Introduction
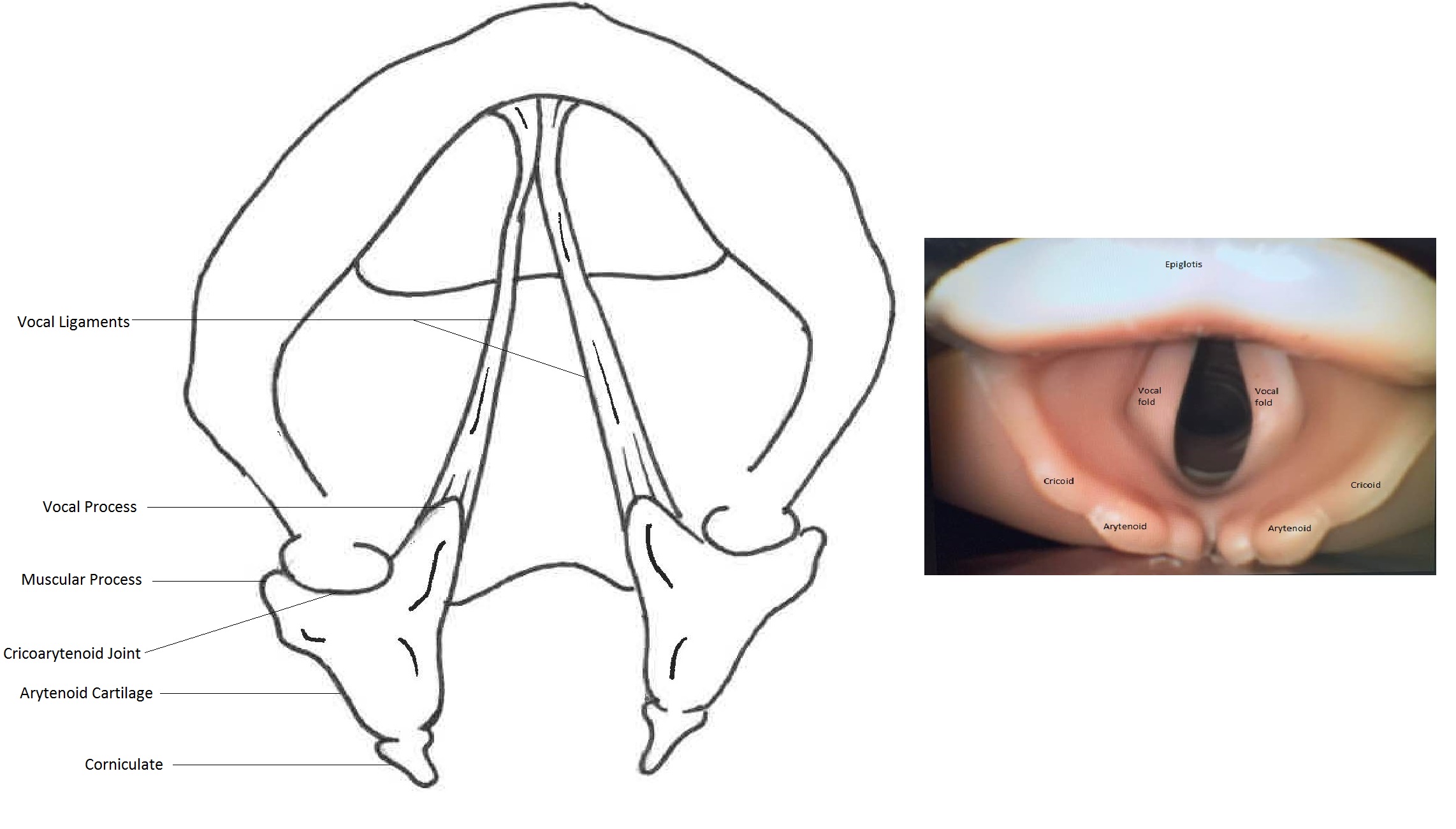
Arytenoid subluxation is partial displacement of the arytenoid cartilage within the cricoarytenoid joint. It is a rare complication that typically occurs after a traumatic injury to the cricoarytenoid junction during laryngoscopy and intubation, upper airway instrumentation, and external laryngeal trauma.[1][2][3][4] The arytenoids are a pair of small pyramid-shaped cartilages which articulate with the cricoid cartilage at the cricoarytenoid joint.[5] Both the arytenoids and cricoarytenoid joints are relatively fragile and very vulnerable to injury during laryngoscopy and intubation. Clinicians commonly visualize the bulge in the mucosal surface overlying the arytenoids during laryngoscopy. [Figure 1]
The arytenoids are composed of an apex, a base, and two processes (vocal and muscular). The vocal processes extend anteriorly and provide attachment to the vocal ligament, and are responsible for tension, relaxation, or approximation of vocal folds, while the muscular processes extend posterolaterally and provide a point of insertion for the lateral and posterior cricoarytenoid muscles. These muscles are responsible for opening and closing the glottis by creating lateral and medial movements of the attached vocal cords. The apex articulates with the aryepiglottic fold and corniculate cartilages, and the base articulates with the cricoid cartilage through several ligaments that form the capsule of the synovial cricoarytenoid joint. The cricoarytenoid joint controls the abduction and adduction of the true vocal cords, allowing respiration, phonation, and airway protection.[5][6]
One often sees the terms subluxation and dislocation used interchangeably. However, a dislocation refers to a complete separation of the arytenoid cartilage from the joint space, whereas a subluxation is partial displacement of the arytenoid within the joint. Both can be considered the same disease with varying degrees of severity, sharing the same pathophysiology. A subluxation can be classified as anterior when the displacement is anteromedial or posterior when the displacement is posterolateral.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Arytenoid subluxation is usually related to acute traumatic events to the cricoarytenoid junction. Protrusion of an endotracheal tube stylet, an unanticipated difficult airway leading to prolonged or traumatic intubations, the use of a gum elastic bougie, blind intubation techniques (e.g., utilization of a lighted stylet or light-wand) and insertion of bulky double-lumen tubes, have all been implicated.[7][8][9][10] The degree of experience of the laryngoscopist, dental malocclusion, retrognathia, and a large tongue may also play a role. There are also reports of severe cough and even spontaneous arytenoid dislocation.[11][12][13]
