Subjective Refraction Technique: Stenopeic Slit
Subjective Refraction Technique: Stenopeic Slit
Introduction
The prevalence of refractive errors, such as astigmatism, myopia, and hyperopia, has been reported in numerous studies conducted worldwide.[1][2] Astigmatism is the most common refractive error in certain countries; the prevalence can approach 50%. As with myopia, the development of astigmatism is influenced by genetic and ethnic factors.[3][4] The astigmatic axis and power are important parameters of this refractive error. In most cases, the amount of astigmatism determines its clinical impact; in some cases, the orientation of astigmatism has a greater effect.[5] Untreated astigmatism may result in loss of visual acuity and amblyopia.[6] Patients with astigmatism can present with monocular diplopia, asthenopia, ocular discomfort, blurred and defective vision, metamorphopsia, and accommodation problems.
The stenopeic slit accurately determines the orientation and power of an astigmatic refractive error. Compared to other techniques, the stenopeic slit performs best when the amount of astigmatism is relatively large but not too large and vision is relatively poor. Other techniques employed to determine the amount and orientation of astigmatism include keratometry, corneal topography, aberrometry, autorefractor measurements, retinoscopy, the Jackson cross cylinder method, and astigmatic dial methods that include the fan-and-block method, and the astigmatic dial technique, the cross dial technique, and others.[7][8][9]
Since many of these methods require more extensive equipment, the stenopeic slit may be the preferred method of assessing astigmatism in settings with limited resources. The stenopeic slit technique requires only an acuity chart, trial frame, and trial lenses, with minor variations.[10]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Astigmatism is a type of refractive error that occurs when parallel rays of light entering the eye are not well-focused on the retina.[11] Light rays propagate in two different planes in an astigmatic eye; the incident light rays fail to converge at a single focal point and instead have two separate foci.[12] The retinal images of distant and near objects appear blurred due to differences in the degree of refraction in different meridians; the distance between the foci is the conoid of Sturm.[13] Astigmatism may be simple, compound, or mixed and regular or irregular. The stenopeic slit method can be used to determine regular and irregular astigmatism.[8] Astigmatism may be described by the location of the foci, the underlying etiology, or the location with the steepest meridian.
When describing astigmatism by the location of the foci, simple myopic astigmatism occurs when one focus is in front of the retina and the other is on the retina. In compound myopic astigmatism, both foci are in front of the retina but at different locations.[14] Simple hyperopic astigmatism is characterized by one focus behind the retina at a virtual location and the other on the retina.[15] Compound hyperopic astigmatism occurs when both foci are at different locations behind the retina.[14] Mixed astigmatism results when the refractive media creates two foci. One focus is positioned in front of the retina, and the other is behind the retina.[16] Irregular astigmatism results from the refractive media creating principle meridia not perpendicular to each other.[17][18]
When describing astigmatism by its underlying etiology, corneal astigmatism is caused by irregularities in the anterior or posterior corneal curvature, as seen with keratoconus, corneal scarring, or a limbal dermoid.[19] Lenticular astigmatism is due to variations in the crystalline lens, such as curvature, position, or refractive index, as with lenticonus, subluxation, or nuclear sclerosis, respectively.[20] Retinal astigmatism is due to an oblique macular placement.[21]
Astigmatism may also be with-the-rule (WTR) or against-the-rule (ATR) based on the location of the steepest meridian. In WTR astigmatism, the vertical meridian is the steepest and has the most convergent focusing power. This vertical meridian will create a horizontal focal line closer to the source of light and the front of the eye than the focal line created by the horizontal meridian. Contrarily, in ATR astigmatism, the horizontal meridian is the steepest and has the most convergent focusing power. This horizontal meridian will create a vertical focal line closer to the source of light and the front of the eye than the focal line created by the vertical meridian.[22]
Indications
The stenopeic slit is an important accessory to detect and refine the amount and orientation of astigmatism. The stenopeic slit is often used when other assessment methods requiring extensive equipment are unavailable. The stenopeic slit technique detects higher amounts of astigmatism and irregular astigmatism that can occur in cases of keratoconus, corneal scarring, postsurgical irregularities, or severe dry eye. When irregular astigmatism is present, the principal meridians are not at a 90-degree angle. The stenopeic slit can isolate the two principal meridians when obliquely oriented.
