Introduction
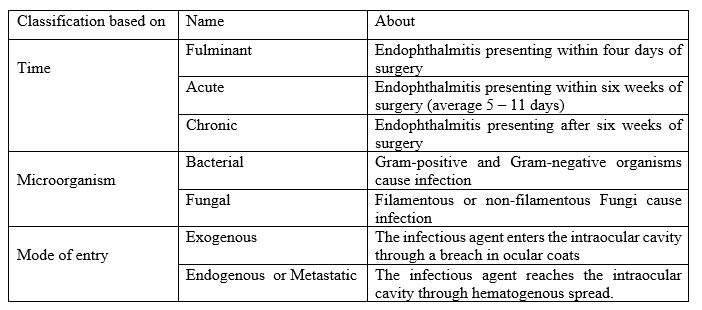
Endophthalmitis is defined as an inflammation of the inner coats of the eye, resulting from intraocular colonization of infectious agents with exudation within intraocular fluids (vitreous and aqueous).[1] Based on the mode of entry of the organism, it is divided into 'exogenous' and 'endogenous.' Depending on the causative event, the exogenous endophthalmitis can be either post-traumatic or postoperative.[2] Some of the definitions used in endophthalmitis are listed in figure 1 (classification of endophthalmitis). Unless diagnosed and treated promptly, acute endophthalmitis can lead to severe vision loss. The category or type of endophthalmitis such as postoperative, post-traumatic or endogenous, and others influence the clinical presentation, microbiology, and visual outcome. Endophthalmitis is one of the most serious ophthalmic emergencies which require urgent medical attention and treatment to save the vision or to salvage the integrity of the eye.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Depending on the infectious agent producing endophthalmitis, two important categories are recognized, bacterial and fungal endophthalmitis. In a recent study on microbial causes of all types of endophthalmitis, 85.1% of all isolates were due to gram-positive bacteria, 10.3% due to gram-negative bacteria, and 4.6% of all cases were due to fungi.[3] The most common bacterial pathogens isolated are Staphylococcus epidermidis (30.3%), other coagulase-negative Staphylococcus (9.1%), Streptococcus viridans (12.1%), Staphylococcus aureus (11.1%), Enterobacteriaceae (3.4%), and Pseudomonas aeruginosa (2.5%).[3]
The predominant organism depends on the source (vegetable matter or retained intraocular foreign body), route of spread (post-surgery, trauma, or delayed onset or hematogenous dissemination), geographic location, and patient characteristics.
In cases of post-traumatic endophthalmitis, Staphylococci and Bacillus cereus are the most common isolates.[4]
Acute postoperative endophthalmitis (within 6 weeks of surgery) results most commonly due to contamination of the intraocular structures with normal bacterial flora of the adnexa such as Staphylococcal epidermidis.
Delayed or chronic post-cataract surgery endophthalmitis (after 6-week of surgery) is characterized by slow course and panuveitis like picture with granulomatous keratic precipitates, inflammatory deposits over the IOL (intraocular lens), white capsular plaque, anterior chamber reaction, vitritis, and cystoid macular edema (CME) which may respond to periocular or systemic steroid but usually recurs.[5] The common causative organism is usually bacterial (most commonly Propionibacterium acnes followed by Coagulase-negative Staphylococcus), though fungal infections (including Aspergillus, Candida, and others) can also occur.[6]
In cases of delayed onset, endophthalmitis associated with bleb (trabeculectomy)/glaucoma drainage implants Streptococci species, and Haemophilus are the predominant culture isolates.[7][8]
The most common organisms isolated in post intravitreal injection endophthalmitis are coagulase-negative staphylococci followed by streptococci.[9]
In certain conditions, exogenous endophthalmitis can occur without a full-thickness breach in ocular coats. For example, after scleral buckling (due to buckle exposure or secondary infections), secondary to contact lens keratitis, and post LASIK.[10][11][12]
Most cases of endogenous endophthalmitis are secondary to fungemia (predominantly Candida species). Among bacterial causes, staphylococcal species predominate in the western population, and among the East Asian population, Klebsiella pneumoniae predominates.[13] Pseudomonas is a virulent and aggressive organism that can also cause endogenous endophthalmitis.[14]
Endophthalmitis after infectious keratitis is usually bacterial (usually Pseudomonas aeruginosa, Staphylococcus sp, and Streptococcus sp), though fungal endophthalmitis (including Aspergillus sp, Fusarium sp) may also occur.[15][16]
Epidemiology
The relative frequency of various subtypes of endophthalmitis varies depending upon the geography, level of specialization at the ophthalmic center, and study duration. For example, studies before 2005 have very few cases of post intravitreal anti-VEGF (vascular endothelial growth factor) injection endophthalmitis as anti-VEGF agents received first FDA approval in 2004.
In a recent retrospective cohort study in the U.S., acute onset endophthalmitis occurred in 0.04% of cataract surgeries and 0.016% of patients receiving an intravitreal injection.[17][18] The incidence of post-traumatic endophthalmitis varies from 0.9% to 17%.[19][20]
Case series from Asian countries have reported an incidence of 0.023% to 0.076% of endophthalmitis in post-cataract surgery setting and 0.01% to 0.10% post intravitreal injections.[21][22][23][24]
Among the intraocular surgeries, secondary intraocular lens implantation seems to have a very high risk (0.36%) for acute endophthalmitis, and trabeculectomy may have a high risk (1.8%, maybe up to 5.7%) for delayed or late-onset endophthalmitis especially after the advent of mitomycin-C or 5-fluorouracil.[2][25][26]
Endophthalmitis after pars plana vitrectomy had the lowest rates (0.046%) when compared with other ocular surgeries [secondary IOL-0.366%, combined penetrating keratoplasty (PK) with cataract surgery- 0.194%, PK- 0.178%, glaucoma surgeries -0.124%, combined trabeculectomy and cataract surgery- 0.114%, overall incidence after intraocular surgery-0.093%, and cataract surgery with or without IOL-0.082%] in a study.[25]
There is no significant difference in the rates of endophthalmitis after intravitreal injection of various anti-VEGF agents.[27][28] Cluster endophthalmitis cases have occurred after intravitreal use of bevacizumab due to either lapse in the cold chain, sub-optimal compounding of bevacizumab aliquots, or fake drug.[29][30]
Pathophysiology
The most critical factor in the causation of endophthalmitis is the breakdown of the ocular blood barrier and intraocular colonization by pathogens (bacteria/fungi). In exogenous endophthalmitis, the inciting injury or surgery causes disruption of globe integrity, which allows invasion of the pathogens. In rare cases of delayed postoperative endophthalmitis, the organisms (usually Propionibacterium acnes sequestered in the capsular bag after cataract surgery) may get released after YAG capsulotomy causing endophthalmitis.[31] In endogenous endophthalmitis, common sources of bacteremia and fungemia include endocarditis, urinary tract infections, intravenous infusions, indwelling catheters or invasive procedures, liver abscess, and others.
The pathogen's ability to cause intraocular damage depends on its virulence and host response. The virulence of an organism depends on:
- Its ability to synthesize toxic factors such as hemolysin BL, cytolysin, pneumolysin, lipopolysaccharide (bacterial outer envelope), and others[32][33][34][35]
- The rapidity of intraocular growth[36]
- Motility of organism[37]
The ability of the host's innate immunity to mount an effective inflammatory response depends on the virulence of the organism. The acute inflammatory response may clear the less virulent organism; However, more virulent organisms may evade the host's immune response by secreting toxins or biofilm around it, in which case the inflammatory response can result in damage to intraocular tissues and loss of vision. The peak of inflammatory mediators such as TNFα, interleukin 1-beta, interferon-gamma coincides with increased inflammatory signs such as fibrin in the anterior chamber, iris synechiae formation, hypopyon, and loss of the red reflex.[38] The elevated levels of complement factors in aqueous and vitreous in cases of intraocular infection contribute to the damage of the uveoretinal tissue.
