 Anatomy, Shoulder and Upper Limb, Axillary Artery
Anatomy, Shoulder and Upper Limb, Axillary Artery
Introduction
The axillary artery is the principal arterial supply of the upper limb, commencing as a continuation of the subclavian artery as it emerges from underneath the 1st rib to enter the axilla (see Image. Branches of the Aorta). This blood vessel provides key landmarks for understanding the position of other important structures in the region, particularly the brachial plexus. The axillary artery gives off 6 branches before terminating at the lower border of the teres major by becoming the brachial artery (see Image. Axillary Artery).
Pathological conditions that may affect the axillary artery include aneurysms, thrombosis, embolism, arteritis, pseudoaneurysms, and thoracic outlet syndrome. This blood vessel is also critical in trauma management, as traumatic disruptions can cause severe bleeding or ischemia in the upper limb. This artery and its branches serve as vital landmarks during surgical procedures, including bypass grafting, shoulder operations, and axillary lymph node dissections, where avoiding arterial damage is essential. Familiarity with the axillary artery's anatomy and function is necessary to minimize morbidity from conditions affecting the upper limb and ensure successful interventions.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The axillary artery commences from the subclavian artery at the outer border of the 1st rib, terminating as it becomes the brachial artery at the outer border of the teres major. The axillary artery is enclosed in the axillary sheath, a continuation of the prevertebral fascia of the neck, and is anatomically divided into 3 parts by the pectoralis minor muscle, providing a useful way to conceptualize its course. The 1st part is located proximal to the pectoralis minor and has 1 branch. The 2nd part lies deep to the pectoralis minor and has 2 branches. The 3rd part runs distally from the pectoralis minor and has 3 branches.[1] The axillary vein runs medially to the artery along its whole course.
A study of 59 cadavers found the average length of the axillary artery to be 11.22 cm, with each section occurring at roughly equal intervals along its course.[2] The surface marking of the axillary artery in the upper limb can be traced by drawing a line from the midclavicular point to the groove behind the coracobrachialis.
The 1st part of the axillary artery is the segment extending from its origin at the lateral border of the 1st rib to its termination point proximal to the pectoralis minor. This segment lies on top of the serratus anterior muscle and has 1 branch, the superior thoracic artery, which supplies the pectoralis minor and major muscles.[3]
The 2nd part of the axillary artery lies deep to the pectoralis minor. The 1st branch of this segment is the thoracoacromial trunk, which pierces the clavipectoral fascia and divides into 4 terminal branches: the acromial, pectoral, clavicular, and deltoid arteries. The 2nd branch of the 2nd part of the axillary artery is the lateral thoracic artery, which follows the lower border of the pectoralis minor and provides blood to the pectoralis, serratus anterior, and the mammary gland.[4]
The 3rd part of the axillary artery lies distal to the lower border of the pectoralis minor, anterior to the subscapularis and teres major.[5] This segment has 3 branches that can vary in order of bifurcation, namely, the subscapular trunk and the anterior and posterior humeral circumflex arteries. The subscapular trunk is typically the largest branch of the axillary artery, running down the posterior wall of the axilla.[6] This blood vessel gives rise to the scapular circumflex and thoracodorsal arteries. The scapular circumflex artery runs through the triangular space and provides blood to the scapular region. This blood vessel eventually anastomoses with the suprascapular artery, thus connecting and providing a collateral route between the 1st and 3rd parts of the axillary artery. The thoracodorsal artery supplies the latissimus dorsi.
The 2 remaining branches of the 3rd part of the axillary artery, the anterior and posterior humeral circumflex arteries, supply the head of the humerus and shoulder joint. These arteries anastomose with one another. The anterior humeral circumflex is smaller and runs anterior to the humerus. The posterior humeral circumflex is larger and runs through the quadrilateral space and then posterior to the humerus, accompanied by the axillary nerve and supplying the deltoid muscle.[7]
The axillary artery terminates at the lower border of the teres major muscle. At this point, the axillary artery becomes the brachial artery, which supplies the distal upper limb.