A stenopeic slit is also used in cases of corneal opacities to find the optimal site for optical iridectomy.[23] After mydriatic-induced pupillary dilation, the stenopeic slit is rotated in front of the eye; the axis which gives maximum clarity is chosen for optical iridectomy.
Vertex distance can also be assessed with the help of a stenopeic slit.
Contraindications
Since the refinement of the axis and power with a stenopeic slit is a subjective assessment method, the patient must be able to understand and follow the instructions. A patient unable to effectively engage with the clinician due to cognitive deficit or other barriers is not a good candidate for this assessment technique. The patient must also tolerate the positioning and wearing of a trial frame.
The stenopeic slit technique is complicated by high amounts of astigmatism that have resulted in meridional amblyopia, habitual squinting, and patients who have developed a habit of "blur-interpretation."
Finally, the best-corrected visual acuity has to be adequate to recognize changes in image clarity provided during the test.
Equipment
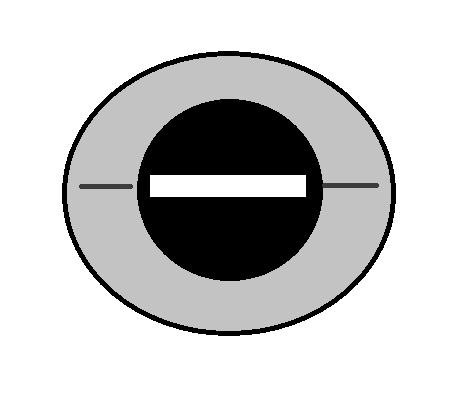
A stenopeic slit is a slit-shaped, elongated, pinhole-like aperture positioned in the center of a disc. The disc is the same size as a trial lens and can be placed in a trial frame. The slit is less than 1 mm wide and approximately 15 mm long. The stenopeic slit device is usually included in a trial lens case as one of the accessories used to determine astigmatism, along with hand-held Jackson cross cylinder lenses.[24]
The stenopeic slit reduces the effective pupil size in the meridian perpendicular to it, producing an axial shift of the circle of least confusion (CLC) and, consequently, a change of the retinal blur size that depends on the orientation of the slit. The stenopeic slit removes the peripheral rays in the meridian perpendicular to the slit, isolating the meridian at which refraction is to be performed.[10]
Personnel
The refinement of the astigmatism axis and power using a stenopeic slit can be performed by anyone who has received appropriate training; however, interpretation of the results is best conducted under the supervision of an optometrist or an ophthalmologist.
Preparation
The stenopeic slit technique should be performed in a dimly lit or dark room. The patient should be educated about the procedure. The patient is asked to view an acuity chart at a standard 6-meter or 20-foot distance. The trial frame should be cleaned thoroughly with an alcohol swab, and all lenses should be cleaned with the cloth provided in the trial set before placing them in the trial frame.
Technique or Treatment
After viewing a visual acuity chart, a trial frame is placed. The stenopeic slit technique is performed monocularly, and vision in the contralateral eye should be blocked with an occluder from the trial set placed in the trial frame.
Steps in the Determination of the Astigmatic Axis and Power
- Obtain the best spherical correction by placing spherical lenses over the eye. Begin with plus power lenses and introduce increasingly more minus (or less plus) power lenses.
- Place a +1.50 DS lens in the trial frame lens holder overtop of the best spherical correction lens. This step is called "fogging."
- Place the stenopeic slit in front of the lenses in the trial frame.
- Manually rotate the slit 360 degrees until the patient reports the clearest vision through the slit. This is the first principal meridian.
- Slowly reduce the power in 0.25 DS increments until the patient reports the best visual acuity.