Several systemic diseases, as well as chronic corticosteroid use, laryngomalacia, and acromegaly may lead to the weakening of the cricoarytenoid joint capsule, thus exacerbating this complication.[14] An elevated BMI might be an independent risk factor, and major cardiac surgery involving the use of transesophageal echocardiography (TEE) probe may also be a possible explanation for the increased incidence.[15] Insertion of the TEE probe is the likely inciting event in these cases.[16]
Epidemiology
The incidence of arytenoid subluxation after endotracheal intubation has been reported to be between 0.01% and 0.1%.[17][4][18] Although the reported incidence suggests that it is rare, the true incidence may be higher. Rudert et al. reported a much higher incidence of 30% in his case series of patients referred to him with prolonged hoarseness following instrumentation of the larynx; 80% to 90% of all cases were related to intubation trauma.[19]
Although it occurs most frequently in adults, arytenoid subluxation/dislocation has been described in children and neonates as well.[20][21][22]
Pathophysiology
As the arytenoid is extremely mobile with a small oval articulating surface, it is vulnerable to displacement from its normal position during intubation. In fact, even slight pressure from the tip of the endotracheal tube directed toward the cricoarytenoid joint is enough to cause anteromedial displacement, dislocating the cartilage.[1][22] Difficult (prolonged and traumatic) intubation is, therefore, a significant risk factor for arytenoid subluxation or dislocation.[23] Traumatic extubation with a partially inflated cuff may also lead to posterolateral arytenoid displacement.[24][25]
Subluxation results in hypomobility of the true vocal cords and incomplete closure of the glottis, mimicking vocal cord paralysis. Left-sided displacements/dislocations occur more often because most anesthesiologists insert the endotracheal tube from the right side of the mouth and oropharynx, placing undue force on the left arytenoid by the convex curvature of the endotracheal tube. After the lesion occurs, hemarthrosis with subsequent fibrosis and paresis of the recurrent laryngeal nerve may occur.[26]
History and Physical
Patients typically present with hoarseness, difficulty swallowing, and pain in the anterior region of the neck after a recent traumatic tracheal intubation or upper airway instrumentation. There are reports of rare instances of severe cough, external blunt trauma, or spontaneous events that lead to this presentation. The development of respiratory problems, dyspnea, and pseudo asthma are also possible.[8][11][27]
The clinician must first rule out life-threatening conditions such as stridor, dyspnea, and internal and external hematomas of the neck. The physical examination must include flexible fiber-optic laryngoscopy and videostroboscopy to allow direct and dynamic evaluation of the laryngeal structures.[17]
Evaluation
There is no gold standard for diagnosis. All patients who develop hoarseness after extubation must be evaluated with a flexible fiberoptic laryngeal examination, videostroboscopy, and computed tomography, focusing on the position and mobility of the vocal fold and arytenoid cartilage as well as traumatic injury to the larynx.