Embryology
The embryological development of the arterial system of the upper limb is highly complex, beginning between days 29 and 31, with the formation of a capillary plexus from the dorsal aorta (Carnegie stage 12). During Carnegie stage 13, this plexus expands with the developing limb and selectively enlarges to form the greater and lesser components of the vasculature. The subclavian and axillary arterial vasculature generally has formed from the capillary plexus by Carnegie stage 15.[8]
Nerves
The brachial plexus is intimately related to the vascular structures of the axilla, as its divisions emerge deep to the clavicle to form the medial, lateral, and posterior cords around the axillary artery (see Image. Brachial Plexus Ultrasound and Schematic Diagram).[9] The lateral and posterior cords lie superolateral to the 1st part of the axillary artery, while the medial cord is posterior to this arterial segment.[10] Furthermore, a loop from the medial cord and lateral cord, which joins the medial and lateral pectoral nerves, is situated anteriorly. The 2nd part of the artery is related to the medial, lateral, and posterior cords, as indicated by their names. In general, the subsequent branches from each cord retain this relation to the 3rd part of the axillary artery.[11][12]
Physiologic Variants
Upper limb arterial variants have been observed in around 25% of the general population.[13] Specific to the axillary artery, 5% to 10% of people have been reported to have a bifid axillary artery that bifurcates in the axilla, with each branch becoming the radial and ulnar arteries.[14] A physiologic variation in the axillary artery branching system is also well-recognized. The pattern typically possesses a common origin for the lateral thoracic and subscapular arteries, anterior and posterior circumflex humeral arteries, or thoracoacromial and lateral thoracic arteries.
Surgical Considerations
The axillary artery may be accessed surgically by an infraclavicular or deltopectoral incision in the upper arm. The pectoralis major and minor must be mobilized to expose the neurovascular bundle, of which the axillary artery is a part. Careful protection of the brachial plexus cords, to which the artery is closely associated, is essential. Depending on the specific pathology, eg, aneurysm, blunt trauma, and gunshot trauma, injury to the axillary artery may be repaired with autologous venous grafting or synthetic grafting with, for example, polytetrafluoroethylene.[15][16]
Clamping the axillary artery may be accomplished without harming the arm. Surgical procedures concerning the axillary artery require delicacy due to the proximity of the brachial plexus. In cardiac surgery, the right axillary artery is frequently used as an arterial cannulation site, especially in the repair of aortic aneurysm or dissection.[17][18][19]
Clinical Significance
Traumatic Shoulder Injuries Affecting the Axillary Artery
Axillary artery injuries are rare but may cause limb loss. Damage most commonly arises from penetrating or blunt trauma to the shoulder. Examples include but are not limited to anterior shoulder dislocation, reduction of anterior shoulder dislocation, and humoral neck fracture.[20][21] These injury mechanisms may cause axillary artery rupture and subsequent thrombosis. Patients may present with pain, pallor, coldness, absent or delayed capillary refill, numbness or tingling, or lack of radial pulses to the injured limb. However, the redundancy of the shoulder's blood supply from collateral vessels may mask some of these symptoms. Consequently, axillary artery injuries present variably, making a high level of suspicion essential.
Axillary Artery Aneurysm
Axillary artery aneurysms may result from penetrating or blunt trauma, although development from atherosclerotic processes over long periods is exceedingly rare.[22][23] These aneurysms are often associated with neurological complications due to the proximity of the axillary artery to the brachial plexus. Improper use of crutches may also lead to aneurysms. Patients may present with upper limb neurological deficits, ischemic fingers, or occlusion of the radial and ulnar arteries caused by embolization from an aneurysm. Imaging confirms axillary aneurysms, with computed tomography angiography being the most effective and currently the gold standard. Magnetic resonance angiography serves as an alternative when intravenous contrast is contraindicated. Ultrasound is another highly effective modality for detecting and diagnosing axillary artery aneurysms.
The common surgical procedure to address axillary artery aneurysms is aneurysmectomy, followed by grafting with a saphenous vein. An alternative treatment option is endovascular aneurysm repair.[24]
Arterial Positional Compression
Axillary artery thrombosis and aneurysm, though rare, can occur in healthy athletes who frequently perform overhead throwing motions, such as pitching a baseball or hitting a volleyball. During the throwing motion, anterior displacement of the humerus compresses the 3rd portion of the axillary artery. This intermittent compression can lead to chronic changes in downstream vascular sufficiency, potentially resulting in thrombosis and aneurysms. Medical staff working with these athletes should remain alert for symptoms of ischemic pain, cold intolerance, numbness, or arm fatigue immediately after practice or competition. Symptoms often appear later in the disease process, as perceptible changes in temperature or sensation typically occur only with significant embolization or reduced blood flow.
