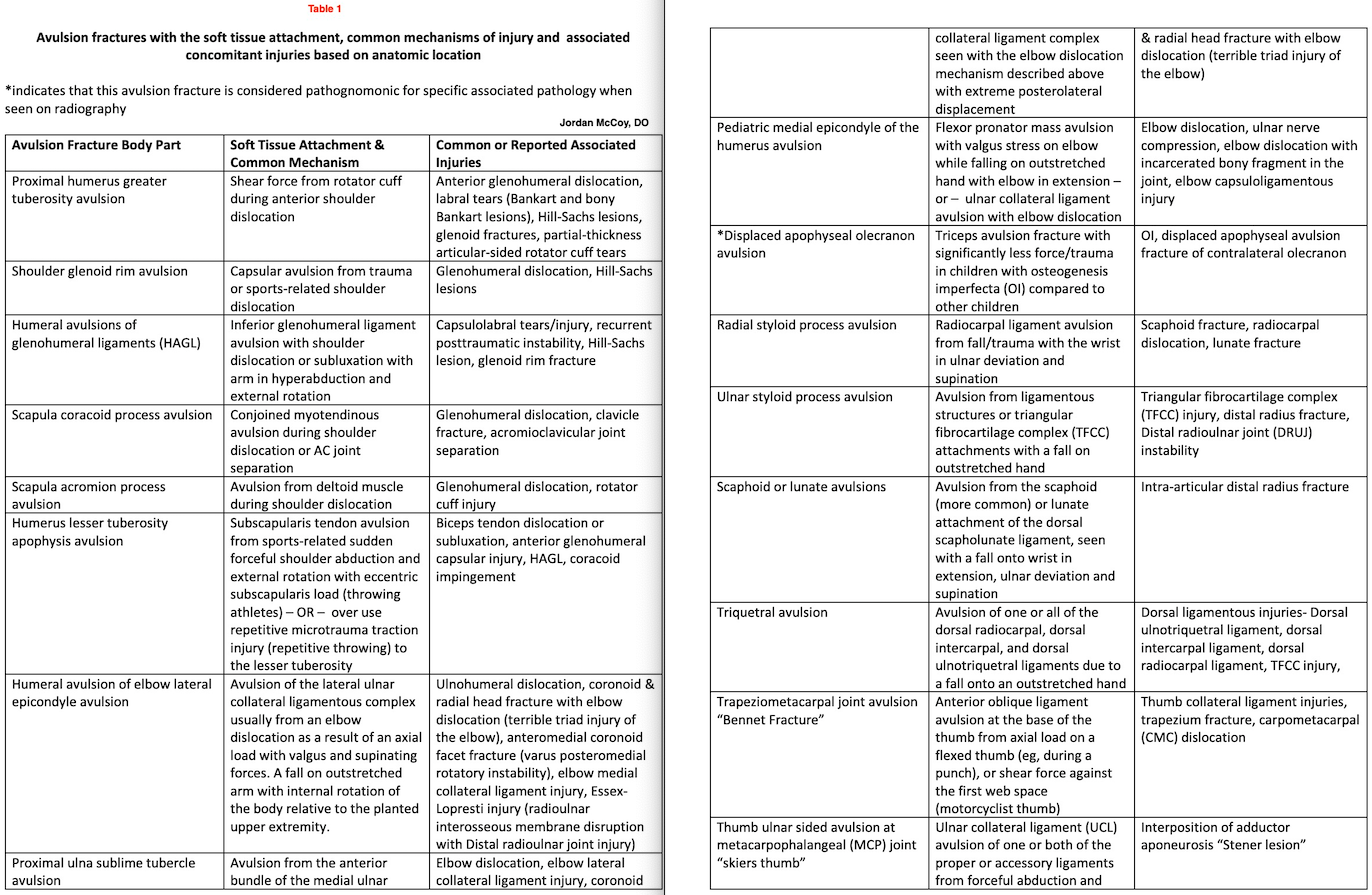
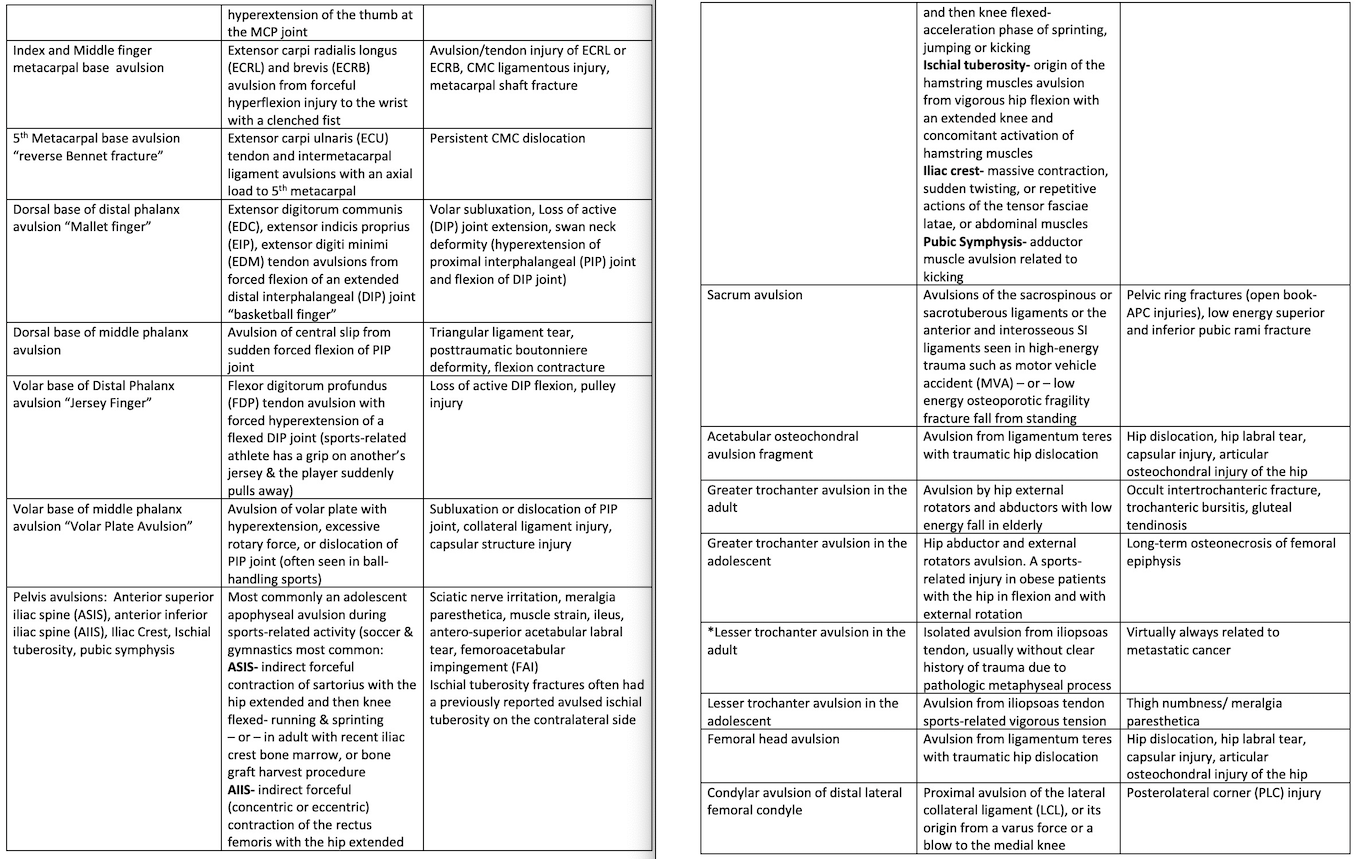
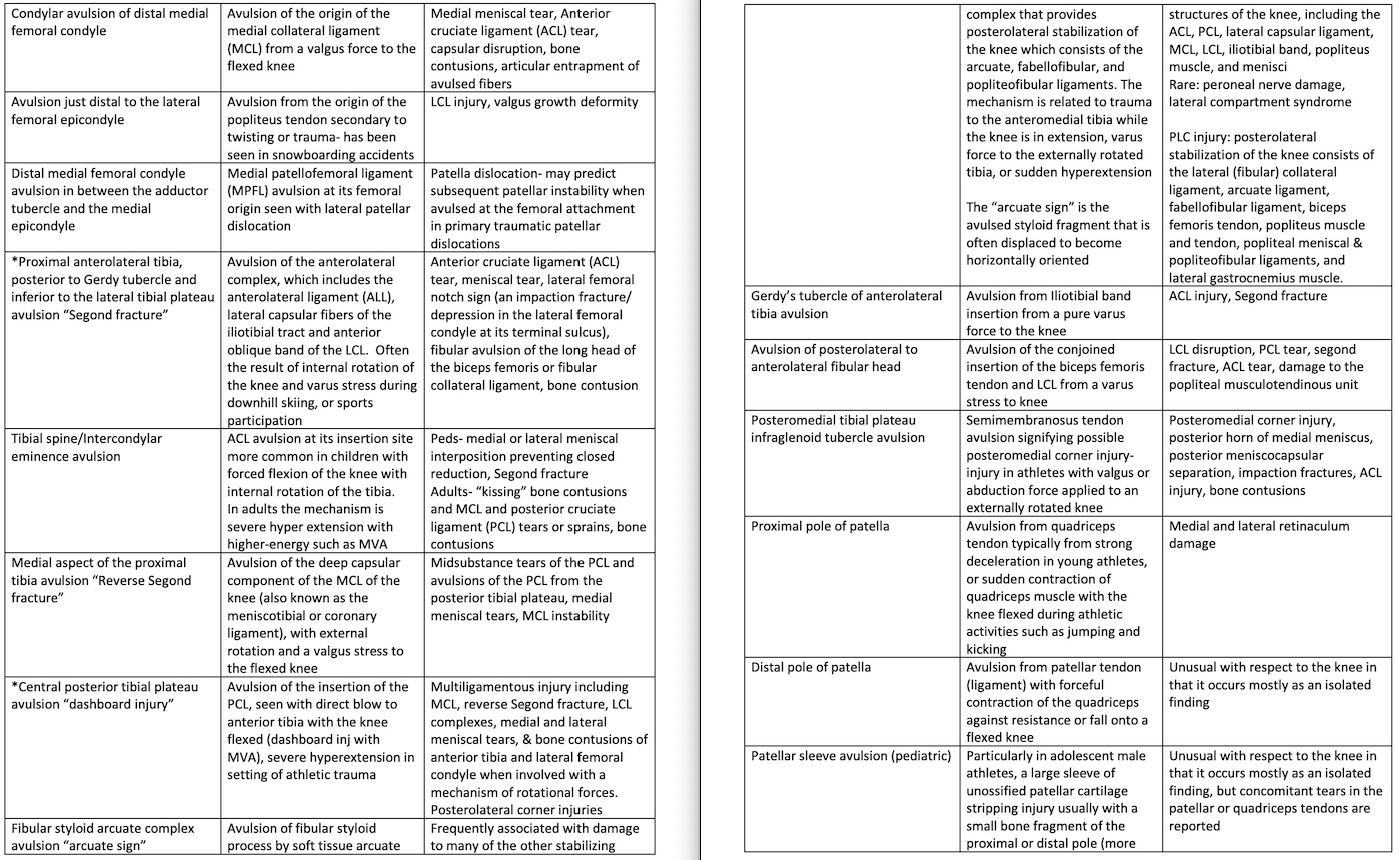
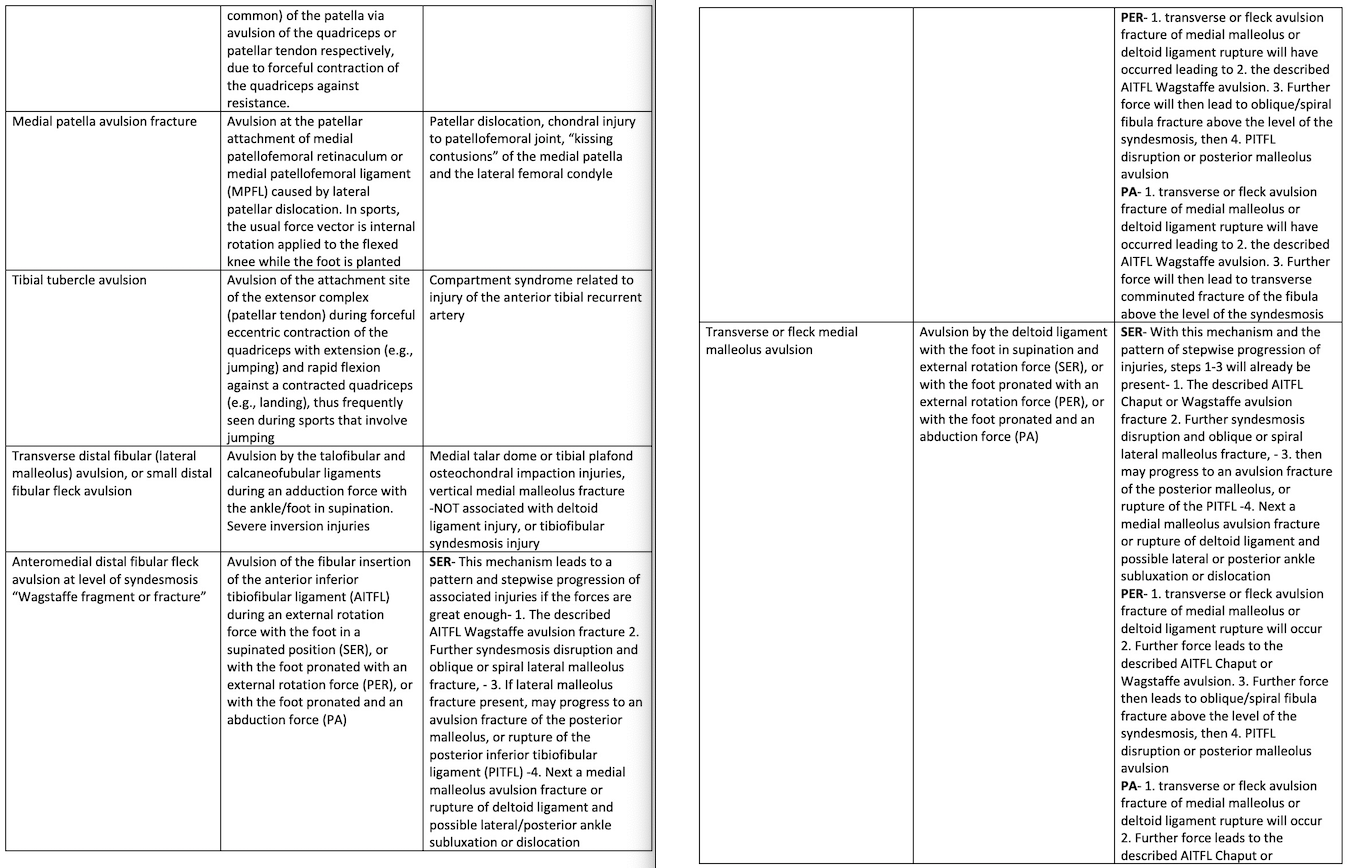
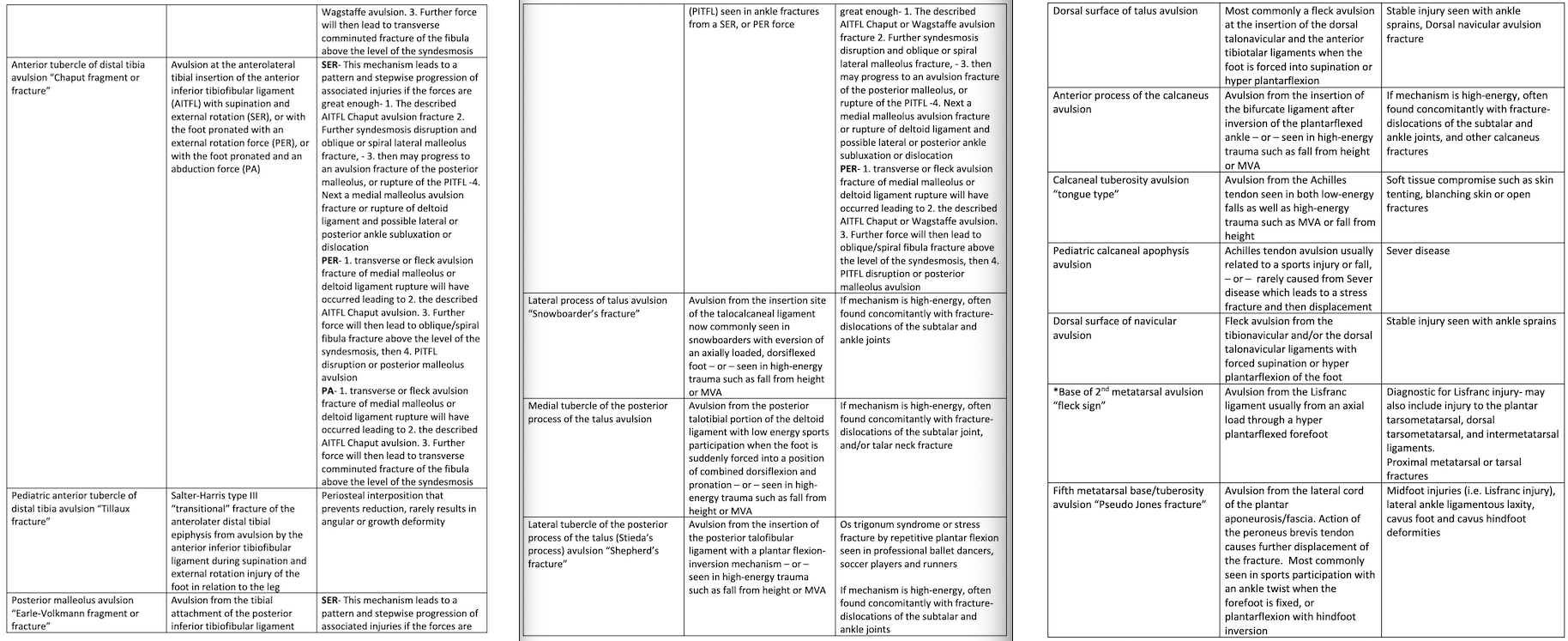
In general, these fractures can occur in adult, adolescent, or pediatric populations, with common characteristics specific to each anatomic location.[1][4] Each specific anatomic avulsion fracture likely warrants specific attention with deeper study beyond this general review. Table 1 provides a list of avulsion fractures by anatomic location along with the avulsing soft tissue attachments, common mechanisms of injury, along with common or reported associated pathologies (see images 1-5).
