Introduction
Pneumonia is a common lower respiratory tract infection that results in significant morbidity and is a leading cause of hospitalization and mortality globally.[1] Pneumonia can occur at any age, even without risk factors. However, it is more common in children younger than 5, adults older than 75, and those with risk factors such as cigarette smoking and chronic obstructive pulmonary disease.[2] Worldwide, pneumonia is the second most common cause of death in children younger than 5. In the United States, it is the second most common cause of hospitalization in children and adults.[3] Depending on when and where the patient has acquired the infection, pneumonia can be divided into community- and hospital-acquired pneumonia.[4] Community-acquired pneumonia is defined as pneumonia acquired in the community when there has been no contact with a healthcare setting.[4] With the advent of rapid diagnostic tests, the organisms responsible for community-acquired pneumonia can now be identified faster, appropriate antimicrobial therapy can be administered sooner, or empiric antimicrobials can be de-escalated, thus practising good antimicrobial stewardship. Community-acquired pneumonia can generally be caused by typical bacteria, viruses, and atypical bacteria. These rapid diagnostics have also demonstrated that respiratory viruses play a more significant role in the epidemiology of community-acquired pneumonia than initially thought.[5] These viruses can be the sole cause or the initial cause of pneumonia, followed by a secondary bacterial infection with a typical bacterium, such as Streptococcus pneumoniae or Staphylococcus aureus. This activity focuses on typical bacteria, including S. pneumoniae, Haemophilus influenzae, S. aureus, and Moraxella catarrhalis.[5][6] Despite advancements in the prevention, diagnosis, and treatment of pneumonia, including vaccines, newer antimicrobials, and more rapid diagnostics, mortality is still high in older adults, especially those who present with respiratory failure or shock.[5]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Community-acquired pneumonia is a heterogeneous entity caused by different pathogens and manifests with different clinical presentations depending on age, geography, and recent exposures. The first definitions for community-acquired pneumonia almost a century ago included only patients in the community who had no prior exposure to healthcare settings.[7] In recent years, as patients have had more contact with healthcare systems and bacteria have become more resistant, a new definition of pneumonia has emerged for those with previous contact with healthcare settings, termed healthcare-associated pneumonia (HCAP). Such bacteria include methicillin-resistant S. aureus, Pseudomonas aeruginosa, and Acinetobacter baumannii.[8][9] The 2019 American Thoracic Society/Infectious Diseases Society of America (ATS/IDSA) community-acquired pneumonia guidelines now include patients in the community who have had contact with healthcare settings but developed pneumonia in the community in the definition of community-acquired pneumonia. Such patients include those who have been hospitalized or who are receiving hemodialysis. Antibiotic resistance is associated with previous use of antibiotics and exposure to healthcare settings, among other risk factors.[5][10]
Identifying the microbial etiology of community-acquired pneumonia is crucial for targeted and timely antibiotic therapy. However, the cause remains unidentified in approximately 50% of patients with pneumonia. High-quality sputum specimens may be able to identify typical bacterial pathogens and differentiate them from normal respiratory flora.[5][6] Traditionally, the bacterial etiology of community-acquired pneumonia was S. pneumoniae, H. influenzae, Mycoplasma pneumoniae, S. aureus, Legionella spp., and M. catarrhalis.[11] M. pneumoniae and Legionella spp. are atypical pathogens and are not discussed here. The microbiology of community-acquired pneumonia is evolving, now including pathogens typically found in healthcare settings, which may exhibit higher antibiotic resistance. Furthermore, with the increased use of molecular diagnostics, such as nucleic acid amplification technology, the diagnosis has been revolutionized, as viral pneumonia has been increasingly detected, alone or as a coinfection with bacteria.[5] We now know that community-acquired pneumonia can be caused not only by bacteria, whether typical or atypical, and fungi, such as histoplasmosis in specific geographic areas, but also by viruses.[5][6]
Identifying the specific cause of community-acquired pneumonia in patients with community-acquired pneumonia has not always been possible, primarily because obtaining an adequate sputum sample is complex. In addition, standard microbiological methods do not detect viruses. The specific microbiology of community-acquired pneumonia varies based on patient demographics, comorbidities, geographic location, and vaccination status. This review discusses typical bacteria that cause community-acquired pneumonia and highlights other pathogens reflecting the current shifting microbiology.
Bacteria can colonize the oropharynx after being transmitted by infected individuals. They can then cause pneumonia when they are micro- or macro-aspirated into the lungs. When this occurs, the host's immune system cannot fight off the infection, or the bacterial inoculum is too large, resulting in pneumonia. Pneumonia can also occur as secondary pneumonia in the setting of a previous or concomitant viral infection, such as during or after viral influenza, respiratory syncytial virus, and COVID-19.[12] Respiratory viruses are found in over half of the children diagnosed with pneumonia in the United States, with the most common viruses being respiratory syncytial virus, rhinovirus, and metapneumovirus.[5]
From the earliest reports on the bacteriological etiology of community-acquired pneumonia until a few decades ago, pneumonia was an infection caused by typical community bacteria. The most common typical bacteria were, and still are, S. pneumoniae and H. influenzae; hospital-acquired pneumonia had not yet become an entity. Large case series between 1917 and 1933 reported that S. pneumoniae was the cause of lobar pneumonia in 95% of cases.[13] Bacterial pneumonia was diagnosed using clinical exams, x-rays, and laboratory values. Etiologic pathogens were identified using sputum Gram stain and culture, and in bacteremic patients, they could also be detected through blood cultures. S. pneumoniae remains the most common bacterial cause of community-acquired pneumonia in all age groups worldwide, followed by H. influenzae, S. aureus, Enterobacterales, Klebsiella spp., P. aeruginosa, and other gram-negative bacteria.[6][13] The incidence of S. pneumoniae and H. influenzae has been declining in the community in some countries, such as the United States, most likely due to the widespread administration of the H. influenzae type b (Hib) and pneumococcal conjugate vaccines in immunization programs.[6][14] The incidence of these bacteria has also likely declined because molecular methods have shown that viruses cause pneumonia in 10% to 30% of cases alone or as a viral/bacterial coinfection.[6] Pneumonias can also develop as secondary bacterial pneumonia, most commonly due to S. pneumoniae and S. aureus, following a viral infection, such as influenza, COVID, and respiratory syncytial virus.
In addition, a small proportion of patients in the community may have risk factors that predispose them to oropharyngeal or pulmonary colonization with bacteria found in healthcare settings, such as methicillin-resistant S. aureus, K. pneumoniae, Enterobacterales, and P. aeruginosa.[8] Furthermore, patients with certain conditions, such as cystic fibrosis and chronic obstructive pulmonary disease, may be colonized with P. aeruginosa or other gram-negative bacteria and develop pneumonia caused by these pathogens.