Computed tomography angiography and magnetic resonance angiography may be used to diagnose or screen athletes at risk of symptomatic arterial positional compression, as in cases of quadrilateral space compression syndrome. The quadrilateral space is bordered by the humerus, teres major, long head of triceps, and teres minor and contains the posterior circumflex humeral artery and axillary nerve, which are vulnerable to compression.[25]
Media
(Click Image to Enlarge)

Branches of the Aorta. This illustration includes the right common carotid artery, right vertebral artery, right subclavian artery, brachiocephalic artery, ascending aorta, left coronary artery, right coronary artery, left common carotid artery, left vertebral artery, left subclavian artery, left axillary artery, left brachial artery, arch of aorta, and descending aorta.
Contributed by Beckie Palmer
(Click Image to Enlarge)
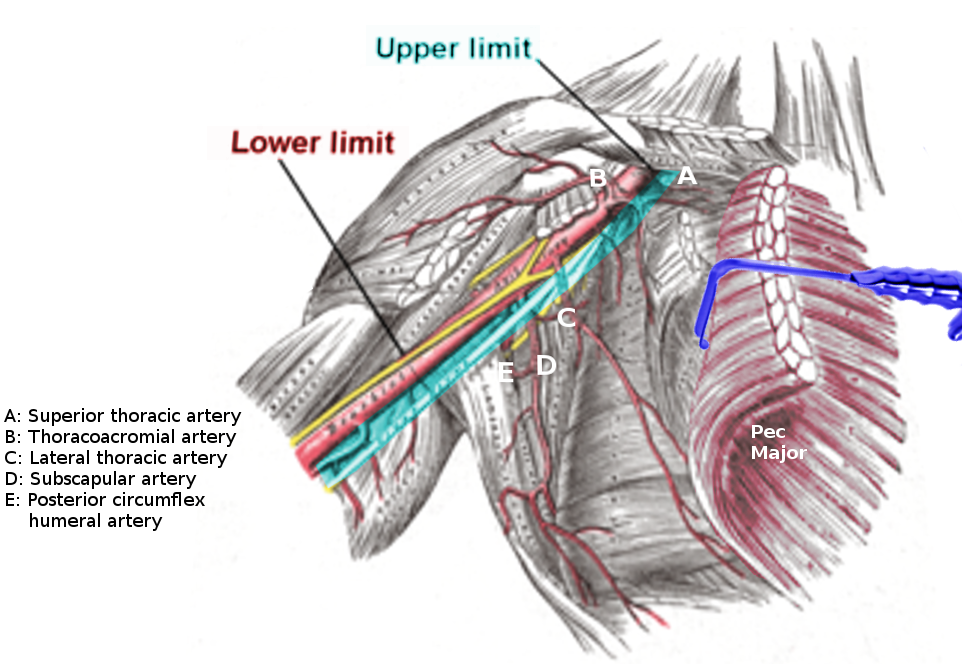
Axillary Artery. This illustration shows the anatomic relations and the general course of the axillary artery. Labeled branches include the (A) superior thoracic artery; (B) thoracoacromial artery; (C) lateral thoracic artery; (D) subscapular artery; and (E) posterior circumflex humeral artery.