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Acute trauma is the most common cause of avulsion fractures. This can be direct or indirect trauma, with both high and low-energy mechanisms described.[10][4][23][19][11][36] Sports-related trauma and injuries are common inciting causes of avulsion fractures.[22][16][4][18][3][37][6][38] Avulsion fractures associated with surgery or a pathologic process are other causes.[1][32]
Epidemiology
Certain fracture types tend to be more common in adolescents, and tend to be associated with sports-related injuries.[18][1][3][9][37][2] Adolescent avulsions most often involve a secondary apophysis, which is a growth plate that does not contribute to longitudinal growth and has been described as similar to a “transitional fracture” of the lower extremity.[4][18]
Adults avulsion fractures, on the other hand, tend to have a higher association with traumatic injuries.[10][22][16][24][31][11][6]
The true prevalence or incidence of many avulsion fractures is not known. Accurate incidence is difficult to know because most of the literature regarding avulsion fractures is comprised of case reports and case series.[1][3][35] This is not only due to a lack of well-defined population-based cohort studies, but also the fact that many people who sustain these injuries may not seek treatment, and many of these injuries can be subtle or missed.[27] Failure to diagnose subtle avulsion fractures is reported with polytrauma patients as well.[15] Incidence is likely underestimated due to these factors.[20][28]
Epidemiologic information varies entirely based on anatomic location and age. Avulsion fractures in certain anatomic areas can be quite common.[5] Overall, the prevalence seems to be highest among adolescents.[1] For example, a recent study found the incidence of Segond fractures in patients with anterior cruciate ligament (ACL) injury was 7.4% but stated the true rate might be as high as 15% due to a high incidence of healed Segond fractures that were also seen.[35] Similarly, current literature shows an incidence of syndesmotic avulsion fracture injuries in 10% to 23% of all ankle fractures and up to 25.8% in ankle fractures that require surgery.[14][28]
It is generally agreed that the prevalence may be increasing due to earlier and more frequent participation in sporting and other athletic activities in young people, with higher demands on growing body parts.[18][19] Increasing awareness and better imaging techniques such as more widespread use of MRI could be other reasons for the perceived increase in the prevalence of avulsion fractures.[9][37][11]
In pediatric and adolescent age groups, males are 3 to 5 times more likely than girls to sustain an avulsion fracture.[4][18][1][3][32][11][2][38]
While the prevalence of avulsion fractures is difficult to know, avulsion fractures overall do have a very high prevalence of associated soft tissue injuries that occur in conjunction with them.[29][26]
Pathophysiology
Pathophysiology
An avulsion fracture occurs when a ligament or other soft tissue attachment to bone overcomes the stress capacity of the bony attachment and tears off a portion of the bone. This usually occurs with forces applied from trauma.[16][24][18][29] The traumatic force can be direct, indirect, or a traction force with axial load.[5]
The anatomic position of some ligaments put them at risk with traumatic mechanisms involving external directional or rotational forces specific to that body part.[14][26]
Some avulsion fractures can become quite displaced due to the distracting soft tissue forces, while the displacement of the avulsed fragment in other areas is prevented from migration by additional soft tissue attachments that remain intact; therefore, holding it relatively non-displaced, or very close to its attachment site.[3][21]
The pathophysiology of sports-related injuries is often related to throwing, the eccentric phase of any sporting activity, rapid acceleration or deceleration, kicking, running, jumping, or abrupt changing of direction.[19][4][18][1][9][2][18]
In the adolescent population, avulsion injuries are almost always the result of failure through the apophysis.[2] An apophysis is a secondary ossification center that contributes to peripheral but not longitudinal skeletal growth.[3] A reason that avulsion fractures are more common among adolescents is because of the apophyseal growth plate that is in between the soft tissue attachment site (the apophysis), and the body of the bone. The Sharpey’s fibers attaching the muscle to the apophysis are stronger than the junction of cells between the calcified and uncalcified apophysis. This weaker junction of cells where the separation usually occurs is in the zone of hypertrophy of the physis.[37] The physis is susceptible to avulsion fractures due to the relative weakness of this area during the period of skeletal growth and maturation that is experienced in adolescent years.[29] The stage of development of bone is a crucial consideration when dealing with avulsion fractures, similar to “transitional fracture” injuries.[1][39] As opposed to long bone epiphyseal growth centers, some secondary ossification centers of the pelvic bones, for example, appear later and tend to fuse at a later age.[3] The concept that there is a relative increase in muscle size, strength, and force being applied through the apophysis in this age group is supported by the fact that virtually every avulsion fracture of the pelvis occurs at adolescent apophyseal sites unless there is some other underlying pathology.
The described imbalance between muscle strength and the weaker unfused apophysis increases with continued growth and maturation until the physis fuses.[7] In addition to this, another reason that these fractures are more common in the adolescent population rather than younger pediatric patients could also be related to hormonal changes in the growth plates. It has been found that epiphyseal cartilage in rats is weakest at the time of pubescence.[3][9]
Bony avulsions are less common overall in adults because once the physis closes or ossifies, the connection between the apophysis and the body of bone becomes stronger, and is no longer the weakest structure in the transference of force between the soft tissue and the bone.[1] Thus, adults are more likely to sustain soft tissue ligamentous, myotendinous, or muscle injuries in situations where an avulsion fracture may occur in the adolescent.[3][7][2][29]
In some areas of the body, the pathophysiology of avulsion fractures is altogether unique. For example, in adolescent tibial tubercle avulsion fractures, the portion of the proximal tibial physis deep to the ossifying tibial tubercle apophysis is composed of fibrocartilage until just before physeal fusion. Close to the time of fusion, this fibrocartilage segment is replaced by weaker hyaline cartilage, which predisposes the tibial tubercle to avulsion fractures during this distinct age and timeframe of development.[29]
The reason behind avulsion fractures in the post-surgical setting may be due to the weakening of bone from removal or alteration during surgery. For example, avulsions of the anterior superior iliac spine, commonly only seen in adolescents, is reported in adults after undergoing bone harvesting procedures from the iliac crest.[1] Other pathologies such as osteomyelitis or cancer can cause intramedullary destruction and adjacent periosteal elevation in areas deep to, or near soft tissue attachment sites.[3]
Mechanisms
The avulsion mechanism at a myotendinous attachment site involves an indirect muscle pull such as forceful flexion or extension of a joint against a myotendinous contraction attempting to move the joint in the opposite direction.
There are many cases with no external trauma, where a body part can be forced into extreme ranges of motion. In such scenarios, there is likely an associated protective forceful muscular contraction that leads to the avulsion of bone.[1] This is seen with sudden excessive passive lengthening of a large muscle group, such as performing the splits.[3]
Dislocation of a joint can cause indirect forces from the distraction force resulting in capsular avulsion fractures, or Shear injury.[22] Dislocation in one direction with attached tendons pulling the piece of bone at their attachment site causes the avulsion fracture as the attached tendon shears away the bony fragment from the main bone.[10][5] Depending on the joint, this same mechanism during dislocation can cause a ligament to provide the avulsion force.[18] There may also be a combination of both a direct force or blow to an area of bone where it is also pulled in the same direction by ligaments or soft tissues attached to the avulsed fragment.[13]
The most common mechanism of avulsion fracture in the adolescent population is sudden tension across an open apophysis from the forceful contraction of a large muscle. Often in an attempt to accelerate or decelerate a limb or the body mass.[3]
Chronic mechanisms whereby avulsion fracture can be the result, stem from repetitive traction, microtrauma, and overuse traction-type injuries.[4][18] Pre-existing pain or osteitis, apophysitis can be seen before an avulsion fracture.[1][9]
Along with avulsion fractures, the mechanism by which so many associated soft tissue injuries occur varies with each joint or body part. These additional soft tissue injuries which happen in concert with avulsion fractures may not be seen or apparent on imaging. Whether the visualized avulsion injury or its associated soft tissue injury occurred first, the general concept that stabilizing soft tissues each plays distinct and intertwined roles in physiologic movement and ranges of motion remains the same. Disruption of one stabilizing structure as a result of the injury force can drastically affect or cause injury to many other related stabilizing soft tissue structures or the cartilage. Without the protection of the normal physiologic restraints, the force and instability lead to additional unnatural forces and further potential destruction.
History and Physical
History
Depending on the level of severity and institution, the initial assessment and management of a patient presenting from trauma may be overseen by the trauma service. Adhering to the principles and protocols of Advanced Trauma Life Support (ATLS) should always take precedence if indicated.
When obtaining a patient history upon initial presentation of an avulsion fracture, the provider must obtain information regarding inciting event. In the setting of trauma, one must determine if the patient sustained high versus low-energy trauma. Discerning the mechanism is important.[15] Typically avulsion fractures have a specific presentation and a specific patient history involving the mechanism.[1][19][37][2] The mechanism can elucidate pathology likely to be encountered and provide insight into the treatment strategy. Questions regarding the patient’s activity, such as sports participation, the position of the limb or injured body part at the time of injury, the direction of force, or the occurrence of any dislocation help determine the exact mechanism. It is important to try to distinguish joint subluxation versus frank dislocation because complete dislocation is accompanied by a higher rate of associated injury.[10][22][16] Thus, one should also determine if there are symptoms of numbness, tingling, or weakness.