History and Physical
In typical postoperative endophthalmitis, poor visual acuity, corneal edema, hypopyon, vitreous inflammation, and poor fundus visualization are the most common clinical signs.[39]
Reduced vision and worsening pain - In Endophthalmitis Vitrectomy Study (EVS) study, reduction in vision and pain accounted for 94% and 74% of all symptoms while in the ESCRS study, it accounted for 92.9% and 79% of all symptoms.[40][41][40] These studies show that though pain is a significant diagnostic sign, pain can be absent in up to 25% of cases. The other common presenting features are swollen eyelid, redness of the eye, circumcorneal congestion, photophobia, ocular discharge, fibrinous membranes in the anterior chamber, iris synechiae formation, loss of fundal red reflex, and floaters. Bleb-related endophthalmitis initially presents as bacterial conjunctivitis with signs and symptoms such as conjunctival hyperemia and discharge, yellowish colored filtering bleb, and variable anterior chamber inflammatory reaction, which later progresses to involve the posterior chamber as well. Certain signs, if seen such as corneal ring abscess, are highly suggestive of Bacillus, while gas bubbles in the anterior chamber, amaurosis, or green-brown hypopyon indicate Clostridium.[42][43]
In chronic endophthalmitis, patients present with low-grade anterior chamber inflammation and vitritis. Visual acuity can remain preserved until late in the presentation. Organisms such as Propionibacterium tend to get localized within the capsular bag and present as posterior capsular plaque.[44] The vital history that should raise suspicion of chronic endophthalmitis following keratitis or intraocular surgery is prolonged uveitis in a subject with no previous history of inflammation and either inadequate response to topical steroids or inability to wean them.[45]
In patients with endogenous endophthalmitis, the presentation can be bilateral with systemic morbidities like sepsis, nausea, vomiting, and fever. Endogenous bacterial endophthalmitis presents with pain, blurred vision, and redness with a variable degree of both anterior chamber and vitreous involvement. A subretinal abscess may be noted.[46] Endogenous fungal endophthalmitis presents initially as focal choroiditis or chorioretinitis, which later extends into the vitreous cavity. Retinal vascular sheathing and vascular occlusion may be present with satellite lesions in certain conditions.[47]
Endophthalmitis after infectious keratitis presents with hypopyon and severe visual loss, sometimes with an inaccurate projection of rays. Ultrasound evaluation of the posterior segment can help to detect vitreous involvement in the form of echoes in the vitreous and confirm the diagnosis.
Progression of the disease may lead to panophthalmitis, corneal infiltration and perforation, and phthisis bulbi.
Due to severe damage to ocular structures, the workup of endophthalmitis is done on an emergency basis.
History
- Inciting event – surgery/trauma/contiguous spread (keratitis)/endogenous endophthalmitis/other procedure
- Onset – fulminant/acute/chronic: Most cases of fulminant endophthalmitis are caused by highly virulent organisms such as Pseudomonas aeruginosa / Bacillus species (see figure on the classification of endophthalmitis)
- The rapidity of progression – Rapid or gradual: Bacterial endophthalmitis progresses faster than fungal endophthalmitis.
- Systemic illness – history of intravenous infusion, prolonged hospitalization, diabetes, renal or liver problems: Helps to localize any source of endogenous endophthalmitis, calibrating drug dosage.
Ophthalmic Assessment
Clinical
1. Visual acuity including projection of rays- When visual acuity is less than counting fingers, EVS standards help in the maintenance of uniform records. After occluding the better eye, with light directed from behind the patient:
Hand movements are tested at a distance of 60 cm
Perception of light is tested at a distance of 90 cm with the bright light of indirect ophthalmoscope
At least four out of five responses should be correct for reading to be considered.
2. Examination of the ocular adnexa- especially to look for severe blepharitis, meibomitis, stye, chronic dacryocystitis, and other sources of infection3. Ocular movements- Reduced or absent ocular movements in a case of endophthalmitis with proptosis and pain, clinically point to the diagnosis of panophthalmitis4. Anterior segment examination [close focus at the sites of entry – SICS(small incision cataract surgery) tunnel/ Corneal entry wound / Bleb/ perforating trauma] look for corneal clarity; corneal infiltrate, Posterior capsular plaque, vitreous in the wound, open wound, unsutured wound, hypopyon, fibrin, posterior synechia5. Intraocular pressure6. Fundus examination (dilated) if media permits to look for any specific pattern as well as mimics such as dropped lens matter/ intraocular foreign body (IOFB)
Grading of vitreous haze (EVS standard) [clinical examination with an indirect ophthalmoscope][40]
- Grade 1: More than 20/40 (6/12) view of the retina
- Grade 2: Second order retinal vessels are visible
- Grade 3: Some vessels visible but not the second-order vessels
- Grade 4: No retinal vessels are visible, only red reflex present
- Grade 5: No red reflex is seen
Evaluation
Imaging
- Slit-lamp photography to document
- Fundus photographs- especially ultra-widefield imaging (Optos) using scanning laser ophthalmoscope principle which can image through the small pupil and vitreous haze[48][49]
- Fundus fluorescein angiogram (FFA) if the fundus is visible- May help to rule out other diseases
- Optical coherence tomography (OCT)- When fundus is visible, OCT can help to characterize the location and other characteristics of retinochoroidal or vascular involvement
- Anterior segment OCT in case of endophthalmitis after infective keratitis and others
- Ultrasound B scan – Endophthalmitis gives rise to vitreous inflammation, which is seen as point echoes in the vitreous cavity with mild to moderate amplitude. Ultrasound examination is also used to look for other features, including retinochoroidal thickening, posteriorly dislocated lens/IOL, concomitant retinal detachment, choroidal detachment, or IOFB, to follow up vitreous inflammatory reaction serially post intravitreal injection. A subretinal abscess at the macula may be present, especially in endogenous endophthalmitis.
- CT scan orbits to look for IOFB in post-trauma cases
Ocular Sampling
1. Anterior chamber tap
With the patient looking straight, a 30G/27G needle is introduced via a selected site on the peripheral cornea tangentially keeping direction parallel to the iris, with the needle directed towards exudate/hypopyon. With active suction, 0.1 to 0.2 cc of aqueous/exudate is aspirated. A cotton tip applicator is applied, and the needle is removed.
2. Vitreous tap/biopsy
Vitreous cultures usually produce more accurate results than do aqueous cultures.[50]
Vitreous Tap
A 26 G needle is connected to a 2 cc syringe and is entered through pars plans (3 mm behind limbus in aphakic, 3.5 mm behind limbus in pseudophakic, and 4 mm behind the limbus in phakic). A sample of 0.2 to 0.3 cc is aspirated. It is controversial in non-vitrectomized eyes due to the possibility of vitreous traction and subsequent retinal detachment. In such cases, vitreous biopsy via vitrectomy cutter is preferred.
Vitreous biopsy
This can be obtained via one port vitrector or by combining it with a three-port diagnostic/ therapeutic pars plana vitrectomy. A 5 ml syringe is connected to the suction port of the vitrectomy cutter, and once the cutter port is visualized through the pupil, the surgical assistant aspirates, without starting the infusion. At the same time, the surgeon activates the cutter until the eye softens visibly. When combined with a three-port vitrectomy, the fluid infusion is turned on once the sample has been collected as described.
