Introduction
Posterior tibial tendon dysfunction (PTTD), now renamed progressive collapsing foot deformity (PCFD), is the most common cause of adult-acquired flatfoot deformity. Failure of the posterior tibial tendon (PTT) affects surrounding ligamentous structures and eventually leads to bony involvement and deformity. PTTD is a progressive and debilitating disorder that can be detrimental to patients due to resulting limitations in mobility, significant pain, and weakness.[1] Risk factors for the disease have been studied and may include hypertension, obesity, diabetes, previous trauma, or steroid exposure.[2] This activity will explain the extent of the disease and its progression.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Historically, Johnson and Strom proposed a 3-stage classification of PTTD based on the condition of the PTT, the position of the hindfoot, and the flexibility of the deformity.[3] Researchers have proposed numerous mechanisms for the degeneration of the PTT, the most common being repetitive loading, which causes microtrauma and progressive failure.
A retromalleolar hypovascular region does exist and may also contribute to the disease. In a study by Manske et al, cadaver specimens showed an area of decreased blood supply from 2.2 cm (SD 0.8 cm) proximal to the medial malleolus to a region 0.6 cm (SD 0.6 cm) proximal to the medial malleolus.[3]
The anatomic course of the PTT likely contributes to the disease, as the tendon makes an acute turn around the medial malleolus. This location puts significant tension on the tendon in the region distal and posterior to the medial malleolus. The adjacent tendons, namely the flexor hallucis longus and the flexor digitorum longus (FDL), do not take this sharp turn.[4]
Metabolic and genetic conditions must also be considered. Diabetes mellitus involves loss of collagen organization, tendon thickening, and calcification, all of which increase the chance of tendon attenuation.[4] Patients with hyperlipidemia have been shown to release proinflammatory cytokines and upregulate matrix-degrading protein, leading to tendon stiffness and decreased healing potential. Moreover, recent studies have demonstrated the influence of genetic inheritance on the predisposition to develop tendinopathy. Genetic predisposition to increased levels of collagen types III and V and matrix metalloproteinases 1, 8, and 13 have been correlated to PTT degeneration.[5] [6]
Although theories of PTT degeneration remain possible causes of PTTD, it is now understood that the deformity can involve a complex combination of midfoot, rearfoot, and ankle deformities not previously described. Furthermore, attenuation or rupture of the plantar fascia, spring ligament, and deltoid ligaments can occur in the absence of PTT rupture, leading to the condition. These factors contributed to the change in nomenclature from PTTD to PCFD.[3]
Isolated spring ligament injury or a combination of spring and deltoid ligament insufficiencies in the absence of PTT degeneration have been shown to cause PCFD.[7] These conditions have been described mainly in small studies, where patients present with normal inversion strength, tenderness anterior to the medial malleolus, and MRI confirmation of spring ligament tear.[8] Other potential culprits include constriction beneath the flexor retinaculum,[5] abnormal anatomy of the talus,[6] degenerative changes associated with osteoarthritis,[7] and preexisting pes planus.[8]
Epidemiology
Although no significant large-scale studies have been performed about the overall incidence of this disease, the prevalence of PCFD is estimated to be between 3.3% and 10%, depending on the sex and age of the patient.[9] A body mass index (BMI) of 25 kg/m2 or higher is prevalent in 81.5% of patients and occurs predominantly in females.[9] The classic PCFD patient is a woman with obesity in her sixth decade of life.[9] A case-control study reported a significantly higher prevalence of leg length discrepancy in PCFD patients compared to the control group, suggesting leg length discrepancy as a predisposing factor for PCFD.[10] PCFD is associated with adult-acquired flatfoot deficiency, which can lead to misdiagnosis, potentially resulting in a much higher actual prevalence than reported in the literature. Additionally, underreporting may occur due to the early, asymptomatic stages of PCFD.
Histopathology
In normal PTT, linear collagen bundles are predominant, accompanied by normal fibroblast cellularity and a low proportion of vascular density. However, in PTTD, the tendon experiences microtrauma, leading to tendinitis characterized by increased mucin content, neovascularization, and fibroblast hypercellularity.[11]
History and Physical
Most patients with PCFD will exhibit medial ankle and foot pain in the early stages of the disease. Later stages may involve lateral pain due to subfibular impingement or peroneal tendon injury.[12]
A comprehensive physical examination is crucial for determining the grading and severity of the disease. The attention should first be turned to grossly inspecting the feet while standing. A weight-bearing examination is essential, as a flexible deformity may normally be present while the patient is non-weight–bearing. The collapse of the medial longitudinal arch leads to pes planus, which is an easily visualized condition. While inspecting the patient, a common observation is the "too many toes" sign; when viewed from behind, more than two toes will flare out laterally due to the valgus alignment of the foot. Equinus contracture is another frequently encountered finding that potentially limits ankle dorsiflexion.