It can be helpful to find out if symptoms are worse with activity, improve with rest, if this has happened before, or if this is a recurrent issue or injury. Patients with continued pain and a preexisting diagnosis of muscle strain or apophysitis should raise concern for an avulsion fracture. Along the same lines, a history of an acute event without previous pain may help differentiate a minimally displaced acute avulsion fracture from the chronic avulsion changes that might appear similar.[29]
Providers must also find out if the patient has a history of cancer or infection.[3] If a patient is presenting with a history of surgery, or a known genetic or pathologic condition such as osteogenesis imperfecta, osteomyelitis, or cancer, the patient may present with minimal trauma such as rising from a seated position or tripping and may even present with no clear traumatic incident.[1][3][32]
In many trauma scenarios, the patient can be unsure of their body position and mechanism of their injury; or there are conflicting stories from witnesses. Likewise, the patient may be unconscious or unable to communicate. Similar to forensic science, in the context of avulsion fractures, it is possible to make an accurate diagnosis as well as determine the mechanism, and find other associated occult injuries, even with very limited, or contradicting information. A thorough physical exam accompanied with the appropriate background knowledge and radiographs may be all that is needed to make the diagnoses to direct appropriate management and follow up.[13]
Physical Examination
Patients may present with pain, swelling, a palpable gap, visible deformation, decreased range of motion, local tenderness, discomfort, guarding, weakness, bruising, inability to bear weight, mild limitation of activity, sudden loss of function, or possibly chronic pain preceding the injury.[3][18][23][26][37][23][3] The adolescent population often experience pain and a popping sensation at the site of injury and difficulty with ambulation.[1]
Providers should attempt to observe the patient’s gait or active range of motion if possible, as well as look for skin tenting or dimpling.[2][20]
Direct palpation of the injured area, specifically trying to derive the area of maximal point of tenderness, can be an essential diagnostic feature in distinguishing a peripheral fracture from an uncomplicated sprain.[15] Very bone-specific palpation seems to be especially useful in the foot and ankle assessment.[38]
Because avulsion fractures are often associated with instability or dislocation, altered function, loss of range of motion, and loss of normal mechanics may be encountered.[10][22][16][24] Therefore, especially in injuries near or involving a joint, the provider should evaluate neurovascular status and stability. This includes an assessment of gross motion, passive range of motion, ligament integrity, block to motion, muscle function, weakness, and crepitus.[10][16][23]
In general, one should always examine the joint above and below the injured body part.[30] It can be very helpful to examine the contralateral, uninjured corresponding body part of a patient for comparison of laxity, range of motion, and strength.[16][20]
During the physical exam addressing an avulsion fracture, the provider must check for associated injuries. For example, in many avulsion fractures about the shoulder, shoulder stability, as well as the biceps tendon, may need to be evaluated.[4] Certain avulsion fractures have additional injuries that are consistently sustained and present together. One such example is the Segond fracture, which is an avulsion fracture of the tibial attachment of the anterolateral ligament and is pathognomonic for an anterior cruciate (ACL) tear.[40] In that scenario, recognition of the Segond avulsion on the plain film radiograph should lead the examiner to assess the integrity of the ACL, obtain additional or more advanced imaging, and initiate appropriate follow up. Lachman’s test may be performed, which is the most sensitive exam test to assess injury to the ACL.[11][25]
One point to consider is that it can be difficult to assess a patient with an acute swollen body part accurately; therefore, the patient may need to be reexamined 10 to 14 days after the injury.[15] Similarly, after hemodynamic stabilization of polytrauma patients, multiple repeat full-body secondary surveys are sometimes required. A repeat examination may also be indicated any time an unconscious or obtunded patient becomes more alert. This can prevent a missed or delayed diagnosis.
Although rare, certain avulsion fractures have a high association with compartment syndrome even without high-energy trauma. Therefore compartments must always be assessed on presentation. In such fractures, even when presenting without signs or symptoms of compartment syndrome, the high association may justify the need to proceed acutely for surgical fixation. If it is determined that immediate surgery is not necessary, observation and serial compartment checks of the extremity may be warranted in these patients.[2]
Lastly, if a patient does present with a fracture-dislocation with the joint still dislocated, the physical examination components discussed above, especially the neurovascular status should be assessed both before and after the reduction is performed.[18][30]
Evaluation
The combination of a good history and an awareness of the characteristic presentations of avulsion fractures should lead to consistent diagnostic accuracy.[3] Knowledge of anatomy and common presentations regarding avulsion fractures is vital to understand. A high clinical suspicion is important to diagnose and direct treatment or additional workup. Physicians should know which soft tissue structure attaches to each avulsed fragment of bone, and be able to identify all possible fragments.[23][18][30][3][37][2][10][22][16][5] This can be essential to identify concomitant injuries or soft tissue entrapment because those findings can be key factors in determining which patients are likely to benefit most from operative or nonoperative management.[36][26]
Knowledge of developmental bone anatomy and physeal closure sequences is very important when evaluating bony injuries in the pediatric or adolescent population.[18][39] What appears to be a very small bony fragment on plain film may be an extensive cartilaginous injury.[11][6]
At the time of initial evaluation, the first imaging study should include plain radiographs.[10][24][30][5][9][19][37][11][25][27]
In some circumstances, gravity-assisted, stress tests, or weight-bearing radiographs can help with a diagnosis of stability, or additional capsuloligamentous or muscle injuries.[18][17][15][26] It can be helpful to obtain comparison radiographs of the contralateral body part. This may help to assess gapping or laxity that can be a normal anatomic variant in that patient. In the pediatric population, this is also something to consider to compare the appearance and location of ossification centers.
Radiographic features alone can provide a wealth of knowledge in injuries involving avulsion fractures. By the anatomic location, fracture pattern, orientation, displacement, and amount of comminution, one can often derive the mechanism, as well as predict additional ligamentous or other common associated soft tissue injuries that are encountered with each avulsion injury.[13]
General radiographic features of acute avulsion fractures often involve small bony fragments with irregular or sharply defined non-sclerotic, non-corticated edges, with the fragment in close proximity to a known soft tissue attachment site.[25] Associated radiographic findings of soft tissue swelling, loss of tissue planes, a non-concentric joint, widened joint space, or effusion might increase suspicion of missed injury or avulsion fracture.[18] This may be in addition to signs of chronic avulsion injuries such as fragmentation or enthesophyte formation.[6]
It is important to note that spontaneous reduction of a traumatically dislocated joint may occur in any joint. This must be taken into consideration whenever there is an avulsion fracture near a joint, which clinically and radiographically appears located on the initial presentation. In these patients, if there is a painful joint with a lack of complete congruity of the joint, spontaneous reduction with interposition within the joint should be suspected. There are certain common avulsion fracture injuries, such as the patella dislocation-relocation injury, in which the patella rarely remains dislocated at the time of initial imaging.[29]
The only other radiographic finding, in addition to the avulsion fracture, is often a joint effusion or soft tissue swelling. Since these are common findings present after minor trauma, this can wrongfully lead a provider to disregard the injury.[11][36] For example, in the patella dislocation-relocation injuries discussed above, which on plain film appear fairly benign with joint effusion and nondisplaced small avulsed piece of bone, up to 95% of are found to have an associated articular cartilage lesion.[29]
Many injuries may require an additional computed tomography (CT) scan to assess comminution, displacement, and assist with operative planning.[22][24][23][18][30][15] Other injuries benefit from studies such as magnetic resonance imaging (MRI) to evaluate any incongruity, chondral damage, soft tissue integrity, or malalignment.[16][4][11][27][23]
Each avulsion fracture site typically has a common fracture pattern, but also a common pattern of injury or associated injuries. Thus, identification is crucial so that patients may be worked up appropriately, including consultation with an orthopedic surgeon and additional imaging as circumstances dictate.[11]
An example of how radiographic patterns can help determine the diagnosis or inciting factor is a radiographic clue sometimes seen with avulsion injuries associated with chronic overuse of calcifications within, or near attachment sites of a tendon.[11] Other patterns, such as distinct bone bruise combinations seen on magnetic resonance imaging (MRI), are extremely specific to individual injuries.[6][27] An additional example is seen with the radiographic assessment of ankle fractures. Based on the location and type of avulsion fractures present on an ankle fracture, one can predict the mechanism of injury as well as additional soft tissue deltoid ligament or syndesmotic injury.[13]
The avulsion fracture itself can be subtle, and diagnosis may be difficult, missed, or delayed.[15] Acute injuries are usually missed due to inaccurate history, incomplete physical examination, or improper imaging.[19][6][20][10][22][4][30][9][37][11][36][41][20]
Clinical suspicion that an avulsion fracture is present but not visualized on plain radiograph should lead to further workup, including advanced imaging such as CT, MRI, or ultrasound.[37][35] These studies often pick up the avulsion fracture, or other highly associated injuries, and adequately define the extent of the damage.[11][7][15][10][22][16][24][30][5][3][19][33][11]
Another scenario in which one should consider a more advanced workup is in the patient presentation with suggestive radiographs, but history and exam that does not match up with a clear mechanism or history of injury. In this case, one must rule out other bone lesions or underlying pathologies, including cancer and infection.[3][32]
Lastly, if a patient presents with a grossly dislocated joint that requires reduction, post-reduction imaging must be obtained. Attention to any widening of the joint space, or a nonconcentric reduction may indicate a trapped osteochondral fragment or may indicate significant instability.[30] In some joints such as the hip, a post-reduction CT scan is considered the standard of care for the evaluation of incarcerated boney fragments. This is commonly a consideration for elbow and ankle fracture-dislocations as well.