Samples are sent for microbiological and molecular diagnostic (PCR) testing. Though PCR allows improved pathogen detection even with low pathogen counts, cost, increased risk of contamination, lack of antibiotic sensitivity testing, lack of quality control standards limit its widespread usage.[51]
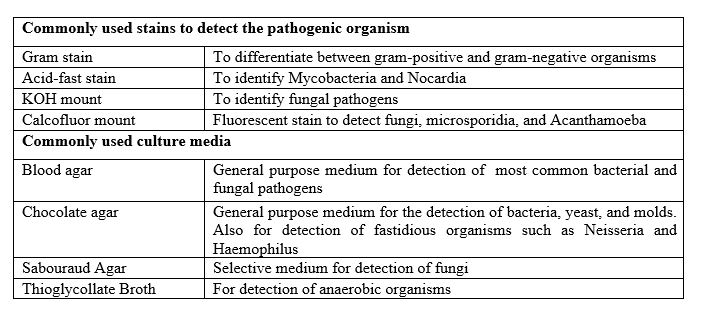
The standard microbiological procedure includes smear preparation for specific stains and inoculation of selective culture media for recovery of intraocular pathogens and antibiotic sensitivity testing. Commonly used stains and culture media are elaborated in figure 2 (commonly used stains and culture media for the detection of microbial agents).
Systemic Assessment
- Look for signs of septicemia – fever, elevated ESR (erythrocyte sedimentation rate)
- Blood culture in cases of endogenous endophthalmitis
- Blood tests – hemogram, renal, and liver function tests (to look for drug toxicity)
- Search for the focus of infection in endogenous endophthalmitis
Treatment / Management
Endophthalmitis is a true ophthalmic emergency and requires appropriate and prompt therapy. The main objectives in endophthalmitis treatment are:
- To eradicate or control infection
- Management of inflammation
- Supportive therapy
1. To Eradicate or Control Infection
A. Systemic Antibiotics
The use of systemic antibiotics in the setting of exogenous endophthalmitis is controversial as most of the drugs given have poor intraocular penetration. The best-documented drugs achieving therapeutic levels in vitreous are fourth-generation fluoroquinolones[52], meropenem, and linezolid.[53]
EVS study used ceftazidime 2 g every 8 hourly, amikacin 7.5 mg/kg initial dose followed by 6 mg/kg every 12 hourly. EVS study has concluded that the use of systemic antibiotics does not affect the final visual outcome in postoperative endophthalmitis.[40](A1)
In endogenous endophthalmitis, systemic antimicrobials, in conjunction with intravitreal antimicrobials, reduce the rates of evisceration or enucleation.[54] (B3)
B. Local Antibiotics (topical/subconjunctival)
A combination of two drugs is preferred during the initial presentation, one having a potent effect on Gram-positive organisms and another on Gram-negative organisms. Once antibiotic sensitivity is determined, targeted intervention is done. In the presence of corneal ulcer or wound abscess, fortified drops (including cefazolin 5% and tobramycin 1.4%) are used. Sub conjunctival antibiotic injections are not routinely used due to issues with patient comfort, subconjunctival hemorrhage, and watering from the eye.
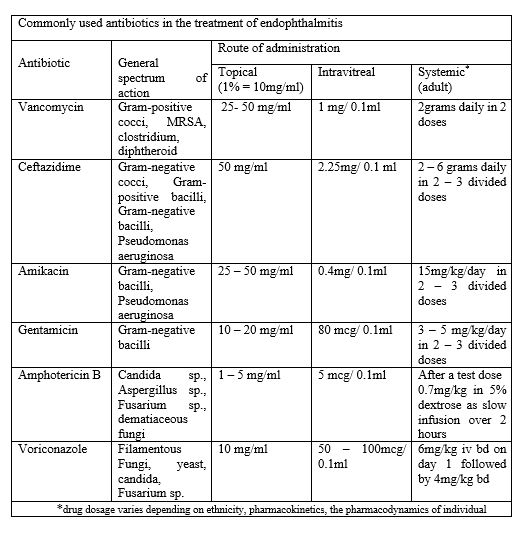
EVS study used vancomycin (25 mg/0.5 ml), ceftazidime (100 mg/0.5 ml) for subconjunctival injection, and topical vancomycin (50 mg/ml) and amikacin (20 mg/ml) every 4 hourly for routine cases or every hour if wound leak was present.[40](A1)
C. Intravitreal Injections
The intravitreal route of drug administration helps in achieving high concentrations of the drug in the vitreous cavity without associated systemic side effects. It is essential to ensure the proper dosage of the drug. While inadequate doses cause treatment failure, the excess dose can cause toxic effects on the retina. Two broad-spectrum antibiotics are chosen initially, EVS study utilized intravitreal vancomycin (1 mg/0.1 ml) and amikacin (0.4 mg/0.1 ml).[40] However, due to the higher retinotoxic potential of amikacin, it has been superseded by ceftazidime (2.25 mg/0.1 ml). Commonly used drugs in the treatment of endophthalmitis and their concentrations are enumerated in figure 3 (Commonly used antibiotics in the treatment of endophthalmitis). Intravitreal gentamicin can cause macular infarction.[55] (A1)
Recently, there is a trend towards the use of other intravitreal antibiotics such as:
- Ampicillin 5000 mcg/0.1 ml[56]
- Piperacillin/tazobactam 225 mcg (piperacillin 200 mcg and tazobactam 25 mcg/0.1 ml)[57]
- Imipenem/cilastatin (rabbit 50 to 100 mcg and 50 to 100 mcg/0.1ml)[58]
- Carbenicillin (rhesus monkey, 1000 mcg/0.1 ml)[59]
- Ticarcillin 3000 mcg/0.1 ml in albino rabbits[60]
- Cefazolin 2250 mcg/0.1 ml,[56]
- Cefotaxime 400 mcg/0.1 ml[56]
- Ceftriaxone 2000 mcg/0.1 ml[61]
- Cefuroxime 1000 mcg/0.1 ml[61]
- Clindamycin 1000 mcg/0.1 ml[61]
- Levofloxacin 625 mcg/0.1 ml[56]
- Moxifloxacin 500 mcg/0.1 ml[62] ( from the sterile moxifloxacin drop 0.5%, the reported patient had vitrectomized eye)
- Ciprofloxacin 100 mcg/0.1 ml[56]
- Aztreonam 100 mcg/0.1 ml[56]
- Colistin 100 mcg/0.1 ml[63][56][61] (B3)
Viruses usually do not cause suppurative inflammation of the eye or endophthalmitis, and rather they cause retinitis, which may be associated with retinitis. Many of such cases are treated by specific antivirals
D. Vitrectomy
Vitrectomy has several advantages over conservative therapy. Vitrectomy improves retinal oxygenation, reduces the inflammatory load within the eye, provides specimens for diagnostic evaluation, allows direct inspection of the retina, allows definitive treatment, reduces the load of infection, and reduces the severity of the disease, and accelerates visual rehabilitation.[64] There are two schools of thought: one based on EVS study and another based on complete and early vitrectomy for endophthalmitis (CEVE) study.[40][64] (A1)
According to the EVS study, vitrectomy was better than vitreous tap and intravitreal antibiotics for the most severe cases, i.e., for patients with initial presenting vision being the perception of light alone, and vitrectomy, if performed, is limited to core vitrectomy without inducing posterior vitreous detachment. Contrary to the EVS study, CEVE (complete and early vitrectomy for endophthalmitis) advocates complete vitrectomy, which includes induction and removal of posterior vitreous to prevent exudates from settling over the macula. However, in the periphery, the surgeon must be conservative to avoid iatrogenic break formation.
In delayed-onset endophthalmitis secondary to propionibacterium acnes, pars plana vitrectomy is combined with total capsulectomy and IOL exchange/removal or wash of the capsular bag with antibiotics.[44] (B3)
2. Management of Inflammation
Corticosteroids are the most potent anti-inflammatory agents used in the management of endophthalmitis. To be useful, they must be given early and in appropriate doses. They should, however, not be used in fungal endophthalmitis as it enhances fungal growth by weakening defense mechanisms within the body. They can be used either as an intravitreal injection, topical drops, or systemically.