Single-limb heel raise is an important clinical test that can differentiate stage I disease from stage II and beyond. A patient with stage I disease should be able to perform this test without pain. In stage II disease, patients may be able to perform the test but will likely have pain. In advanced stages, rigid deformities may prevent the patient from completing the test. Additionally, foot flexibility warrants examination during evaluation.[12]
Evaluation
Imaging is critical in determining the severity of PCFD and subsequent treatment. Anteroposterior (AP) and lateral radiographs of the foot are necessary. Increased talonavicular uncoverage and increased talo-first metatarsal angle (or Simmons angle) will be evident on the AP radiograph. The normal talo-first metatarsal angle is around 7 degrees, and angles over 16 degrees indicate flatfoot deformity.[11] Talonavicular coverage is expressed as the proportion of the talus not in contact with the navicular medially, with values surpassing 30% to 40% typically suggestive of forefoot abduction, characteristic of stages II to IV PCFD.[9] A cutoff value of 25.4 degrees of talonavicular coverage serves as a discriminator between patients with or without sinus tarsi impingement.[13] On the weight-bearing lateral radiograph, assessment should include the evaluation of an increased talo-first metatarsal angle (or Meary angle), which typically measures 0±4 degrees but exceeds 20 degrees in cases of flatfoot deformity.[10]
When considering advanced imaging, options such as weight-bearing computed tomography (WBCT) and magnetic resonance imaging (MRI) are available. WBCT has demonstrated an enhanced ability to recognize deformities, accompanied by excellent inter-rater reliability.[14] Although the orthopedic consensus group opted against incorporating MRI into a classification system,[3] it remains a valuable tool for assessing the condition of affected soft tissue (see Image. MRI of Posterior Tibial Tendon Dysfunction).
Treatment / Management
The treatment approach outlined for PTTD stages is historically suitable for the new PCFD nomenclature.
- All stages (initially):
- Conservative management with nonsteroidal anti-inflammatory drugs (NSAIDs) and activity modification. This is also indicated for nonsurgical candidates or low-demand, older patients.[15]
(B2)
- Stage I:
- Conservative management through immobilization in a walking boot or cast for up to 3 to 4 weeks may be warranted to allow for healing of the PTT, followed by eccentric strengthening with physical therapy.[1]
- If immobilization and physical therapy are successful, transitioning to custom-molded orthotics or ankle-foot orthosis (AFO) is appropriate to maintain relief, with a crucial emphasis on medial forefoot posting. University of California Biomechanics Laboratory (UCBL) orthoses, featuring a custom insert with a lace-up component, can help maintain midfoot height.[16]
- Conservative therapy is recommended for 3 to 4 months overall, with surgical intervention being considered if conservative measures fail. A tenosynovectomy, coupled with tubularization, may be indicated in such cases.
(A1)
- Stage IIA:
- Conservative management includes immobilization and physical therapy, following the recommendations for stage I, along with the use of orthotics or AFO.
- Surgical treatment involves medial calcaneal osteotomy with posterior tendon debridement and repair. Ancillary procedures may include any or all of the following: FDL transfer, spring ligament reconstruction, or Achilles tendon lengthening.[17]
(B2)
- Stage IIB:
- All previously listed procedures in stage IIA are considered +/- lateral column lengthening or isolated subtalar joint arthrodesis.
- Stage III:
- Conservative therapies, as mentioned above, are typically used.
- Surgical treatment is often warranted due to rearfoot arthritic changes. Common procedures include medial double arthrodesis or triple arthrodesis (subtalar, calcaneocuboid, and talonavicular arthrodesis), with or without deltoid ligament repair.[18]
- Stage IV:
- Conservative therapies, as mentioned above, are typically used.