Treatment / Management
The initial treatment of most acute avulsion fractures related to dislocations includes initial reduction attempt and stabilization.[30]
Appropriate treatment modalities are very broad and tailored to each body part. There are many things to consider, which all factor into selecting the most appropriate treatment. Factors that may influence nonoperative treatment versus surgery can be the acuity, size of the avulsed segment, the anatomic site, displacement, associated injuries, instability, high demand patients or high-level athletes, nerve dysfunction resulting from the fracture, hand dominance (when applicable), individual patient occupation or function, intra-articular fracture extension, degree of comminution, or the age of the patient and involvement or extension into an epiphyseal growth plate. Symptomatic malunions or nonunions may also require surgical correction or fixation.[2][10][1][7][5][24][9][29][15][9][2](B2)
With or without surgery, early motion may be the goal with some body parts, with or without bracing, while other avulsion injuries require longer periods of immobilization due to stronger distracting forces.[2][16][23][30][38][2] Some injuries must be immobilized in a position that permits relaxation of the deforming muscle group, decreasing the distracting tensile forces on the fragment.[3][15]
Avulsion fractures may require initial close follow up and even weekly radiographs to evaluate healing, and to monitor for displacement, inadequate reduction or redisplacement.[36][5][37][36](B3)
Similar to many acute musculoskeletal injuries, ice, non-steroidal anti-inflammatories (NSAIDs), rest, and a period of partial or non-weight bearing is often included in the first phase of nonoperative treatment.[3][19][37][3](B3)
Physical therapy, or a carefully directed rehabilitation program, usually with levels of progression, can be beneficial.[16] Advancement is usually based on aspects of clinical evaluation, including radiographic monitoring of the fracture displacement and healing.[3] These programs can include range of motion, strengthening, gait training, proprioceptive recovery, and much more.
A common nonoperative treatment regimen described for patients involved in sporting activities include the following, or similar phases of physical therapy and rehab. Phase one consists of rest, ice, and protection. Phase two initiates a gradual increase in the excursion of the injured myotendinous unit. Phase three begins when 75% of motion is regained, or complete active range of motion without secondary resistance is achieved. In this phase, a patient may begin a guided, progressive resistance program. This phase ends when the involved muscles have reached 50% of their anticipated strength. Phase four is the integrated use of the injured musculotendinous unit with the use of other muscles of the surrounding area and limb. Full weight-bearing is initiated, leading to beginning simple patterns of activity and motion, such as gentle jogging. It is important to continue stretching and strengthening throughout all phases. Phase four is the most common phase at which reinjury occurs. Phase five is the preparation of the athlete for a full return to competitive status. Sufficient callus strength, muscular strength, and agility must be achieved before attempting a return.[3][37]
Treatment in many scenarios, including avulsion injuries, may be controversial. In injuries where definitive treatment is less clear, it may be acceptable to undergo an initial trial of nonoperative management and guided therapy with close monitoring, with surgery as an option if the nonoperative trial is unsuccessful.[37]
Common absolute indications for surgery include open fractures, fracture fragments incarcerated in a joint, gross instability,[18] compartment syndrome, anatomic areas that rarely heal because of strong muscle contraction causing fracture displacement,[2][42] potential skin compromise such as tenting or blanching, or disruption of anatomic features that are vital to normal physiologic function such as the extensor mechanism of the knee.[29]
Fracture blisters and soft tissue trauma may necessitate provisional fixation or delay in definitive surgery to avoid wound complications.[42]
The basic goals of surgery most commonly include open reduction and internal fixation (ORIF) of large or displaced fragments, and to restore articular congruity and stability.[30] Open reduction internal fixation (ORIF) of intraarticular fractures hopes to reduce joint incongruity and prevent instability, long- term development posttraumatic osteoarthritis, and chronic pain. If the avulsion injury leads to instability despite not meeting other surgical criteria, it must be addressed.[24] An additional goal of surgery is to achieve a faster return to sport or full activity.[9] Regardless of what modality is chosen, surgical treatment seeks the benefit of maximizing functional outcomes with increased strength and range of motion while minimizing pain.[30][26]
Despite a provider’s best efforts to avoid surgery, many avulsion fractures require surgical fixation based on the significance, location, and associated conditions or injuries.[10][22][16][24][4][23][18][30] Surgical stabilization may not only allow earlier range of motion, but may also limit complications such as stiffness, instability, and posttraumatic arthritis of specific body parts, which are certain outcomes if treated non-operatively.[23]
The nature of avulsion fractures usually indicates that the ligaments which are attached to bone fragments remain intact; therefore, emphasis toward anatomic reduction and/or fixation is important for the restoration of stability and function.[30] Non-anatomic fixation can lead to adjacent, uninjured joints to become unstable.[23]
In treating avulsion fractures, one must recognize that although bony fixation is important, soft tissue reconstruction can be of most importance in some regions such as the shoulder, elbow, knee, and ankle.[22][17] In many cases, although not desirable, this may require excision of the small or comminuted avulsed bony fragments and reattachment of the soft tissue to bone.[2][15] Other joints may require primary arthrodesis to achieve stability and appropriate outcomes.[26]
Many soft tissue injuries do occur in isolation without avulsion fractures such as ACL tears, but the addition of an avulsion fracture (such as the Segond fracture) in addition to the soft tissue injury may actually indicate more than usual instability and may need to be taken into consideration when fixing the ligamentous or soft tissue injury. Repairing the fracture or performing a reinforcement procedure may be needed to stabilize the joint during reconstruction fully.[35][17]
With any treatment modality or surgery to address a particular issue regarding joint instability, high failure rates or chronic residual instability may be due to the presence of an undiagnosed, missed, or untreated avulsion fracture.[19] The lack of recognition of a concomitant injury, or failure to treat the associated injury is commonly seen with residual shoulder instability, knee injuries, and ankle fractures. For example, recurrent posttraumatic shoulder instability may persist after treatment of tears of the glenoid labrum (i.e., a Bankart lesion) due to failure to recognize or address a humeral avulsion of glenohumeral ligaments (HAGL) lesion. Failure of an anterior or posterior cruciate ligament reconstruction may be secondary to a failure to address posterolateral corner instability. Likewise, in ankle fractures with syndesmotic injury, the bony fractures may be fixed and heal in anatomic position, yet have been found to result in poor outcomes with chronic pain and residual instability if the disrupted syndesmosis is not addressed.[16][11][29][14](B2)
Intraoperative stress testing may need to be performed to assess the stability or soft tissue integrity after repair or fixation of the bone and soft tissues.[28]
In some avulsion fracture cases, treatment is geared toward prophylaxis to prevent other known associated injuries or impending fractures from happening or worsening. One example includes surgical fixation of isolated greater trochanter avulsion fractures in the elderly due to the high rate of occult intertrochanteric fracture extension found on MRI. Prophylactic fixation prevents further displacement or completion of the occult fracture.[33] Another such case is seen with prophylactic fixation of the femur with isolated lesser trochanter avulsion fractures in adults to prevent the highly reported, impending subtrochanteric femur fracture that is likely to ensue.[32](B3)
Differential Diagnosis
- Simple dislocation
- Fracture with a different mechanism, not caused by avulsion or pull of soft tissue
- Hydroxyapatite deposition disease[5]
- Accessory ossicles
- Apophysitis[19][37]
- Posttraumatic or reactive bone lesions
- Chronic tendon abnormalities
- Exostosis
- Myositis ossificans
- Reactive bone lesion
- “Groin pull,” “torn hamstring” or “hip pointer,” muscle spasm, intraabdominal pathology, osteomyelitis, Ewing sarcoma[3]
- Simple muscle strain, tendon tear, tendonitis[9]
- Trochanteric bursitis, gluteus medius, and minimus tears, stress fractures, degenerative arthropathy, stress fracture, entrapment syndromes[7]
- Jumper’s knee, Sinding-Larsen-Johansson syndrome, Osgood -Schlatter disease[11]
- Sesamoid bones, cyamella, bipartite patella, synchondrosis, enthesopathy, benign avulsive cortical irregularity[6]
- Compartment syndrome, hamstring syndrome, athletic pubalgia, Sever disease[2]
- Pellegrini-Stieda lesion[27]
- Os subfibulare[20]
- Os trigonum, posterior ankle impingement[15]
Prognosis
When discussing avulsion fractures as a whole, there are many factors to consider when trying to determine prognosis. The topic is complicated by the fact that a certain side effect after treatment may translate into a poor prognosis in some body parts, yet seem to yield very few negative consequences in other anatomic locations.