The most commonly used corticosteroid intravitreally is dexamethasone (0.4 mg/ 0.1 ml). However, there is no clear consensus regarding the role of intravitreal corticosteroids.[65] Topical steroids can penetrate an intact cornea, and their efficacy is proportional to the frequency of installation. Systemic steroids are preferred at a dose of 1 to 1.5 mg/kg body weight administered in three divided doses to achieve uniform concentration during the day, unlike in chronic uveitis where once a day regimen is preferred.[66]
EVS study utilized only topical (prednisolone acetate 1% eye drops), subconjunctival (dexamethasone 6 mg/0.25 ml), and systemic steroids (prednisolone 30 mg twice a day for 5 to 10 days).[40](A1)
3. Supportive Therapy
Cycloplegic agent (homatropine 2%, atropine 1%) is an essential part of treatment that relieves ciliary spasms and prevents synechiae formation.
In patients with elevated intraocular pressure, oral and topical medications need to be added. Vitreous tap before intravitreal injection also reduces intraocular pressure.
Hypertonic saline (5% drop or 6% ointment) may be needed in cases of severe corneal edema.
Prophylaxis
Endophthalmitis cannot be prevented entirely, but due to various measures taken in recent times, its incidence has come down. Most of the cases of endophthalmitis are exogenous, which prompts for taking prophylactic action.
Proposed measures as prophylaxis of postoperative endophthalmitis include preoperative 5% povidone-iodine antisepsis of conjunctival cul de sac, check for lid infections preoperatively, checking the patency of nasolacrimal duct, use of intracameral cefuroxime 1000 mcg/0.1 ml[67][41] (according to the guideline by European society for cataract and refractive surgery)[68]/moxifloxacin (0.5% weight by volume from the sterile moxifloxacin drop 0.5%)[69][70]at the end of the surgical procedure, prompt repair of conjunctival erosions, leaking blebs.[71](A1)
A large study on 2 million eyes undergoing cataract surgery in the Aravind Eye Care System showed that intracameral moxifloxacin reduced the incidence of postcataract surgery endophthalmitis, especially in cases with complicated cataract surgery with posterior capsular rent.[70]
However, caution needs to be exercised regarding the use of intracameral antibiotics, as there are reports of retinal toxicity with certain antibiotics. For example, hemorrhagic occlusive retinal vasculitis (HORV) has been reported after the use of intracameral vancomycin.[72]
The most common contaminants in cases of post-intravitreal injections are streptococci, which are common members of oral flora, and oral flora bacteria may be aerosolized during the speech. The use of masks and adhering to a strict no-talking policy has been noted to be effective in reducing the overall incidence of post-injection endophthalmitis and particularly the incidence of streptococcal endophthalmitis.[73][74][73](B3)
Prompt surgical repair of open globe injuries and prophylactic intravitreal injection of antibiotics (particularly in the setting of retained intraocular foreign body) with or without systemic antibiotics have been associated with reduced rates of post-traumatic endophthalmitis.[75][76](A1)
Differential Diagnosis
Post-surgical Endophthalmitis
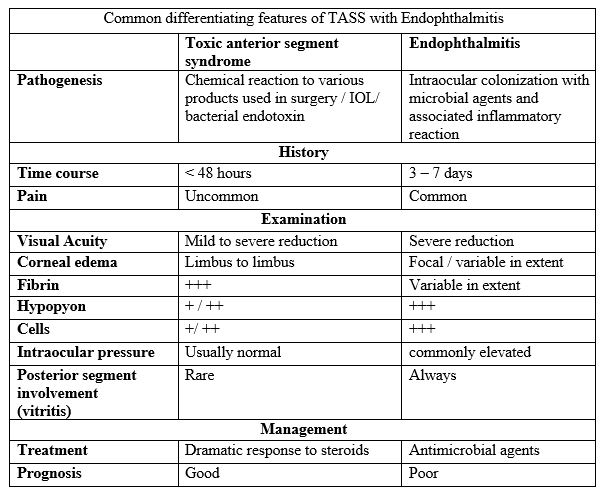
- Toxic anterior segment syndrome (TASS) is an acute inflammatory condition presenting within 24 hours of surgery with a severe anterior chamber reaction, limbus to limbus corneal edema. However, there is no adnexal involvement, and the patient responds dramatically to the addition of steroids.[77] Various features differentiating TASS from acute postoperative endophthalmitis are listed in figure 4 (common differentiating features of TASS with endophthalmitis).
- Posteriorly dislocated lens matter
- Fibrinous reaction post vitrectomy
- Phacoanaphylaxis etc.
Non-surgical Endophthalmitis
- Chronic uveitis – certain cases of chronic indolent endophthalmitis may be confused for chronic panuveitis.
- Retained intraocular foreign body
- Old vitreous hemorrhage
- Toxoplasma retinochoroiditis
- Necrotic retinoblastoma
- Acute retinal necrosis
- Severe panuveitis
- Seasonal hyperacute panuveitis (SHAPU)
- Intravitreal cysticercus with intraocular inflammation
Prognosis
Visual outcome in a patient with endophthalmitis depends on various variables.
- Nature of endophthalmitis: Better visual acuity has been reported in cases with culture-negative post-surgical endophthalmitis.[78] Bleb-associated endophthalmitis carries a poor visual prognosis.[79] Endogenous bacterial and fungal endophthalmitis also carries a poor visual prognosis.[54][80]
- Organism: Endophthalmitis due to Streptococcus,[78] Bacillus,[81] Pseudomonas,[82] and Candida[83] carry poor visual prognosis.
- Presenting visual acuity: In the EVS study, it has been noted that presenting visual acuity remains more powerful than microbiological factors in predicting visual outcome and response to vitrectomy.[40]
- Time to initiation of appropriate therapy: It is of utmost importance in cases of post-traumatic endophthalmitis, especially with Bacillus species.[84] In the EVS study, in the group with a vision of light perception only, early vitrectomy resulted in a three-fold increased chance to achieve ≥ 20/40 (33%), a two-fold increased chance to achieve ≥ 20/100 (56%) and was less likely to worsen <5/200 (20%).[40]
- Systemic stability of the patient: Immunocompromised patients, patients with endogenous endophthalmitis, have concurrent polymicrobial infections which influence the final outcome.[54]
In the EVS study in post-cataract surgery endophthalmitis, it was noted that only 53% of treated eyes had final visual acuity of 20/40 or better, and 15% had a final visual acuity of 20/200 or worse.[40]
If left untreated or inadequately treated, endophthalmitis progresses to panophthalmitis, requiring evisceration or enucleation of the eyeball. It is noted that patients suffering from a corneal ulcer, endogenous endophthalmitis, and low visual acuity are at higher risk of requiring evisceration or enucleation.[85]
Complications
- Panophthalmitis
- Glaucoma
- Orbital cellulitis
- Intracranial spread
- Septicemia
- Loss of vision
- Phthisis
- Hypotony
- Painful blind eye
Deterrence and Patient Education
Patients should be explained about the warning signs of endophthalmitis such as pain, redness of the eye and blurring of vision, etc. at discharge after any intraocular procedure. Early detection and prompt treatment are the key. Patients should be explained the seriousness of the condition and the need for intensive pharmacotherapy.