- Rotate the slit by 90° and reduce the power in 0.25 DS increments until the patient reports the best visual acuity. This is the second principal meridian.
- Draw the two meridians in an optical cross format.
- The difference in power between the two meridians is the amount of astigmatism.
- For the minus cylinder format notation of the refractive error, the first principal meridian orientation is also the axis of the minus cylinder.
- For the plus cylinder format notation of the refractive error, the second principal meridian orientation is also the axis of the plus cylinder.
If reducing the power in steps 2 through 5 results in increasingly blurred vision, there are more than 3 diopters of astigmatism; the first principal meridian may actually have more plus power. In this case, the clearest image is obtained by increasing the plus power of the lenses in 0.25 DS increments as part of step 5. The test can then be continued as described in step 6.
The Thorington Method
The Thorington method is an alternate refraction technique using the stenopeic slit. When employing the Thorington method, fogging is performed with a +0.50 DS lens placed in the trial frame to move the posterior line of focus closer to the retina. A logMAR chart with multiple lines of letters at a 6-meter distance is used as the viewing target. The patient should be able to read at least 2 lines above the limit of visual acuity with the fogging lens in place. The stenopeic slit is initially positioned at 90°, and the patient is instructed to use the knob on the trial frame to keep rotating the slit until its position gives the clearest view.
The Thorington method is rarely employed in subjective refraction to find the axes of refractive error of an astigmatic eye because of the general perception that the Jackson cross cylinder (JCC) method provides greater accuracy. However, the JCC method can be tedious for patients with reduced vision, as patients can have difficulty detecting any changes between the views produced by two lenses of different axis or power. The Thorington method is very useful in cases of high astigmatism and poor visual acuity or where the retinoscopic reflex is difficult to visualize.
Determination of Vertex Distance
Place a trial frame to determine the vertex distance using the stenopeic slit and ask the patients to close their eyes. The slit device should be kept in the trial frame. Pass a thin ruler through the slit until the ruler touches the eyelid; note the measurement and add 1 mm to compensate for eyelid thickness. A stenopeic slit is also useful in cases of high astigmatism or low visual acuity.[25]
Complications
The stenopeic slit test is a noninvasive procedure with rare complications. Patients may develop conjunctivitis if the trial frame is not cleaned properly before use. Patients may provide incorrect answers during this subjective test resulting in an incorrect refractive correction.
Clinical Significance
Astigmatism causes deterioration of the retinal image and affects the quality of vision. Therefore, the diagnosis of astigmatism and its proper treatment are critical. This is especially true for children who can develop meridional amblyopia if the power of their astigmatism is significant. The optical defocus caused by astigmatism can cause asthenopia, monocular diplopia, and blur.
Different techniques to assess the axis of astigmatism include keratometry, corneal topography, aberrometry, autorefractor measurements, retinoscopy, the Jackson cross cylinder method, and astigmatic dial methods that include the fan-and-block method, the astigmatic dial technique, the cross dial technique, and others.[26][27][28]
Astigmatism can be managed with spectacles, contact lenses, or surgical correction through refractive surgery, toric intraocular lens implantation, and limbal relaxing incisions.[29]
As the orientation of the stenopeic slit changes, the retinal blur size in an astigmatic eye changes due to an axial shift of the circle of least confusion. When the stenopeic slit is aligned with one of the principal meridians of astigmatism, the spherocylindrical refractive error becomes purely spherical. This orientation produces the sharpest image because the refractive error is the lowest. Patients have different tolerance for visual blur; therefore, the decision on the astigmatic power prescription is dictated by their tolerance level. However, factors such as age and the need to prevent long-term complications may dictate the need to correct astigmatism.
A higher degree of astigmatism is noted in infants and neonates and is reported to be even higher in preterm newborns. An inverse correlation is noted between postconceptional age and birth weight. The occurrence of astigmatism in childhood naturally declines with the process of emmetropization. In almost all cases, significant astigmatism resolves spontaneously in the first year of life. This resolution occurs because of a physiological decrease in the toricity of the cornea and anterior lens surface, combined with reduced variability of corneal-lenticular surfaces.