In general, the severity of the injury and the speed of the healing process will help determine the prognosis.[3] A greater amount of displacement may be associated with worse outcomes if treated without surgery.[9]
Outcomes of avulsion fractures are largely dependent on the body part involved. While some avulsion fractures tend to be less disabling and less symptomatic, others are much more so.[7][20][7] For example, certain avulsion fracture nonunions are known to cause pain and many other complications, while others, although associated with higher rates of nonunion, are not associated with higher rates of pain, instability, or other clinically significant prognostic factors.[18] Regardless, even asymptomatic nonunions occasionally become symptomatic long after an injury.[20] In general, uncertainty persists regarding optimal treatment and prognosis with many avulsion fracture injuries.[15]
Another prognostic indicator appears dependent on the optimization of stability and articular congruity. However, despite appropriate treatment, avulsion fractures still frequently result in residual stiffness and arthrosis.[30] Thus, even with successful fracture union, if chronic pain and arthrosis develop, patients may require additional surgeries in the future such as arthrodesis, arthroplasty, or other procedures.[15] On the other hand, as mentioned, the prognosis does not seem to be negatively affected in some injuries with a notable loss of range of motion.[18]
Avulsion fractures that are stable injuries and considered insignificant do have better functional outcomes when treatment of early motion and progression of weight bearing is applied compared to patients with the same injury who are treated with a period of immobilization or non-weight bearing.[38]
Early diagnosis may also be a key to obtaining the best outcomes, as it can carefully direct the appropriate treatment.[3] If the injury is not properly diagnosed and treated, or if there is a delay of diagnosis and treatment, then these injuries can be debilitating and lead to negative long-term consequences.[11][25][37] The worst outcomes seem to be found in patients with the longest delay in diagnosis and treatment.[15][26]
Knowledge of developmental bone anatomy, growth, and physeal closure sequences is very important to assist in predicting the prognosis of avulsion injuries in the pediatric or adolescent population. Nevertheless, the adolescent population seems to have a better overall prognosis and higher return to the previous level of sport or activity, while older age and osteoporosis may be associated with worse outcomes.[3][42]
Long-term outcomes of many adolescent avulsion fractures have not been well studied.[9] Some studies found that surgical management may assist in earlier return to full activity, while other studies argue that earlier return is not clear.[37] Surgical patients may have more complications, and further, follow up has revealed comparable results between non-operative and surgical treatments.[9] Actual knowledge is limited due to a lack of standardization in examining functional outcomes as well.[34]
Certain anatomic areas are more prone to recurrent instability or laxity.[36][22][16][41][36] Similarly, patients who have not regained full strength, range of motion, and proper musculotendinous reintegration, are more prone to re-injury and a delayed recovery pattern.[3] In ankle fractures, failure to treat associated soft tissue injuries such as the syndesmosis at the time of fracture fixation will result in chronic ankle instability and post-traumatic arthritis.[14]
One study found that an avulsion fracture associated with an intraarticular soft tissue injury in the knee may indicate more instability, but was not found to have a higher risk of revision surgery compared to those who sustained the same soft tissue injury without the accompanying avulsion fracture.[35] On the other hand, joint rigidity, which does negatively affect outcomes, can occur in up to 60% of surgically treated patients.[36] Other studies have determined fracture patterns can predict a worse prognosis based on whether an avulsion fracture occurred at the origin or insertional attachment site of a ligament. For example, worse outcomes of subsequent patellar instability, and significantly lower ability to regain previous activity levels were able to be predicted with avulsions of the medial patellofemoral ligament at the femoral attachment site in patella dislocations.[12]
Lastly, in cases of avulsion fractures associated with pathologic lesions, such as metastatic cancer, the overall prognosis of the patient may not be affected, or dependent on the treatment and outcome of the avulsion fracture, but rather on the prognosis of the underlying pathologic disease.[32]
Complications
Some complications regarding avulsion fractures are directly related to the injury. The injury alone can lead to heterotrophic ossification, hematoma, cause neurovascular injury or irritation, and loss of proprioception.[9][19][20][10][24][23][9][11] The interposition of tissue with retracted or displaced fractures may result in mechanical block to healing or impingement syndromes.[14][5] Some injuries have a high association with soft tissue compromise or complications.[42] Even when treated appropriately, patients may remain symptomatic for a prolonged period.[15]
Compartment syndrome from avulsion fractures is very rare, or not at all described in some body parts, while certain fractures such as pediatric tibial tubercle avulsion fractures are especially at risk for this complication. One must be extremely vigilant when addressing that injury.[2][23][11][9][11]
In adolescent apophyseal avulsion fractures, the most common complications are painful nonunion and exostosis formation.[37] However, limb length or angular growth abnormalities such as recurvatum, or varus or valgus growth disturbances can occur, which may require additional surgeries.[29][2] The most common complications associated with pediatric tibial spine avulsion fractures are residual laxity, arthrofibrosis, nonunion, malunion, and physeal arrest.[36]
A missed injury or a delay in appropriate treatment has been reported to lead to complications such as pain, nonunion, malunion, recurrent injury or instability, bone loss, bone resorption, erosion, accelerated arthrosis, contracture, loss of function, irreversible injury, avascular necrosis, chronic pain, delayed return to sport, and pseudoarthrosis.[5][23][9][2][3][2] In some instances, delays may also complicate the appropriate surgery as compared to situations in which they are addressed acutely.[10][22][16][24][19]
Even with prompt diagnosis, failure to treat an associated soft tissue injury at the time of fixing the fracture is an avoidable complication and, as discussed, can lead to many other complications.[14]
Because avulsion fractures often involve joints and stabilizing structures, loss of motion should always be discussed with the patient as a possible complication. Some risk factors specific to joint rigidity include delayed treatment, prolonged operative time, malunion, prominent hardware, fracture displacement, reoperations, and prolonged immobilization.[36]
Although necessary for many injuries, surgical intervention of any kind does not come without complications. Commonly discussed surgical complications include wound infection, wound dehiscence, septic arthritis, myositis ossificans, pin-tract infections, blood loss, osteonecrosis, heterotrophic ossification, and nerve injury, although the actual incidence of these complications is low.[37][18][5][9][5] Hardware irritation and the need for removal, weakness, and malreduction are complications that are slightly more common in the treatment of avulsion fractures.[8][9][37][28][37]
Altogether, complications from surgery vary greatly, as the nature of some avulsion fractures require greater exposure with large incisions and more extensive dissections, while others can be adequately treated with minimally invasive, percutaneous, or arthroscopic techniques.[29]
Perhaps most complications occur during the healing or rehabilitation phase after either operative or non-operative treatment has been administered. Inadequate protection or inadequately supervised rehabilitation programs can potentially lead to muscle contracture, nonunion, or weakness.[3] Return to activity when adequate healing has not yet taken place can lead to increased migration of the avulsed fragment and delay or impede healing, or create an abundance of bony growth, which may become symptomatic. Reinjury to an athlete is most likely to occur at a time when they are undergoing rehabilitation and attempt a complete return to participation without full strength and integration of muscle function.[3][9][41]
Deterrence and Patient Education
With appropriate early diagnosis and treatment, many avulsion fracture injuries have satisfactory outcomes. Nevertheless, it is important to understand that regardless of which type of avulsion fracture a patient may sustain, the associated mechanism and additional injuries to surrounding soft tissues may lead to prolonged recovery or complications despite appropriate conservative or operative management of their injury.
In the setting of sports and exercise, it is extremely important to focus on pre-exercise warm-up activities and pre-season strengthening programs as much as possible as preventative mechanisms.[1] Reinjury is common when an injured patient attempts to return to full participation before they are properly rehabilitated or physically ready.[3]
Chronic overuse can lead to significant symptoms of pain and weakness and produce swelling at soft tissue attachment sites to bone. This is due to repetitive microtrauma and avulsive forces, usually related to sports activities or repetitive actions that can be required in some occupations. This occasionally leads to inflammation, weakening, or fragmentation of the bone and can be a precursor or potential risk factor for an acute avulsion fracture in that area.[6] Therefore, these areas of pain should not be ignored and should be addressed with appropriate activity modifications, rest, ice, and in some cases, a period of immobilization to prevent further or potentially worse injury to the area.[2]
Pearls and Other Issues
General pearls, as they relate to avulsion fractures, highlight why they may be clinically relevant compared to many other injuries. Depending on the body part, the pull of the soft tissue that is still attached to the fracture fragment can make reduction, and therefore healing more difficult. This may cause fractures to heal in the wrong anatomic location (malunion), commonly with distraction and rotational malalignment. This can lead to weakness, pain, and dysfunction.[10][4][2]
Related injuries include entrapment of soft tissue structures, fracture extension, intra-articular loose bodies, ligament and supporting tendon, soft tissue, and retinacula injuries.[29]
The rate of neurologic injury is higher in some avulsion fractures if they are associated with dislocation.[10][23]
In cases of residual joint instability, displacement or dislocation, the pull of adjacent or surrounding soft tissue and the fracture itself be an obstruction to the reduction of the fracture and/or a dislocated joint.[24][18]
In general, joints are responsible for varying degrees of complex ranges of motion between bones. Bones provide attachment sites for muscles via tendons, which facilitate movement. Together with ligaments, capsules, and other soft tissues, the muscles and tendons around a joint form a stable soft tissue envelope and allow a base of motion specific to each joint. There are often static and dynamic stabilizers of joints, and the motion and stability of many of these joints rely on coordinated sensorimotor systems. Coordinated muscle contractions in concert with biofeedback from capsuloligamentous structures result in normal motion and functional stability.[24][5] Various joints are more inherently stable than others, while some lack inherent stability.[28][34][26][24] Less stable joints rely more upon the balanced forces of the various muscles, tendons, ligaments, and bones that make up the static and dynamic stabilizers for stability. An avulsion fracture by nature indicates that there is an injury to a stabilizing structure, and can indicate the loss of a soft tissue stabilizer as well as bony restraint.