K. pneumoniae warrants special mention due to its frequent multidrug resistance (MDR) and can be hypervirulent, causing hospital outbreaks. K. pneumoniae has also emerged as a community-acquired pathogen globally in recent years, particularly in many Asian countries such as Japan, South Korea, and China, demonstrating epidemic spread.[15][16][17] The increasing presence of MDR strains in the community poses a growing public health threat. The etiology of community-acquired pneumonia in many Asian countries, especially China, is slightly different from that in other countries, with gram-negative bacilli, especially P. aeruginosa, K. pneumoniae, and A. baumanii, being the most frequent causes of community-acquired pneumonia. Documented increases in nasopharyngeal carriage of these pathogens further contribute to their spread in the community.[6][16]
Epidemiology
Community-acquired pneumonia is a leading cause of mortality and morbidity, with substantial clinical and economic impact and loss of disability-adjusted life-years.[1][18] Community-acquired pneumonia results in 3 million deaths annually globally.[19] Reliable data are available only from a few countries and are used in the Global Burden of Disease (GBD) reports. According to the GBD 2019, lower respiratory tract infections were the cause of 2.49 million deaths, and mortality was the highest in adults older than 70. Lower respiratory tract infections were the second leading cause of disability-adjusted life-years in children younger than 10 and the sixth in adults older than 75.[18][20]
Pneumonia can be caused by a wide range of pathogens, including bacteria (typical and atypical), viruses, and fungi, and the etiology depends on age, comorbidities, geographical location, exposure to healthcare settings, and the host's immune system. Pneumonia occurs more frequently in susceptible individuals, particularly in children younger than 5 and adults older than 70, with or without comorbidities.[5] According to the GBD 2016, there were 2,377,697 deaths due to lower respiratory tract infections in individuals of all ages and 1,080,958 deaths in adults older than 70.[5] The leading bacterial cause of morbidity and mortality from lower respiratory tract infections was S. pneumoniae, followed by H. influenzae, causing more deaths than all other infectious causes of lower respiratory tract infections combined in 2016, namely Hib, influenza virus, and respiratory syncytial virus.[1]
Risk factors for developing community-acquired pneumonia include male gender, age younger than 5 and older adults (especially those older than 65), passive and active smoking, malnutrition, diabetes mellitus, cardiovascular disease, asthma and chronic bronchitis, neurological disease with impaired swallowing, immunosuppression, alcohol dependence, influenza infection, poor dental hygiene, contact with children, and the use of proton pump inhibitors.[5][21]
A systematic analysis of the 2021 GBC report on non-COVID respiratory infections estimated 4350 cases of lower respiratory tract infections per 100,000 population. Among these, 502,000 deaths were in children younger than 5, and of these, 254,000 deaths took place in low socio-demographic index countries.[18] Of the 18 pathogen categories identified in 2021, S. pneumoniae was responsible for the highest proportions of lower respiratory tract infection episodes, with an estimated 97.9 million episodes and 505,000 deaths globally.[18] In the United States, 2.1% of total deaths from 1999 to 2019 were due to pneumonia. During that time, mortality declined in women and men in most age cohorts. Pneumonia rates and deaths were higher among males compared to females.[22] The incidence of community-acquired pneumonia in Europe differs across the continent, ranging from 20.6 in Iceland [23] to 79.9 cases per 10,000 person-years in the United Kingdom.[24]
A comprehensive study by Liu et al examined the etiology, causal characteristics, and infection patterns of community-acquired pneumonia in all age groups in China.[16] Respiratory syncytial virus and S. pneumoniae (12.61%) were the most common causes of severe community-acquired pneumonia in children younger than 5, and influenza and P. aeruginosa (15.7%) among older adults. Multivariate analyses revealed that severe community-acquired pneumonia was significantly associated with infections caused by human adenovirus, human rhinovirus, K. pneumoniae, or coinfections of respiratory syncytial virus with H. influenzae or respiratory syncytial virus with S. aureus in children and adolescents younger than 18. In adults aged 18 or older, severe community-acquired pneumonia was significantly linked to infections with P. aeruginosa, K. pneumoniae, or S. pneumoniae, and coinfections involving P. aeruginosa and K. pneumoniae.[16]
Pathophysiology
The pulmonary system and airways are continuously exposed to particulate matter and environmental pathogens. The oropharynx and healthy airways typically contain some bacterial species and are not sterile, but bacteria can colonize the oropharynx after transmission from another person. The primary routes by which bacteria reach the lung parenchyma and cause pneumonia include micro-aspiration, macro-aspiration, and hematogenous spread.[25]
The pulmonary defense mechanisms, such as the cough reflex, mucociliary clearance, and immune response, help maintain low microbiome levels in the oropharynx and the bronchial tree. Community-acquired pneumonia occurs when there are lower host defenses; impaired cough reflex; impaired mucociliary clearance; accumulations of secretions, as observed in conditions such as cystic fibrosis; and when defects in the immune response are present. When a virulent pathogen is present or the infectious microbial inoculum is substantial, a deficiency in the host's defense mechanisms can result in pneumonia.[25]
The alveolar macrophage is the predominant immune cell that responds to bacteria in the lower airways. However, when a highly virulent pathogen or a large bacterial inoculum is present, the immune response intensifies as alveolar macrophages recruit polymorphonuclear neutrophils to phagocytose and eliminate the bacteria. The alveolar macrophages release cytokines, namely, tumor necrosis factor-alpha (TNF-α) and interleukins. Interleukin-8 (IL-8) and granulocyte colony-stimulating factor promote neutrophil chemotaxis and maturation. The leakage of the alveolar-capillary membrane due to cytokines can lead to decreased lung compliance, resulting in dyspnea. Cytokines such as IL-1 and TNF can lead to constitutional symptoms such as fever. Bacterial pneumonia is a result of this inflammatory response. These cytokines are essential for immunity, but the excess can lead to sepsis and multiorgan failure. The body balances cytokines' deleterious effects by attenuating several inflammatory mechanisms with IL-10.[25] The acute inflammation produced by this immune response generates an influx of inflammatory cells into the alveoli, resulting in a radiological consolidation pattern.
Please see StatPearls' companion resource, "Bacterial Pneumonia", for further information.
Histopathology
Pneumonia is an acute infection of the lung parenchyma caused by various pathogens, excluding bronchiolitis.[26] Based on the area of the lung involved, pneumonia can be classified histologically into lobular, lobar, bronchopneumonia, and interstitial. Lobar pneumonia is an acute exudative inflammation of the entire lobe with a complete or near-complete lung lobe consolidation. The majority of these cases are caused by S. pneumoniae.[25][27]
If left untreated, lobar pneumonia progresses through four classical stages of the inflammatory response: [25][27]
- Congestion/consolidation occurs in the first 24 hours when the lungs appear heavy, red, and boggy. Microscopically, this condition is characterized by vascular engorgement and intra-alveolar edema, with many bacteria and few neutrophils present.
