Introduction
Pustular psoriasis is a rare, immune-mediated systemic skin disorder characterized by yellowish pustules on an erythematous base with a variety of clinical presentations and distribution patterns.[1] Pustular psoriasis is considered a variant of psoriasis vulgaris. The pustules can be widespread or localized and are characterized by a sterile predominantly neutrophilic infiltrate. Unlike chronic plaque psoriasis (the most common variant of psoriasis vulgaris), lesions of pustular psoriasis are often tender to palpation.[2] Pustular psoriasis can be further subdivided based on the clinical presentation and the location of pustules.
Subtypes of pustular psoriasis include:
- Generalized:
- von Zumbusch subtype: Diffuse generalized pustular eruption with associated systemic symptoms (fevers, arthralgias, etc.)
- Annular subtype: Annular lesions with pustules along the advancing edge.
- Exanthematic subtype: Acute pustular eruption without systemic symptoms that resolves after a few days.
- Impetigo herpetiformis: Pustular psoriasis occurring during pregnancy.
- Localized:
- Acrodermatitis continua of Hallopeau: Pustules affecting the fingers, toes, and nail beds.
- Palmoplantar psoriasis: Pustules affecting the palms and soles
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Pustular psoriasis occurs in genetically susceptible individuals and can be triggered by certain risk factors leading to psoriasiform changes and marked neutrophil accumulation in the epidermis.[3] Patients with pustular psoriasis have an increased frequency of the HLA-B27 allele compared to the general population. Most cases of pustular psoriasis are idiopathic, however, risk factors that may have a role in the etiology of pustular psoriasis include [4][5]:
- Sudden withdrawal of systemic steroids
- Skin infections (Staphylococcus aureus)
- Electrolytes imbalance; hypocalcemia (i.e., von Zumbusch subtype)
- Medications (lithium, iodine, penicillin, interferon-alpha, etc.)
- Pregnancy (i.e., impetigo herpetiformis)
- Phototherapy
- Vaccinations (BCG and H1N1)
Epidemiology
Pustular psoriasis is a rare disease. It affects both children and adults in a bimodal age distribution. In the adult age group, the disorder appears between ages 40 to 50, whereas in the pediatric age group, it tends to present in infancy. Asians tend to be more affected than Caucasians.[6] Women and men are affected equally. The pustular variants of psoriasis represent approximately 1% of all clinical cases of psoriasis vulgaris.[5]
Pathophysiology
The exact pathogenesis of pustular psoriasis has not been fully elucidated. However, based on the expression of certain cytokines and responses to specific medications, several mechanisms have been proposed. A combination of genetic susceptibility and exposure to certain inciting factors (e.g., withdrawal of systemic corticosteroids) lead to an upregulation of specific cytokines and accumulation of neutrophils in the epidermis.[5] Additionally, dermal dendritic cells release elastase, which may play a role in the formation of pustules.[7] Both pustular psoriasis and chronic plaque psoriasis exhibit overexpression of IL-1, IL-17, IL-23, IL-36, TNF-alpha, and IFN-gamma. However, the expression of IL-1 and IL-36 are more prominent in pustular psoriasis. Studies have also identified an IL-36 receptor antagonist deficiency in patients with pustular psoriasis and patients with pustular psoriasis have also been successfully treated with a novel monoclonal antibody against the IL-36 receptor.[8] Therefore, IL-36 likely plays a critical role in the pathogenesis of pustular psoriasis.
Histopathology
Many of the histopathological features of pustular psoriasis mimic that of psoriasis vulgaris, including retention of the nuclei in the stratum corneum (parakeratosis), a thick stratum spinosum (hyperkeratosis), elongation of the rete ridges, reduced stratum granulosum, and thinning of the suprapapillary epidermis.[5] In addition to the classic histologic features of psoriasis vulgaris, there is also a prominent neutrophilic infiltrate in the papillary dermis and epidermis, causing basal keratinocytes to herniate into the papillary dermis disrupting desmosomal junctions of keratinocytes (spongiosis), and leading to the development of superficial micro-abscesses.[9] Neutrophilic infiltration of the epidermis is more prominent in pustular psoriasis than other variants of psoriasis vulgaris.