- Surgical treatment is often necessary due to arthritic changes in the ankle and rearfoot. Surgical options may encompass a variety of procedures, including triple arthrodesis with Achilles tendon lengthening, deltoid ligament reconstruction, and total ankle arthroplasty with replacement.[18] Alternatively, medial double arthrodesis, deltoid ligament reconstruction, and total ankle arthroplasty with replacement can be considered if ankle deformity is reducible. A staged approach is recommended for patients deemed suitable candidates for total ankle arthroplasty. This involves performing rearfoot arthrodesis and soft tissue balancing initially, followed by a second stage for total ankle arthroplasty 4 to 8 weeks later.
- Tibiotalocalcaneal arthrodesis is indicated for a rigid hindfoot with a significant valgus alignment of the talus within the ankle mortise.[19][20] Pantalar Pantalar arthrodesis, which involves triple arthrodesis with the addition of ankle arthrodesis, is also considered in such cases.
The PCFD classification does not outline a treatment algorithm similar to the former PTTD, but the orthopedic consensus agreed on the following statements:[21](B3)
- Preservation of range of motion and mobility should be a primary goal.
- Talonavicular (TN) joint fusion should be considered in cases of arthritis, joint stiffness, significant sagittal plane deformities, severe deformities, and inadequate correction of TN abduction with other procedures.
- Patients with a BMI exceeding 30 experience poorer outcomes with reconstructive surgery compared to hindfoot fusions.
- Joint preservation procedures should be attempted for young patients.
Differential Diagnosis
Although PCFD is the most prevalent cause of adult-acquired flatfoot deformity, numerous related conditions exist. The following diagnoses can manifest with striking similarity to PCFD and thus warrant consideration during evaluation:[22]
- Tarsal coalition
- Inflammatory arthritis
- Charcot arthropathy
- Neuromuscular disease
- Traumatic disruption of midfoot ligaments
Staging
The Johnson and Strom classification for PTTD insufficiency, modified by Myerson and described below, defines radiographic findings, physical examination findings, and associated deformities. This classification has been widely accepted for many years.
Stage I: Normal radiographs, able to perform single-heel raise, and mild tenosynovitis.
Stage IIA: Arch collapse on a radiograph, unable to perform single-heel raise, and a flexible flatfoot deformity.
Stage IIB: Arch collapse and talonavicular uncoverage (over 40%) on a radiograph, unable to perform single-heel raise, flexible flatfoot deformity, and characteristic forefoot abduction or "too many toes" sign.[23]
Stage III: Subtalar arthritis on a radiograph, unable to perform single-heel raise, flatfoot deformity with rigid forefoot abduction, and hindfoot valgus
Stage IV: Valgus deformity of the talus in the ankle mortise, visualized on an AP radiograph of the ankle with talar tilt due to deltoid ligament compromise; subtalar arthritis on radiographs; unable to perform a single-heel raise; flatfoot deformity with rigid forefoot abduction; and hindfoot valgus.[23]
In 2020, Myerson et al, together with the consensus group, proposed the newest accepted classification with the nomenclature change to PCFD:
- Stage I is flexible
- Stage II is rigid
Both stages I and II can be subdivided into classes A through E.
Class A: Hindfoot valgus deformity
- Hindfoot valgus alignment
- Increased hindfoot moment arm, hindfoot alignment angle, foot and ankle offset
Class B: Midfoot/forefoot abduction deformity
- Decreased talar head coverage
- Increased talonavicular coverage angle
- Presence of sinus tarsi impingement
Class C: Forefoot varus deformity/medial column instability
- Increased talus-first metatarsal angle
- Plantar gapping first tarsometatarsal (TMT)/naviculocuneiform (NC) joints
- Clinical forefoot varus
Class D: Peritalar subluxation/dislocation
- Significant subtalar joint subluxation/subfibular impingement
Class E: Ankle instability
- Valgus tilting of the ankle joint
Prognosis
PCFD is a progressive disorder that worsens without intervention. Early detection and intervention are crucial for slowing its progression. Patients who receive custom orthotics and undergo rehabilitation typically experience significant improvement. In a recent study conducted by Alvarez et al, approximately 89% of patients with stages I and II PCFD responded positively to orthotics and physical therapy, with nearly all regaining full strength within 4 months.[20]
Orthotic management has also shown promising outcomes for injuries to the spring ligament.[7] However, analyses of surgical outcomes reveal less predictable results, with no assurance of returning to the pre-disease state. Patients may experience residual effects even after reconstructive surgeries.[24]
Complications
General complications of surgical reconstruction include thromboembolic events, infection, wound dehiscence, neurologic injury, and painful hardware, either individually or in combination. Reports indicate that up to one-third of patients undergoing flatfoot reconstruction experience wound-healing complications, underscoring the paramount importance of diligent wound care.[25]
Postoperative and Rehabilitation Care
Postoperative care is crucial for the success of the procedures. Typically, patients will be fitted with a non-weight–bearing cast or splint for 6 to 8 weeks. Follow-up appointments for suture removal evaluation should be scheduled between 10 and 14 days after the procedure. Physical therapy may be deemed necessary for some patients.