Image courtesy S Bhimji MD
(Click Image to Enlarge)
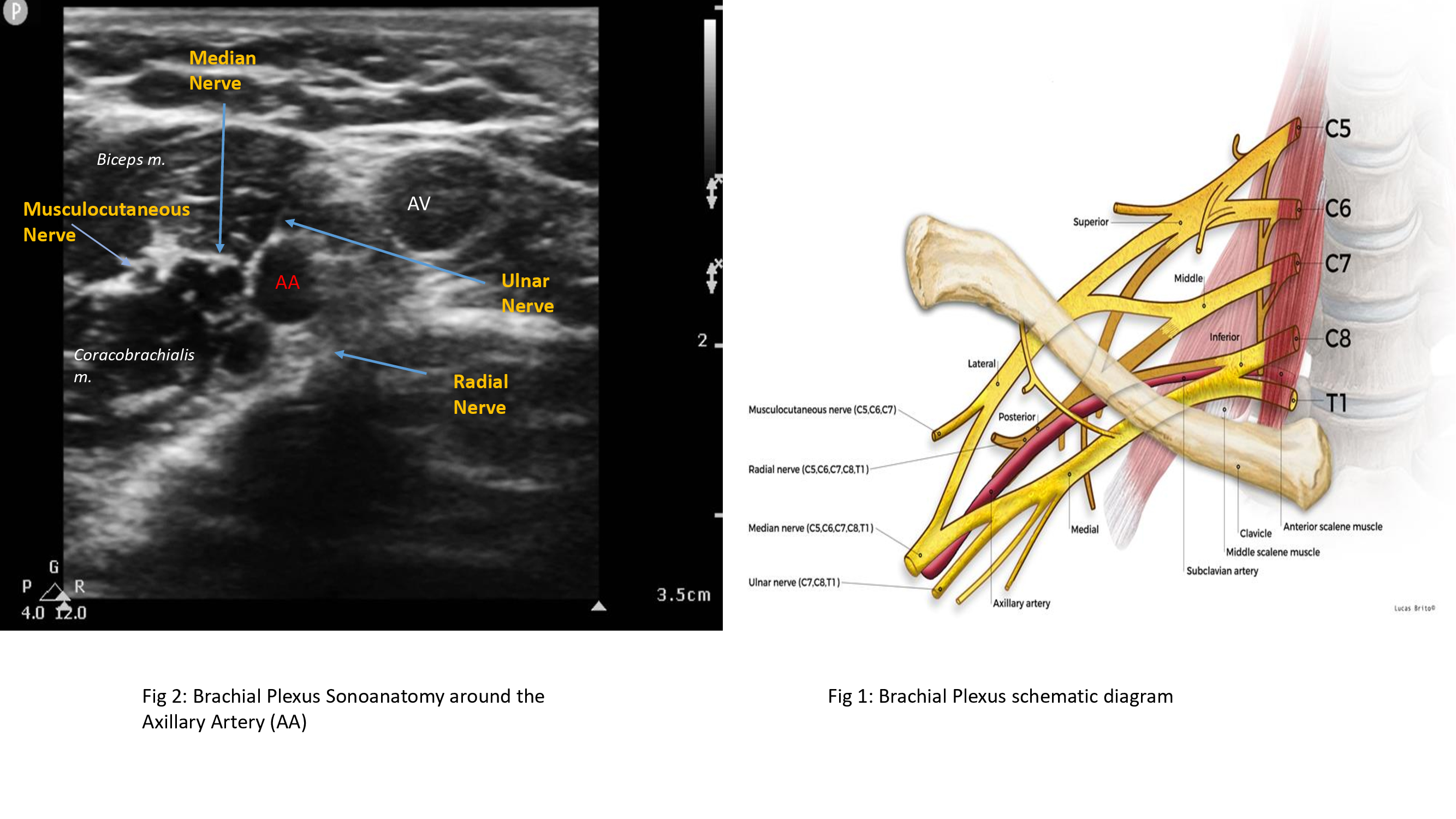
Brachial Plexus Ultrasound and Schematic Diagram. The left image shows an ultrasonographic view of the brachial plexus, while the right image shows the nerve plexus' schematic diagram and anatomic relationships. Labeled structures in the ultrasound image include the median, musculocutaneous, radial, and ulnar nerves; the axillary artery and vein; and the biceps and coracobrachialis muscles. Labeled structures in the schematic diagram include the vertebrae C5 to T1; the superior, middle, and inferior trunks of the plexus; the lateral, posterior, and medial cords of the plexus; the musculocutaneous, radial, median, ulnar, and axillary nerves; the clavicle; the subclavian artery; and the anterior and middle scalene muscles.