Enhancing Healthcare Team Outcomes
Most cases of endophthalmitis are exogenous and are seen in the postoperative period. Patients with uncontrolled blood sugar levels, high temperature (can be secondary to underlying septicemia) are prone to postoperative endophthalmitis. Hence the nursing staff and physician must check for systemic stability before any surgical procedure to reduce the chances of postoperative endophthalmitis. Nursing staff posted at the daycare or inpatient ward should look for preoperative risk factors such as blepharitis, dacryocystitis, open wound, etc. before shifting the case to the operating room. Nursing staff plays a vital role in monitoring the patient, charting the vital parameters, and reporting the issues to the treating physician. Certain cases with fulminant endophthalmitis might require evisceration/ enucleation; hence pre-surgical counseling of patients by a psychiatrist helps to reduce the morbidity. Cases with endogenous endophthalmitis have systemic comorbidities such as invasive aspergillosis or chronic renal failure with prolonged catheterization, etc., and hence may not primarily present to the ophthalmologist with ocular complaints. Therefore specialists other than an ophthalmologist must be aware of such an entity and promptly refer such cases to improve outcomes.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Durand ML. Endophthalmitis. Clinical microbiology and infection : the official publication of the European Society of Clinical Microbiology and Infectious Diseases. 2013 Mar:19(3):227-34. doi: 10.1111/1469-0691.12118. Epub [PubMed PMID: 23438028]
Sunaric-Mégevand G, Pournaras CJ. Current approach to postoperative endophthalmitis. The British journal of ophthalmology. 1997 Nov:81(11):1006-15 [PubMed PMID: 9505828]
Gentile RC, Shukla S, Shah M, Ritterband DC, Engelbert M, Davis A, Hu DN. Microbiological spectrum and antibiotic sensitivity in endophthalmitis: a 25-year review. Ophthalmology. 2014 Aug:121(8):1634-42. doi: 10.1016/j.ophtha.2014.02.001. Epub 2014 Apr 2 [PubMed PMID: 24702755]
Level 2 (mid-level) evidenceJonas JB, Knorr HL, Budde WM. Prognostic factors in ocular injuries caused by intraocular or retrobulbar foreign bodies. Ophthalmology. 2000 May:107(5):823-8 [PubMed PMID: 10811069]
Level 2 (mid-level) evidenceVerma L, Chakravarti A. Prevention and management of postoperative endophthalmitis: A case-based approach. Indian journal of ophthalmology. 2017 Dec:65(12):1396-1402. doi: 10.4103/ijo.IJO_1058_17. Epub [PubMed PMID: 29208820]
Level 3 (low-level) evidenceMaalouf F, Abdulaal M, Hamam RN. Chronic postoperative endophthalmitis: a review of clinical characteristics, microbiology, treatment strategies, and outcomes. International journal of inflammation. 2012:2012():313248. doi: 10.1155/2012/313248. Epub 2012 Feb 22 [PubMed PMID: 22550607]
Jacobs DJ, Leng T, Flynn HW Jr, Shi W, Miller D, Gedde SJ. Delayed-onset bleb-associated endophthalmitis: presentation and outcome by culture result. Clinical ophthalmology (Auckland, N.Z.). 2011:5():739-44. doi: 10.2147/OPTH.S17975. Epub 2011 Jun 2 [PubMed PMID: 21691583]
Gedde SJ, Scott IU, Tabandeh H, Luu KK, Budenz DL, Greenfield DS, Flynn HW Jr. Late endophthalmitis associated with glaucoma drainage implants. Ophthalmology. 2001 Jul:108(7):1323-7 [PubMed PMID: 11425695]
Level 3 (low-level) evidenceMcCannel CA. Meta-analysis of endophthalmitis after intravitreal injection of anti-vascular endothelial growth factor agents: causative organisms and possible prevention strategies. Retina (Philadelphia, Pa.). 2011 Apr:31(4):654-61. doi: 10.1097/IAE.0b013e31820a67e4. Epub [PubMed PMID: 21330939]
Level 1 (high-level) evidenceChhablani J, Nayak S, Jindal A, Motukupally SR, Mathai A, Jalali S, Pappuru RR, Sharma S, Das T, Flynn HW Jr, Pathengay A. Scleral buckle infections: microbiological spectrum and antimicrobial susceptibility. Journal of ophthalmic inflammation and infection. 2013 Dec 13:3(1):67. doi: 10.1186/1869-5760-3-67. Epub 2013 Dec 13 [PubMed PMID: 24330530]
Rosenberg KD, Flynn HW Jr, Alfonso EC, Miller D. Fusarium endophthalmitis following keratitis associated with contact lenses. Ophthalmic surgery, lasers & imaging : the official journal of the International Society for Imaging in the Eye. 2006 Jul-Aug:37(4):310-3. doi: 10.3928/15428877-20060701-08. Epub [PubMed PMID: 16898392]
Level 3 (low-level) evidenceMulhern MG, Condon PI, O'Keefe M. Endophthalmitis after astigmatic myopic laser in situ keratomileusis. Journal of cataract and refractive surgery. 1997 Jul-Aug:23(6):948-50 [PubMed PMID: 9292683]
Level 3 (low-level) evidenceWong JS, Chan TK, Lee HM, Chee SP. Endogenous bacterial endophthalmitis: an east Asian experience and a reappraisal of a severe ocular affliction. Ophthalmology. 2000 Aug:107(8):1483-91 [PubMed PMID: 10919895]
Level 2 (mid-level) evidenceChawla R, Venkatesh P, Garg SP, Tripathy K. Bilateral metastatic endophthalmitis due to Pseudomonas aeruginosa after vaginal delivery. Journal of obstetrics and gynaecology : the journal of the Institute of Obstetrics and Gynaecology. 2016 Nov:36(8):1016-1017 [PubMed PMID: 27750450]
Srujana D, Singh R, Tripathy K. Comment on "Surgical management of fungal endophthalmitis resulting from fungal keratitis". International journal of ophthalmology. 2017:10(9):1479-1480. doi: 10.18240/ijo.2017.09.24. Epub 2017 Sep 18 [PubMed PMID: 28944212]
Level 3 (low-level) evidenceSafneck JR. Endophthalmitis: A review of recent trends. Saudi journal of ophthalmology : official journal of the Saudi Ophthalmological Society. 2012 Apr:26(2):181-9. doi: 10.1016/j.sjopt.2012.02.011. Epub 2012 Mar 3 [PubMed PMID: 23960990]
Pershing S, Lum F, Hsu S, Kelly S, Chiang MF, Rich WL 3rd, Parke DW 2nd. Endophthalmitis after Cataract Surgery in the United States: A Report from the Intelligent Research in Sight Registry, 2013-2017. Ophthalmology. 2020 Feb:127(2):151-158. doi: 10.1016/j.ophtha.2019.08.026. Epub 2019 Aug 28 [PubMed PMID: 31611015]
Xu K, Chin EK, Bennett SR, Williams DF, Ryan EH, Dev S, Mittra RA, Quiram PA, Davies JB, Parke DW 3rd, Johnson JB, Cantrill HL, Almeida DRP. Endophthalmitis after Intravitreal Injection of Vascular Endothelial Growth Factor Inhibitors: Management and Visual Outcomes. Ophthalmology. 2018 Aug:125(8):1279-1286. doi: 10.1016/j.ophtha.2018.01.022. Epub 2018 Feb 21 [PubMed PMID: 29477689]