Consultations
Patients experiencing discomfort due to flat feet should undergo evaluation by podiatry and physical therapy. If these interventions prove ineffective, referral to orthopedics should be considered.
Deterrence and Patient Education
Patient education and emphasis on a conservative approach can improve patient outcomes:
- Activity restriction and modification are significant initial steps in nonoperative management.
- Evidence supports conservative therapy in the early stages of the disease, including the use of NSAIDs.
- In many cases, prescriptions for medial arch support insoles or custom orthotics are often necessary.
- Surgery is usually considered a last resort if conservative interventions are ineffective and recovery is prolonged.
- When performing surgery, temper patient expectations, as reconstruction options commonly result in residual symptoms.
Pearls and Other Issues
- Staging posterior PCFD using the Johnson and Strom classification can be helpful for treatment guidance.
- Other soft tissue structures besides the PTT, such as the deltoid and spring ligaments, should be evaluated and considered for operative treatment.
- Identifying the specific location of arthritic changes on radiographs will help to differentiate the deformity.
Enhancing Healthcare Team Outcomes
Early diagnosis of PCFD is essential, as it may prevent rapid deterioration through conservative measures. Primary care physicians and nurse practitioners can refer patients to sub-specialists, such as podiatrists, physical therapists, and foot and ankle orthopedic surgeons, for a more thorough workup or evaluation, which can lead to significantly better patient outcomes.
PCFD requires an interprofessional team approach, including physicians, specialists, specialty-trained nurses, and pharmacists, collaborating across disciplines to achieve optimal patient results.
Media
(Click Image to Enlarge)
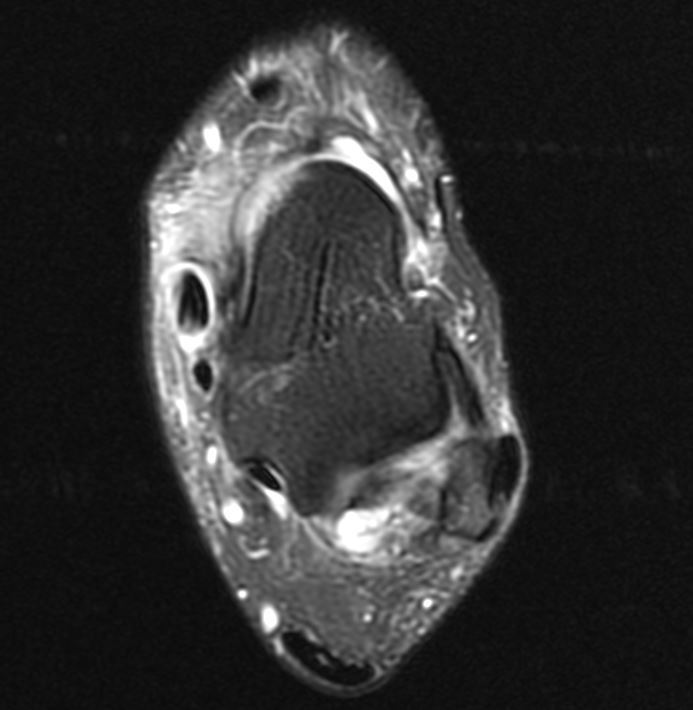
MRI of Posterior Tibial Tendon Dysfunction. The image illustrates magnetic resonance imaging (MRI) of posterior tibial tendon dysfunction, also known as progressive collapsing foot deformity. The MRI demonstrates extensive tenosynovitis of the posterior tibial tendon (PTT); no tears were noted. The PTT is over double the size of the flexor digitorum longus tendon (FDL).
