Introduction
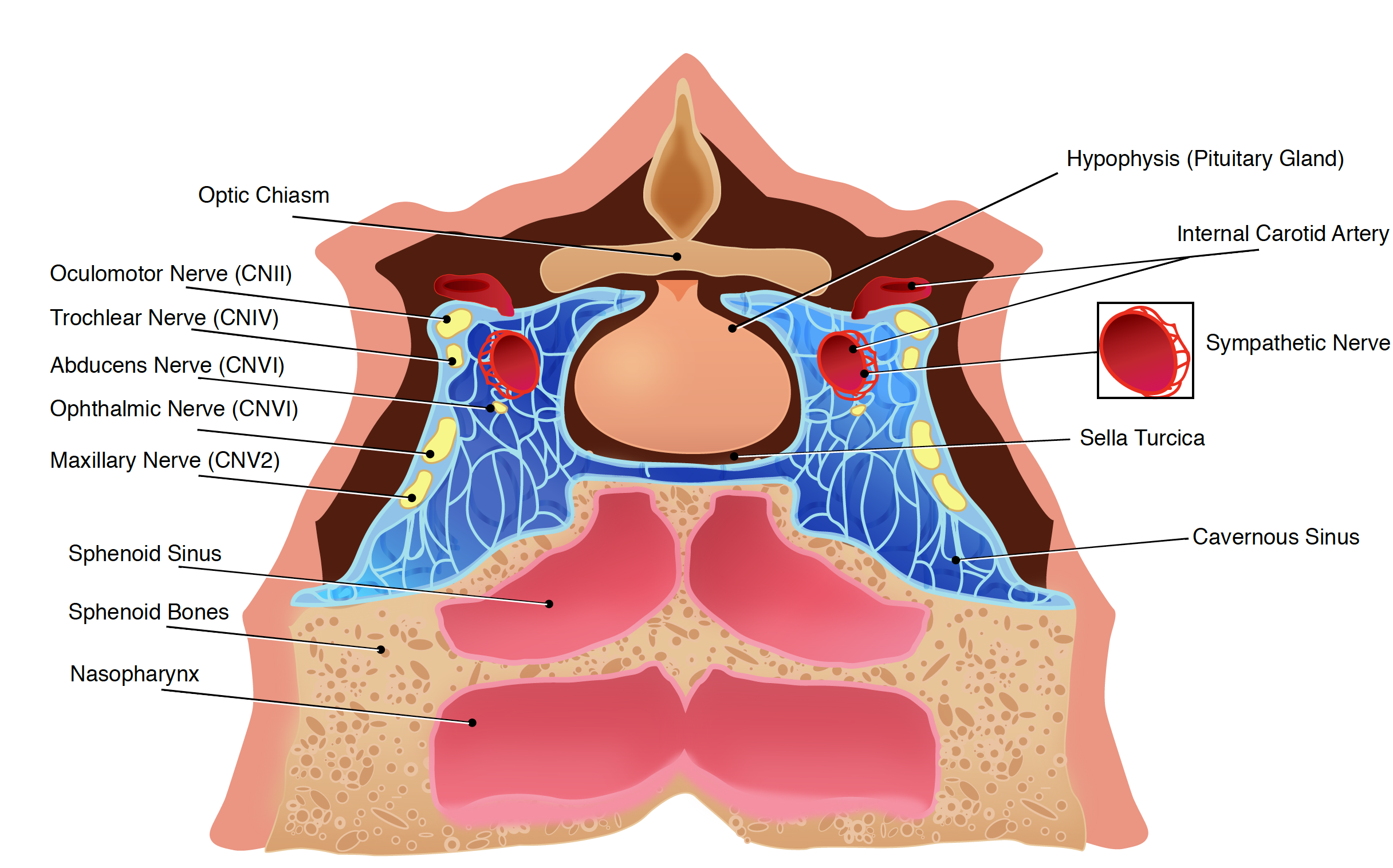
Understanding the clinical management of cavernous sinus syndrome (CCS) requires an extensive understanding of its anatomy. It is a small but complex, and it contains several important structures. The cavernous sinus (CS) is not a venous plexus, but it is a true dural venous sinus.[1] It is bordered by the temporal bone of the skull and the sphenoid bone and lies lateral to the sella turcica. The inferior and lateral walls and the roof of CS are extensions of the dura mater. There may or may not be a thin layer of collagen at the medial wall. The blood-filled space contains the internal carotid artery (carotid siphon) surrounded by sympathetic fibers, as well as cranial nerves (CN). In particular, CN III (oculomotor nerve), IV (trochlear nerve), 2 branches of the V (trigeminal nerve): V1 (ophthalmic) and V2 (maxillary), all pass through this blood-filled space (Figure "Anatomy of the cavernous sinus").[2] Cavernous sinus syndrome is any disease process involving the CS. CCA is characterized by signs and symptoms resulting in ophthalmoplegia, chemosis, proptosis, Horner syndrome, or trigeminal sensory loss.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Determining the etiology of CCS remains difficult, despite the improvement of diagnostic techniques including improvements in imaging and analysis of blood and CSD. It is also difficult to make a diagnosis from CS tissue. Neoplastic (metastatic vs. primary), infectious, inflammatory, vascular, and traumatic processes are the principal causes of CCS. Jefferson first classified the disorder in 1938 into 3 types: anterior, middle, and posterior CCS. This classification is based on the extent of involvement of the trigeminal nerve. In 1996, Ishikawa emphasized the lack of a clinical-anatomical correlation in Jefferson's classification and proposed a new classification of CCS. CCS was classified into 3 separated part such as the anterior, middle, posterior by Ishikawa. They used the optic canal and the maxillary nerve as anatomical landmarks. The Ishikawa classification in a study with 162 patients with CS lesions was shown to be superior in identifying and classifying the localization of CS lesions.[3] However, Ishikawa classification is not superior to Jefferson based on etiology, shown by a study at a tertiary care center in Northern India with 73 consecutive CCS patients.[4]
