Introduction
The obturator nerve arises from the lumbar plexus and provides sensory and motor innervation to the thigh. This nerve provides motor innervation to the medial compartment of the thigh and as a result, is essential to the adduction of the thigh. The nerve provides sensory innervation to the medial upper thigh and provides articular branches to the hip and knee. The obturator nerve is clinically relevant in certain pathologic conditions and procedures involving the hip and knee. Additionally, its location in the pelvis and upper thigh, as well as its origin in the lumbar plexus, make the obturator nerve a relevant anatomic structure in several clinical settings.[1]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
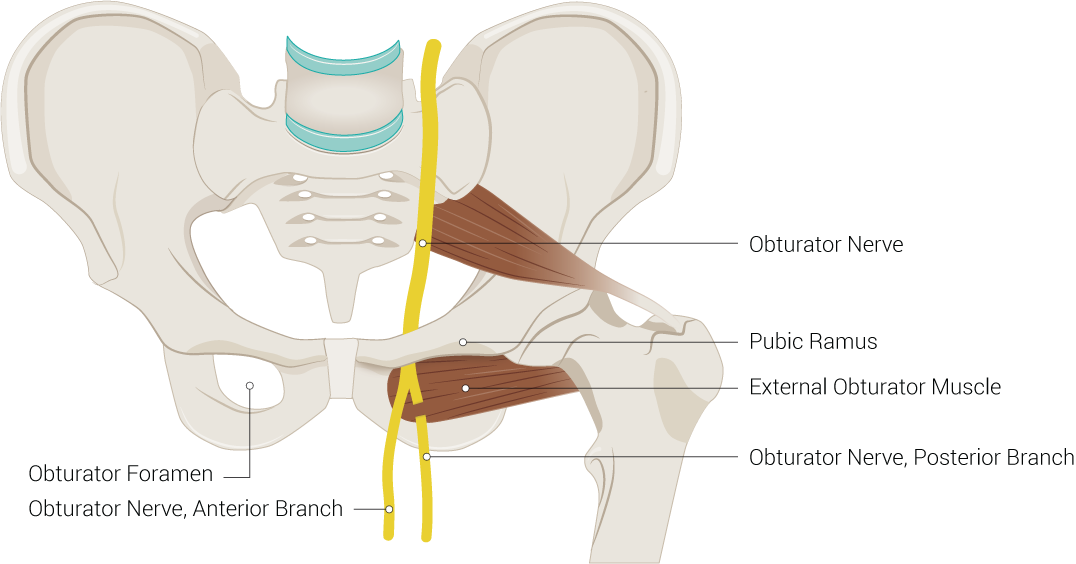
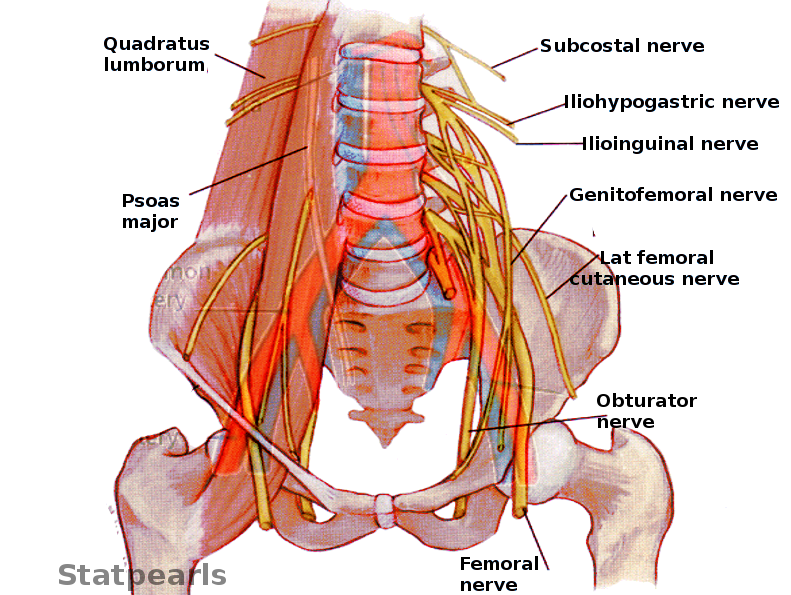
The obturator nerve arises from the second through fourth lumbar plexus nerve roots. These roots form the obturator nerve, which travels along the iliopectineal line and descends through the muscle fibers of the psoas major muscle. The nerve emerges from the medial border of the psoas major near the pelvic brim. Then, the obturator nerve runs posterior to the common iliac arteries and continues on the lateral side of the internal iliac artery and distal segment of the ureter as it descends towards the obturator canal. In the lower pelvis, it courses anterior to the obturator vessels. The nerve exits the pelvis en route to the medial thigh by passing through the obturator canal. Near the obturator canal, it divides into the anterior and posterior divisions. The anterior branch of the obturator nerve continues its course between the adductor longus and adductor brevis and eventually terminates as the cutaneous branch of the obturator nerve. The posterior branch travels between the adductor brevis and the adductor magnus.[1][2][3]
The obturator nerve provides sensory innervation to the skin of the medial region of the upper thigh via the terminal branch of the anterior division. It also provides motor innervation to the adductor muscles of the lower leg: the adductor longus, external obturator, adductor magnus, adductor brevis, and gracilis. Specifically, the anterior branch of the obturator nerve innervates the adductor brevis, adductor longus, gracilis, and in rare circumstances, the pectineus. The posterior branch of the obturator nerve provides innervation to the adductor magnus, adductor brevis, and occasionally the adductor longus and obturator externus. Furthermore, the obturator nerve provides articular branches to the hip and knee joints. In terms of cutaneous innervation, the anterior branch of the obturator nerve supplies the medial thigh, and just above the medial knee.[3]
Embryology
The peripheral nervous system arises from neuroepithelial cells. These neuroepithelial cells migrate from the pia mater to the periphery, differentiating into neurons, glioblasts, and ependymal cells. These cells facilitate the growth of structures such as the lumbar plexus and the eventual obturator nerve.[1]
Nerves
The obturator nerve divides into anterior and posterior divisions of the obturator nerve. These divisions both provide skeletal musculature innervation, and the anterior division terminates as the cutaneous branch of the obturator nerve.
Physiologic Variants