Contributed by MA Dreyer, DPM, FACFAS
References
Ross MH, Smith MD, Mellor R, Vicenzino B. Exercise for posterior tibial tendon dysfunction: a systematic review of randomised clinical trials and clinical guidelines. BMJ open sport & exercise medicine. 2018:4(1):e000430. doi: 10.1136/bmjsem-2018-000430. Epub 2018 Sep 19 [PubMed PMID: 30271611]
Level 1 (high-level) evidenceHolmes GB Jr, Mann RA. Possible epidemiological factors associated with rupture of the posterior tibial tendon. Foot & ankle. 1992 Feb:13(2):70-9 [PubMed PMID: 1349292]
Level 2 (mid-level) evidenceMyerson MS, Thordarson DB, Johnson JE, Hintermann B, Sangeorzan BJ, Deland JT, Schon LC, Ellis SJ, de Cesar Netto C. Classification and Nomenclature: Progressive Collapsing Foot Deformity. Foot & ankle international. 2020 Oct:41(10):1271-1276. doi: 10.1177/1071100720950722. Epub 2020 Aug 28 [PubMed PMID: 32856474]
Godoy-Santos AL, Schmidt EL, Chaparro F. What Are the Updates on Epidemiology of Progressive Collapsing Foot Deformity? Foot and ankle clinics. 2021 Sep:26(3):407-415. doi: 10.1016/j.fcl.2021.05.006. Epub 2021 Jun 27 [PubMed PMID: 34332726]
Diniz-Fernandes T, Godoy-Santos AL, Santos MC, Pontin P, Pereira CAA, Jardim YJ, Velosa APP, Maffulli N, Teodoro WR, Capelozzi VL. Matrix metalloproteinase-1 (MMP-1) and (MMP-8) gene polymorphisms promote increase and remodeling of the collagen III and V in posterior tibial tendinopathy. Histology and histopathology. 2018 Sep:33(9):929-936. doi: 10.14670/HH-11-982. Epub 2018 Mar 13 [PubMed PMID: 29532899]
de Araujo Munhoz FB, Baroneza JE, Godoy-Santos A, Fernandes TD, Branco FP, Alle LF, de Souza RL, Dos Santos MC. Posterior tibial tendinopathy associated with matrix metalloproteinase 13 promoter genotype and haplotype. The journal of gene medicine. 2016 Nov:18(11-12):325-330. doi: 10.1002/jgm.2934. Epub [PubMed PMID: 27886420]
Richie DH Jr. Injuries to the Spring Ligament: Nonoperative Treatment. Clinics in podiatric medicine and surgery. 2022 Jul:39(3):461-476. doi: 10.1016/j.cpm.2022.02.007. Epub [PubMed PMID: 35717063]
Krautmann K, Kadakia AR. Spring and Deltoid Ligament Insufficiency in the Setting of Progressive Collapsing Foot Deformity. An Update on Diagnosis and Management. Foot and ankle clinics. 2021 Sep:26(3):577-590. doi: 10.1016/j.fcl.2021.05.004. Epub 2021 Jun 27 [PubMed PMID: 34332736]
Rhim HC, Dhawan R, Gureck AE, Lieberman DE, Nolan DC, Elshafey R, Tenforde AS. Characteristics and Future Direction of Tibialis Posterior Tendinopathy Research: A Scoping Review. Medicina (Kaunas, Lithuania). 2022 Dec 16:58(12):. doi: 10.3390/medicina58121858. Epub 2022 Dec 16 [PubMed PMID: 36557060]
Level 2 (mid-level) evidenceSanhudo JA, Gomes JL. Association between leg length discrepancy and posterior tibial tendon dysfunction. Foot & ankle specialist. 2014 Apr:7(2):119-26. doi: 10.1177/1938640014522096. Epub 2014 Feb 12 [PubMed PMID: 24525616]
Mosier SM, Lucas DR, Pomeroy G, Manoli A 2nd. Pathology of the posterior tibial tendon in posterior tibial tendon insufficiency. Foot & ankle international. 1998 Aug:19(8):520-4 [PubMed PMID: 9728698]
Ellis SJ, Deyer T, Williams BR, Yu JC, Lehto S, Maderazo A, Pavlov H, Deland JT. Assessment of lateral hindfoot pain in acquired flatfoot deformity using weightbearing multiplanar imaging. Foot & ankle international. 2010 May:31(5):361-71. doi: 10.3113/FAI.2010.0361. Epub [PubMed PMID: 20460061]