Epidemiology
Estimates of the incidence of CCS are not well documented in the literature. An analysis of 151 cases from Los Angeles in 1996[5] showed 89 (59%) were men. The average age was 39 years, with a range of 15 to 72 years. The tumor is the most common cause of CCS at 30%, followed by trauma at 24%. Other series excluded trauma as a cause of CCS. A series of 126 patients from Barcelona, Spain in 2007[6] showed that 42% were men. The average age was 55.5 with a range of 40 to 70 years. Tumor, again, being the most common cause of CCS with at 63%. According to this study, the second most common cause is of vascular etiology at 20%. In a 2017 study of 73 cases at tertiary care centers in Northern India showed that 64% were men. The average age was 44 years, with a range of 11 to 70 years. The tumor was still the most common cause of CCS at 30%, but unlike previously described series from the Western world, the prevalence of fungal infections was 24.6%, and the prevalence of Tolosa-Hunt syndrome (THS) was also much higher at 23.2%.[7] Overall, CCS was not predominant in any gender. Patients may present at any age, ranging from 20 to 80 years of age.
Pathophysiology
Cavernous Sinus Tumors
- Tumors were the most frequent cause of CCS as previously mentioned
- Tumors may be primary or metastatic and have a wide differential, including meningiomas, schwannomas of CN III, IV, V1/V2 (the most common) or VI, haemangiomas, haemangiopericytomas, and metastatic disease (i.e., the perineural spread of tumor through neural foramina) from lung, breast or prostate.
- Tumors also may arise from either a pituitary tumor or by locally spreading, such as nasopharyngeal carcinoma with intracranial extension (more in Southeast Asia).[8]
Cavernous sinus vascular pathologies; vascular pathologies in the CS include carotid-cavernous fistulas (CCFs), carotid-cavernous aneurysms (CCAs), and cavernous sinus thrombosis (CST)
- CCAs do not carry a major risk of subarachnoid hemorrhage. CCFs may arise spontaneously or from secondary causes such as trauma, CCAs, and venous thrombosis.
- CCFs can be classified as indirect, low-flow, or dural CCFs (an indirect communication between the cavernous sinus and branches of the internal or external carotid artery within the adjacent dura). They can also be classified as being direct or high-flow CCFs (a direct connection between the intracavernous carotid artery and the cavernous sinus).[9]
- The causes of CST are aseptic or infectious. Infections can spread from a nasal furuncle (50%), sphenoidal or ethmoidal sinus, (30%) as well as dental infections (10%). Aseptic causes typically occur after surgery or trauma. The most common causative microorganism is Staphylococcus aureus, followed by milleri group streptococci which include Streptococcus constellatus, Streptococcus intermedius, and Streptococcus anginosus. Septic cavernous sinus thrombosis is a rare but serious complication of cavernous sinus infections.[10]
Infections
- Bacterial infection sources are explained above. One patient with tuberculosis is also reported.
- Fungal infection is the second common cause of CCS in Northern India. Out of 18 fungal infections, Aspergillosis accounted for 44.4%, mucormycosis accounted for 22.2%, and other fungal infections accounted for 33.3%.[7]
Inflammation
- An inflammatory process of unknown etiology causes Tolosa-Hunt syndrome. Inflammation causes swelling, pressure and then dysfunction of the structures, particularly of the CN.
- Sarcoid or Wegener granulomatosis can also predispose to cavernous sinus syndrome.
- Herpes zoster can cause inflammation.
History and Physical
Complaints that occur in different etiologies of SSC share common symptoms such as a headache (up to 90%), diplopia (up to 90%), painless or painful ophthalmoplegia, ptosis, proptosis, chemosis, facial sensory loss, visual loss, fever, facial asymmetry, hearing loss, and seizure. Assessment should include a determination of whether symptoms are unilateral or bilateral, and if the onset of symptoms is acute, subacute, or chronic, and if conditions are painful or painless.
Physical exam findings depend on the etiology as well as the extent of CS involvement. The following sign(s) may be seen in patients with CCS:
- Involvement of cranial nerves with motor and/or sensory findings: the most common are CN III (85%), VI (70%), V1 and/or V2, and IV
- Reflexes: Decreased or absent corneal, direct and/or indirect light reflexes
- Ophthalmoplegia, painful or painless
- Chemosis, the swelling (or edema) of the conjunctiva
- Proptosis, protrusion or displacement of an eye
- Ocular and cranial bruits
- Funduscopic findings: Papilledema, pallor and/or retinal hemorrhages
- Visual problems: Visual field cut, blurry vision, diplopia and/or vision loss
Common symptoms and signs on presentation can usually accompany the specific etiologies below:
- Cavernous sinus tumors may cause isolated or combined ophthalmoplegia, painful ophthalmoplegia, anesthesia in CNIII, unitemporal or bitemporal visual field defects, acromegaly, and galactorrhea.
- Carotid-cavernous fistulas may cause ocular bruit (auscultated over the globe in high-flow CCFs), proptosis, chemosis, and conjunctival injection, ocular and/or orbital pain, headache, diplopia, blurry vision.
- Cavernous sinus thrombosis may present signs of an infectious process involving paranasal sinuses and/or orbital cellulitis, conjunctival injection, chemosis, proptosis.
- Tolosa-Hunt syndrome may cause typically unilateral (bilateral symptoms 4% to 5%)[11], painful ophthalmoplegia, diplopia from cranial mono- or polyneuropathy (the most common CNIII), Horner syndrome if the involvement of periarterial sympathetic fibers.[12]
- Sarcoidosis may cause systemic signs, uveitis, ophthalmoplegia, and facial diplegia.
- Herpes zoster also may present with acute zoster ophthalmicus, typical skin lesion, and keratitis.
Evaluation
The diagnosis of CSS is challenging because of a wide variety of possible etiologies. Studies of the orbit, sella, and parasellar region play a major role in making a diagnosis. Precontrast and postcontrast scans are advisable. Contrast-enhanced computed tomography (CT) scans give a better visualization of bone and calcium. Magnetic resonance imaging (MRI) provides better detail of all soft tissues contained in the sinuses. CT angiography (CTA), CT venography (CTV) magnetic resonance angiography (MRA), MR venography (MRV) and conventional digital subtraction angiography helps to visualize all vascular structures with details. Routine, cytologic, infectious, and/or inflammatory examinations of serum and cerebral spinal fluid (CSF) may be helpful as well.
Cavernous Sinus Tumors
- To find out a source of mass. Is it primary, metastasis or local spread?