The location of the bifurcation of the obturator nerve is variable between sites within the pelvic cavity, obturator canal, or medial thigh. Typically, the obturator nerve enters the thigh after passing through the obturator canal and divides into the anterior and posterior divisions. However, the bifurcation of the obturator nerve can be within the obturator canal (51.78%), in the thigh (25%), or intrapelvic (23.22%). Additionally, the anterior branch can form anywhere from two to four branches, with three branches being the most predominant. In comparison, the posterior branch can form one to four subdivisions, with two divisions being the dominant variant. The articular branches of the obturator nerve demonstrated nine different branching patterns. In terms of cutaneous innervation, research has shown that the obturator nerve provides innervation to the skin surface of the medial thigh, although, has been shown to provide no cutaneous innervation in more than 50% of cases.[4][5]
Surgical Considerations
The obturator nerve is at risk of injury during surgeries that require pelvic dissection and access. In the case of repair of pelvic organ prolapse, the obturator nerve and ureter are particularly at risk of injury, regardless of the surgical approach. The obturator nerve may also suffer an injury during laparoscopic pelvic procedures, such as laparoscopic lymphadenectomy. Furthermore, the obturator nerve can get injured in transvaginal mid-urethral sling placements.[6][7][8]
The obturator nerve has particular utility in transurethral resection of bladder tumor (TURBT), which is common in the treatment of bladder wall masses. Because of the obturator nerve's proximity to the inferolateral wall of the bladder, bladder neck, and prostatic urethra, electrical stimulation caused by tumor resection may cause sudden adductor contraction or "adductor jerk." This sudden thigh movement may cause perforation of the bladder and extravesical seeding of the tumor. Additionally, the adductor jerk may result in damage to the obturator artery. By performing an obturator nerve block with a local anesthetic, the adductor jerk can be eliminated and enable a safe and effective TURBT.[9]
Clinical Significance
Because of the obturator nerve's innervation of the thigh adductor muscles, blocking the obturator nerve has clinical utility. As described previously, the obturator nerve block (ONB) can help to immobilize the adductor musculature during surgery. Furthermore, due to the obturator nerve's articular branches to the hip and knee, ONB can provide analgesia for hip and knee surgeries, improve chronic groin/thigh pain, and treat adductor spasticity. As a result, conditions such as total knee replacement, hip fracture, traumatic brain injury, and multiple sclerosis can benefit from ONB. If a simple ONB is not effective in providing analgesia, some studies have suggested utility in percutaneous radiofrequency lesioning of the articular branches of the obturator nerve in easing hip joint pain.[3][10]
The obturator nerve is relevant in multiple pathologic conditions. Obturator hernias typically occur in elderly, emaciated women or patients with elevated intra-abdominal pressure due to ascites, chronic cough, or COPD. In an obturator hernia, the hernia sac enters the obturator foramen and follows the course of the obturator canal, obstructing the small bowel. The clinical course is characterized by acute small bowel obstruction and pain in the medial aspect of the upper thigh due to compression of the obturator nerve. Computed tomography (CT) is the imaging modality with the highest sensitivity and accuracy for the timely diagnosis of an obturator hernia. Meanwhile, the definitive treatment is a surgical fixation of the hernia. If the bowel is ischemic, bowel resection and/or a colostomy may be required dependent upon the intraoperative findings. In addition to older women, obturator hernias may also occur during pregnancy due to relaxation of the pelvic peritoneum and development of a wider and more horizontal obturator canal.[11]