Prominent in the orthopedic surgery literature and training are certain avulsion fractures that, when recognized, are pathognomonic for other associated injuries or conditions. Displaced pediatric apophyseal avulsion fractures of the olecranon, isolated greater trochanter avulsion fractures in the elderly, adult lesser trochanter avulsion fractures, the Segond fracture, posterior proximal tibial avulsion in a “dashboard injury,” and the “fleck sign” in the foot are six such examples which are briefly discussed below.
It has been recommended that a diagnosis of osteogenesis imperfecta be considered when displaced apophyseal avulsion fractures of the olecranon are seen in the pediatric population with relatively low-energy trauma. This is especially true if the injury occurs bilaterally. In patients with osteogenesis imperfecta who sustain this fracture, they are generally more displaced than children without the disorder, and the risk of incurring the same fracture on the other side is around 70%.[8]
Approximately 90% of elderly adults with an isolated greater trochanter avulsion fracture on plain radiographs have been found to have occult intertrochanteric extension on MRI.[33]
In adults, lesser trochanteric pathology in the setting of avulsion injury without a clear trauma history is virtually always secondary to metastatic disease in the trochanteric region. This should be regarded as secondary to metastatic neoplasm until proven otherwise.[7][32]
The Segond fracture has been extensively documented in association with ACL disruption and meniscal tear that accompany it.[11] It is usually a small avulsion fracture of the anterolateral tibia at the insertion site of the anterolateral ligament (ALL) or of the anterolateral complex, which includes the ALL, lateral capsular fibers of the iliotibial tract and anterior oblique band of the lateral collateral ligament, posterior to the Gerdy tubercle and inferior to the lateral tibial plateau.[35][27][40] It has been shown to have 75% to 100% positive predictive value for an ACL tear.[25] Additional physical exam tests, such as a Lachman’s test to assess the ACL and other soft tissues around the knee, should be performed. Likewise, an MRI must be obtained to assess the extent of internal derangement that is likely to be present in association with the Segond fracture.[6]
A small posterior tibial plateau avulsion fracture seen after a so-called “dashboard injury” in the setting of a motor vehicle accident with an anteroposterior force applied to the proximal tibia on a flexed knee is essentially pathognomonic for posterior cruciate ligament (PCL) injury. Additional physical exam tests to assess the integrity of the PCL and other soft tissues around the knee should be performed, such as assessing for posterior sag of the tibia. Likewise, an MRI must be obtained to assess the extent of internal derangement that is likely to be present in association with the fracture and mechanism of injury.[25][6]
The “fleck sign” seen as a bony fragment in the basal first intermetatarsal space on an anterior-posterior view radiograph represents an avulsion of the Lisfranc ligament and is diagnostic of Lisfranc injury. The Lisfranc ligament is a plantar interosseous ligament spanning from the lateral zone of the medial cuneiform to the medial zone of the second metatarsal. Widening of the interval between the first and second metatarsal bases is often seen, as well as dorsal displacement of the proximal base of the first or second metatarsal on the lateral view. The Lisfranc injury is a tarsometatarsal fracture-dislocation with disruption of the articulation of the medial cuneiform and base of the second metatarsal, which is the unifying factor in the disruption of the tarsometatarsal joint complex. The severity of injuries range, and can be purely ligamentous. Regardless of the type of Lisfranc injury, they must be treated. Missed injuries result in chronic pain, instability, dysfunction, and often progressive foot deformities. Although not diagnostic, a common physical exam finding of plantar ecchymosis at the level of the midfoot is highly suggestive of a Lisfranc injury and has been described as a pathognomonic sign of Lisfranc injury.[26]
Enhancing Healthcare Team Outcomes
Avulsion fractures may be small or have a relatively benign appearance to those unfamiliar with these injuries. The uninformed provider may be inclined to deem these injuries inconsequential, when in fact they are a sign of potentially more severe underlying damage to other major stabilizing structures of a joint.[11] Avulsion fractures potentially indicate more complex injury, often associated with joint instability, or dislocations and are complicated injuries that can be challenging to treat; however, not all of these injuries are equivalent. Understanding body and joint biomechanics and mechanism of injury provide valuable insight into the variations of pathology that may be observed. Identification of the particular fracture pattern encountered at the time of the initial presentation helps guide appropriate treatment and follow up.[30]
Accurate diagnosis is paramount because treatments and potential additional workup differ between each type of avulsion fracture.[19] With a careful understanding of anatomy, mechanism of injury, and treatment options, many of these fractures can be successfully diagnosed and treated acutely in the hope of preventing the chronic morbidity associated with delayed treatment.[37]
Patients with prior chronic apophysitis, or repetitive avulsion injury at the site of tendon insertions, may be at increased risk for acute avulsion injuries.[29] Even in avulsion fractures that are considered insignificant, they need to be recognized early and promptly diagnosed to administer proper symptomatic treatment and appropriate reassurance. If not correctly diagnosed on presentation, patients can be overly concerned that a ‘fracture was missed,’ which can lead to confusion and anxiety.[21]
Avulsions are best cared for by an interprofessional team consisting of primary care providers, emergency medical personnel, radiologists, orthopedists, specialty trained nurses, physiatrists, and physical therapists. [Level 5]
Media
(Click Image to Enlarge)
(Click Video to Play)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Porr J, Lucaciu C, Birkett S. Avulsion fractures of the pelvis - a qualitative systematic review of the literature. The Journal of the Canadian Chiropractic Association. 2011 Dec:55(4):247-55 [PubMed PMID: 22131561]
Level 2 (mid-level) evidenceSchiller J, DeFroda S, Blood T. Lower Extremity Avulsion Fractures in the Pediatric and Adolescent Athlete. The Journal of the American Academy of Orthopaedic Surgeons. 2017 Apr:25(4):251-259. doi: 10.5435/JAAOS-D-15-00328. Epub [PubMed PMID: 28291142]
Metzmaker JN, Pappas AM. Avulsion fractures of the pelvis. The American journal of sports medicine. 1985 Sep-Oct:13(5):349-58 [PubMed PMID: 4051093]
Popkin CA, Levine WN, Ahmad CS. Evaluation and management of pediatric proximal humerus fractures. The Journal of the American Academy of Orthopaedic Surgeons. 2015 Feb:23(2):77-86. doi: 10.5435/JAAOS-D-14-00033. Epub [PubMed PMID: 25624360]
Weintraub MD, Hansford BG, Stilwill SE, Allen H, Leake RL, Hanrahan CJ, Chan BY, Soltanolkotabi M, Kobes P, Mills MK. Avulsion Injuries of the Hand and Wrist. Radiographics : a review publication of the Radiological Society of North America, Inc. 2020 Jan-Feb:40(1):163-180. doi: 10.1148/rg.2020190085. Epub [PubMed PMID: 31917655]
Mellado JM, Ramos A, Salvadó E, Camins A, Calmet J, Saurí A. Avulsion fractures and chronic avulsion injuries of the knee: role of MR imaging. European radiology. 2002 Oct:12(10):2463-73 [PubMed PMID: 12271386]
Nachtrab O, Cassar-Pullicino VN, Lalam R, Tins B, Tyrrell PN, Singh J. Role of MRI in hip fractures, including stress fractures, occult fractures, avulsion fractures. European journal of radiology. 2012 Dec:81(12):3813-23. doi: 10.1016/j.ejrad.2011.04.003. Epub 2011 Apr 29 [PubMed PMID: 21531099]
Gwynne-Jones DP. Displaced olecranon apophyseal fractures in children with osteogenesis imperfecta. Journal of pediatric orthopedics. 2005 Mar-Apr:25(2):154-7 [PubMed PMID: 15718892]
Calderazzi F, Nosenzo A, Galavotti C, Menozzi M, Pogliacomi F, Ceccarelli F. Apophyseal avulsion fractures of the pelvis. A review. Acta bio-medica : Atenei Parmensis. 2018 Nov 15:89(4):470-476. doi: 10.23750/abm.v89i4.7632. Epub 2018 Nov 15 [PubMed PMID: 30657114]