Thompson JT, Parver LM, Enger CL, Mieler WF, Liggett PE. Infectious endophthalmitis after penetrating injuries with retained intraocular foreign bodies. National Eye Trauma System. Ophthalmology. 1993 Oct:100(10):1468-74 [PubMed PMID: 8414406]
Thompson WS, Rubsamen PE, Flynn HW Jr, Schiffman J, Cousins SW. Endophthalmitis after penetrating trauma. Risk factors and visual acuity outcomes. Ophthalmology. 1995 Nov:102(11):1696-701 [PubMed PMID: 9098264]
Level 2 (mid-level) evidenceJabbarvand M, Hashemian H, Khodaparast M, Jouhari M, Tabatabaei A, Rezaei S. Endophthalmitis Occurring after Cataract Surgery: Outcomes of More Than 480 000 Cataract Surgeries, Epidemiologic Features, and Risk Factors. Ophthalmology. 2016 Feb:123(2):295-301. doi: 10.1016/j.ophtha.2015.08.023. Epub 2015 Dec 15 [PubMed PMID: 26704882]
Yao K, Zhu Y, Zhu Z, Wu J, Liu Y, Lu Y, Hao Y, Bao Y, Ye J, Huang Y, Li Z, Shentu X, Yu Y. The incidence of postoperative endophthalmitis after cataract surgery in China: a multicenter investigation of 2006-2011. The British journal of ophthalmology. 2013 Oct:97(10):1312-7. doi: 10.1136/bjophthalmol-2013-303282. Epub 2013 Jul 24 [PubMed PMID: 23884695]
Level 2 (mid-level) evidenceMithal K, Mathai A, Pathengay A, Jalali S, Relhan N, Motukupally SR, Sharma S, Das T. Endophthalmitis following intravitreal anti-VEGF injections in ambulatory surgical centre facility: incidence, management and outcome. The British journal of ophthalmology. 2013 Dec:97(12):1609-12. doi: 10.1136/bjophthalmol-2013-303222. Epub 2013 Sep 24 [PubMed PMID: 24064940]
Level 3 (low-level) evidenceFalavarjani KG, Modarres M, Hashemi M, Parvaresh MM, Naseripour M, Zare-Moghaddam A, Nekoozadeh S. Incidence of acute endophthalmitis after intravitreal bevacizumab injection in a single clinical center. Retina (Philadelphia, Pa.). 2013 May:33(5):971-4. doi: 10.1097/IAE.0b013e31826f0675. Epub [PubMed PMID: 23400076]
Level 2 (mid-level) evidenceAaberg TM Jr, Flynn HW Jr, Schiffman J, Newton J. Nosocomial acute-onset postoperative endophthalmitis survey. A 10-year review of incidence and outcomes. Ophthalmology. 1998 Jun:105(6):1004-10 [PubMed PMID: 9627649]
Level 2 (mid-level) evidenceWolner B, Liebmann JM, Sassani JW, Ritch R, Speaker M, Marmor M. Late bleb-related endophthalmitis after trabeculectomy with adjunctive 5-fluorouracil. Ophthalmology. 1991 Jul:98(7):1053-60 [PubMed PMID: 1891213]
Level 2 (mid-level) evidenceKumar A, Tripathy K, Chawla R. Intraocular use of bevacizumab in India: An issue resolved? The National medical journal of India. 2017 Nov-Dec:30(6):345-347. doi: 10.4103/0970-258X.239079. Epub [PubMed PMID: 30117450]
Pilli S, Kotsolis A, Spaide RF, Slakter J, Freund KB, Sorenson J, Klancnik J, Cooney M. Endophthalmitis associated with intravitreal anti-vascular endothelial growth factor therapy injections in an office setting. American journal of ophthalmology. 2008 May:145(5):879-82. doi: 10.1016/j.ajo.2007.12.036. Epub 2008 Mar 10 [PubMed PMID: 18329624]
Level 3 (low-level) evidenceKhan P,Khan L,Mondal P, Cluster endophthalmitis following multiple intravitreal bevacizumab injections from a single use vial. Indian journal of ophthalmology. 2016 Sep [PubMed PMID: 27853027]
Gonzalez S, Rosenfeld PJ, Stewart MW, Brown J, Murphy SP. Avastin doesn't blind people, people blind people. American journal of ophthalmology. 2012 Feb:153(2):196-203.e1. doi: 10.1016/j.ajo.2011.11.023. Epub [PubMed PMID: 22264942]
Carlson AN, Koch DD. Endophthalmitis following Nd:YAG laser posterior capsulotomy. Ophthalmic surgery. 1988 Mar:19(3):168-70 [PubMed PMID: 3258419]
Level 3 (low-level) evidenceCallegan MC, Jett BD, Hancock LE, Gilmore MS. Role of hemolysin BL in the pathogenesis of extraintestinal Bacillus cereus infection assessed in an endophthalmitis model. Infection and immunity. 1999 Jul:67(7):3357-66 [PubMed PMID: 10377113]
Level 3 (low-level) evidenceJett BD, Jensen HG, Nordquist RE, Gilmore MS. Contribution of the pAD1-encoded cytolysin to the severity of experimental Enterococcus faecalis endophthalmitis. Infection and immunity. 1992 Jun:60(6):2445-52 [PubMed PMID: 1587612]
Level 3 (low-level) evidenceNg EW, Costa JR, Samiy N, Ruoff KL, Connolly E, Cousins FV, D'Amico DJ. Contribution of pneumolysin and autolysin to the pathogenesis of experimental pneumococcal endophthalmitis. Retina (Philadelphia, Pa.). 2002 Oct:22(5):622-32 [PubMed PMID: 12441729]
Level 3 (low-level) evidenceHunt JJ, Astley R, Wheatley N, Wang JT, Callegan MC. TLR4 contributes to the host response to Klebsiella intraocular infection. Current eye research. 2014 Aug:39(8):790-802. doi: 10.3109/02713683.2014.883412. Epub 2014 Mar 3 [PubMed PMID: 24588082]
Level 3 (low-level) evidenceCallegan MC, Booth MC, Jett BD, Gilmore MS. Pathogenesis of gram-positive bacterial endophthalmitis. Infection and immunity. 1999 Jul:67(7):3348-56 [PubMed PMID: 10377112]
Level 3 (low-level) evidenceCallegan MC, Kane ST, Cochran DC, Novosad B, Gilmore MS, Gominet M, Lereclus D. Bacillus endophthalmitis: roles of bacterial toxins and motility during infection. Investigative ophthalmology & visual science. 2005 Sep:46(9):3233-8 [PubMed PMID: 16123424]
Level 3 (low-level) evidencePetropoulos IK, Vantzou CV, Lamari FN, Karamanos NK, Anastassiou ED, Pharmakakis NM. Expression of TNF-alpha, IL-1beta, and IFN-gamma in Staphylococcus epidermidis slime-positive experimental endophthalmitis is closely related to clinical inflammatory scores. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2006 Oct:244(10):1322-8 [PubMed PMID: 16544114]
Level 3 (low-level) evidenceScott IU, Flynn HW Jr, Dev S, Shaikh S, Mittra RA, Arevalo JF, Kychenthal A, Acar N. Endophthalmitis after 25-gauge and 20-gauge pars plana vitrectomy: incidence and outcomes. Retina (Philadelphia, Pa.). 2008 Jan:28(1):138-42. doi: 10.1097/IAE.0b013e31815e9313. Epub [PubMed PMID: 18185150]
. Results of the Endophthalmitis Vitrectomy Study. A randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Endophthalmitis Vitrectomy Study Group. Archives of ophthalmology (Chicago, Ill. : 1960). 1995 Dec:113(12):1479-96 [PubMed PMID: 7487614]