Flexible fiberoptic laryngoscopy can reveal the arytenoid displacement or dislocation with or without glottic edema. Videostroboscopy allows better visualization of any discrepancy in the lengths of the vocal cord and height of the vocal processes during phonation. It helps to differentiate cricoarytenoid subluxation from vocal cord palsy.[17][28]
Computed tomography with thin-section and multiplanar reformation will reveal disparities in the height of the vocal cords, a unique finding for arytenoid dislocation. Still, its value is limited in young patients, as the cartilage may not yet be ossified.[29][30][31]
Laryngeal electromyography may help distinguish between cricoarytenoid joint subluxation and vocal palsy. A dislocated arytenoid cartilage would most probably show normal EMG patterns, while in the case of recurrent laryngeal nerve palsy, the EMG pattern will be abnormal. However, both dislocation/subluxation and hematoma can occur with recurrent laryngeal nerve paresis and can lead to misdiagnosis.
The most accurate diagnosis seems to be obtained by the combination of history and physical, flexible fiberoptic laryngoscopy, laryngeal CT, and electromyography.[32][28][33]
Treatment / Management
The most common treatment is direct laryngoscopy with closed arytenoid reduction. The arytenoid cartilage should be repositioned on top of the cricoid while ensuring that the vocal process is placed as symmetrically as possible to the contralateral vocal process. The scheduling of this procedure must take place as soon as the diagnosis is made to improve the outcome.[34][35] This process can be performed under sedation while assessing phonation in real-time. Immediate improvement of symptoms confirms the diagnosis. Concomitant nerve injury is usually associated with delayed or no improvement. (B2)
With a delayed diagnosis, fibrosis and scarring may develop, making treatment more challenging. Open procedures such as thyroplasty and arytenoidopexy are options in selected cases.[36] [37][38] Botulinum toxin and voice therapy are important adjuvants in the treatment of arytenoid subluxation.[39] For patients with surgical contraindications, an alternative is vocal cord augmentation procedures such as injection laryngoplasty with temporary injectable materials such as absorbable gelatin powder or long-lasting and permanent agents such as polytetrafluoroethylene past and voice therapy. Vocal cord augmentation procedures allow for better phonation and alleviate the risk of aspiration.[40][41][42] (B2)
Conservative management with voice therapy, which entails voice exercises, relaxation techniques of the larynx and voice compensation mechanisms have also shown good results.[23](B3)
Differential Diagnosis
The most important differential diagnosis is vocal cord paralysis due to recurrent laryngeal nerve paralysis. Laryngeal electromyography is an important diagnostic test to differentiate between arytenoid subluxation and recurrent laryngeal nerve paralysis. Further, it may offer some prognostic information regarding potential vocal fold paralysis recovery.[33][43]
It may have some limitations since a transient paresis may be present with both a subluxation or a hematoma.
Prognosis
In about 19% of patients, spontaneous reduction and resolution occur without treatment.[44] Early treatment is associated with better outcomes, with almost all patients regaining normal voice and vocal fold mobility immediately after closed reduction.[45][35] Adequate voice recovery can be obtained even with late intervention. Patients with delayed or no improvement often have associated nerve injury, and in some instances, may recover with time. If not promptly reduced, an arytenoid joint can become fibrosed and fixed in an unfavorable position.