George MS. Fractures of the greater tuberosity of the humerus. The Journal of the American Academy of Orthopaedic Surgeons. 2007 Oct:15(10):607-13 [PubMed PMID: 17916784]
Gottsegen CJ, Eyer BA, White EA, Learch TJ, Forrester D. Avulsion fractures of the knee: imaging findings and clinical significance. Radiographics : a review publication of the Radiological Society of North America, Inc. 2008 Oct:28(6):1755-70. doi: 10.1148/rg.286085503. Epub [PubMed PMID: 18936034]
Sillanpää PJ, Peltola E, Mattila VM, Kiuru M, Visuri T, Pihlajamäki H. Femoral avulsion of the medial patellofemoral ligament after primary traumatic patellar dislocation predicts subsequent instability in men: a mean 7-year nonoperative follow-up study. The American journal of sports medicine. 2009 Aug:37(8):1513-21. doi: 10.1177/0363546509333010. Epub 2009 Apr 17 [PubMed PMID: 19376939]
Level 2 (mid-level) evidenceLAUGE-HANSEN N. Fractures of the ankle. II. Combined experimental-surgical and experimental-roentgenologic investigations. Archives of surgery (Chicago, Ill. : 1920). 1950 May:60(5):957-85 [PubMed PMID: 15411319]
Birnie MFN, van Schilt KLJ, Sanders FRK, Kloen P, Schepers T. Anterior inferior tibiofibular ligament avulsion fractures in operatively treated ankle fractures: a retrospective analysis. Archives of orthopaedic and trauma surgery. 2019 Jun:139(6):787-793. doi: 10.1007/s00402-019-03138-2. Epub 2019 Feb 15 [PubMed PMID: 30770996]
Level 2 (mid-level) evidenceBerkowitz MJ, Kim DH. Process and tubercle fractures of the hindfoot. The Journal of the American Academy of Orthopaedic Surgeons. 2005 Dec:13(8):492-502 [PubMed PMID: 16330511]
George MS, Khazzam M, Kuhn JE. Humeral avulsion of glenohumeral ligaments. The Journal of the American Academy of Orthopaedic Surgeons. 2011 Mar:19(3):127-33 [PubMed PMID: 21368093]
Nwosu K, Schneiderman BA, Shymon SJ, Harris T. A Medial Malleolar "Fleck Sign" May Predict Ankle Instability in Ligamentous Supination External Rotation Ankle Fractures. Foot & ankle specialist. 2018 Jun:11(3):246-251. doi: 10.1177/1938640017729494. Epub 2017 Sep 7 [PubMed PMID: 28877594]
Gottschalk HP, Eisner E, Hosalkar HS. Medial epicondyle fractures in the pediatric population. The Journal of the American Academy of Orthopaedic Surgeons. 2012 Apr:20(4):223-32. doi: 10.5435/JAAOS-20-04-223. Epub [PubMed PMID: 22474092]
Ghanem IB, Rizkallah M. Pediatric avulsion fractures of pelvis: current concepts. Current opinion in pediatrics. 2018 Feb:30(1):78-83. doi: 10.1097/MOP.0000000000000575. Epub [PubMed PMID: 29176354]
Level 3 (low-level) evidenceHaraguchi N, Toga H, Shiba N, Kato F. Avulsion fracture of the lateral ankle ligament complex in severe inversion injury: incidence and clinical outcome. The American journal of sports medicine. 2007 Jul:35(7):1144-52 [PubMed PMID: 17379919]
Level 2 (mid-level) evidenceRobinson KP, Davies MB. Talus avulsion fractures: are they accurately diagnosed? Injury. 2015 Oct:46(10):2016-8. doi: 10.1016/j.injury.2015.06.041. Epub 2015 Jul 7 [PubMed PMID: 26190632]
Bigliani LU, Newton PM, Steinmann SP, Connor PM, Mcllveen SJ. Glenoid rim lesions associated with recurrent anterior dislocation of the shoulder. The American journal of sports medicine. 1998 Jan-Feb:26(1):41-5 [PubMed PMID: 9474399]
Rouleau DM, Sandman E, van Riet R, Galatz LM. Management of fractures of the proximal ulna. The Journal of the American Academy of Orthopaedic Surgeons. 2013 Mar:21(3):149-60. doi: 10.5435/JAAOS-21-03-149. Epub [PubMed PMID: 23457065]
Ropp AM, Davis DL. Scapular Fractures: What Radiologists Need to Know. AJR. American journal of roentgenology. 2015 Sep:205(3):491-501. doi: 10.2214/AJR.15.14446. Epub [PubMed PMID: 26295635]
Beckett R, Le P, Rheinboldt M, Petraszko A. Avulsion fractures of the knee: a review of the pathophysiology, radiographic, and cross-sectional imaging features. Emergency radiology. 2019 Dec:26(6):683-689. doi: 10.1007/s10140-019-01711-1. Epub 2019 Aug 13 [PubMed PMID: 31410608]
Level 2 (mid-level) evidenceMoracia-Ochagavía I, Rodríguez-Merchán EC. Lisfranc fracture-dislocations: current management. EFORT open reviews. 2019 Jul:4(7):430-444. doi: 10.1302/2058-5241.4.180076. Epub 2019 Jul 2 [PubMed PMID: 31423327]
Lee CH, Tan CF, Kim O, Suh KJ, Yao MS, Chan WP, Wu JS. Osseous Injury Associated With Ligamentous Tear of the Knee. Canadian Association of Radiologists journal = Journal l'Association canadienne des radiologistes. 2016 Nov:67(4):379-386. doi: 10.1016/j.carj.2016.02.002. Epub 2016 Aug 4 [PubMed PMID: 27499452]
Rammelt S, Obruba P. An update on the evaluation and treatment of syndesmotic injuries. European journal of trauma and emergency surgery : official publication of the European Trauma Society. 2015 Dec:41(6):601-14. doi: 10.1007/s00068-014-0466-8. Epub 2014 Nov 12 [PubMed PMID: 26037997]
Merrow AC, Reiter MP, Zbojniewicz AM, Laor T. Avulsion fractures of the pediatric knee. Pediatric radiology. 2014 Nov:44(11):1436-45; quiz 1433-6. doi: 10.1007/s00247-014-3126-6. Epub 2014 Oct 21 [PubMed PMID: 25331022]
Wyrick JD, Dailey SK, Gunzenhaeuser JM, Casstevens EC. Management of complex elbow dislocations: a mechanistic approach. The Journal of the American Academy of Orthopaedic Surgeons. 2015 May:23(5):297-306. doi: 10.5435/JAAOS-D-14-00023. Epub [PubMed PMID: 25911662]
Steinke H, Hammer N, Lingslebe U, Höch A, Klink T, Böhme J. Ligament-induced sacral fractures of the pelvis are possible. Clinical anatomy (New York, N.Y.). 2014 Jul:27(5):770-7. doi: 10.1002/ca.22312. Epub 2014 Jan 22 [PubMed PMID: 24452928]
Phillips CD, Pope TL Jr, Jones JE, Keats TE, MacMillan RH 3rd. Nontraumatic avulsion of the lesser trochanter: a pathognomonic sign of metastatic disease? Skeletal radiology. 1988:17(2):106-10 [PubMed PMID: 3363377]
Level 3 (low-level) evidenceKim SJ, Ahn J, Kim HK, Kim JH. Is magnetic resonance imaging necessary in isolated greater trochanter fracture? A systemic review and pooled analysis. BMC musculoskeletal disorders. 2015 Dec 24:16():395. doi: 10.1186/s12891-015-0857-y. Epub 2015 Dec 24 [PubMed PMID: 26704907]
Irwin TA, Lien J, Kadakia AR. Posterior malleolus fracture. The Journal of the American Academy of Orthopaedic Surgeons. 2013 Jan:21(1):32-40. doi: 10.5435/JAAOS-21-01-32. Epub [PubMed PMID: 23281469]
Slagstad I, Parkar AP, Strand T, Inderhaug E. Incidence and Prognostic Significance of the Segond Fracture in Patients Undergoing Anterior Cruciate Ligament Reconstruction. The American journal of sports medicine. 2020 Apr:48(5):1063-1068. doi: 10.1177/0363546520905557. Epub 2020 Mar 2 [PubMed PMID: 32119785]
Tuca M, Bernal N, Luderowski E, Green DW. Tibial spine avulsion fractures: treatment update. Current opinion in pediatrics. 2019 Feb:31(1):103-111. doi: 10.1097/MOP.0000000000000719. Epub [PubMed PMID: 30531228]
Level 3 (low-level) evidenceMcKinney BI, Nelson C, Carrion W. Apophyseal avulsion fractures of the hip and pelvis. Orthopedics. 2009 Jan:32(1):42 [PubMed PMID: 19226032]
Zwitser EW, Breederveld RS. Fractures of the fifth metatarsal; diagnosis and treatment. Injury. 2010 Jun:41(6):555-62. doi: 10.1016/j.injury.2009.05.035. Epub 2009 Jun 30 [PubMed PMID: 19570536]
Ali Al-Ashhab ME, Mahmoud Mohamed AA. Treatment for displaced Tillaux fractures in adolescent age group. Foot and ankle surgery : official journal of the European Society of Foot and Ankle Surgeons. 2020 Apr:26(3):295-298. doi: 10.1016/j.fas.2019.04.001. Epub 2019 Apr 16 [PubMed PMID: 31031149]
Kennedy MI, Claes S, Fuso FA, Williams BT, Goldsmith MT, Turnbull TL, Wijdicks CA, LaPrade RF. The Anterolateral Ligament: An Anatomic, Radiographic, and Biomechanical Analysis. The American journal of sports medicine. 2015 Jul:43(7):1606-15. doi: 10.1177/0363546515578253. Epub 2015 Apr 17 [PubMed PMID: 25888590]
Yamaguchi S, Akagi R, Kimura S, Sadamasu A, Nakagawa R, Sato Y, Kamegaya M, Sasho T, Ohtori S. Avulsion fracture of the distal fibula is associated with recurrent sprain after ankle sprain in children. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2019 Sep:27(9):2774-2780. doi: 10.1007/s00167-018-5055-7. Epub 2018 Jul 10 [PubMed PMID: 29992464]
Mitchell PM, OʼNeill DE, Branch E, Mir HR, Sanders RW, Collinge CA. Calcaneal Avulsion Fractures: A Multicenter Analysis of Soft-Tissue Compromise and Early Fixation Failure. Journal of orthopaedic trauma. 2019 Nov:33(11):e422-e426. doi: 10.1097/BOT.0000000000001582. Epub [PubMed PMID: 31425410]