Level 1 (high-level) evidenceEndophthalmitis Study Group, European Society of Cataract & Refractive Surgeons. Prophylaxis of postoperative endophthalmitis following cataract surgery: results of the ESCRS multicenter study and identification of risk factors. Journal of cataract and refractive surgery. 2007 Jun:33(6):978-88 [PubMed PMID: 17531690]
Level 1 (high-level) evidenceMiller JJ, Scott IU, Flynn HW Jr, Smiddy WE, Murray TG, Berrocal A, Miller D. Endophthalmitis caused by Bacillus species. American journal of ophthalmology. 2008 May:145(5):883-8. doi: 10.1016/j.ajo.2007.12.026. Epub 2008 Mar 4 [PubMed PMID: 18295182]
Level 2 (mid-level) evidenceBhagat N, Nagori S, Zarbin M. Post-traumatic Infectious Endophthalmitis. Survey of ophthalmology. 2011 May-Jun:56(3):214-51. doi: 10.1016/j.survophthal.2010.09.002. Epub 2011 Mar 12 [PubMed PMID: 21397289]
Level 3 (low-level) evidenceDeramo VA, Ting TD. Treatment of Propionibacterium acnes endophthalmitis. Current opinion in ophthalmology. 2001 Jun:12(3):225-9 [PubMed PMID: 11389352]
Level 3 (low-level) evidenceSamson CM, Foster CS. Chronic postoperative endophthalmitis. International ophthalmology clinics. 2000 Winter:40(1):57-67 [PubMed PMID: 10713914]
Venkatesh P, Temkar S, Tripathy K, Chawla R. Intralesional antibiotic injection using 41G needle for the management of subretinal abscess in endogenous endophthalmitis. International journal of retina and vitreous. 2016:2():17 [PubMed PMID: 27847635]
Sridhar J, Flynn HW Jr, Kuriyan AE, Miller D, Albini T. Endogenous fungal endophthalmitis: risk factors, clinical features, and treatment outcomes in mold and yeast infections. Journal of ophthalmic inflammation and infection. 2013 Sep 20:3(1):60. doi: 10.1186/1869-5760-3-60. Epub 2013 Sep 20 [PubMed PMID: 24053550]
Tripathy K, Chawla R, Venkatesh P, Sharma YR, Vohra R. Ultrawide Field Imaging in Uveitic Non-dilating Pupils. Journal of ophthalmic & vision research. 2017 Apr-Jun:12(2):232-233. doi: 10.4103/2008-322X.205360. Epub [PubMed PMID: 28540019]
Tripathy K, Chawla R, Vohra R. Evaluation of the fundus in poorly dilating diabetic pupils using ultrawide field imaging. Clinical & experimental optometry. 2017 Nov:100(6):735-736. doi: 10.1111/cxo.12484. Epub 2016 Oct 5 [PubMed PMID: 27704602]
Barza M, Pavan PR, Doft BH, Wisniewski SR, Wilson LA, Han DP, Kelsey SF. Evaluation of microbiological diagnostic techniques in postoperative endophthalmitis in the Endophthalmitis Vitrectomy Study. Archives of ophthalmology (Chicago, Ill. : 1960). 1997 Sep:115(9):1142-50 [PubMed PMID: 9298055]
Level 1 (high-level) evidenceCornut PL, Boisset S, Romanet JP, Maurin M, Carricajo A, Benito Y, Vandenesch F, Chiquet C. Principles and applications of molecular biology techniques for the microbiological diagnosis of acute post-operative endophthalmitis. Survey of ophthalmology. 2014 May-Jun:59(3):286-303. doi: 10.1016/j.survophthal.2013.08.002. Epub 2013 Dec 18 [PubMed PMID: 24359808]
Level 3 (low-level) evidenceLott MN, Fuller JJ, Hancock HA, Singh J, Singh H, McGwin G Jr, Marcus DM. Vitreal penetration of oral moxifloxacin in humans. Retina (Philadelphia, Pa.). 2008 Mar:28(3):473-6. doi: 10.1097/IAE.0b013e31814fb0ed. Epub [PubMed PMID: 18327141]
Brockhaus L, Goldblum D, Eggenschwiler L, Zimmerli S, Marzolini C. Revisiting systemic treatment of bacterial endophthalmitis: a review of intravitreal penetration of systemic antibiotics. Clinical microbiology and infection : the official publication of the European Society of Clinical Microbiology and Infectious Diseases. 2019 Nov:25(11):1364-1369. doi: 10.1016/j.cmi.2019.01.017. Epub 2019 Feb 14 [PubMed PMID: 30771529]
Jackson TL, Eykyn SJ, Graham EM, Stanford MR. Endogenous bacterial endophthalmitis: a 17-year prospective series and review of 267 reported cases. Survey of ophthalmology. 2003 Jul-Aug:48(4):403-23 [PubMed PMID: 12850229]
Level 3 (low-level) evidenceShirodkar AR, Pathengay A, Flynn HW Jr. Intravitreal gentamicin-induced macular infarction: SD-OCT features. Ophthalmic surgery, lasers & imaging : the official journal of the International Society for Imaging in the Eye. 2011 Aug 4:42 Online():e67-70. doi: 10.3928/15428877-20110728-01. Epub 2011 Aug 4 [PubMed PMID: 21805955]
Level 3 (low-level) evidenceLuaces-Rodríguez A, González-Barcia M, Blanco-Teijeiro MJ, Gil-Martínez M, Gonzalez F, Gómez-Ulla F, Lamas MJ, Otero-Espinar FJ, Fernández-Ferreiro A. Review of Intraocular Pharmacokinetics of Anti-Infectives Commonly Used in the Treatment of Infectious Endophthalmitis. Pharmaceutics. 2018 May 29:10(2):. doi: 10.3390/pharmaceutics10020066. Epub 2018 May 29 [PubMed PMID: 29844284]
Pathengay A, Mathai A, Shah GY, Ambatipudi S. Intravitreal piperacillin/tazobactam in the management of multidrug-resistant Pseudomonas aeruginosa endophthalmitis. Journal of cataract and refractive surgery. 2010 Dec:36(12):2210-1. doi: 10.1016/j.jcrs.2010.09.013. Epub [PubMed PMID: 21111328]
Level 3 (low-level) evidenceLoewenstein A, Zemel E, Lazar M, Perlman I. Drug-induced retinal toxicity in albino rabbits: the effects of imipenem and aztreonam. Investigative ophthalmology & visual science. 1993 Nov:34(12):3466-76 [PubMed PMID: 8225881]
Level 3 (low-level) evidenceBarza M, Kane A, Baum J. Pharmacokinetics of intravitreal carbenicillin, cefazolin, and gentamicin in rhesus monkeys. Investigative ophthalmology & visual science. 1983 Dec:24(12):1602-6 [PubMed PMID: 6654640]
Level 3 (low-level) evidenceHeigle TJ,Peyman GA, Retinal toxicity of intravitreal ticarcillin. Ophthalmic surgery. 1990 Aug [PubMed PMID: 2234805]
Level 3 (low-level) evidenceRadhika M, Mithal K, Bawdekar A, Dave V, Jindal A, Relhan N, Albini T, Pathengay A, Flynn HW. Pharmacokinetics of intravitreal antibiotics in endophthalmitis. Journal of ophthalmic inflammation and infection. 2014:4():22. doi: 10.1186/s12348-014-0022-z. Epub 2014 Sep 10 [PubMed PMID: 25667683]
Jacobs DJ, Grube TJ, Flynn HW Jr, Greven CM, Pathengay A, Miller D, Sanke RF, Thorman J. Intravitreal moxifloxacin in the management of Ochrobactrum intermedium endophthalmitis due to metallic intraocular foreign body. Clinical ophthalmology (Auckland, N.Z.). 2013:7():1727-30. doi: 10.2147/OPTH.S44212. Epub 2013 Aug 27 [PubMed PMID: 24039392]