History and Physical
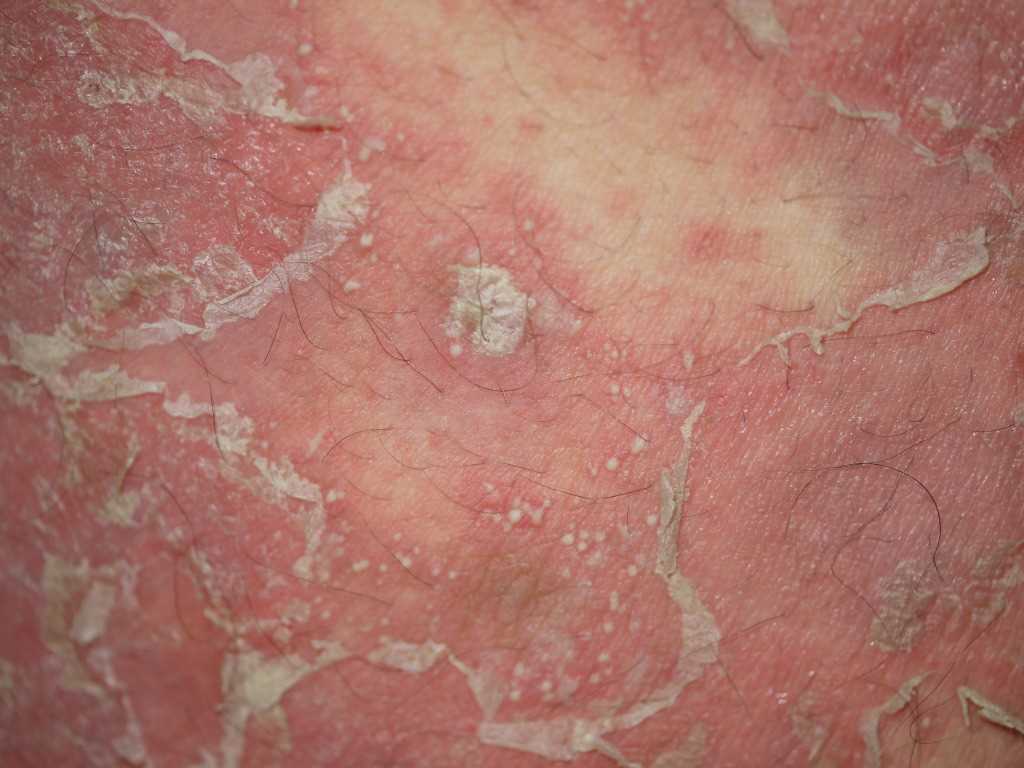
Pustular psoriasis appears as numerous discrete or confluent superficial, yellowish pustules on a background of erythema. Pustular psoriasis can be diffuse or localized. A full body skin examination should be performed, including careful evaluation of the mucous membranes and the nails for other signs of psoriasis and to exclude other causes of pustulosis.
Pustular psoriasis starts as red papules or plaques that quickly evolve into yellowish, superficial pustules on a background of erythema. The generalized von Zumbusch subtype usually presents with systemic symptoms like fever, joint pain, headaches, and leukocytosis. In contrast, the exanthematic subtype presents as an acute pustular eruption without systemic symptoms. The annular subtype is seen more frequently in children as annular lesions with pustules along the advancing edge.[10] Acrodermatitis continua of Hallopeau affects the finger, toes, and nailbeds. Palmoplantar psoriasis, which can be seen as part of SAPHO syndrome, affects the palms and soles.
Evaluation
Patients with suspected pustular psoriasis require careful evaluation, as the von Zumbusch subtype can be life-threatening. Laboratory investigations should include a complete blood count (CBC) to evaluate for leukocytosis, an electrolyte panel to assess for hypocalcemia, and a liver panel to assess for transaminitis. A pregnancy test should be ordered in all women of childbearing age. A punch biopsy can be performed in equivocal cases. Cultures of weeping lesions may be useful to exclude primary or secondary infections.