Complications
Patients can develop cricoarytenoid ankylosis and scarring with persistent hoarseness, dysphagia, and even respiratory complications if the condition persists.
Postoperative and Rehabilitation Care
Postoperatively voice therapy is a possible adjunct, or it can serve as a valid and effective intervention in patients who prefer conservative therapy.
Consultations
An otolaryngologist should be alerted immediately if an arytenoid subluxation is suspected. A screening flexible laryngeal endoscopy with stroboscopy (specialized viewing of vocal cord vibration) should be done to confirm the diagnosis to prevent treatment delays.
Deterrence and Patient Education
All patients undergoing endotracheal intubation must be made aware of possible complications of the procedure and must be advised to seek medical attention if acute, persistent hoarseness or dysphagia develop.
Pearls and Other Issues
The inclusion of arytenoid subluxation/dislocation must be a consideration in the differential diagnosis of prolonged postoperative hoarseness after endotracheal intubation. Although rare, it is a complication that can cause significant distress to patients. It has an excellent prognosis if diagnosed and treated promptly.
Gentle instrumentation of the airway and completely deflating the endotracheal tube cuff before extubation may prevent this injury. The use of a stylet appears to protect against arytenoid dislocation.
Enhancing Healthcare Team Outcomes
Arytenoid dislocation is not an uncommon complication of orotracheal intubation, and when the diagnosed is missed or delayed, it carries high morbidity. Thus, an interprofessional team should participate in diagnosis and management.
The anesthesiologist and anesthesia nurse have to communicate with an otolaryngologist if they believe the patient has suffered arytenoid dislocation during intubation. Clinicians (MDs, DOs, NPs, PAs) need to all consider this in their differential in intubated patients, as well as those who present with sudden unexplained hoarseness, dysphagia, and anterior neck pain. In the event of confirmed arytenoid dislocation, the entire team (clinicians, nursing, and afterward, voice therapists) need to communicate both during and following the corrective procedures.
It is crucial during the transfer of care for anesthesiologists to communicate any difficulties encountered during intubation with an emphasis on direct trauma during laryngoscopy. The diagnosis is not straightforward and may require several imaging studies. Acute dislocations are reducible during surgery, but chronic cases may require botulinum toxin and gel foam injection. A speech therapist must be involved in the care as the outcomes appear to be much better when combining the above treatments with voice therapy. Perianesthesia and critical care nurses can monitor post-procedure, and report to the clinician or even the voice therapist any findings of note.
The entire interprofessional team, including the clinicians, nursing, and therapists need to work collaboratively to manage the case through to a successful outcome. [Level V]
Outcomes
Early treatment is associated with better outcomes, with almost all patients regaining normal voice and vocal fold mobility immediately after closed reduction.[45][35] Adequate voice recovery can be obtained even with late intervention. Patients with delayed or no improvement often have associated nerve injury, and in some instances, may recover with time. If not promptly reduced, an arytenoid joint can become fibrosed and fixed in an unfavorable position.