Level 3 (low-level) evidenceSamant P, Ramugade S. Successful use of intravitreal and systemic colistin in treating multidrug resistant Pseudomonas aeruginosa post-operative endophthalmitis. Indian journal of ophthalmology. 2014 Dec:62(12):1167-70. doi: 10.4103/0301-4738.126991. Epub [PubMed PMID: 25579363]
Kuhn F, Gini G. Ten years after... are findings of the Endophthalmitis Vitrectomy Study still relevant today? Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2005 Dec:243(12):1197-9 [PubMed PMID: 16136321]
Bui DK, Carvounis PE. Evidence for and against intravitreous corticosteroids in addition to intravitreous antibiotics for acute endophthalmitis. International ophthalmology clinics. 2014 Spring:54(2):215-24. doi: 10.1097/IIO.0000000000000020. Epub [PubMed PMID: 24613894]
Das T, Dogra MR, Gopal L, Jalali S, Kumar A, Malpani A, Natarajan S, Rajeev B, Sharma S. Postsurgical endophthalmitis: diagnosis and management. Indian journal of ophthalmology. 1995 Sep:43(3):103-16 [PubMed PMID: 8822484]
Ciulla TA,Starr MB,Masket S, Bacterial endophthalmitis prophylaxis for cataract surgery: an evidence-based update. Ophthalmology. 2002 Jan [PubMed PMID: 11772573]
Level 1 (high-level) evidenceBarry P, Seal DV, Gettinby G, Lees F, Peterson M, Revie CW, ESCRS Endophthalmitis Study Group. ESCRS study of prophylaxis of postoperative endophthalmitis after cataract surgery: Preliminary report of principal results from a European multicenter study. Journal of cataract and refractive surgery. 2006 Mar:32(3):407-10 [PubMed PMID: 16631047]
Level 1 (high-level) evidenceHaripriya A, Chang DF, Namburar S, Smita A, Ravindran RD. Efficacy of Intracameral Moxifloxacin Endophthalmitis Prophylaxis at Aravind Eye Hospital. Ophthalmology. 2016 Feb:123(2):302-308. doi: 10.1016/j.ophtha.2015.09.037. Epub 2015 Oct 30 [PubMed PMID: 26522705]
Haripriya A, Chang DF, Ravindran RD. Endophthalmitis reduction with intracameral moxifloxacin in eyes with and without surgical complications: Results from 2 million consecutive cataract surgeries. Journal of cataract and refractive surgery. 2019 Sep:45(9):1226-1233. doi: 10.1016/j.jcrs.2019.04.018. Epub 2019 Jul 29 [PubMed PMID: 31371152]
Kim EA, Law SK, Coleman AL, Nouri-Mahdavi K, Giaconi JA, Yu F, Lee JW, Caprioli J. Long-Term Bleb-Related Infections After Trabeculectomy: Incidence, Risk Factors, and Influence of Bleb Revision. American journal of ophthalmology. 2015 Jun:159(6):1082-91. doi: 10.1016/j.ajo.2015.03.001. Epub 2015 Mar 5 [PubMed PMID: 25748577]
Level 2 (mid-level) evidenceWitkin AJ, Shah AR, Engstrom RE, Kron-Gray MM, Baumal CR, Johnson MW, Witkin DI, Leung J, Albini TA, Moshfeghi AA, Batlle IR, Sobrin L, Eliott D. Postoperative Hemorrhagic Occlusive Retinal Vasculitis: Expanding the Clinical Spectrum and Possible Association with Vancomycin. Ophthalmology. 2015 Jul:122(7):1438-51. doi: 10.1016/j.ophtha.2015.03.016. Epub 2015 Apr 15 [PubMed PMID: 25886796]
Brynskov T, Kemp H, Sørensen TL. No cases of endophthalmitis after 20,293 intravitreal injections in an operating room setting. Retina (Philadelphia, Pa.). 2014 May:34(5):951-7. doi: 10.1097/IAE.0000000000000071. Epub [PubMed PMID: 24317292]
Level 3 (low-level) evidenceGarg SJ, Dollin M, Hsu J, Storey P, Vander JF. Effect of a Strict 'No-Talking' Policy During Intravitreal Injection on Post-Injection Endophthalmitis. Ophthalmic surgery, lasers & imaging retina. 2015 Nov-Dec:46(10):1028-34. doi: 10.3928/23258160-20151027-07. Epub [PubMed PMID: 26599245]
Narang S, Gupta V, Gupta A, Dogra MR, Pandav SS, Das S. Role of prophylactic intravitreal antibiotics in open globe injuries. Indian journal of ophthalmology. 2003 Mar:51(1):39-44 [PubMed PMID: 12701861]
Level 1 (high-level) evidenceSoheilian M, Rafati N, Mohebbi MR, Yazdani S, Habibabadi HF, Feghhi M, Shahriary HA, Eslamipour J, Piri N, Peyman GA, Traumatic Endophthalmitis Trial Research Group. Prophylaxis of acute posttraumatic bacterial endophthalmitis: a multicenter, randomized clinical trial of intraocular antibiotic injection, report 2. Archives of ophthalmology (Chicago, Ill. : 1960). 2007 Apr:125(4):460-5 [PubMed PMID: 17420365]
Level 1 (high-level) evidencePark CY, Lee JK, Chuck RS. Toxic anterior segment syndrome-an updated review. BMC ophthalmology. 2018 Oct 25:18(1):276. doi: 10.1186/s12886-018-0939-3. Epub 2018 Oct 25 [PubMed PMID: 30359246]
Driebe WT Jr, Mandelbaum S, Forster RK, Schwartz LK, Culbertson WW. Pseudophakic endophthalmitis. Diagnosis and management. Ophthalmology. 1986 Apr:93(4):442-8 [PubMed PMID: 3486397]
Yamamoto T, Kuwayama Y, Nomura E, Tanihara H, Mori K, Japan Glaucoma Society Survey of Bleb-related Infection. Changes in visual acuity and intra-ocular pressure following bleb-related infection: the Japan Glaucoma Society Survey of Bleb-related Infection Report 2. Acta ophthalmologica. 2013 Sep:91(6):e420-6. doi: 10.1111/aos.12079. Epub 2013 Jul 2 [PubMed PMID: 23819592]
Level 3 (low-level) evidenceShen X, Xu G. Vitrectomy for endogenous fungal endophthalmitis. Ocular immunology and inflammation. 2009 May-Jun:17(3):148-52. doi: 10.1080/09273940802689396. Epub [PubMed PMID: 19585356]
Level 2 (mid-level) evidenceDas T, Choudhury K, Sharma S, Jalali S, Nuthethi R, Endophthalmitis Research Group. Clinical profile and outcome in Bacillus endophthalmitis. Ophthalmology. 2001 Oct:108(10):1819-25 [PubMed PMID: 11581055]
Level 2 (mid-level) evidenceIrvine WD, Flynn HW Jr, Miller D, Pflugfelder SC. Endophthalmitis caused by gram-negative organisms. Archives of ophthalmology (Chicago, Ill. : 1960). 1992 Oct:110(10):1450-4 [PubMed PMID: 1417545]
Level 2 (mid-level) evidenceChakrabarti A, Shivaprakash MR, Singh R, Tarai B, George VK, Fomda BA, Gupta A. Fungal endophthalmitis: fourteen years' experience from a center in India. Retina (Philadelphia, Pa.). 2008 Nov-Dec:28(10):1400-7 [PubMed PMID: 19009680]
Level 2 (mid-level) evidenceNicoară SD, Irimescu I, Călinici T, Cristian C. Outcome and Prognostic Factors for Traumatic Endophthalmitis over a 5-Year Period. Journal of ophthalmology. 2014:2014():747015. doi: 10.1155/2014/747015. Epub 2014 Sep 15 [PubMed PMID: 25302113]
Lu X, Ng DS, Zheng K, Peng K, Jin C, Xia H, Chen W, Chen H. Risk factors for endophthalmitis requiring evisceration or enucleation. Scientific reports. 2016 Jun 15:6():28100. doi: 10.1038/srep28100. Epub 2016 Jun 15 [PubMed PMID: 27302573]