Just as the obturator nerve can become compressed by a hernia, the obturator nerve can become compressed by fascia or other tissue in the pelvis. Specifically, the nerve can become entrapped at the exit of the obturator canal or more distally by fascia. Entrapment of the obturator nerve causes exercise-induced medial thigh pain, typically in athletes. Hip abduction and extension aggravate the pain, whereas resisted adduction does not elicit pain. Conservative treatment has not been the target of much research, but stretching and strengthening exercises, cognitive behavioral education, neural gliding, and manual therapy may have utility in easing symptoms. Neurolysis or neurectomy may merit consideration if symptoms are refractory to treatment.[12][13]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Singh O, Al Khalili Y. Anatomy, Back, Lumbar Plexus. StatPearls. 2023 Jan:(): [PubMed PMID: 31424721]
Khan IA, Bordoni B, Varacallo M. Anatomy, Bony Pelvis and Lower Limb: Thigh Gracilis Muscle. StatPearls. 2023 Jan:(): [PubMed PMID: 30855817]
Yoshida T, Nakamoto T, Kamibayashi T. Ultrasound-Guided Obturator Nerve Block: A Focused Review on Anatomy and Updated Techniques. BioMed research international. 2017:2017():7023750. doi: 10.1155/2017/7023750. Epub 2017 Feb 9 [PubMed PMID: 28280738]
Anagnostopoulou S, Kostopanagiotou G, Paraskeuopoulos T, Chantzi C, Lolis E, Saranteas T. Anatomic variations of the obturator nerve in the inguinal region: implications in conventional and ultrasound regional anesthesia techniques. Regional anesthesia and pain medicine. 2009 Jan-Feb:34(1):33-9. doi: 10.1097/AAP.0b013e3181933b51. Epub [PubMed PMID: 19258986]
Bouaziz H, Vial F, Jochum D, Macalou D, Heck M, Meuret P, Braun M, Laxenaire MC. An evaluation of the cutaneous distribution after obturator nerve block. Anesthesia and analgesia. 2002 Feb:94(2):445-9, table of contents [PubMed PMID: 11812716]
De Decker A, Fergusson R, Ondruschka B, Hammer N, Zwirner J. Anatomical structures at risk using different approaches for sacrospinous ligament fixation. Clinical anatomy (New York, N.Y.). 2020 May:33(4):522-529. doi: 10.1002/ca.23404. Epub 2019 May 29 [PubMed PMID: 31087424]
Menderes G, Vilardo N, Schwab CL, Azodi M. Incidental injury and repair of obturator nerve during laparoscopic pelvic lymphadenectomy. Gynecologic oncology. 2016 Jul:142(1):208. doi: 10.1016/j.ygyno.2016.05.023. Epub 2016 May 27 [PubMed PMID: 27234143]
Aydogmus S, Kelekci S, Aydogmus H, Ekmekci E, Secil Y, Ture S. Obturator Nerve Injury: An Infrequent Complication of TOT Procedure. Case reports in obstetrics and gynecology. 2014:2014():290382. doi: 10.1155/2014/290382. Epub 2014 Sep 29 [PubMed PMID: 25343052]
Level 3 (low-level) evidencePanagoda PI, Vasdev N, Gowrie-Mohan S. Avoiding the Obturator Jerk during TURBT. Current urology. 2018 Oct:12(1):1-5. doi: 10.1159/000447223. Epub 2018 Jun 30 [PubMed PMID: 30374273]
Kawaguchi M, Hashizume K, Iwata T, Furuya H. Percutaneous radiofrequency lesioning of sensory branches of the obturator and femoral nerves for the treatment of hip joint pain. Regional anesthesia and pain medicine. 2001 Nov-Dec:26(6):576-81 [PubMed PMID: 11707799]
Level 3 (low-level) evidenceKulkarni SR, Punamiya AR, Naniwadekar RG, Janugade HB, Chotai TD, Vimal Singh T, Natchair A. Obturator hernia: A diagnostic challenge. International journal of surgery case reports. 2013:4(7):606-8. doi: 10.1016/j.ijscr.2013.02.023. Epub 2013 Apr 17 [PubMed PMID: 23708307]
Level 3 (low-level) evidenceMartin R, Martin HD, Kivlan BR. NERVE ENTRAPMENT IN THE HIP REGION: CURRENT CONCEPTS REVIEW. International journal of sports physical therapy. 2017 Dec:12(7):1163-1173 [PubMed PMID: 29234567]
Bradshaw C, McCrory P, Bell S, Brukner P. Obturator nerve entrapment. A cause of groin pain in athletes. The American journal of sports medicine. 1997 May-Jun:25(3):402-8 [PubMed PMID: 9167824]