Media
(Click Image to Enlarge)
References
Friedlander E, Pascual PM, Da Costa Belisario J, Serafini DP. Subluxation of the Cricoarytenoid Joint After External Laryngeal Trauma: A Rare Case and Review of the Literature. Indian journal of otolaryngology and head and neck surgery : official publication of the Association of Otolaryngologists of India. 2017 Mar:69(1):130-132. doi: 10.1007/s12070-016-1028-7. Epub 2016 Oct 18 [PubMed PMID: 28239594]
Level 3 (low-level) evidenceOppenheimer AG, Gulati V, Kirsch J, Alemar GO. Case 223: Arytenoid Dislocation. Radiology. 2015 Nov:277(2):607-11. doi: 10.1148/radiol.2015140145. Epub [PubMed PMID: 26492026]
Level 3 (low-level) evidenceTolley NS, Cheesman TD, Morgan D, Brookes GB. Dislocated arytenoid: an intubation-induced injury. Annals of the Royal College of Surgeons of England. 1990 Nov:72(6):353-6 [PubMed PMID: 2241051]
Level 3 (low-level) evidenceRubin AD, Hawkshaw MJ, Moyer CA, Dean CM, Sataloff RT. Arytenoid cartilage dislocation: a 20-year experience. Journal of voice : official journal of the Voice Foundation. 2005 Dec:19(4):687-701 [PubMed PMID: 16301111]
Andaloro C, Sharma P, La Mantia I. Anatomy, Head and Neck: Larynx Arytenoid Cartilage. StatPearls. 2023 Jan:(): [PubMed PMID: 30020624]
Allen E, Minutello K, Murcek BW. Anatomy, Head and Neck, Larynx Recurrent Laryngeal Nerve. StatPearls. 2023 Jan:(): [PubMed PMID: 29261997]
Wu L, Shen L, Zhang Y, Zhang X, Huang Y. Association between the use of a stylet in endotracheal intubation and postoperative arytenoid dislocation: a case-control study. BMC anesthesiology. 2018 May 31:18(1):59. doi: 10.1186/s12871-018-0521-9. Epub 2018 May 31 [PubMed PMID: 29855263]
Level 2 (mid-level) evidenceLee DH, Yoon TM, Lee JK, Lim SC. Clinical Characteristics of Arytenoid Dislocation After Endotracheal Intubation. The Journal of craniofacial surgery. 2015 Jun:26(4):1358-60. doi: 10.1097/SCS.0000000000001749. Epub [PubMed PMID: 26080195]
Debo RF, Colonna D, Dewerd G, Gonzalez C. Cricoarytenoid subluxation: complication of blind intubation with a lighted stylet. Ear, nose, & throat journal. 1989 Jul:68(7):517-20 [PubMed PMID: 2791919]
Level 3 (low-level) evidenceMikuni I, Suzuki A, Takahata O, Fujita S, Otomo S, Iwasaki H. Arytenoid cartilage dislocation caused by a double-lumen endobronchial tube. British journal of anaesthesia. 2006 Jan:96(1):136-8 [PubMed PMID: 16311281]
Level 3 (low-level) evidenceCho R, Zamora F, Dincer HE. Anteromedial Arytenoid Subluxation Due to Severe Cough. Journal of bronchology & interventional pulmonology. 2018 Jan:25(1):57-59. doi: 10.1097/LBR.0000000000000403. Epub [PubMed PMID: 28926355]
Unusual cause of hoarseness: Arytenoid cartilage dislocation without a traumatic event., Okazaki Y,Ichiba T,Higashi Y,, The American journal of emergency medicine, 2018 Jan [PubMed PMID: 29066184]
Nerurkar N, Chhapola S. Arytenoid subluxation after a bout of coughing: a rare case. American journal of otolaryngology. 2012 Mar-Apr:33(2):275-8. doi: 10.1016/j.amjoto.2011.07.001. Epub 2011 Aug 15 [PubMed PMID: 21840624]
Level 3 (low-level) evidenceRieger A, Hass I, Gross M, Gramm HJ, Eyrich K. [Intubation trauma of the larynx--a literature review with special reference to arytenoid cartilage dislocation]. Anasthesiologie, Intensivmedizin, Notfallmedizin, Schmerztherapie : AINS. 1996 Jun:31(5):281-7 [PubMed PMID: 8767240]
Lou Z, Yu X, Li Y, Duan H, Zhang P, Lin Z. BMI May Be the Risk Factor for Arytenoid Dislocation Caused by Endotracheal Intubation: A Retrospective Case-Control Study. Journal of voice : official journal of the Voice Foundation. 2018 Mar:32(2):221-225. doi: 10.1016/j.jvoice.2017.05.010. Epub 2017 Jun 7 [PubMed PMID: 28601417]
