Introduction
Vertebral compression fractures (VCFs) of the spinal column occur secondary to an axial/compressive (and to a lesser extent, flexion) load with resultant biomechanical failure of the bone resulting in a fracture. VCFs by definition compromise the anterior column of the spine, thereby resulting in compromise to the anterior half of the vertebral body (VB) and the anterior longitudinal ligament (ALL). This leads to the characteristic wedge-shaped deformity. [1][2][3]
VCFs do not involve the posterior half of the VB and do not involve the posterior osseous components or the posterior ligamentous complex (PLC). The former distinguishes a compression fracture from a burst fracture. The implications of these compression fractures are related to the stability of the resulting structure and potential for deformity progression. Compression fractures are usually considered stable and do not require surgical instrumentation.[4][5]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The most common etiology of VCFs is osteoporosis, making these fractures the most common fragility fracture. However, compression fractures demonstrate a bimodal distribution with younger patients sustaining these injuries secondary to high energy mechanisms (fall from a height, MVA, etc.). [6][7][8]
Due to the ligamentous and anatomical changes noted as one travels from the thoracic to the lumbar level, inherent areas of instability make this a frequent site of injury.
For the spinal column, traditional teaching is that the column can be divided into three sections: (1) anterior column (anterior longitudinal ligament, anterior annulus, the anterior portion of the vertebral body, (2) middle column (posterior vertebral body, posterior annulus, and posterior longitudinal ligament), and (3) the posterior column (ligamentum flavum, neural arch, facets, posterior ligamentous complex). If two of these three columns are compromised, the injury is considered unstable, and the patient potentially needs surgery.
Compression fractures by definition only involve compromise to the anterior column alone. Thus, VCFs are considered "stable" fracture patterns. When the fracture pattern involves the middle column they are classified as burst fractures and lack the stability of a VCF.
Epidemiology
VCFs are the most common fragility fracture reported in the literature. Approximately 1- to 1.5 million VCFs occur annually in the United States (US) alone. Based on the age- and sex-adjusted incidence, it is estimated that 25% of women 50 years of age and older have at least one VCF.[9] Moreover, it is estimated that 40% to 50% of patients over age 80 years have sustained a VCF either acutely or recognized incidentally during clinical workup for a separate condition.[10]
Recent reports cite the thoracolumbar junction (i.e., the segment from T12 to L2) as the location afflicted with 60% to 75% of VCFs, and another 30% occur at the L2 to L5 region.
In younger patients, about 50% of spine fractures are due to motor vehicle collisions with another 25% being due to falls.
This is in stark contrast to the elderly mechanism of injury at presentation. Studies have reported an estimate of 30% of VCFs occurring while the patient is in bed. As the population continues to age, the population at risk of sustaining low energy fragility fractures will continue to increase as well. Currently, 10 million Americans are already diagnosed with osteoporosis, and another 34 million have osteopenia. The number of patients aging and having a diagnosis of osteoporosis is projected to rise.[9] Population studies have shown that the annual incidence of VCFs is 10.7 per 1000 women and 5.7 per 1000 men.
Pathophysiology
During a fall or trauma, the spinal column will rotate around a center of axis for this rotation. There is also an associated axial force applied due to this flexion/extension of the spine. An axial force more than the forces tolerable by the vertebral body leads initially to a compression fracture with more significant forces resulting in a burst fracture. The resulting kyphotic (forward flexion of the spine) deformity of the compression fracture may alter the spine biomechanics, placing additional stresses on other spine levels. The altered biomechanics risk additional fractures and progressive deformity. The occurrence of an osteoporotic compression fracture increases the risk of an additional compression fracture.
History and Physical
Initial evaluation of spine fractures, once the patient has been stabilized, includes an evaluation of the neurologic function of the arms, legs, bladder, and bowels. The keys to a thorough exam are organization and patience. Of note, many high-energy compression fractures have associated abdominal, cerebral, and extremity injuries, and these all should be evaluated. One should not only evaluate strength in addition to sensation and reflexes. It is also important to inspect the skin along the back and document the presence of tenderness to palpation. Documentation is paramount as these initial findings will likely be used as a baseline for all future evaluations.