- Red hepatization/early consolidation begins 2 to 3 days after consolidation and lasts 2 to 4 days. This stage is named after its firm, liver-like consistency. The affected lung is red-pink, dry, granular, and airless. Fibrin strands replace the edema fluid of the previous phase. Microscopically, there is a marked neutrophilic exudate, some containing ingested bacteria, along with extravasated erythrocytes, desquamated epithelial cells, and fibrin within the alveoli. The alveolar septa become less prominent because of the exudate.
- Grey hepatization/late consolidation occurs 2 to 3 days following red hepatization and lasts 4 to 8 days. The lung appears gray with liver-like consistency due to fibrinopurulent exudate, progressive disintegration of red blood cells, and hemosiderin. The macrophages begin to appear.
- Resolution and restoration of the pulmonary architecture start by the eighth day. The enzymatic action begins centrally and spreads peripherally, liquefying the previously solid fibrinous content and restoring aeration. Macrophages are the predominant cells, containing engulfed neutrophils and debris.[25]
Toxicokinetics
S. pneumoniae is the most common cause of typical bacterial pneumonia worldwide. The polysaccharide capsule of S. pneumoniae inhibits the complement binding to the cell surface, thereby hindering phagocytosis. Virulent pneumococcal proteins include IgA1 protease, neuraminidase, pneumolysin, autolysin, and surface proteins.[28][29]
History and Physical
Obtaining a detailed history and performing a thorough clinical physical examination are essential when evaluating any patient who seeks medical care. The signs and symptoms of pneumonia vary depending on disease severity, age, underlying diseases, and pathogen. Comorbidities such as cardiopulmonary disease, neurological impairment, HIV, renal and liver disease, age, sex, smoking, alcohol misuse, and poor dental hygiene can increase the risk of community-acquired pneumonia.[21][30] Vaccination history may be relevant for H. influenzae and B. pertussis infections.[31] Intravenous drug use can be a risk factor for bacterial pneumonia, including Staphylococcal pneumonia.[32] The most common symptoms of bacterial pneumonia include fever, cough, shortness of breath, and sputum production. Other symptoms include fatigue, headache, myalgia, hemoptysis, rigors, and arthralgias. Pleuritic chest pain due to localized inflammation of the pleura may also be present. In severe cases, hypotension may be present. Signs of pneumonia may include tachypnea, tachycardia, use of accessory muscles, and altered mental status, especially in severe disease or older patients.[5][10]
Obtaining the patient's medical history, including any history of cancer, immunosuppression, or difficulty swallowing, is essential. A history of asthma, chronic obstructive pulmonary disease, smoking, and immunocompromised status can suggest H. influenzae infection.[33][34] A detailed social history should also be obtained, such as whether the patient is or was a smoker, where the patient has lived, and whether they have had any recent sick contacts. The patient's immunization history is also essential, most notably whether the patient has received the pneumococcal and annual influenza vaccines. Distinguishing between viral and bacterial lower respiratory tract infections can be challenging based on history alone or in conjunction with the physical examination.[5][10]
The character of the patient's sputum may point towards specific bacteria in acute respiratory illness. S. pneumoniae may produce rust-colored sputum, P. aeruginosa may produce green sputum, and H influenzae may have red-currant jelly-colored sputum. Anaerobic pneumonia produces foul-smelling sputum.[5][10] However, more recent evidence suggests that sputum color may not always correlate with indicative organisms.[35]
On examination, auscultation of the lungs may reveal crackles, rales, and bronchial breath sounds. Depending on the degree of consolidation and presence/absence of pleural effusion, increased vocal fremitus, egophony, and dullness to percussion are the major clinical signs.[5][10]
Please see StatPearls' companion resource, "Bacterial Pneumonia", for further information.
Evaluation
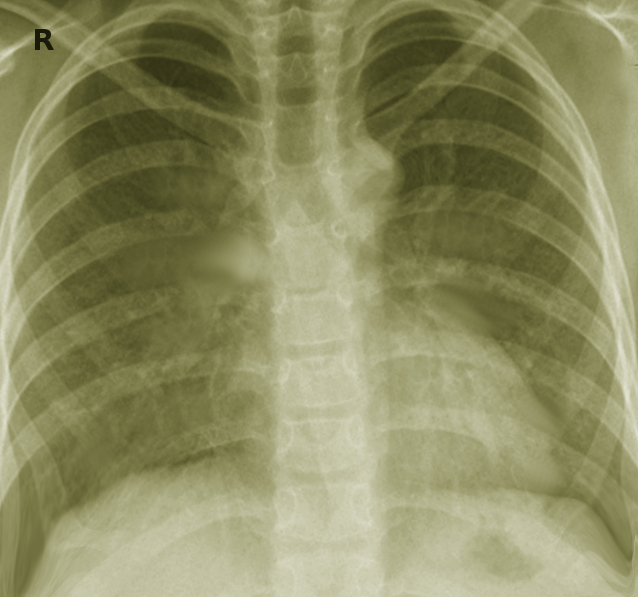
The diagnosis of community-acquired pneumonia initially relies on clinical evaluation with signs and symptoms that include cough, sputum production, fever, pleuritic chest pain, dyspnea, and hypoxia. Radiographic findings on a chest x-ray aid in confirming the diagnosis when an infiltrate is present. A chest x-ray can not only show the presence of a pulmonary infiltrate but also provide clues to the type of pneumonia present, such as lobar or interstitial, and can also show evidence of a para-pneumonic effusion. Infection with typical bacteria typically results in lobar pneumonia with or without parapneumonic pleural effusions.[5][10] However, a chest x-ray cannot differentiate a bacterial from a non-bacterial cause, such as viral infections, and other parameters are needed. A chest x-ray showing pneumonia is considered the gold standard, especially when laboratory tests and clinical features point toward diagnosing pneumonia. Computed tomography can also be used if the diagnosis is not confirmed by chest x-ray, when more definition needs to be visualized, or when other processes may be present.[5][10]
Evaluating the severity of the disease is crucial in determining whether the patient needs to be hospitalized or treated as an outpatient. The CURB-65 pneumonia severity score or expanded CURB-65 can be used to stratify patients. One point is given for each parameter below: [5][10]
- Confusion
- Uremia: Blood urea nitrogen >20 mg/dL
- Respiratory rate >30 breaths/min
- Hypotension: Systolic blood pressure <90 mm Hg and diastolic blood pressure <60 mm Hg
- Age older than 65
A CURB-65 score of ≥2 is an indication for hospitalization. A score of ≥4 indicates intensive care unit admission.