Treatment / Management
The first step in managing cases of pustular psoriasis is identifying disease triggers, such as an underlying infection. Generalized pustular psoriasis (e.g., von Zumbusch subtype) may require admission to the hospital. Systemic symptoms including fever and joint pain will require treatment with antipyretics and anti-inflammatory medications. Disease-specific medications including systemic retinoids (acitretin, isotretinoin), methotrexate, cyclosporine, and infliximab are considered first-line in adult patients. In pediatric patients, acitretin, cyclosporine, methotrexate, and etanercept are preferred.[11]
Second line options include systemic treatments in diffuse disease (e.g., etanercept and adalimumab) or topical treatments in localized disease (e.g., corticosteroids, calcipotriene, and tacrolimus). All of these options can be used as monotherapy or in combination with first-line options.[12] Phototherapy is another treatment option.[13] Early delivery is recommended in pregnant patients with impetigo herpetiformis.
Recent reports indicate the successful use of IL-1 receptor antagonists (e.g., anakinra) and IL-36 receptor antagonists in treating pustular psoriasis.[8] Tocilizumab, a monoclonal antibody against the IL-6 receptor, has also shown efficacy in some recalcitrant cases of pustular psoriasis.[14] (A1)
Differential Diagnosis
- Acute generalized exanthematous pustulosis
- Drug eruption reaction
- Pemphigus vulgaris
- Pemphigus foliaceous
- Impetigo
- Dermatitis Herpetiformis
- Infected eczema
- Erythroderma
- Acute cutaneous lupus
- Dyshidrotic eczema
- Disseminated herpes simplex virus
Prognosis
Pustular psoriasis is a chronic disease marked by recurrent episodes or flares. Treatment is aimed to shorten the duration of relapse, prevent complications, and extend disease-free periods. Compared to other subtypes, the von Zumbusch subtype of pustular psoriasis has a higher risk of mortality because of systemic involvement, especially with underlying comorbidities, such as cancer, renal failure, or liver failure. The localized subtypes of pustular psoriasis have a much lower risk of mortality.
Complications
- Hypocalcemia
- Septicemia, especially in the generalized form
- Hyperthermia
- Liver damage
- Acute renal failure
- Malnutrition
Deterrence and Patient Education
Patients with psoriasis should be educated to avoid abrupt steroid withdrawal, which can trigger episodes of pustular psoriasis. Flaccid lesions should be treated with proper wound care to avoid complications and secondary infections.
Enhancing Healthcare Team Outcomes
Management of pustular psoriasis requires an interprofessional team approach, including providers from primary care, dermatology, and infectious disease. A detailed history and complete physical examination are critical in diagnosing cases of pustular psoriasis. A dermatologist can help in the initial diagnostic workup and to assess for complications. Depending on the surface area involved, admission to the hospital may be required (e.g., von Zumbusch subtype). In equivocal cases, a biopsy can be performed, as the differential diagnosis for pustulosis is rather vast. Treatment is targeted to prevent relapses and shorten the duration of flares.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Tsuchida Y, Hayashi R, Ansai O, Nakajima M, Oginezawa M, Kawai T, Yokoyama R, Deguchi T, Hama N, Shinkuma S, Abe R. Generalized pustular psoriasis complicated with bullous pemphigoid. International journal of dermatology. 2019 Mar:58(3):e66-e67. doi: 10.1111/ijd.14332. Epub 2018 Dec 5 [PubMed PMID: 30516289]
Negrotto L, Correale J. Palmar pustular psoriasis associated with teriflunomide treatment. Multiple sclerosis and related disorders. 2019 Jan:27():400-402. doi: 10.1016/j.msard.2018.11.020. Epub 2018 Nov 19 [PubMed PMID: 30513502]