Evaluation
Evaluation of patients with suspected back trauma includes anterior-posterior (AP) and lateral radiographs of the impacted area. In the trauma setting these initially, should be obtained supine with spine precautions until cleared by the spine team or bracing has been provided. At some point, standing radiographs in the brace are helpful to guide treatment as a supine position may artificially reduce a displaced fracture.[11][12][13]
A CT should also be obtained in all trauma settings. If there is a suspected posterior column injury not able to be confirmed on CT, an MRI will indicate disruption of the posterior ligamentous complex. Radiographs showing 30 degrees of traumatic kyphosis (forward flexion of the spine) and 50% vertebral body height loss are historically thought to be unstable fractures, but new evidence is changing this belief. Furthermore, any neurologic deficit necessitates an MRI for additional evaluation. Elderly patients with low energy compression fractures likely will not require an MRI. Serial standing lateral radiographs obtained in the clinic will help track the fracture progression and healing.
Treatment / Management
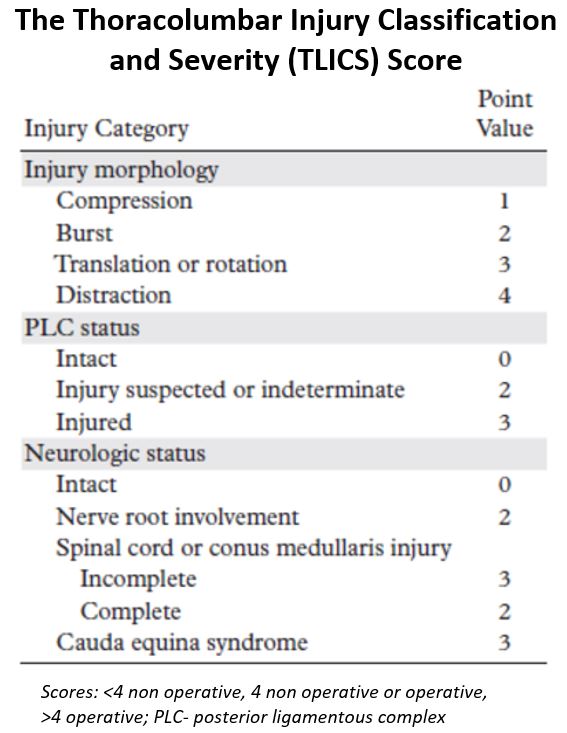
Determining the need for surgery is at times controversial. In 2005, a classification system was introduced to provide more uniformity in management and provide simple treatment recommendations. The Thoracolumbar Injury Classification and Severity (TLICS) Scale uses the integrity of the PLC, injury morphology, and neurological status of the patient to provide a score (one to ten) that can guide intervention: a score less than four leads to non-surgical treatment, greater than four suggests surgical treatment, and a score of four being managed either surgically or nonsurgically depending on the physicians' clinical acumen. Of course, these are general guidelines, predominantly for trauma patients, and each case should be evaluated carefully. Interestingly, newer studies have shown that historical considerations such as loss of vertebral body height, segmental kyphosis, and canal compromise, do not correlate with the need for surgery in neurologically intact patients. Of note, currently, there have been no randomized trials evaluating surgery versus brace treatment in “unstable” compression fractures.[14][15][16][17](B3)
Orthosis/bracing modalities accomplish conservative management for a period of four to 12 weeks. Discontinuation of the bracing can be considered when there is radiographic evidence of healing, and the patient no longer is tender over the fracture site. While midthoracic and upper lumbar VCFs can be treated with a thoracolumbosacral orthosis (TLSO), lower lumbar VCFs may need a lumbosacral corset for adequate immobilization. Bracing is not benign and can be difficult in a barrel-chested patient, a patient with pulmonary compromise or in an obese patient. These factors must be taken into consideration. Analgesic medications and bracing can be poorly tolerated in some patients. If bracing is not effective or poorly tolerated, the physician may alternatively consider percutaneous procedures for stabilization of the fracture.
Surgical options are largely dependent on fracture characteristics and neurologic injury. Rarely would compression fractures require instrumented stabilization. Cement augmentation in the form of vertebroplasty or kyphoplasty is the common surgical considerations for these patients. Initially developed for spinal hemangiomas, vertebroplasty is a minimally invasive procedure during which cement is injected into the vertebral body through the pedicle. Spinal alignment is improved during the procedure by supine positioning with extension; the vertebroplasty itself is not meant to restore alignment. Kyphoplasty is a procedure in which the wedge-shaped vertebra is first reduced to improve the residual local kyphotic alignment through inflation of a balloon; once vertebral height is restored, cement is injected. For patients that have failed a trial of conservative treatment or are hospitalized due to pain and decreased function associated with a VCF, cement augmentation should be considered.[9] Recent randomized controlled trials have shown kyphoplasties allowing for significantly more rapid improvement in the quality of life, function, pain, and mobility.[18](A1)
Differential Diagnosis
When evaluating a patient with back pain and a suspected VCF, several other diagnoses must be excluded. Prior to imaging, one must think of nonspinal etiologies for the pain such as musculoskeletal, pulmonary, abdominal, renal or vascular depending on the location of the pain. If a vertebral body fracture is identified on imaging, a close inspection of the posterior vertebral body cortex and of the posterior spinal column structures must be performed to rule out a more unstable fracture pattern.