Routine laboratory tests are optional for stable patients in outpatient settings. However, for patients presenting with severe community-acquired pneumonia, specific laboratory tests such as a chemistry panel, including creatinine and liver function tests, and a complete blood count with a manual differential should be ordered.[5][10] Leukocytosis may be present with or without a leftward shift, supporting the diagnosis of infection. Leukopenia and thrombocytopenia may be observed and may be related to the severity of the infection. Inflammatory biomarkers, such as erythrocyte sedimentation rate and acute phase reactants like C-reactive protein (CRP), should be ordered as supportive markers for inflammation and severity.[5][10]
Clinical signs and symptoms and CRP levels cannot be used reliably to differentiate between viral and bacterial pneumonia. Simultaneously, testing for respiratory viruses should also be performed, as secondary bacterial pneumonia can occur following a viral infection, and coinfection is also possible.[5][10] Testing for viruses could include a respiratory viral panel, but certainly influenza.[5]
Identifying the etiologic bacteria to guide antibiotic therapy is crucial when obtaining a good sputum sample. This approach is important due to the evolving landscape of microbiology, the potential emergence of resistant pathogens, and the opportunity to administer targeted antibiotic treatment. In addition, it allows for the possibility of de-escalating therapy when appropriate.[5][10]
Sputum and blood cultures should be obtained from all patients with severe community-acquired pneumonia. Additional microbiological tests, such as microscopy, phenotypic, and molecular tests, can be used to define the causative organism. Bench tests that may suggest typical bacterial organisms include:
- Gram staining
- Gram-positive cocci: S. pneumoniae, S. aureus
- Gram-negative bacilli: H. influenzae, P. aeruginosa, A. baumannii, K. pneumoniae
- Gram-negative coccobacilli: B. pertussis, M. catarrhalis.
- Coagulase testing
- S. aureus
- Catalase testing
- Staphylococci versus Streptococci
- Optochin testing
- S. pneumoniae
- Antibiotic susceptibility testing/disc diffusion
- Aerobic versus anaerobic testing
Diagnosing the causative pathogen can be challenging and is achieved in only 50% of cases.[5][10] Obtaining a good sputum sample can be difficult, as expectoration may produce saliva containing oral flora rather than sputum. In addition, patients may already have received antibiotics, making their sputum sterile.[5][10]
Other methods include antigen-based rapid diagnostics tests, which have demonstrated a high specificity but medium sensitivity.[36] The S. pneumoniae urinary antigen test, previously recommended in the 2007 ATS/IDSA guidelines, is no longer advised in the 2019 guidelines. This change is due to the lack of supporting evidence and its inability to alter the antibiotic regimen.[7][37][38] Rapid nucleic-acid amplification tests showed similar results but can be performed more rapidly than a polymerase chain reaction.[36]
Please see StatPearls' companion resource, "Bacterial Pneumonia", for further information.
Treatment / Management
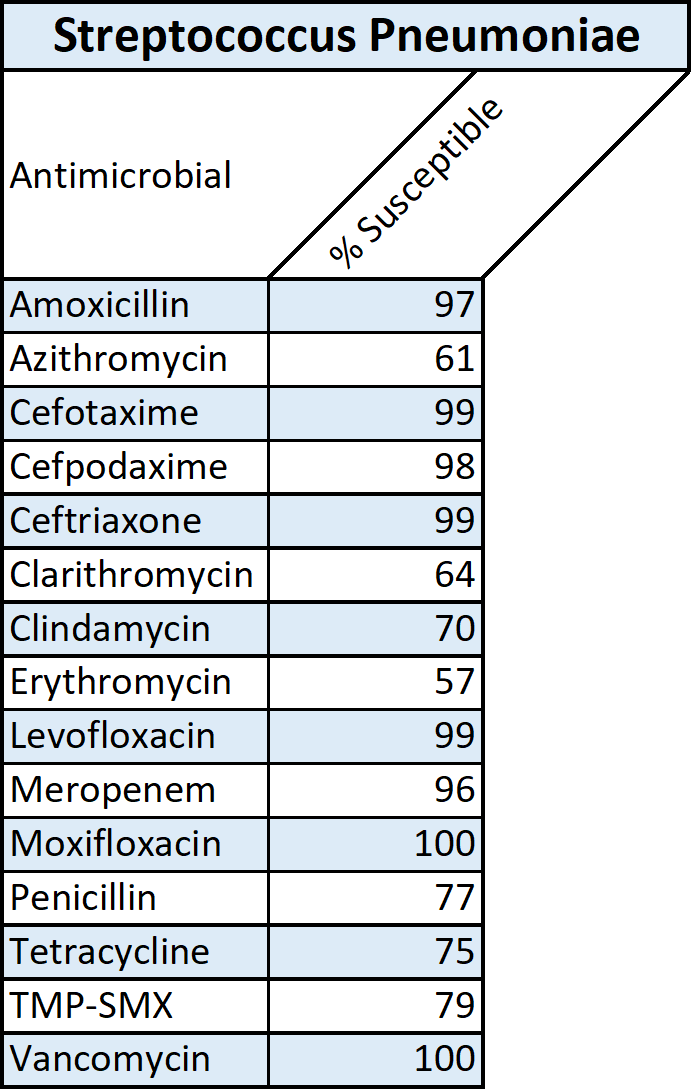
Antibiotic therapy is the mainstay of treatment of community-acquired pneumonia and should be initiated promptly. The choice of antibiotics can either target the typical bacteria or be broadened to include coverage for other pathogens, including MDR ones. In such cases, broad-spectrum antibiotics may be administered, with de-escalation of therapy required as appropriate.[5][10] Empirical antibiotic therapy should be chosen based on the most likely etiology, which is determined by factors such as the severity of the infection, patient comorbidities, whether the patient is hospitalized or managed as an outpatient, and risk factors for MDR bacteria or pathogens commonly associated with healthcare settings, such as methicillin-resistant S. aureus, P. aeruginosa, and K pneumoniae.[5][10] Determining whether the patient requires inpatient or outpatient treatment is essential. The CURB-65 pneumonia severity score and the expanded CURB-65 are examples of bedside scoring systems that can stratify patients.[5][10] Local antibiotic resistance profiles of typical bacteria should be considered when deciding on the antibiotic of choice. In the case of S. pneumoniae, antibiotic resistance to macrolides is emerging and, in some countries, is significant.(A1)
Outpatient Management
- Patients with no risk factors for MDR pathogens and no comorbidities should be treated with effective antibiotics against typical bacteria. According to the 2019 ATS/IDSA guidelines, the following regimens are recommended based on the strength of evidence: [5][10]
- Amoxicillin 1 g 3 times daily (based on strong evidence) OR
- Doxycycline 100 mg twice daily (based on conditional recommendation with low quality of evidence) OR
- A macrolide only in areas with pneumococcal resistance to macrolides <25% (conditional recommendation, moderate quality of evidence).