However, higher degrees of infantile astigmatism are associated with increased astigmatism and myopia in school-aged children.[30] WTR astigmatism occurs most often, followed by ATR astigmatism; oblique astigmatism is much rarer.[31] These changes are usually attributed to alterations in the position and tension or tightness of the eyelid and extraocular muscles, biomechanical properties of the cornea, and genetic factors.[32] Numerous guidelines exist to help practitioners decide on the degree of astigmatism that needs to be corrected.
The visual system may not be very sensitive to the blur induced by astigmatism during the initial stages of life, but from then on, uncorrected astigmatic error, especially when oblique, can induce retinal blur during the early developmental phase leading to a condition called meridional amblyopia.
Factors such as the palpebral fissure slant can affect corneal toricity, which in turn induces astigmatism. Patients with Trisomy 21 and Treacher-Collins syndrome show oblique astigmatism due to an upward or downward slant of the palpebral fissure.[33] Reduced corneal rigidity can also increase astigmatism caused by eyelid pressure.[34] The pupil size also affects astigmatism. Larger pupil size is correlated with high cylindrical power and WTR astigmatism. A higher degree of astigmatism induces chromatic aberrations like coma, which becomes an important consideration before doing refractive surgeries.[35] Tear film changes also affect the cornea and can result in astigmatism.[36]
Management of Astigmatism
Nonsurgical management options for astigmatism are spectacles, toric soft contact lenses, and rigid gas permeable contact lenses (RGPCLs). RGPCL options for astigmatism include front-surface, back-surface, and bitoric lenses. In some cases, spherical RGPCLs are combined with spectacle correction. Surgical options for astigmatism include refractive surgery procedures, toric intraocular lens implants, and limbal relaxing incisions.[37][38][39]
Astigmatic Lens Types
Plano-cylindrical lenses contain one meridian that has no focusing power, the plano meridian, and the other meridian that focuses light, the cylindrical meridian. The plano meridian creates a focal line at infinity, while the cylindrical meridian creates a focal line at a finite distance. Therefore, in the case of the plano-cylindrical lens, one of the focal lines is at infinity, and because the circle of least confusion is halfway in between the two focal lines, its location is at infinity as well.[12]
Sphero-cylindrical lenses contain both meridians with focusing power, and both will create a focal line at a finite distance. The circle of least confusion is halfway between the two focal lines.
For both lenses, the focal line is perpendicular to the orientation of the meridian.
Enhancing Healthcare Team Outcomes
Astigmatism negatively affects vision quality. Correction of power and proper axis is imperative, especially in symptoms like eyestrain, squinting, dry eye, and headaches. Patients with these or similar complaints require a thorough ocular evaluation best performed by an eyecare professional such as an ophthalmologist or optometrist. Patients that can not be corrected to a visual acuity of 6/6 or 20/20 and have progressive or high astigmatism should be evaluated for corneal ectasia; corneal topography becomes essential in such cases. Similarly, when astigmatism is identified as the underlying cause of meridional amblyopia, referral to a practitioner that can manage amblyopia is indicated.
Headache, diplopia, and blurring of vision can also be associated with underlying neurological or medical disorders, so other healthcare professionals must consider an existing refractive error or squint before considering the patients for systemic evaluation and radiological tests.