Prognosis
In elderly patients with osteoporotic compression fractures, there is an increase in mortality compared with age-matched controlled. Survival rates have been cited to be 53.9% at 3 years, 30.9% at 5 years and 10.5% at 7 years.[19]
Complications
Nonoperative management of these fractures can lead to continued back pain and progression of a kyphotic deformity. There is a high likelihood of patients having a progression of vertebral body collapse in addition to having additional fractures in the future.
With cement augmentation, there have been several complications identified. There have been case reports of neurologic injury during the procedure, but this a rare occurrence. The increased stiffness of a vertebral body filled with cement causes increased stress on the adjacent levels which can lead to secondary fractures. As mentioned above, however, the patients in this population are often at risk for this regardless of operative treatment. Most patients will experience cement extravasation, but this does not seem to have much clinical significance. Embolization of the cement occurs rarely, but it can lead to devastating complications such as pulmonary embolism or stroke.[9]
Pearls and Other Issues
The most important consideration when evaluating fractures of the spine should be the neurologic exam as compression of the spinal canal may alter treatment options. Regarding a kyphoplasty treatment for compression fractures, several contraindications should be remembered. These include current neurologic compromise, burst fractures (fractures of the posterior vertebral body wall), spine infections, current sepsis, or underlying bleeding diatheses. Not addressed above are patients with diffuse idiopathic skeletal hyperostosis (DISH) and ankylosing spondylitis (AS). Both of these result in brittle spinal columns and a fracture of any type should be considered unstable and require CT, MRI, and potentially surgery.
Enhancing Healthcare Team Outcomes
Patients with vertebral fractures are often managed by an interprofessional team that includes an orthopedic nurse specialist, emergency department physician, neurologist, radiologist, neurosurgeon, physical therapist, and an intensivist. All patients with severe injuries and neurological deficits are monitored in the ICU by trauma nurses. Complications should be discussed and reported to the team. Mild injuries may be managed with conservative care but severe injuries with neurological deficits may require surgery. Due to the pain involved, the pharmacist should assist with pain management medication selection and monitoring for clinical effect. The prognosis of these patients is dependent on age, type and extent of the injury, other associated injuries, the presence of neurological deficits and the need for mechanical ventilation.[20][21] (Level V)
Media
(Click Image to Enlarge)
References
Urrutia J,Besa P,Piza C, Incidental identification of vertebral compression fractures in patients over 60 years old using computed tomography scans showing the entire thoraco-lumbar spine. Archives of orthopaedic and trauma surgery. 2019 Nov [PubMed PMID: 30900019]
Liu J,Liu Z,Luo J,Gong L,Cui Y,Song Q,Xiao PF,Zhou Y, Influence of vertebral bone mineral density on total dispersion volume of bone cement in vertebroplasty. Medicine. 2019 Mar [PubMed PMID: 30896660]
Shi G,Feng F,Hao C,Pu J,Li B,Tang H, A case of multilevel percutaneous vertebroplasty for vertebral metastases resulting in temporary paraparesis. The Journal of international medical research. 2020 Feb [PubMed PMID: 30880529]
Level 3 (low-level) evidenceChen YC,Zhang L,Li EN,Ding LX,Zhang GA,Hou Y,Yuan W, Unilateral versus bilateral percutaneous vertebroplasty for osteoporotic vertebral compression fractures in elderly patients: A meta-analysis. Medicine. 2019 Feb; [PubMed PMID: 30813133]
Level 1 (high-level) evidenceClerk-Lamalice O,Beall DP,Ong K,Lorio MP, ISASS Policy 2018-Vertebral Augmentation: Coverage Indications, Limitations, and/or Medical Necessity. International journal of spine surgery. 2019 Jan; [PubMed PMID: 30805279]
Maempel JF,Maempel FZ, The speedboat vertebral fracture: a hazard of holiday watersports. Scottish medical journal. 2018 Nov 14; [PubMed PMID: 30426854]
Zarghooni K,Hopf S,Eysel P, [Management of osseous complications in multiple myeloma]. Der Internist. 2019 Jan [PubMed PMID: 30560368]
Donnally CJ 3rd,Rivera S,Rush AJ 3rd,Bondar KJ,Boden AL,Wang MY, The 100 most influential spine fracture publications. Journal of spine surgery (Hong Kong). 2019 Mar; [PubMed PMID: 31032444]
Savage JW,Schroeder GD,Anderson PA, Vertebroplasty and kyphoplasty for the treatment of osteoporotic vertebral compression fractures. The Journal of the American Academy of Orthopaedic Surgeons. 2014 Oct [PubMed PMID: 25281260]
Kim HJ,Park S,Park SH,Park J,Chang BS,Lee CK,Yeom JS, Prevalence of Frailty in Patients with Osteoporotic Vertebral Compression Fracture and Its Association with Numbers of Fractures. Yonsei medical journal. 2018 Mar [PubMed PMID: 29436202]
Expert Panels on Neurological Imaging, Interventional Radiology, and Musculoskeletal Imaging:, Shah LM, Jennings JW, Kirsch CFE, Hohenwalter EJ, Beaman FD, Cassidy RC, Johnson MM, Kendi AT, Lo SS, Reitman C, Sahgal A, Scheidt MJ, Schramm K, Wessell DE, Kransdorf MJ, Lorenz JM, Bykowski J. ACR Appropriateness Criteria(®) Management of Vertebral Compression Fractures. Journal of the American College of Radiology : JACR. 2018 Nov:15(11S):S347-S364. doi: 10.1016/j.jacr.2018.09.019. Epub [PubMed PMID: 30392604]
Acaroğlu E,Nordin M,Randhawa K,Chou R,Côté P,Mmopelwa T,Haldeman S, The Global Spine Care Initiative: a summary of guidelines on invasive interventions for the management of persistent and disabling spinal pain in low- and middle-income communities. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2018 Sep; [PubMed PMID: 29322309]
Musbahi O,Ali AM,Hassany H,Mobasheri R, Vertebral compression fractures. British journal of hospital medicine (London, England : 2005). 2018 Jan 2; [PubMed PMID: 29315051]
Alpantaki K,Dohm M,Korovessis P,Hadjipavlou AG, Surgical options for osteoporotic vertebral compression fractures complicated with spinal deformity and neurologic deficit. Injury. 2018 Feb [PubMed PMID: 29150315]
Bernardo WM,Anhesini M,Buzzini R,Brazilian Medical Association (AMB)., Osteoporotic vertebral compression fracture - Treatment with kyphoplasty and vertebroplasty. Revista da Associacao Medica Brasileira (1992). 2018 Mar [PubMed PMID: 29641781]
Parreira PCS,Maher CG,Megale RZ,March L,Ferreira ML, An overview of clinical guidelines for the management of vertebral compression fracture: a systematic review. The spine journal : official journal of the North American Spine Society. 2017 Dec [PubMed PMID: 28739478]
Level 3 (low-level) evidenceGenev IK,Tobin MK,Zaidi SP,Khan SR,Amirouche FML,Mehta AI, Spinal Compression Fracture Management: A Review of Current Treatment Strategies and Possible Future Avenues. Global spine journal. 2017 Feb; [PubMed PMID: 28451512]
Anderson PA,Froyshteter AB,Tontz WL Jr, Meta-analysis of vertebral augmentation compared with conservative treatment for osteoporotic spinal fractures. Journal of bone and mineral research : the official journal of the American Society for Bone and Mineral Research. 2013 Feb [PubMed PMID: 22991246]
Level 1 (high-level) evidenceLau E,Ong K,Kurtz S,Schmier J,Edidin A, Mortality following the diagnosis of a vertebral compression fracture in the Medicare population. The Journal of bone and joint surgery. American volume. 2008 Jul [PubMed PMID: 18594096]
Level 2 (mid-level) evidenceWatanabe Y,Ishikawa S,Nagata H,Kojima M, Determinants Associated with Prolonged Hospital Stays for Patients Aged 65 Years or Older with a Vertebral Compression Fracture in a Rural Hospital in Japan. The Tohoku journal of experimental medicine. 2019 Jan; [PubMed PMID: 30651405]
Crouser N,Malik AT,Jain N,Yu E,Kim J,Khan SN, Discharge to Inpatient Care Facility After Vertebroplasty/Kyphoplasty: Incidence, Risk Factors, and Postdischarge Outcomes. World neurosurgery. 2018 Oct [PubMed PMID: 30257300]