(A1)
- For patients with comorbidities such as diabetes mellitus, cardiovascular disease, and asplenia, the following treatments are recommended, in no particular order: [5][10]
- Combination therapy:
- Amoxicillin/clavulanate 500 mg/125 mg 3 times daily, or amoxicillin/clavulanate 875 mg/125 mg twice daily, or 2000 mg/125 mg twice daily, or
- Cephalosporin (cefpodoxime 200 mg twice daily or cefuroxime 500 mg twice daily) PLUS
- Macrolide (azithromycin 500 mg on the first day, then 250 mg daily; clarithromycin (500 mg twice daily or extended-release 1000 mg once daily)) (strong recommendation, moderate quality of evidence for combination therapy) OR
- Doxycycline 100 mg twice daily (conditional recommendation, low quality of evidence for combination therapy); OR
- Monotherapy:
- Respiratory fluoroquinolone (levofloxacin 750 mg daily, moxifloxacin 400 mg daily, or gemifloxacin 320 mg daily) (strong recommendation, moderate quality of evidence).
(A1) - Combination therapy:
Inpatient Management
- Patients with non-severe community-acquired pneumonia without risk factors for methicillin-resistant S. aureus or P. aeruginosa: [5][10]
- Combination therapy with a β-lactam (ampicillin+sulbactam 1.5-3 g every 6 h, cefotaxime 1-2 g every 8 h, ceftriaxone 1-2 g daily, or ceftaroline 600 mg every 12 h) PLUS a macrolide (azithromycin 500 mg daily or clarithromycin 500 mg twice daily) (based on strong recommendation, high quality of evidence) OR
- Monotherapy with a respiratory fluoroquinolone (levofloxacin 750 mg daily, moxifloxacin 400 mg daily) (based on strong recommendation, high quality of evidence).[5][10]
- If there is a contraindication to macrolides and fluoroquinolones, this alternative is another option. Combination therapy with a β-lactam (ampicillin+sulbactam, cefotaxime, ceftaroline, or ceftriaxone, doses as above) and doxycycline 100 mg twice daily (conditional recommendation, low quality of evidence).
(A1)
- Patients with severe community-acquired pneumonia without risk factors for methicillin-resistant S. aureus or P. aeruginosa: [5][10]
- A β-lactam plus a macrolide (strong recommendation, moderate quality of evidence); OR
- A β-lactam plus a respiratory fluoroquinolone (strong recommendation, low quality of evidence).
(A1)
Please see StatPearls' companion resource, "Bacterial pneumonia", for further information.
Differential Diagnosis
When diagnosing typical bacterial pneumonia, it is essential to differentiate it from a variety of conditions that can present with similar respiratory symptoms, including:
- Asthma or reactive airway disease
- Viral pneumonia
- Fungal pneumonia
- Atypical bacterial pneumonia
- Lung abscess
- Bronchiectasis
- Bronchiolitis
- Asthma
- Acute and chronic bronchitis
- Atelectasis
- Croup
- Respiratory distress syndrome
- Cardiac diseases, including heart failure
- Aspiration of a foreign body [39][40]
Prognosis
Typical pneumonia can vary in prognosis, depending on many factors, including age; cognitive status; comorbidities, such as malignancy and chronic respiratory diseases; immunosuppression; chronic alcohol misuse; inpatient or outpatient status; and the need for ventilatory support.[41] Older patients are more likely to have poorer clinical outcomes than younger individuals.[42] In an observational study, patients aged 65 or older with pneumonia secondary to S. pneumoniae had higher mortality rates by day 30 compared to those without S. pneumoniae, despite adjusting for vaccination.[43] Mortality in typical bacterial pneumonia may also be associated with the causative pathogen involved in infection, with Pseudomonas spp., S. aureus, and polymicrobial infections having higher mortality rates compared to other species.[44][45][46][47]
If left untreated, the overall mortality may be up to 30%.[42][48] A higher PSI score has been associated with poorer resolution of pneumonia. Raised inflammatory markers, anemia, confusion, and elevated blood urea nitrogen are also associated with poorer outcomes.[49] Early clinical failure has been associated with persisting tachypnea, hypoxia, confusion, and arterial blood acidosis by day 3 of treatment for pneumonia.[50] Coinfection with viral respiratory infections, such as influenza and COVID-19, has been associated with an increased risk of mortality when infected with bacterial pneumonia, indicating the public health importance of vaccination in vulnerable and at-risk populations.[51][52]
Please see StatPearls' companion resource, "Bacterial Pneumonia", for more information.
Complications
Complications associated with typical bacterial pneumonia can arise due to the progression of the infection or its impact on surrounding tissues, leading to severe outcomes such as:
- Pleural effusion
- Empyema
- Lung abscess
- Acute respiratory distress syndrome
- Pulmonary fibrosis
- Sepsis
- Bacteremia
- Chronic hypoxemia
Deterrence and Patient Education
Patients with relevant risk factors for developing typical pneumonia should be counselled to prevent future episodes, including smoking cessation, abstinence from hazardous alcohol use, and maintaining dental hygiene.[53][54][55] Since bacterial pneumonia is transmitted by direct inoculation from fomites or respiratory droplets, appropriate hand hygiene is strongly encouraged to prevent transmission.[56] Vaccination should be encouraged in at-risk populations against Hib, S. pneumoniae, influenza, and respiratory syncytial virus.[57]
Enhancing Healthcare Team Outcomes
Pneumonia is a common infectious lung disease that requires an interprofessional approach involving multiple subspecialties. A patient-centered model that includes clinicians, physiotherapists, respiratory therapists, nurses, pharmacists, and support groups plays a crucial role in improving the quality of care for pneumonia patients. This collaborative approach not only reduces hospital admission rates but also enhances disease outcomes.
For healthy patients, the outcomes after treatment are excellent, but in older individuals and those with comorbidities, the outcomes are guarded based on their pre-existing health status and course of disease. Various non-pharmacological measures can help reduce future risk, including appropriate dental care in collaboration with dentists, speech pathology input for any dysphagia, and involvement of psychology and drug and alcohol teams for individuals at risk of hazardous alcohol use or injection drug use. Treating clinicians should remain aware of the complementary management strategies these interprofessional healthcare teams provide to optimize care for patients with typical bacterial pneumonia.
Please see StatPearls' companion resource, "Bacterial Pneumonia", for further information.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
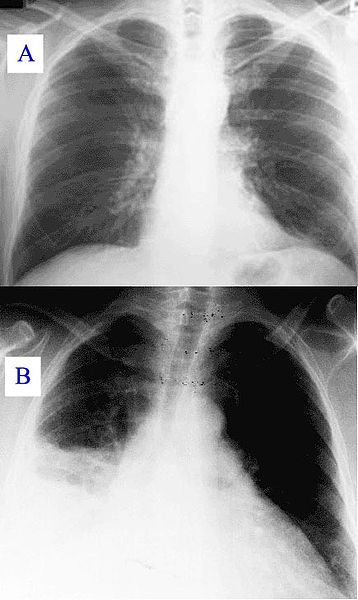
Healthy Lung and Q Fever Pneumatic Lung, Chest X-ray. X-ray A represents a normal healthy lung; X-ray B represents a lung with Q fever pneumonia.
Hehkuviini, Public Domain, via Wikimedia Commons.
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
GBD 2016 Lower Respiratory Infections Collaborators. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet. Infectious diseases. 2018 Nov:18(11):1191-1210. doi: 10.1016/S1473-3099(18)30310-4. Epub 2018 Sep 19 [PubMed PMID: 30243584]
Level 1 (high-level) evidenceGBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet (London, England). 2020 Oct 17:396(10258):1204-1222. doi: 10.1016/S0140-6736(20)30925-9. Epub [PubMed PMID: 33069326]
Level 1 (high-level) evidenceKaiser SV, Rodean J, Coon ER, Mahant S, Gill PJ, Leyenaar JK. Common Diagnoses and Costs in Pediatric Hospitalization in the US. JAMA pediatrics. 2022 Mar 1:176(3):316-318. doi: 10.1001/jamapediatrics.2021.5171. Epub [PubMed PMID: 34962555]
Burnham JP, Kollef MH. CAP, HCAP, HAP, VAP: The Diachronic Linguistics of Pneumonia. Chest. 2017 Nov:152(5):909-910. doi: 10.1016/j.chest.2017.05.002. Epub [PubMed PMID: 29126531]
Torres A, Cilloniz C, Niederman MS, Menéndez R, Chalmers JD, Wunderink RG, van der Poll T. Pneumonia. Nature reviews. Disease primers. 2021 Apr 8:7(1):25. doi: 10.1038/s41572-021-00259-0. Epub 2021 Apr 8 [PubMed PMID: 33833230]
Shoar S, Musher DM. Etiology of community-acquired pneumonia in adults: a systematic review. Pneumonia (Nathan Qld.). 2020:12():11. doi: 10.1186/s41479-020-00074-3. Epub 2020 Oct 5 [PubMed PMID: 33024653]
Level 1 (high-level) evidenceMandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, Dowell SF, File TM Jr, Musher DM, Niederman MS, Torres A, Whitney CG, Infectious Diseases Society of America, American Thoracic Society. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2007 Mar 1:44 Suppl 2(Suppl 2):S27-72 [PubMed PMID: 17278083]
Level 3 (low-level) evidenceLe MN, Kayama S, Yoshikawa M, Hara T, Kashiyama S, Hisatsune J, Tsuruda K, Onodera M, Ohge H, Tsuga K, Sugai M. Oral colonisation by antimicrobial-resistant Gram-negative bacteria among long-term care facility residents: prevalence, risk factors, and molecular epidemiology. Antimicrobial resistance and infection control. 2020 Mar 4:9(1):45. doi: 10.1186/s13756-020-0705-1. Epub 2020 Mar 4 [PubMed PMID: 32131899]
American Thoracic Society, Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. American journal of respiratory and critical care medicine. 2005 Feb 15:171(4):388-416 [PubMed PMID: 15699079]
Level 1 (high-level) evidenceMetlay JP, Waterer GW, Long AC, Anzueto A, Brozek J, Crothers K, Cooley LA, Dean NC, Fine MJ, Flanders SA, Griffin MR, Metersky ML, Musher DM, Restrepo MI, Whitney CG. Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. American journal of respiratory and critical care medicine. 2019 Oct 1:200(7):e45-e67. doi: 10.1164/rccm.201908-1581ST. Epub [PubMed PMID: 31573350]
Level 1 (high-level) evidenceDel Rio-Pertuz G, Gutiérrez JF, Triana AJ, Molinares JL, Robledo-Solano AB, Meza JL, Ariza-Bolívar OM, Acosta-Reyes J, Garavito A, Viasus D, Carratalà J. Usefulness of sputum gram stain for etiologic diagnosis in community-acquired pneumonia: a systematic review and meta-analysis. BMC infectious diseases. 2019 May 10:19(1):403. doi: 10.1186/s12879-019-4048-6. Epub 2019 May 10 [PubMed PMID: 31077143]
Level 1 (high-level) evidenceMorens DM, Taubenberger JK, Fauci AS. Predominant role of bacterial pneumonia as a cause of death in pandemic influenza: implications for pandemic influenza preparedness. The Journal of infectious diseases. 2008 Oct 1:198(7):962-70. doi: 10.1086/591708. Epub [PubMed PMID: 18710327]
Gadsby NJ, Musher DM. The Microbial Etiology of Community-Acquired Pneumonia in Adults: from Classical Bacteriology to Host Transcriptional Signatures. Clinical microbiology reviews. 2022 Dec 21:35(4):e0001522. doi: 10.1128/cmr.00015-22. Epub 2022 Sep 27 [PubMed PMID: 36165783]
Moberley S, Holden J, Tatham DP, Andrews RM. Vaccines for preventing pneumococcal infection in adults. The Cochrane database of systematic reviews. 2013 Jan 31:2013(1):CD000422. doi: 10.1002/14651858.CD000422.pub3. Epub 2013 Jan 31 [PubMed PMID: 23440780]
Level 1 (high-level) evidenceChen IR, Lin SN, Wu XN, Chou SH, Wang FD, Lin YT. Clinical and Microbiological Characteristics of Bacteremic Pneumonia Caused by Klebsiella pneumoniae. Frontiers in cellular and infection microbiology. 2022:12():903682. doi: 10.3389/fcimb.2022.903682. Epub 2022 Jun 23 [PubMed PMID: 35811668]
Liu YN, Zhang YF, Xu Q, Qiu Y, Lu QB, Wang T, Zhang XA, Lin SH, Lv CL, Jiang BG, Li H, Li ZJ, Gao GF, Yang WZ, Hay SI, Wang LP, Fang LQ, Liu W, Chinese Center for Disease Control and Prevention Etiology Surveillance Study Team of Acute Respiratory Infections. Infection and co-infection patterns of community-acquired pneumonia in patients of different ages in China from 2009 to 2020: a national surveillance study. The Lancet. Microbe. 2023 May:4(5):e330-e339. doi: 10.1016/S2666-5247(23)00031-9. Epub 2023 Mar 28 [PubMed PMID: 37001538]
Level 2 (mid-level) evidenceMarr CM, Russo TA. Hypervirulent Klebsiella pneumoniae: a new public health threat. Expert review of anti-infective therapy. 2019 Feb:17(2):71-73. doi: 10.1080/14787210.2019.1555470. Epub 2018 Dec 5 [PubMed PMID: 30501374]
GBD 2021 Lower Respiratory Infections and Antimicrobial Resistance Collaborators. Global, regional, and national incidence and mortality burden of non-COVID-19 lower respiratory infections and aetiologies, 1990-2021: a systematic analysis from the Global Burden of Disease Study 2021. The Lancet. Infectious diseases. 2024 Sep:24(9):974-1002. doi: 10.1016/S1473-3099(24)00176-2. Epub 2024 Apr 15 [PubMed PMID: 38636536]