Level 2 (mid-level) evidenceTsuru S, Wakimoto M, Iritakenishi T, Ogawa M, Hayashi Y. Cardiovascular operation: A significant risk factor of arytenoid cartilage dislocation/subluxation after anesthesia. Annals of cardiac anaesthesia. 2017 Jul-Sep:20(3):309-312. doi: 10.4103/aca.ACA_71_17. Epub [PubMed PMID: 28701595]
Norris BK, Schweinfurth JM. Arytenoid dislocation: An analysis of the contemporary literature. The Laryngoscope. 2011 Jan:121(1):142-6. doi: 10.1002/lary.21276. Epub [PubMed PMID: 21181984]
Kambic V, Radsel Z. Intubation lesions of the larynx. British journal of anaesthesia. 1978 Jun:50(6):587-90 [PubMed PMID: 666934]
Rudert H. [Uncommon injuries of the larynx following intubation. Recurrent paralysis, torsion and luxation of the cricoarytenoid joints]. HNO. 1984 Sep:32(9):393-8 [PubMed PMID: 6501014]
Roberts D, McQuinn T, Beckerman RC. Neonatal arytenoid dislocation. Pediatrics. 1988 Apr:81(4):580-2 [PubMed PMID: 3353193]
Level 3 (low-level) evidenceMallon AS, Portnoy JE, Landrum T, Sataloff RT. Pediatric arytenoid dislocation: diagnosis and treatment. Journal of voice : official journal of the Voice Foundation. 2014 Jan:28(1):115-22. doi: 10.1016/j.jvoice.2013.08.016. Epub 2013 Oct 8 [PubMed PMID: 24119642]
Level 2 (mid-level) evidenceChen X, Wang Z, Xia Z. [Cause and treatment analysis of arytenoid dislocation caused by endotracheal intubation after general anesthesia of children]. Lin chuang er bi yan hou tou jing wai ke za zhi = Journal of clinical otorhinolaryngology, head, and neck surgery. 2014 Nov:28(21):1701-2 [PubMed PMID: 25735107]
Tan V, Seevanayagam S. Arytenoid subluxation after a difficult intubation treated successfully with voice therapy. Anaesthesia and intensive care. 2009 Sep:37(5):843-6 [PubMed PMID: 19775054]
Level 3 (low-level) evidenceTalmi YP, Wolf M, Bar-Ziv J, Nusem-Horowitz S, Kronenberg J. Postintubation arytenoid subluxation. The Annals of otology, rhinology, and laryngology. 1996 May:105(5):384-90 [PubMed PMID: 8651633]
Level 3 (low-level) evidenceHabe K,Kawasaki T,Horishita T,Sata T, [Airway problem during the operation with beach-chair position: a case of arytenoid dislocation and the relationship between intra-cuff pressure of endotrachial tube and the neck position]. Masui. The Japanese journal of anesthesiology. 2011 Jun [PubMed PMID: 21710762]
Level 3 (low-level) evidenceIchikawa J, Kodaka M, Nishiyama K, Kawamata M, Komori M, Ozaki M. [Prolonged hoarseness and arytenoid dislocation after endotracheal intubation]. Masui. The Japanese journal of anesthesiology. 2010 Dec:59(12):1490-3 [PubMed PMID: 21229688]
Level 3 (low-level) evidenceDíaz-Tantaleán JA, Velasco M, Muñoz X. Cricoarytenoid subluxation: another cause of pseudoasthma. Chest. 2014 Nov:146(5):e182-e183. doi: 10.1378/chest.14-1603. Epub [PubMed PMID: 25367498]
Level 3 (low-level) evidenceZhuang P, Nemcek S, Surender K, Hoffman MR, Zhang F, Chapin WJ, Jiang JJ. Differentiating arytenoid dislocation and recurrent laryngeal nerve paralysis by arytenoid movement in laryngoscopic video. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2013 Sep:149(3):451-6. doi: 10.1177/0194599813491222. Epub 2013 May 29 [PubMed PMID: 23719396]
Level 2 (mid-level) evidenceKösling S,Heider C,Heider C,Bartel-Friedrich S, [CT findings in isolated laryngeal trauma]. Laryngo- rhino- otologie. 2005 Aug [PubMed PMID: 16080060]
Level 2 (mid-level) evidenceWang Z, Xia L, Wang C. [Utility of spiral computed tomography in the study of dislocation of cricoarytenoid joint]. Zhonghua er bi yan hou ke za zhi. 2002 Jun:37(3):223-5 [PubMed PMID: 12772329]
Alexander AE Jr, