Introduction
Tricuspid valve infective endocarditis (TVIE) is an uncommon entity, especially when compared to left-sided infective endocarditis. Right-sided infected infective endocarditis (RSIE) accounts for approximately 5 – 10% of all cases of infective endocarditis (IE). [1] The overwhelming number of cases of RSIE involve the tricuspid valve with some estimates as high as 90%. The majority of TVIE are associated with IV drug use (IVDU). Given the rise of IVDU in the United States, rates of TVIE have also increased significantly since 2006. [2] Along with IVDU, hemodialysis catheters, pacemakers, and defibrillator leads are also risk factors. Staphylococcus aureus is the most common organism, which causes TVIE. However, various skin flora, as well as various Staphylococcus and Streptococcus species can infect the tricuspid valve. Duke’s Criteria is used to establish the diagnosis of TVIE. However, there are certain aspects of TVIE which can make it detection difficult. Such features include absent murmur, concurrent pneumonia, and less peripheral phenomena such as splinter hemorrhages. [3] Regardless, TVIE is treatable and has favorable outcomes if detected and treated early in its course. Although RSIE and TVIE are increasing in prevalence, antibiotics and surgical options remain a mainstay of successful treatment.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Important risk factors for tricuspid valve infective endocarditis (TVIE) include:
Intravenous drug users (IVDU): Infections resulting from IVDU involve 30% to 40% of all TVIE cases.
Cardiac implantable electronic device (CIED) Infection: TVIE is considered device related if there is evidence of valvular vegetation and tricuspid regurgitation in the presence of positive blood cultures.
Indwelling catheter: hemodialysis, parenteral nutrition, and chemotherapy requiring long term central venous access.
Epidemiology
It is certain that cases of right-sided infective endocarditis (RSIE) and TVIE are increasing. In one study, hospitalizations for IVDU related infective endocarditis increased 12-percent. [4] IVDU accounts for 86% of TVIE. TVIE is more common among males, although the ratio is normalizing. Over time, the population with TVIE has become younger, and more commonly white. [4]
History and Physical
History and physical exam are essential towards making an adequate diagnosis in cases of TVIE. Establishing diagnosis can be more difficult in these cases because presentation can often be subacute or present with absence of typical IE features. Peripheral phenomenon such as splinter hemorrhages is less common, as is a cardiac murmur. However, clinicians must always be aware of potential complications of this disease process that are manifested by the various embolic phenomenon. Characteristics, which should lead clinicians to consider TVIE, include:
- Fever
- Chills
- Anorexia
- Weight loss
- Fatigue
- Malaise
- Arthralgia
- Dyspnea on exertion
- A cough
- Pleuritic pain
- Abdominal Pain
Physical Exam Findings
- Tachypnea
- Hypotension
- Cardiac murmur
- Splenomegaly
- Splinter hemorrhages
- Petechiae
- Janeway lesions
- Osler nodes
- Roth spots
- Focal neurologic deficits
- Joint effusion
- Clubbing
Evaluation
Diagnosis of TVIE is based upon the modified Duke Criteria. This criterion is widely used to diagnose TVIE like all other forms of IE. This criterion allows one to stratify infective endocarditis into a category of definite, possible, or rejected. Based on clinical criteria definite endocarditis is defined as two primary criteria, one major with three minor criteria, or five minor criteria. Possible endocarditis is measured by the presence of one major with two minor criteria, or with three minor criteria alone. [5] The criteria classes are as follows:
Major Criteria
Positive blood culture(any of the followings):
- Two separate blood cultures with organisms known to cause infective endocarditis or
- Organism consistent with endocarditis from blood cultures obtained 12 hours apart or
- Positive culture for organisms that are common skin contaminant in 3 or the majority of ≥4 separate blood cultures (first and last sample drawn at least 1 hour apart) or
- Single positive blood culture of Coxiella burnetti
Evidence of endocardial involvement (vegetation, abscess, new valvular regurgitation, dehiscence of a prosthetic valve)
Minor Criteria
- Fever > 38 degrees C (100.4 degrees F)
- Immunologic occurrence: Roth spots, Osler nodes, glomerulonephritis.
- Predisposing heart defect or IVDU
- Vascular phenomena: septic emboli, arterial emboli, conjunctival hemorrhages, splinter hemorrhages, Janeway lesions, mycotic aneurysm
- A positive blood culture that does not meet essential criteria.
Routine laboratory values in IE are generally nonspecific. Basic workup should be done. Some abnormalities which may be found include leukocytosis, elevated ESR, elevated CRP, normocytic anemia, or urinalysis revealing hematuria, proteinuria, or pyuria. EKG may reveal conduction anomalies such as heart block. [6]
- Chest radiographs should be obtained to evaluate for septic emboli or infiltrate.
- CT scan of the abdomen is helpful to evaluate for metastatic emboli. Such emboli include splenic or renal infarcts. Clinicians should have a low threshold to locate these potential foci.
- Blood cultures should be obtained in all individuals with suspected TVIE. A minimum of three sets should be collected from different sites. [26341945]
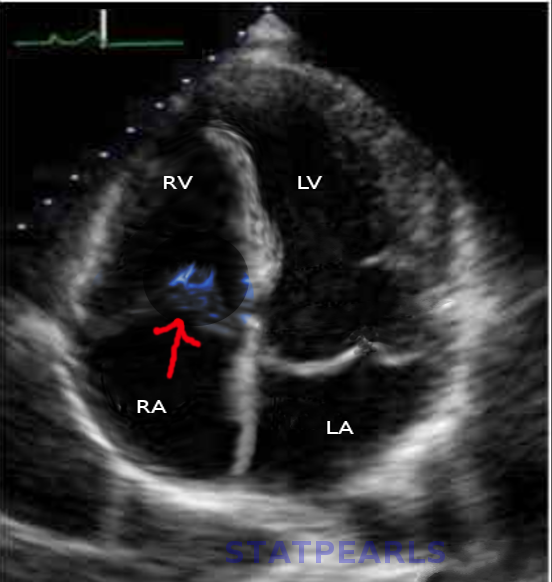
- Echocardiography should be performed in all individuals with suspected TVIE. Transthoracic echocardiogram (TTE) is the first test that is done. TTE is very specific. Transesophageal echocardiography should be pursued if TTE is negative, but a high clinical suspicion for IE exists. TEE may also be used if significant valve regurgitation exists and needs to be further evaluated prior to surgery. [7]
Treatment / Management
Some individuals with TVIE may be candidates for shorter duration antibiotic regimens(no evidence of renal failure, the absence of extrapulmonary metastatic infections or simultaneous left sided infection). The 2-week regimens are not used in patients with IE of the aortic or mitral valve, in patients with MRSA, or patients with complicated IE. [8] Patients with TVIE should be started on an empiric antibiotic regimen once it is suspected.
Initial empiric antibiotics should include coverage against the most common pathogens. Thus staphylococcus and streptococcus coverage are recommended. Vancomycin is used as an initial choice of antibiotic. These medicines should be tailored based upon blood cultures results. Once an organism has been specified, antibiotics regimen should typically be continued for six weeks from the date of first negative blood culture. Very limited patients can be trialed with a short duration course. These candidates include those with isolated TVIE, those without any complications secondary to IE, and those with IE from HACEK organisms. [9] For patients with methicillin-sensitive Staph aureus (MSSA) IE, it is vital to change vancomycin to an antibiotic more specific against MSSA. Such antibiotics include nafcillin, oxacillin, or cefazolin. Patient with MRSA IE should be treated with vancomycin for six weeks.(B3)
Surgical treatment of IE is reserved for individuals with the following: [10](A1)
- TV vegetation > 2cm with septic pulmonary emboli.
- Persistent bacteremia for one week despite adequate treatment.
- Severe tricuspid regurgitation with right-sided heart failure.
Differential Diagnosis
Infective endocarditis of any form can be difficult to identify. IE can have many nonspecific complaints which can overlap in various autoimmune, infectious, or neoplastic processes. It is important to think of IE as a syndrome. The Duke Modified Criteria serves as the principal diagnostic tool that takes into account all the potential manifestations of this disease process. Some of the differential diagnoses which may also be considered include:
- Systemic lupus erythematosus
- Polymyalgia rheumatic
- Lyme Disease
- Antiphospholipid syndrome
- Libman sacks endocarditis
- Atrial myxoma
- Rheumatic fever
- Marantic endocarditis
Prognosis
Patients with TVIE have good prognosis compared to those with other forms of IE. The fatality rate is lower in these patients. [11] In one study evaluating native valve endocarditis, overall mortality was 6%. [12] Vegetation size is an important prognostic factor. Those with vegetation greater than 1cm have significantly increased mortality. Individuals who have concurrent left-sided infective endocarditis have a worse prognosis. This diagnosis is due to the higher risk of abscess development in these cases. [1]
Complications
Complications of TVIE include [13]
- Peri-annular abscesses
- Septic pulmonary emboli
- Splenic abscess
- A mycotic aneurysm
- Heart failure
Consultations
Infective Endocarditis requires management by a group of physicians. Some physicians who should be involved in the care of these patients include
- Internal medicine
- Infectious disease
- Cardiology
- Cardiothoracic surgery
Deterrence and Patient Education
Patients should be made aware of the potential risk factors for developing TVIE. When hospitalized, efforts should be made to educate these patients about the hazards of IV drug abuse. Furthermore, all available resources should be used to prevent these individuals from relapsing into IVDU again. These include information and access to local rehab centers, education, and pharmacologic options.
Enhancing Healthcare Team Outcomes
interprofessional management of the patient with IE is essential to ensure positive outcomes. Physicians are important clinicians in assessing these patients and helping establish the diagnosis of TVIE. Nurses involved in the patient's care can identify changes in clinical status or clinical deterioration. Pharmacists have an important role in assisting with antimicrobial management. Some aspects of this care include appropriate empiric regimens, narrowing antimicrobial coverage, and ensuring an adequate therapeutic range of medications and their dosages. Case managers and social workers also play an essential role in finding rehab facilities to help prevent future IVDU, as well as to help arrange for outpatient facilities to obtain longer term IV antibiotics if necessary. Treating TVIE requires a team approach to ensure successful outcomes. The outcomes for patients with TVIE depends on patient age, comorbidity, hemodynamic status, the presence of sepsis and time of treatment.