Level 1 (high-level) evidenceFerreira-Coimbra J, Sarda C, Rello J. Burden of Community-Acquired Pneumonia and Unmet Clinical Needs. Advances in therapy. 2020 Apr:37(4):1302-1318. doi: 10.1007/s12325-020-01248-7. Epub 2020 Feb 18 [PubMed PMID: 32072494]
Level 3 (low-level) evidenceGBD 2019 LRI Collaborators. Age-sex differences in the global burden of lower respiratory infections and risk factors, 1990-2019: results from the Global Burden of Disease Study 2019. The Lancet. Infectious diseases. 2022 Nov:22(11):1626-1647. doi: 10.1016/S1473-3099(22)00510-2. Epub 2022 Aug 11 [PubMed PMID: 35964613]
Torres A, Peetermans WE, Viegi G, Blasi F. Risk factors for community-acquired pneumonia in adults in Europe: a literature review. Thorax. 2013 Nov:68(11):1057-65. doi: 10.1136/thoraxjnl-2013-204282. Epub [PubMed PMID: 24130229]
Bondarchuk CP, Grobman B, Mansur A, Lu CY. National trends in pneumonia-related mortality in the United States, 1999-2019. Infectious diseases (London, England). 2025 Jan:57(1):56-65. doi: 10.1080/23744235.2024.2390180. Epub 2024 Aug 8 [PubMed PMID: 39115964]
Bjarnason A, Westin J, Lindh M, Andersson LM, Kristinsson KG, Löve A, Baldursson O, Gottfredsson M. Incidence, Etiology, and Outcomes of Community-Acquired Pneumonia: A Population-Based Study. Open forum infectious diseases. 2018 Feb:5(2):ofy010. doi: 10.1093/ofid/ofy010. Epub 2018 Feb 8 [PubMed PMID: 29479548]
Millett ER, Quint JK, Smeeth L, Daniel RM, Thomas SL. Incidence of community-acquired lower respiratory tract infections and pneumonia among older adults in the United Kingdom: a population-based study. PloS one. 2013:8(9):e75131. doi: 10.1371/journal.pone.0075131. Epub 2013 Sep 11 [PubMed PMID: 24040394]
Jain V, Vashisht R, Yilmaz G, Bhardwaj A. Pneumonia Pathology. StatPearls. 2025 Jan:(): [PubMed PMID: 30252372]
Mackenzie G. The definition and classification of pneumonia. Pneumonia (Nathan Qld.). 2016:8():14. doi: 10.1186/s41479-016-0012-z. Epub 2016 Aug 22 [PubMed PMID: 28702293]
Kradin RL, Digumarthy S. The pathology of pulmonary bacterial infection. Seminars in diagnostic pathology. 2017 Nov:34(6):498-509. doi: 10.1053/j.semdp.2017.06.001. Epub 2017 Jun 7 [PubMed PMID: 28655479]
Yamaguchi M, Minamide Y, Terao Y, Isoda R, Ogawa T, Yokota S, Hamada S, Kawabata S. Nrc of Streptococcus pneumoniae suppresses capsule expression and enhances anti-phagocytosis. Biochemical and biophysical research communications. 2009 Dec 4:390(1):155-60. doi: 10.1016/j.bbrc.2009.09.099. Epub 2009 Sep 30 [PubMed PMID: 19799870]
Cools F, Torfs E, Vanhoutte B, de Macedo MB, Bonofiglio L, Mollerach M, Maes L, Caljon G, Delputte P, Cappoen D, Cos P. Streptococcus pneumoniae galU gene mutation has a direct effect on biofilm growth, adherence and phagocytosis in vitro and pathogenicity in vivo. Pathogens and disease. 2018 Oct 1:76(7):. doi: 10.1093/femspd/fty069. Epub 2018 Oct 1 [PubMed PMID: 30215741]
Almirall J, Serra-Prat M, Bolíbar I, Balasso V. Risk Factors for Community-Acquired Pneumonia in Adults: A Systematic Review of Observational Studies. Respiration; international review of thoracic diseases. 2017:94(3):299-311. doi: 10.1159/000479089. Epub 2017 Jul 25 [PubMed PMID: 28738364]
Level 1 (high-level) evidenceJohnston ID, Strachan DP, Anderson HR. Effect of pneumonia and whooping cough in childhood on adult lung function. The New England journal of medicine. 1998 Feb 26:338(9):581-7 [PubMed PMID: 9475765]
Level 2 (mid-level) evidenceHind CR. Pulmonary complications of intravenous drug misuse. 2. Infective and HIV related complications. Thorax. 1990 Dec:45(12):957-61 [PubMed PMID: 2281430]
Chin CL, Manzel LJ, Lehman EE, Humlicek AL, Shi L, Starner TD, Denning GM, Murphy TF, Sethi S, Look DC. Haemophilus influenzae from patients with chronic obstructive pulmonary disease exacerbation induce more inflammation than colonizers. American journal of respiratory and critical care medicine. 2005 Jul 1:172(1):85-91 [PubMed PMID: 15805181]
Level 3 (low-level) evidenceHerrod HG, Gross S, Insel R. Selective antibody deficiency to Haemophilus influenzae type B capsular polysaccharide vaccination in children with recurrent respiratory tract infection. Journal of clinical immunology. 1989 Sep:9(5):429-34 [PubMed PMID: 2621246]
Miravitlles M, Kruesmann F, Haverstock D, Perroncel R, Choudhri SH, Arvis P. Sputum colour and bacteria in chronic bronchitis exacerbations: a pooled analysis. The European respiratory journal. 2012 Jun:39(6):1354-60. doi: 10.1183/09031936.00042111. Epub 2011 Oct 27 [PubMed PMID: 22034649]
Level 1 (high-level) evidenceGentilotti E, De Nardo P, Cremonini E, Górska A, Mazzaferri F, Canziani LM, Hellou MM, Olchowski Y, Poran I, Leeflang M, Villacian J, Goossens H, Paul M, Tacconelli E. Diagnostic accuracy of point-of-care tests in acute community-acquired lower respiratory tract infections. A systematic review and meta-analysis. Clinical microbiology and infection : the official publication of the European Society of Clinical Microbiology and Infectious Diseases. 2022 Jan:28(1):13-22. doi: 10.1016/j.cmi.2021.09.025. Epub 2021 Oct 1 [PubMed PMID: 34601148]
Level 1 (high-level) evidenceHyams C, Williams OM, Williams P. Urinary antigen testing for pneumococcal pneumonia: is there evidence to make its use uncommon in clinical practice? ERJ open research. 2020 Jan:6(1):. pii: 00223-2019. doi: 10.1183/23120541.00223-2019. Epub 2020 Jan 10 [PubMed PMID: 31956656]