Level 3 (low-level) evidenceKim J, Rajan L, Fuller R, Sofka C, Cororaton A, Demetracopoulos C, Ellis S, Deland J. Radiographic Cutoff Values for Predicting Lateral Bony Impingement in Progressive Collapsing Foot Deformity. Foot & ankle international. 2022 Sep:43(9):1219-1226. doi: 10.1177/10711007221099010. Epub 2022 Jun 14 [PubMed PMID: 35699393]
Barbachan Mansur NS, Lalevée M, Lee HY, Ehret A, Fayed A, Mann TS, de Carvalho KAM, de Cesar Netto C. Influence of Weightbearing Computed Tomography in the Progressive Collapsing Foot Deformity Classification System. Foot & ankle international. 2023 Feb:44(2):125-129. doi: 10.1177/10711007221141898. Epub 2023 Jan 13 [PubMed PMID: 36639923]
Nielsen MD, Dodson EE, Shadrick DL, Catanzariti AR, Mendicino RW, Malay DS. Nonoperative care for the treatment of adult-acquired flatfoot deformity. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 2011 May-Jun:50(3):311-4. doi: 10.1053/j.jfas.2011.02.002. Epub 2011 Mar 31 [PubMed PMID: 21458301]
Level 2 (mid-level) evidenceImhauser CW, Abidi NA, Frankel DZ, Gavin K, Siegler S. Biomechanical evaluation of the efficacy of external stabilizers in the conservative treatment of acquired flatfoot deformity. Foot & ankle international. 2002 Aug:23(8):727-37 [PubMed PMID: 12199387]
Myerson MS, Badekas A, Schon LC. Treatment of stage II posterior tibial tendon deficiency with flexor digitorum longus tendon transfer and calcaneal osteotomy. Foot & ankle international. 2004 Jul:25(7):445-50 [PubMed PMID: 15319100]
Level 2 (mid-level) evidenceKadakia AR, Haddad SL. Hindfoot arthrodesis for the adult acquired flat foot. Foot and ankle clinics. 2003 Sep:8(3):569-94, x [PubMed PMID: 14560906]
Pellegrini MJ, Schiff AP, Adams SB Jr, DeOrio JK, Easley ME, Nunley JA 2nd. Outcomes of Tibiotalocalcaneal Arthrodesis Through a Posterior Achilles Tendon-Splitting Approach. Foot & ankle international. 2016 Mar:37(3):312-9. doi: 10.1177/1071100715615398. Epub 2015 Nov 17 [PubMed PMID: 26578482]
Smith JT, Bluman EM. Update on stage IV acquired adult flatfoot disorder: when the deltoid ligament becomes dysfunctional. Foot and ankle clinics. 2012 Jun:17(2):351-60. doi: 10.1016/j.fcl.2012.03.011. Epub 2012 Apr 10 [PubMed PMID: 22541531]
Sangeorzan BJ, Hintermann B, de Cesar Netto C, Day J, Deland JT, Ellis SJ, Johnson JE, Myerson MS, Schon LC, Thordarson DB. Progressive Collapsing Foot Deformity: Consensus on Goals for Operative Correction. Foot & ankle international. 2020 Oct:41(10):1299-1302. doi: 10.1177/1071100720950759. Epub 2020 Aug 27 [PubMed PMID: 32851848]
Level 3 (low-level) evidencePomeroy GC, Pike RH, Beals TC, Manoli A 2nd. Acquired flatfoot in adults due to dysfunction of the posterior tibial tendon. The Journal of bone and joint surgery. American volume. 1999 Aug:81(8):1173-82 [PubMed PMID: 10466651]
Iossi M, Johnson JE, McCormick JJ, Klein SE. Short-term radiographic analysis of operative correction of adult acquired flatfoot deformity. Foot & ankle international. 2013 Jun:34(6):781-91. doi: 10.1177/1071100713475432. Epub 2013 Feb 5 [PubMed PMID: 23386748]
Level 2 (mid-level) evidencePinney SJ, Lin SS. Current concept review: acquired adult flatfoot deformity. Foot & ankle international. 2006 Jan:27(1):66-75 [PubMed PMID: 16442033]
Coetzee JC, Hansen ST. Surgical management of severe deformity resulting from posterior tibial tendon dysfunction. Foot & ankle international. 2001 Dec:22(12):944-9 [PubMed PMID: 11783917]