Media
References
Rezvan F, Khabazkhoob M, Fotouhi A, Hashemi H, Ostadimoghaddam H, Heravian J, Azizi E, Khorasani AA, Yekta AA. Prevalence of refractive errors among school children in Northeastern Iran. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians (Optometrists). 2012 Jan:32(1):25-30. doi: 10.1111/j.1475-1313.2011.00879.x. Epub 2011 Oct 24 [PubMed PMID: 22023649]
Yekta A, Fotouhi A, Hashemi H, Dehghani C, Ostadimoghaddam H, Heravian J, Derakhshan A, Yekta R, Behnia M, Khabazkhoob M. Prevalence of refractive errors among schoolchildren in Shiraz, Iran. Clinical & experimental ophthalmology. 2010 Apr:38(3):242-8. doi: 10.1111/j.1442-9071.2010.02247.x. Epub [PubMed PMID: 20447119]
Sawada A, Tomidokoro A, Araie M, Iwase A, Yamamoto T, Tajimi Study Group. Refractive errors in an elderly Japanese population: the Tajimi study. Ophthalmology. 2008 Feb:115(2):363-370.e3. doi: 10.1016/j.ophtha.2007.03.075. Epub [PubMed PMID: 18243904]
Level 2 (mid-level) evidenceSaw SM, Gazzard G, Koh D, Farook M, Widjaja D, Lee J, Tan DT. Prevalence rates of refractive errors in Sumatra, Indonesia. Investigative ophthalmology & visual science. 2002 Oct:43(10):3174-80 [PubMed PMID: 12356821]
Fotouhi A, Hashemi H, Yekta AA, Mohammad K, Khoob MK. Characteristics of astigmatism in a population of schoolchildren, Dezful, Iran. Optometry and vision science : official publication of the American Academy of Optometry. 2011 Sep:88(9):1054-9. doi: 10.1097/OPX.0b013e318221727d. Epub [PubMed PMID: 21623251]
Level 2 (mid-level) evidenceBlair K, Cibis G, Gulani AC. Amblyopia. StatPearls. 2023 Jan:(): [PubMed PMID: 28613640]
Aluyi-Osa G, Musa MJ, Zeppieri M. Jackson Cross Cylinder. StatPearls. 2023 Jan:(): [PubMed PMID: 36508527]
Metzger M,Navel V,Barrière JV,Kwiatkowski F,Hébraud J,Mulliez A,Béral L,Chiambaretta F,Dutheil F, Benefits of using corneal topography to choose subjective refraction technique in keratoconus (RE-CON): a prospective comparative crossover clinical study. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2022 Jan; [PubMed PMID: 34415365]
Level 2 (mid-level) evidenceRao DP, Negiloni K, Gurunathan S, Velkumar S, Sivaraman A, Baig AU, B K, Murali K. Validation of a Simple-to-Use, Affordable, Portable Wavefront Aberrometry-Based Auto Refractometer in a Paediatric Population. Clinical ophthalmology (Auckland, N.Z.). 2022:16():4281-4291. doi: 10.2147/OPTH.S387831. Epub 2022 Dec 22 [PubMed PMID: 36578668]
Level 1 (high-level) evidenceMuñoz-Escrivá L, Furlan WD. Subjective refraction techniques in the frame of the three-dimensional dioptric space. Optometry and vision science : official publication of the American Academy of Optometry. 2001 Feb:78(2):106-12 [PubMed PMID: 11265925]
Wajuihian SO. Characteristics of astigmatism in Black South African high school children. African health sciences. 2017 Dec:17(4):1160-1171. doi: 10.4314/ahs.v17i4.25. Epub [PubMed PMID: 29937888]
Sutter E, Foster A, Francis V. Optics & refraction. Community eye health. 2000:13(33):8 [PubMed PMID: 17491945]
Parthasarathi P, Stokkermans TJ. The Conoid of Sturm. StatPearls. 2023 Jan:(): [PubMed PMID: 36508529]
Parrey MUR, Elmorsy E. Prevalence and pattern of refractive errors among Saudi adults. Pakistan journal of medical sciences. 2019 Mar-Apr:35(2):394-398. doi: 10.12669/pjms.35.2.648. Epub [PubMed PMID: 31086521]
Remón L, Tornel M, Furlan WD. Visual acuity in simple myopic astigmatism: influence of cylinder axis. Optometry and vision science : official publication of the American Academy of Optometry. 2006 May:83(5):311-5 [PubMed PMID: 16699444]
Xu G, Xu B, Zhou J. [A clinical report on mixed astigmatism]. [Zhonghua yan ke za zhi] Chinese journal of ophthalmology. 1996 Mar:32(2):126-9 [PubMed PMID: 9206230]
Santodomingo-Rubido J, Carracedo G, Suzaki A, Villa-Collar C, Vincent SJ, Wolffsohn JS. Keratoconus: An updated review. Contact lens & anterior eye : the journal of the British Contact Lens Association. 2022 Jun:45(3):101559. doi: 10.1016/j.clae.2021.101559. Epub 2022 Jan 4 [PubMed PMID: 34991971]
Koh S. Irregular Astigmatism and Higher-Order Aberrations in Eyes With Dry Eye Disease. Investigative ophthalmology & visual science. 2018 Nov 1:59(14):DES36-DES40. doi: 10.1167/iovs.17-23500. Epub [PubMed PMID: 30481804]
Mohammadi SF, Khorrami-Nejad M, Hamidirad M. Posterior corneal astigmatism: a review article. Clinical optometry. 2019:11():85-96. doi: 10.2147/OPTO.S210721. Epub 2019 Aug 12 [PubMed PMID: 31496856]
Bamotra RK, Meenakshi, Kesarwani PC, Qayum S. Simultaneous Bilateral Anterior and Posterior Lenticonus in Alport Syndrome. Journal of clinical and diagnostic research : JCDR. 2017 Aug:11(8):ND01-ND02. doi: 10.7860/JCDR/2017/25521.10369. Epub 2017 Aug 1 [PubMed PMID: 28969174]
Davitt BV, Dobson V, Quinn GE, Hardy RJ, Tung B, Good WV, Early Treatment for Retinopathy of Prematurity Cooperative Group. Astigmatism in the Early Treatment for Retinopathy Of Prematurity Study: findings to 3 years of age. Ophthalmology. 2009 Feb:116(2):332-9. doi: 10.1016/j.ophtha.2008.09.035. Epub 2008 Dec 16 [PubMed PMID: 19091409]
Level 1 (high-level) evidenceRefai TA. Evaluation of the orientation of the steepest meridian of regular astigmatism among highly myopic Egyptian patients seeking non-ablative surgical correction of the refractive error. Electronic physician. 2015 Sep:7(5):1296-300. doi: 10.14661/1296. Epub 2015 Sep 16 [PubMed PMID: 26435831]
Rajagopal RN, Fernandes M. Peters Anomaly: Novel Non-Invasive Alternatives to Penetrating Keratoplasty. Seminars in ophthalmology. 2023 Apr:38(3):275-282. doi: 10.1080/08820538.2023.2176238. Epub 2023 Feb 14 [PubMed PMID: 36788651]
María Revert A, Conversa MA, Albarrán Diego C, Micó V. An alternative clinical routine for subjective refraction based on power vectors with trial frames. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians (Optometrists). 2017 Jan:37(1):24-32. doi: 10.1111/opo.12343. Epub [PubMed PMID: 28030877]
Schiefer U, Kraus C, Baumbach P, Ungewiß J, Michels R. Refractive errors. Deutsches Arzteblatt international. 2016 Oct 14:113(41):693-702. doi: 10.3238/arztebl.2016.0693. Epub [PubMed PMID: 27839543]
Worthey JA. Simplified analysis of meridional refraction data. American journal of optometry and physiological optics. 1977 Nov:54(11):771-5 [PubMed PMID: 610437]
Musa MJ, Zeppieri M. Subjective Refraction Technique: Astigmatic Dial. StatPearls. 2023 Jan:(): [PubMed PMID: 36943999]
Dhungel D, Shrestha GS. Visual symptoms associated with refractive errors among Thangka artists of Kathmandu valley. BMC ophthalmology. 2017 Dec 21:17(1):258. doi: 10.1186/s12886-017-0659-0. Epub 2017 Dec 21 [PubMed PMID: 29268725]
Lake JC, Victor G, Clare G, Porfírio GJ, Kernohan A, Evans JR. Toric intraocular lens versus limbal relaxing incisions for corneal astigmatism after phacoemulsification. The Cochrane database of systematic reviews. 2019 Dec 17:12(12):CD012801. doi: 10.1002/14651858.CD012801.pub2. Epub 2019 Dec 17 [PubMed PMID: 31845757]
Level 1 (high-level) evidenceSemeraro F, Forbice E, Nascimbeni G, Cillino S, Bonfiglio VME, Filippelli ME, Bartollino S, Costagliola C. Ocular Refraction at Birth and Its Development During the First Year of Life in a Large Cohort of Babies in a Single Center in Northern Italy. Frontiers in pediatrics. 2019:7():539. doi: 10.3389/fped.2019.00539. Epub 2020 Jan 29 [PubMed PMID: 32083036]
Namba H, Sugano A, Murakami T, Utsunomiya H, Nishitsuka K, Ishizawa K, Kayama T, Yamashita H. Age-Related Changes in Astigmatism and Potential Causes. Cornea. 2020 Nov:39 Suppl 1():S34-S38. doi: 10.1097/ICO.0000000000002507. Epub [PubMed PMID: 33038156]
Yang S, Zhang J, Tan Y, Wang Y. Unraveling the mechanobiology of cornea: From bench side to the clinic. Frontiers in bioengineering and biotechnology. 2022:10():953590. doi: 10.3389/fbioe.2022.953590. Epub 2022 Oct 3 [PubMed PMID: 36263359]
Garcia ML, Huang D, Crowe S, Traboulsi EI. Relationship between the axis and degree of high astigmatism and obliquity of palpebral fissure. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus. 2003 Feb:7(1):14-22 [PubMed PMID: 12690364]
Level 2 (mid-level) evidenceWang LL, Wang W, Han XT, He MG. Influence of severity and types of astigmatism on visual acuity in school-aged children in southern China. International journal of ophthalmology. 2018:11(8):1377-1383. doi: 10.18240/ijo.2018.08.20. Epub 2018 Aug 18 [PubMed PMID: 30140644]
Wang Y, Zhao K, Jin Y, Niu Y, Zuo T. Changes of higher order aberration with various pupil sizes in the myopic eye. Journal of refractive surgery (Thorofare, N.J. : 1995). 2003 Mar-Apr:19(2 Suppl):S270-4 [PubMed PMID: 12699188]
Teshigawara T, Meguro A, Mizuki N. Effects of Rebamipide on Differences in Power and Axis of Corneal Astigmatism Between Two Intra-patient Keratometric Measurements in Dry Eyes. Ophthalmology and therapy. 2021 Dec:10(4):891-904. doi: 10.1007/s40123-021-00368-9. Epub 2021 Jul 22 [PubMed PMID: 34292514]
Kessel L, Andresen J, Tendal B, Erngaard D, Flesner P, Hjortdal J. Toric Intraocular Lenses in the Correction of Astigmatism During Cataract Surgery: A Systematic Review and Meta-analysis. Ophthalmology. 2016 Feb:123(2):275-286. doi: 10.1016/j.ophtha.2015.10.002. Epub 2015 Nov 18 [PubMed PMID: 26601819]
Level 1 (high-level) evidenceHiep NX, Khanh PTM, Quyet D, Thai TV, Nga VT, Dinh TC, Bac ND. Correcting Corneal Astigmatism with Corneal Arcuate Incisions during Femtosecond Laser Assisted Cataract Surgery. Open access Macedonian journal of medical sciences. 2019 Dec 30:7(24):4260-4265. doi: 10.3889/oamjms.2019.371. Epub 2019 Dec 20 [PubMed PMID: 32215074]
Wu HK. Astigmatism and LASIK. Current opinion in ophthalmology. 2002 Aug:13(4):250-5 [PubMed PMID: 12165710]
Level 3 (low-level) evidence