- CT, MRI and chest/abdomen/pelvic CT
- A lumbar puncture with cytologic examination
- A biopsy of the cavernous sinus tumors is rarely needed for diagnosis of primary tumors if no tumors are spreading from another primary source.
Cavernous Sinus Vascular
- Vascular etiologies can be seen on CTA, MRI, MRA and angiography.
- Conventional digital subtraction angiography is the gold-standard test for diagnosis of CCF. CCFs can be seen on an orbital or trans-cranial ultrasound as well.
- Intraocular pressure should be checked on patients with ocular sequelae.
- Infectious workup, D-dimer and MRV or CTV should be performed if there is a suspicion for CST.
- An aseptic thrombosis may be associated with hypercoagulable states as well as lymphoproliferative disorders. The patient may need further hematological workup.
Infections
- To do further infectious workup with RPR, HIV, fluorescent treponemal antibody test, Lyme serology, Quantiferon-TB gold test, cultures for bacteria, fungi, and mycobacteria in serum.
- Order workup with protein, glucose, cell counts, cytology, Lyme and syphilis serology in cerebrospinal (CSF).
Inflammation
- Investigate additional systemic inflammatory and granulomatous processes after other common causes have been excluded such as those from a tumor or vascular etiology.
- Workup should include an erythrocyte sedimentation rate, C-reactive protein, angiotensin converting enzyme, antinuclear antibody, anti-dsDNA antibody, anti-Sm antibody, anti-neutrophil cytoplasmic antibody, serum protein electrophoresis with immunotyping from serum, CSF protein, glucose, cell counts, cytology, and angiotensin-converting enzyme.
- The specific diagnostic criteria of THS recommended by the International Headache Society are summarized. A unilateral headache localized around the ipsilateral brow and eye, oculomotor paresis for less than 2 weeks, granulomatous inflammation of the cavernous sinus, superior orbital fissure or orbit, established by MRI or biopsy, paresis of one or more of the ipsilateral CN III, IV, and/or VI and symptoms not accounted for by an alternative diagnosis. [11] Glucocorticoid administration has diagnostic as well as therapeutic utility.
Treatment / Management
Cavernous Sinus Tumors
- Tumors in CS represent a major challenge for surgical resection because of their proximity to critical neurologic structures making it difficult for complete excision or leaving a high risk of complications with surgical resection. Radiotherapy is important in providing excellent tumor control and avoiding the risk of surgery.[13]
- About 400 patients with cavernous sinus meningiomas treated with stereotactic radiosurgery in three large series from a dose of 12 to 14 Gy resulted in a five-year tumor control rate ranging from 94 to 98 percent.[14][15][16]
- Transsphenoidal surgery is the preferred treatment for most kinds of pituitary adenomas. Gamma knife surgery (GKS) is a common treatment for recurrent or residual pituitary adenomas.[17]
- Radiotherapy may offer transient relief, particularly in nasopharyngeal cancer.
- Whole radiotherapy may offer a transient improvement of metastatic lesions. (B2)
Cavernous Sinus Vascular
- Carotid-cavernous aneurysms have the lowest rates of rupture is shown for unruptured cerebral aneurysms in a Japanese cohort.[18]
- Unruptured intracranial aneurysms treatment has been evaluated by a 2003 ISUIA performing cost-effectiveness analyzes that showed treatment was ineffective or not cost-effective for large aneurysms (greater than 25 mm) and located in the cavernous carotid artery for 40-year-old patients.[19]
- The management of CCFs depends on the classification of CCFs, the onset of symptoms, and the risk of long-term neurological impairment. Most of (20% to 60%)indirect CCFs will close spontaneously.[20] Direct CCFs should be closed if symptomatic and at risk of progression with attendant morbidity because these CCFs are unlikely to close spontaneously.
- Endovascular treatment with trans-arterial or transvenous embolization is the preferred approach for closure of CCFs.
- Surgery can be considered when endovascular treatment is not possible or is unsuccessful. Surgery includes placement of packing, sealing with fascia and glue, suturing or clipping the fistula.
- Stereotactic radiosurgery is indicated when an endovascular approach is not feasible, and surgical intervention is difficult or carries a risk of significant morbidity.[21]
- The management of increased intraocular pressure with topical agents, beta-blockers, acetazolamide, and intravenous corticosteroids may give some relief. If vision loss is threatened or intraocular pressure remains elevated, closure of the fistula required for favorable pressure control.
- The management of CST should include antimicrobial with/without surgical drainage of the air sinuses or mastoid regions and antithrombotic therapies.
- Patient with CST should be treated for 3 to 4 weeks with intravenous antibiotic(s) or somites 6 to 7 weeks on the clinical picture. Treatment should be broad-spectrum with vancomycin vs. nafcillin plus a third-generation cephalosporin plus metronidazole until a definite pathogen.[22] Antifungal therapy with Amphotericin-B is required in the developing countries.
- Retrospective analysis suggests that treatment with heparin may reduce mortality in carefully selected cases of septic cavernous-sinus thrombosis.[23]
- Steroids in the acute phase of cerebral venous thrombosis (CVT) were not useful and were detrimental in patients without parenchymal cerebral lesions. These results do not support the use of steroids in CVT (evidence level III) in the International Study on Cerebral Veins and Dural Sinus Thrombosis (ISCVT).[24] The potential benefit of using the corticosteroid on CST would be decreased inflammation and vasogenic edema surrounding cranial nerves and orbital structures. (B2)
Inflammation
- Glucocorticoids have been used for the management of THS since the 1960s.[25] Initial high-dose glucocorticoids for two to four weeks followed by a gradual taper for at least 4 to 6 weeks up to several months. Close clinical follow-up with repeat MRI every 1 to 2 months is necessary to be sure followed by a gradual taper for at least 4 to 6 weeks up to several months. Close clinical follow-up with repeat MRI, 1 to 2 months, is necessary to be sure the glucocorticoid treatment remains effective, and no evidence of another etiology develops, as seen in a case report showing the progression of THS to a CCF.[26][27]
- Radiotherapy and immunosuppressive medications like cyclosporine, azathioprine, methotrexate, mycophenolate mofetil, and infliximab have been tried in many case reports with benefits.[28][29][30]
- Other inflammatory CCS may respond to treatment of the specific systemic inflammation or vasculitis etiology. (B2)
Differential Diagnosis
- Carotid-cavernous aneurysms
- Carotid-cavernous fistulas
- Cavernous sinus thrombosis
- Chondromas
- Herpes zoster
- Lymphomas
- Meningiomas
- Neurofibromas
- Sarcoidosis
- Tuberculosis
Enhancing Healthcare Team Outcomes
CSS are difficult to diagnose and manage. Because there are many causes of CSS, they are best managed by an interprofessional team that includes a specialty trained neurology nurse, neurologist, ophthalmologist, neurosurgeon, radiologist, internist, ENT surgeon, and an infectious disease specialist. The majority of these patients require monitoring by the ICU nurse. The treatment of SCC depends on the cause. Because of the vast number of structures that run in the cavernous sinus, some type of residual visual and neurological deficit may persist after treatment.
Media
References
Yasuda A, Campero A, Martins C, Rhoton AL Jr, de Oliveira E, Ribas GC. Microsurgical anatomy and approaches to the cavernous sinus. Neurosurgery. 2008 Jun:62(6 Suppl 3):1240-63. doi: 10.1227/01.neu.0000333790.90972.59. Epub [PubMed PMID: 18695545]
Charbonneau F, Williams M, Lafitte F, Héran F. No more fear of the cavernous sinuses! Diagnostic and interventional imaging. 2013 Oct:94(10):1003-16. doi: 10.1016/j.diii.2013.08.012. Epub 2013 Oct 5 [PubMed PMID: 24099909]