Davis MR, McCreary EK, Trzebucki AM. Things We Do for No Reason - Ordering Streptococcus Pneumoniae Urinary Antigen in Patients With Community-Acquired Pneumonia. Open forum infectious diseases. 2024 Mar:11(3):ofae089. doi: 10.1093/ofid/ofae089. Epub 2024 Feb 8 [PubMed PMID: 38524231]
Hauswaldt J, Blaschke S. [Dyspnea]. Der Internist. 2017 Sep:58(9):925-936. doi: 10.1007/s00108-017-0276-2. Epub [PubMed PMID: 28608125]
Berliner D, Schneider N, Welte T, Bauersachs J. The Differential Diagnosis of Dyspnea. Deutsches Arzteblatt international. 2016 Dec 9:113(49):834-845. doi: 10.3238/arztebl.2016.0834. Epub [PubMed PMID: 28098068]
Ito A, Ishida T, Tokumasu H, Washio Y, Yamazaki A, Ito Y, Tachibana H. Prognostic factors in hospitalized community-acquired pneumonia: a retrospective study of a prospective observational cohort. BMC pulmonary medicine. 2017 May 2:17(1):78. doi: 10.1186/s12890-017-0424-4. Epub 2017 May 2 [PubMed PMID: 28464807]
Level 2 (mid-level) evidenceHespanhol V, Bárbara C. Pneumonia mortality, comorbidities matter? Pulmonology. 2020 May-Jun:26(3):123-129. doi: 10.1016/j.pulmoe.2019.10.003. Epub 2019 Nov 29 [PubMed PMID: 31787563]
Ruiz LA, España PP, Gómez A, Bilbao A, Jaca C, Arámburu A, Capelastegui A, Restrepo MI, Zalacain R. Age-related differences in management and outcomes in hospitalized healthy and well-functioning bacteremic pneumococcal pneumonia patients: a cohort study. BMC geriatrics. 2017 Jun 20:17(1):130. doi: 10.1186/s12877-017-0518-0. Epub 2017 Jun 20 [PubMed PMID: 28633626]
Cillóniz C, Ewig S, Polverino E, Marcos MA, Esquinas C, Gabarrús A, Mensa J, Torres A. Microbial aetiology of community-acquired pneumonia and its relation to severity. Thorax. 2011 Apr:66(4):340-6. doi: 10.1136/thx.2010.143982. Epub 2011 Jan 21 [PubMed PMID: 21257985]
Level 2 (mid-level) evidencePoovieng J, Sakboonyarat B, Nasomsong W. Bacterial etiology and mortality rate in community-acquired pneumonia, healthcare-associated pneumonia and hospital-acquired pneumonia in Thai university hospital. Scientific reports. 2022 May 30:12(1):9004. doi: 10.1038/s41598-022-12904-z. Epub 2022 May 30 [PubMed PMID: 35637232]
Vlaeminck J, Raafat D, Surmann K, Timbermont L, Normann N, Sellman B, van Wamel WJB, Malhotra-Kumar S. Exploring Virulence Factors and Alternative Therapies against Staphylococcus aureus Pneumonia. Toxins. 2020 Nov 18:12(11):. doi: 10.3390/toxins12110721. Epub 2020 Nov 18 [PubMed PMID: 33218049]
Liao C, Huang X, Wang Q, Yao D, Lu W. Virulence Factors of Pseudomonas Aeruginosa and Antivirulence Strategies to Combat Its Drug Resistance. Frontiers in cellular and infection microbiology. 2022:12():926758. doi: 10.3389/fcimb.2022.926758. Epub 2022 Jul 6 [PubMed PMID: 35873152]
Fine MJ, Smith MA, Carson CA, Mutha SS, Sankey SS, Weissfeld LA, Kapoor WN. Prognosis and outcomes of patients with community-acquired pneumonia. A meta-analysis. JAMA. 1996 Jan 10:275(2):134-41 [PubMed PMID: 8531309]
Level 1 (high-level) evidenceLi JS, Hou ZK, Yu XQ, Li SY, Sun ZK, Zhang W, Jia XH, Zheng SP, Wang MH, Wang HF. Prognostic factors for community-acquired pneumonia in middle-aged and elderly patients treated with integrated medicine. Journal of traditional Chinese medicine = Chung i tsa chih ying wen pan. 2012 Jun:32(2):179-86 [PubMed PMID: 22876440]
Hoogewerf M, Oosterheert JJ, Hak E, Hoepelman IM, Bonten MJ. Prognostic factors for early clinical failure in patients with severe community-acquired pneumonia. Clinical microbiology and infection : the official publication of the European Society of Clinical Microbiology and Infectious Diseases. 2006 Nov:12(11):1097-104 [PubMed PMID: 17002609]
Level 2 (mid-level) evidenceBarnes CE, MacIntyre CR. Risk modelling the mortality impact of antimicrobial resistance in secondary pneumococcal pneumonia infections during the 2009 influenza pandemic. International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases. 2019 Aug:85():1-6. doi: 10.1016/j.ijid.2019.05.005. Epub 2019 May 13 [PubMed PMID: 31096052]
Scott H, Zahra A, Fernandes R, Fries BC, Thode HC Jr, Singer AJ. Bacterial infections and death among patients with Covid-19 versus non Covid-19 patients with pneumonia. The American journal of emergency medicine. 2022 Jan:51():1-5. doi: 10.1016/j.ajem.2021.09.040. Epub 2021 Sep 28 [PubMed PMID: 34637995]
Level 2 (mid-level) evidenceBaskaran V, Murray RL, Hunter A, Lim WS, McKeever TM. Effect of tobacco smoking on the risk of developing community acquired pneumonia: A systematic review and meta-analysis. PloS one. 2019:14(7):e0220204. doi: 10.1371/journal.pone.0220204. Epub 2019 Jul 18 [PubMed PMID: 31318967]
Level 1 (high-level) evidencede Roux A, Cavalcanti M, Marcos MA, Garcia E, Ewig S, Mensa J, Torres A. Impact of alcohol abuse in the etiology and severity of community-acquired pneumonia. Chest. 2006 May:129(5):1219-25 [PubMed PMID: 16685012]
Son M, Jo S, Lee JS, Lee DH. Association between oral health and incidence of pneumonia: a population-based cohort study from Korea. Scientific reports. 2020 Jun 12:10(1):9576. doi: 10.1038/s41598-020-66312-2. Epub 2020 Jun 12 [PubMed PMID: 32533077]
Rabie T, Curtis V. Handwashing and risk of respiratory infections: a quantitative systematic review. Tropical medicine & international health : TM & IH. 2006 Mar:11(3):258-67 [PubMed PMID: 16553905]
Level 1 (high-level) evidenceTessmer A, Welte T, Schmidt-Ott R, Eberle S, Barten G, Suttorp N, Schaberg T, CAPNETZ study group. Influenza vaccination is associated with reduced severity of community-acquired pneumonia. The European respiratory journal. 2011 Jul:38(1):147-53. doi: 10.1183/09031936.00133510. Epub 2010 Dec 9 [PubMed PMID: 21148226]
Level 2 (mid-level) evidence