Contributed and Created by Muhammad Salman Janjua, with Permission from Lucas Brio
References
Shi D, Bai J, Zhang L, Wang X. The "Hand as Foot" teaching method in axillary artery anatomy. Asian journal of surgery. 2022 Feb:45(2):800-801. doi: 10.1016/j.asjsur.2021.12.001. Epub 2021 Dec 29 [PubMed PMID: 34973859]
Yang K, Lee H, Choi IJ, Jeong W, Kim HT, Wei Q, Lee JH. Topography and Anatomical Variations of the Axillary Artery. BioMed research international. 2021:2021():6393780. doi: 10.1155/2021/6393780. Epub 2021 May 24 [PubMed PMID: 34124252]
Stowell JT, McComb BL, Mendoza DP, Cahalane AM, Chaturvedi A. Axillary Anatomy and Pathology: Pearls and "Pitfalls" for Thoracic Imagers. Journal of thoracic imaging. 2022 May 1:37(3):W28-W40. doi: 10.1097/RTI.0000000000000639. Epub 2022 Feb 10 [PubMed PMID: 35142752]
Loukas M, du Plessis M, Owens DG, Kinsella CR Jr, Litchfield CR, Nacar A, Lu O, Tubbs RS. The lateral thoracic artery revisited. Surgical and radiologic anatomy : SRA. 2014 Aug:36(6):543-9. doi: 10.1007/s00276-013-1234-x. Epub 2013 Nov 27 [PubMed PMID: 24281130]
Jaiswal LS, Neupane D, Yadav P. Rare variation of the right brachial artery. ANZ journal of surgery. 2022 May:92(5):1281-1282. doi: 10.1111/ans.17291. Epub 2021 Oct 17 [PubMed PMID: 34661957]
Mills NL, Dupin CL, Everson CT, Leger CL. The subscapular artery: an alternative conduit for coronary bypass. Journal of cardiac surgery. 1993 Jan:8(1):66-71 [PubMed PMID: 8422491]
Level 3 (low-level) evidenceOlinger A, Benninger B. Branching patterns of the lateral thoracic, subscapular, and posterior circumflex humeral arteries and their relationship to the posterior cord of the brachial plexus. Clinical anatomy (New York, N.Y.). 2010 May:23(4):407-12. doi: 10.1002/ca.20958. Epub [PubMed PMID: 20235185]
Rodríguez-Niedenführ M, Burton GJ, Deu J, Sañudo JR. Development of the arterial pattern in the upper limb of staged human embryos: normal development and anatomic variations. Journal of anatomy. 2001 Oct:199(Pt 4):407-17 [PubMed PMID: 11693301]
Benes M, Kachlik D, Belbl M, Kunc V, Havlikova S, Whitley A, Kunc V. A meta-analysis on the anatomical variability of the brachial plexus: Part I - Roots, trunks, divisions and cords. Annals of anatomy = Anatomischer Anzeiger : official organ of the Anatomische Gesellschaft. 2021 Nov:238():151751. doi: 10.1016/j.aanat.2021.151751. Epub 2021 Apr 30 [PubMed PMID: 33940116]
Level 1 (high-level) evidenceFakoya AOJ, Aguinaldo E, Velasco-Nieves NM, Vandeveer ZT, Morales-Marietti N, Mathew S, Afolabi AG, McCracken T. Unusual Splitting of Medial Cord of the Right Brachial Plexus and Its Relation to the Axillary Artery and Subscapular Artery: A Case Report. Open access Macedonian journal of medical sciences. 2019 Jun 30:7(12):2006-2009. doi: 10.3889/oamjms.2019.561. Epub 2019 Jun 30 [PubMed PMID: 31406546]
Level 3 (low-level) evidenceLeinberry CF, Wehbé MA. Brachial plexus anatomy. Hand clinics. 2004 Feb:20(1):1-5 [PubMed PMID: 15005376]
Gili S, Abreo A, GóMez-Fernández M, Solà R, Morros C, Sala-Blanch X. Patterns of Distribution of the Nerves Around the Axillary Artery Evaluated by Ultrasound and Assessed by Nerve Stimulation During Axillary Block. Clinical anatomy (New York, N.Y.). 2019 Jan:32(1):2-8. doi: 10.1002/ca.23225. Epub 2018 Oct 20 [PubMed PMID: 30341965]