Yoshihara M, Saito N, Kashima Y, Ishikawa H. The Ishikawa classification of cavernous sinus lesions by clinico-anatomical findings. Japanese journal of ophthalmology. 2001 Jul-Aug:45(4):420-4 [PubMed PMID: 11485777]
Bhatkar S, Goyal MK, Takkar A, Modi M, Mukherjee KK, Singh P, Radotra BD, Singh R, Lal V. Which Classification of Cavernous Sinus Syndrome is Better - Ishikawa or Jefferson? A Prospective Study of 73 Patients. Journal of neurosciences in rural practice. 2016 Dec:7(Suppl 1):S68-S71. doi: 10.4103/0976-3147.196448. Epub [PubMed PMID: 28163507]
Keane JR. Cavernous sinus syndrome. Analysis of 151 cases. Archives of neurology. 1996 Oct:53(10):967-71 [PubMed PMID: 8859057]
Level 3 (low-level) evidenceFernández S, Godino O, Martínez-Yélamos S, Mesa E, Arruga J, Ramón JM, Acebes JJ, Rubio F. Cavernous sinus syndrome: a series of 126 patients. Medicine. 2007 Sep:86(5):278-281. doi: 10.1097/MD.0b013e318156c67f. Epub [PubMed PMID: 17873757]
Bhatkar S, Goyal MK, Takkar A, Mukherjee KK, Singh P, Singh R, Lal V. Cavernous sinus syndrome: A prospective study of 73 cases at a tertiary care centre in Northern India. Clinical neurology and neurosurgery. 2017 Apr:155():63-69. doi: 10.1016/j.clineuro.2017.02.017. Epub 2017 Feb 22 [PubMed PMID: 28260625]
Level 3 (low-level) evidenceAzarpira N, Taghipour M, Pourjebely M. Nasopharyngeal carcinoma with skull base erosion cytologic findings. Iranian Red Crescent medical journal. 2012 Aug:14(8):492-4 [PubMed PMID: 23105987]
Level 3 (low-level) evidenceBarrow DL, Spector RH, Braun IF, Landman JA, Tindall SC, Tindall GT. Classification and treatment of spontaneous carotid-cavernous sinus fistulas. Journal of neurosurgery. 1985 Feb:62(2):248-56 [PubMed PMID: 3968564]
Weerasinghe D, Lueck CJ. Septic Cavernous Sinus Thrombosis: Case Report and Review of the Literature. Neuro-ophthalmology (Aeolus Press). 2016 Dec:40(6):263-276 [PubMed PMID: 27928417]
Level 3 (low-level) evidenceZhang X, Zhou Z, Steiner TJ, Zhang W, Liu R, Dong Z, Wang X, Wang R, Yu S. Validation of ICHD-3 beta diagnostic criteria for 13.7 Tolosa-Hunt syndrome: Analysis of 77 cases of painful ophthalmoplegia. Cephalalgia : an international journal of headache. 2014 Jul:34(8):624-32. doi: 10.1177/0333102413520082. Epub 2014 Jan 29 [PubMed PMID: 24477599]
Level 2 (mid-level) evidenceCakirer S. MRI findings in Tolosa-Hunt syndrome before and after systemic corticosteroid therapy. European journal of radiology. 2003 Feb:45(2):83-90 [PubMed PMID: 12536085]
Pollock BE, Stafford SL, Link MJ, Garces YI, Foote RL. Single-fraction radiosurgery for presumed intracranial meningiomas: efficacy and complications from a 22-year experience. International journal of radiation oncology, biology, physics. 2012 Aug 1:83(5):1414-8. doi: 10.1016/j.ijrobp.2011.10.033. Epub 2011 Dec 29 [PubMed PMID: 22209154]
Level 2 (mid-level) evidenceLee JY, Niranjan A, McInerney J, Kondziolka D, Flickinger JC, Lunsford LD. Stereotactic radiosurgery providing long-term tumor control of cavernous sinus meningiomas. Journal of neurosurgery. 2002 Jul:97(1):65-72 [PubMed PMID: 12134934]
Level 2 (mid-level) evidenceNicolato A, Foroni R, Alessandrini F, Bricolo A, Gerosa M. Radiosurgical treatment of cavernous sinus meningiomas: experience with 122 treated patients. Neurosurgery. 2002 Nov:51(5):1153-9; discussion 1159-61 [PubMed PMID: 12383360]
Spiegelmann R, Cohen ZR, Nissim O, Alezra D, Pfeffer R. Cavernous sinus meningiomas: a large LINAC radiosurgery series. Journal of neuro-oncology. 2010 Jun:98(2):195-202. doi: 10.1007/s11060-010-0173-1. Epub 2010 Apr 20 [PubMed PMID: 20405308]
Level 2 (mid-level) evidenceSheehan JP,Pouratian N,Steiner L,Laws ER,Vance ML, Gamma Knife surgery for pituitary adenomas: factors related to radiological and endocrine outcomes. Journal of neurosurgery. 2011 Feb [PubMed PMID: 20540596]
UCAS Japan Investigators, Morita A, Kirino T, Hashi K, Aoki N, Fukuhara S, Hashimoto N, Nakayama T, Sakai M, Teramoto A, Tominari S, Yoshimoto T. The natural course of unruptured cerebral aneurysms in a Japanese cohort. The New England journal of medicine. 2012 Jun 28:366(26):2474-82. doi: 10.1056/NEJMoa1113260. Epub [PubMed PMID: 22738097]
Wiebers DO, Whisnant JP, Huston J 3rd, Meissner I, Brown RD Jr, Piepgras DG, Forbes GS, Thielen K, Nichols D, O'Fallon WM, Peacock J, Jaeger L, Kassell NF, Kongable-Beckman GL, Torner JC, International Study of Unruptured Intracranial Aneurysms Investigators. Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet (London, England). 2003 Jul 12:362(9378):103-10 [PubMed PMID: 12867109]
Level 2 (mid-level) evidencede Keizer R. Carotid-cavernous and orbital arteriovenous fistulas: ocular features, diagnostic and hemodynamic considerations in relation to visual impairment and morbidity. Orbit (Amsterdam, Netherlands). 2003 Jun:22(2):121-42 [PubMed PMID: 12789591]
O'Leary S, Hodgson TJ, Coley SC, Kemeny AA, Radatz MW. Intracranial dural arteriovenous malformations: results of stereotactic radiosurgery in 17 patients. Clinical oncology (Royal College of Radiologists (Great Britain)). 2002 Apr:14(2):97-102 [PubMed PMID: 12069135]
Desa V, Green R. Cavernous sinus thrombosis: current therapy. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2012 Sep:70(9):2085-91. doi: 10.1016/j.joms.2011.09.048. Epub 2012 Feb 9 [PubMed PMID: 22326173]
Level 3 (low-level) evidenceSouthwick FS, Richardson EP Jr, Swartz MN. Septic thrombosis of the dural venous sinuses. Medicine. 1986 Mar:65(2):82-106 [PubMed PMID: 3512953]
Level 3 (low-level) evidenceCanhão P, Cortesão A, Cabral M, Ferro JM, Stam J, Bousser MG, Barinagarrementeria F, ISCVT Investigators. Are steroids useful to treat cerebral venous thrombosis? Stroke. 2008 Jan:39(1):105-10 [PubMed PMID: 18063833]
Level 2 (mid-level) evidenceHUNT WE, MEAGHER JN, LEFEVER HE, ZEMAN W. Painful opthalmoplegia. Its relation to indolent inflammation of the carvernous sinus. Neurology. 1961 Jan:11():56-62 [PubMed PMID: 13716871]
Zurawski J, Akhondi H. Tolosa-Hunt syndrome--a rare cause of headache and ophthalmoplegia. Lancet (London, England). 2013 Sep 7:382(9895):912. doi: 10.1016/S0140-6736(13)61442-7. Epub [PubMed PMID: 24012271]
Level 3 (low-level) evidenceSugano H, Iizuka Y, Arai H, Sato K. Progression of Tolosa-Hunt syndrome to a cavernous dural arteriovenous fistula: a case report. Headache. 2003 Feb:43(2):122-6 [PubMed PMID: 12558766]
Level 3 (low-level) evidenceWilmut I, Haley CS, Simons JP, Webb R. The potential role of molecular genetic manipulation in the improvement of reproductive performance. Journal of reproduction and fertility. Supplement. 1992:45():157-73 [PubMed PMID: 1304029]
Level 3 (low-level) evidenceSmith JR, Rosenbaum JT. A role for methotrexate in the management of non-infectious orbital inflammatory disease. The British journal of ophthalmology. 2001 Oct:85(10):1220-4 [PubMed PMID: 11567968]
Level 2 (mid-level) evidenceHalabi T, Sawaya R. Successful Treatment of Tolosa-Hunt Syndrome after a Single Infusion of Infliximab. Journal of clinical neurology (Seoul, Korea). 2018 Jan:14(1):126-127. doi: 10.3988/jcn.2018.14.1.126. Epub [PubMed PMID: 29629550]