Media
(Click Image to Enlarge)
References
Hussain ST, Witten J, Shrestha NK, Blackstone EH, Pettersson GB. Tricuspid valve endocarditis. Annals of cardiothoracic surgery. 2017 May:6(3):255-261. doi: 10.21037/acs.2017.03.09. Epub [PubMed PMID: 28706868]
Wurcel AG, Anderson JE, Chui KK, Skinner S, Knox TA, Snydman DR, Stopka TJ. Increasing Infectious Endocarditis Admissions Among Young People Who Inject Drugs. Open forum infectious diseases. 2016 Sep:3(3):ofw157 [PubMed PMID: 27800528]
Chambers HF, Korzeniowski OM, Sande MA. Staphylococcus aureus endocarditis: clinical manifestations in addicts and nonaddicts. Medicine. 1983 May:62(3):170-7 [PubMed PMID: 6843356]
Fruauff AA, Barasch ES, Rosenthal A. Solitary myeloblastoma presenting as acute hydrocephalus: review of literature, implications for therapy. Pediatric radiology. 1988:18(5):369-72 [PubMed PMID: 3050842]
Level 3 (low-level) evidenceHansen JB, Jagt T, Gundtoft P, Sorensen HR. Pharyngo-oesophageal diverticula. A clinical and cineradiographic follow-up study of 23 cases treated by diverticulectomy. Scandinavian journal of thoracic and cardiovascular surgery. 1973:7(1):81-6 [PubMed PMID: 4632890]
Level 3 (low-level) evidenceDinubile MJ. Heart block during bacterial endocarditis: a review of the literature and guidelines for surgical intervention. The American journal of the medical sciences. 1984 May-Jun:287(3):30-2 [PubMed PMID: 6731477]
Level 3 (low-level) evidenceDe Castro S, Cartoni D, d'Amati G, Beni S, Yao J, Fiorell M, Gallo P, Fedele F, Pandian NG. Diagnostic accuracy of transthoracic and multiplane transesophageal echocardiography for valvular perforation in acute infective endocarditis: correlation with anatomic findings. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2000 May:30(5):825-6 [PubMed PMID: 10816155]
Torres-Tortosa M, de Cueto M, Vergara A, Sánchez-Porto A, Pérez-Guzmán E, González-Serrano M, Canueto J. Prospective evaluation of a two-week course of intravenous antibiotics in intravenous drug addicts with infective endocarditis. Grupo de Estudio de Enfermedades Infecciosas de la Provincia de Cádiz. European journal of clinical microbiology & infectious diseases : official publication of the European Society of Clinical Microbiology. 1994 Jul:13(7):559-64 [PubMed PMID: 7805683]
Gould FK, Denning DW, Elliott TS, Foweraker J, Perry JD, Prendergast BD, Sandoe JA, Spry MJ, Watkin RW, Working Party of the British Society for Antimicrobial Chemotherapy. Guidelines for the diagnosis and antibiotic treatment of endocarditis in adults: a report of the Working Party of the British Society for Antimicrobial Chemotherapy. The Journal of antimicrobial chemotherapy. 2012 Feb:67(2):269-89. doi: 10.1093/jac/dkr450. Epub 2011 Nov 14 [PubMed PMID: 22086858]
Level 3 (low-level) evidenceNishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Guyton RA, O'Gara PT, Ruiz CE, Skubas NJ, Sorajja P, Sundt TM 3rd, Thomas JD, ACC/AHA Task Force Members. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014 Jun 10:129(23):2440-92. doi: 10.1161/CIR.0000000000000029. Epub 2014 Mar 3 [PubMed PMID: 24589852]
Level 1 (high-level) evidenceOrtiz-Bautista C, López J, García-Granja PE, Sevilla T, Vilacosta I, Sarriá C, Olmos C, Ferrera C, Sáez C, Gómez I, San Román JA. Current profile of infective endocarditis in intravenous drug users: The prognostic relevance of the valves involved. International journal of cardiology. 2015:187():472-4. doi: 10.1016/j.ijcard.2015.03.368. Epub 2015 Mar 27 [PubMed PMID: 25846656]
Martín-Dávila P, Navas E, Fortún J, Moya JL, Cobo J, Pintado V, Quereda C, Jiménez-Mena M, Moreno S. Analysis of mortality and risk factors associated with native valve endocarditis in drug users: the importance of vegetation size. American heart journal. 2005 Nov:150(5):1099-106 [PubMed PMID: 16291005]
Mocchegiani R, Nataloni M. Complications of infective endocarditis. Cardiovascular & hematological disorders drug targets. 2009 Dec:9(4):240-8 [PubMed PMID: 19751182]