Burzotta F, Brancati MF, Porto I, Saffioti S, Aurigemma C, Niccoli G, Leone AM, Coluccia V, Crea F, Trani C. Comparison of Right and Left Upper Limb Arterial Variants in Patients Undergoing Bilateral Transradial Procedures. Circulation. Cardiovascular interventions. 2015 Dec:8(12):e002863. doi: 10.1161/CIRCINTERVENTIONS.115.002863. Epub [PubMed PMID: 26643739]
Bigeleisen PE. The bifid axillary artery. Journal of clinical anesthesia. 2004 May:16(3):224-5 [PubMed PMID: 15217666]
Rogovskyi VM, Gybalo RV, Lurin IA, Sivash YY, Oklei DV, Taraban IA. A Case of Surgical Treatment of a Gunshot Wound to the Left Scapular Region With Damage to the Distal Axillary and Proximal Brachial Arteries. World journal of surgery. 2022 Jul:46(7):1625-1628. doi: 10.1007/s00268-022-06577-y. Epub 2022 Apr 28 [PubMed PMID: 35484404]
Level 3 (low-level) evidenceTetik O, Yilik L, Besir Y, Can A, Ozbek C, Akcay A, Gurbuz A. Surgical treatment of axillary artery aneurysm. Texas Heart Institute journal. 2005:32(2):186-8; discussion 185 [PubMed PMID: 16107110]
Level 2 (mid-level) evidenceBertoglio L, Grandi A, Melloni A, Kahlberg A, Melissano G, Chiesa R. Percutaneous AXillary Artery (PAXA) Access at the First Segment During Fenestrated and Branched Endovascular Aortic Procedures. European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery. 2020 Jun:59(6):929-938. doi: 10.1016/j.ejvs.2020.01.027. Epub 2020 Feb 20 [PubMed PMID: 32089506]
Branzan D, Steiner S, Haensig M, Scheinert D, Schmidt A. Percutaneous Axillary Artery Access for Endovascular Treatment of Complex Thoraco-abdominal Aortic Aneurysms. European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery. 2019 Sep:58(3):344-349. doi: 10.1016/j.ejvs.2019.01.011. Epub 2019 Jul 30 [PubMed PMID: 31375342]
Agrusa CJ, Connolly PH, Ellozy SH, Schneider DB. Safety and Effectiveness of Percutaneous Axillary Artery Access for Complex Aortic Interventions. Annals of vascular surgery. 2019 Nov:61():326-333. doi: 10.1016/j.avsg.2019.05.046. Epub 2019 Aug 5 [PubMed PMID: 31394224]
Stone MA, Ihn HE, Gipsman AM, Iglesias B, Minneti M, Noorzad AS, Omid R. Surgical anatomy of the axillary artery: clinical implications for open shoulder surgery. Journal of shoulder and elbow surgery. 2021 Jun:30(6):1266-1272. doi: 10.1016/j.jse.2020.09.018. Epub 2020 Oct 15 [PubMed PMID: 33069906]
Bucci G, Lucar-López G, Sanchez-Gonzalez J, Malagelada F, Palencia Lopez J, Guevara-Noriega KA. Axillary artery injury and brachial plexus palsy as a complication of proximal humerus fractures. Journal of orthopaedics. 2017 Sep:14(3):340-341. doi: 10.1016/j.jor.2017.06.001. Epub 2017 Jun 24 [PubMed PMID: 28706376]
Michalakis D, Lerais JM, Goffette P, Royer V, Brenot R, Kastler B. [True isolated atherosclerotic aneurysm of the axillary artery]. Journal de radiologie. 2003 Sep:84(9):1016-9 [PubMed PMID: 13679756]
Level 3 (low-level) evidenceSzuchmacher PH, Freed JS. Axillary aneurysms. New York state journal of medicine. 1980 Apr:80(5):795-6 [PubMed PMID: 6930558]
Level 3 (low-level) evidenceBranco BC, Boutrous ML, DuBose JJ, Leake SS, Charlton-Ouw K, Rhee P, Mills JL Sr, Azizzadeh A. Outcome comparison between open and endovascular management of axillosubclavian arterial injuries. Journal of vascular surgery. 2016 Mar:63(3):702-9. doi: 10.1016/j.jvs.2015.08.117. Epub 2015 Oct 23 [PubMed PMID: 26506937]
Charmode S, Mehra S, Kushwaha S. Revisiting the Surgical Approaches to Decompression in Quadrilateral Space Syndrome: A Cadaveric Study. Cureus. 2022 Feb:14(2):e22619. doi: 10.7759/cureus.22619. Epub 2022 Feb 26 [PubMed PMID: 35371758]