Epple A, Paffhausen JE, Fink C, Enk A, Sedlaczek O, Haenssle HA. Chronic recurrent multifocal osteomyelitis with psoriatic skin manifestations in a 12-year-old female. Dermatology practical & conceptual. 2018 Oct:8(4):297-298. doi: 10.5826/dpc.0804a09. Epub 2018 Oct 31 [PubMed PMID: 30479859]
Madanagobalane S, Secukinumab in Generalized Pustular Psoriasis. Indian dermatology online journal. 2018 Nov-Dec [PubMed PMID: 30505796]
Boehner A, Navarini AA, Eyerich K. Generalized pustular psoriasis - a model disease for specific targeted immunotherapy, systematic review. Experimental dermatology. 2018 Oct:27(10):1067-1077. doi: 10.1111/exd.13699. Epub 2018 Jul 20 [PubMed PMID: 29852521]
Level 1 (high-level) evidenceKomatsuda S, Kamata M, Chijiwa C, Namiki K, Fukaya S, Hayashi K, Fukuyasu A, Tanaka T, Ishikawa T, Ohnishi T, Abe K, Yamamoto T, Aozasa N, Sugiura K, Tada Y. Gastrointestinal bleeding with severe mucosal involvement in a patient with generalized pustular psoriasis without IL36RN mutation. The Journal of dermatology. 2019 Jan:46(1):73-75. doi: 10.1111/1346-8138.14711. Epub 2018 Nov 26 [PubMed PMID: 30474867]
Zhang Z, Xu JH. Investigation of Psoriasis Susceptibility Loci in Psoriatic Arthritis and a Generalized Pustular Psoriasis Cohort. The journal of investigative dermatology. Symposium proceedings. 2018 Dec:19(2):S83-S85. doi: 10.1016/j.jisp.2018.09.008. Epub [PubMed PMID: 30471759]
Bachelez H, Choon SE, Marrakchi S, Burden AD, Tsai TF, Morita A, Turki H, Hall DB, Shear M, Baum P, Padula SJ, Thoma C. Inhibition of the Interleukin-36 Pathway for the Treatment of Generalized Pustular Psoriasis. The New England journal of medicine. 2019 Mar 7:380(10):981-983. doi: 10.1056/NEJMc1811317. Epub [PubMed PMID: 30855749]
Gabeff R, Safar R, Leducq S, Maruani A, Sarrabay G, Touitou I, Samimi M. Successful therapy with secukinumab in a patient with generalized pustular psoriasis carrying homozygous IL36RN p.His32Arg mutation. International journal of dermatology. 2019 Jan:58(1):e16-e17. doi: 10.1111/ijd.14293. Epub 2018 Nov 14 [PubMed PMID: 30430544]
Su Z, Paulsboe S, Wetter J, Salte K, Kannan A, Mathew S, Horowitz A, Gerstein C, Namovic M, Todorović V, Seagal J, Edelmayer RM, Viner M, Rinaldi L, Zhou L, Leys L, Huang S, Wang L, Sadhukhan R, Honore P, McGaraughty S, Scott VE. IL-36 receptor antagonistic antibodies inhibit inflammatory responses in preclinical models of psoriasiform dermatitis. Experimental dermatology. 2019 Feb:28(2):113-120. doi: 10.1111/exd.13841. Epub 2018 Dec 21 [PubMed PMID: 30417427]
Meier-Schiesser B, Feldmeyer L, Jankovic D, Mellett M, Satoh TK, Yerly D, Navarini A, Abe R, Yawalkar N, Chung WH, French LE, Contassot E. Culprit Drugs Induce Specific IL-36 Overexpression in Acute Generalized Exanthematous Pustulosis. The Journal of investigative dermatology. 2019 Apr:139(4):848-858. doi: 10.1016/j.jid.2018.10.023. Epub 2018 Nov 2 [PubMed PMID: 30395846]
Li ZT, Wang S. [Genetic Polymorphism of IL36RN in Han Patients with Generalized Pustular Psoriasis Alone in Sichuan Region]. Sichuan da xue xue bao. Yi xue ban = Journal of Sichuan University. Medical science edition. 2018 Jul:49(4):582-586 [PubMed PMID: 30378314]
Okubo Y, Mabuchi T, Iwatsuki K, Elmaraghy H, Torisu-Itakura H, Morisaki Y, Nakajo K. Long-term efficacy and safety of ixekizumab in Japanese patients with erythrodermic or generalized pustular psoriasis: subgroup analyses of an open-label, phase 3 study (UNCOVER-J). Journal of the European Academy of Dermatology and Venereology : JEADV. 2019 Feb:33(2):325-332. doi: 10.1111/jdv.15287. Epub 2018 Nov 15 [PubMed PMID: 30317671]
Cro S, Smith C, Wilson R, Cornelius V. Treatment of pustular psoriasis with anakinra: a statistical analysis plan for stage 1 of an adaptive two-staged randomised placebo-controlled trial. Trials. 2018 Oct 3:19(1):534. doi: 10.1186/s13063-018-2914-y. Epub 2018 Oct 3 [PubMed PMID: 30285894]
Level 1 (high-level) evidence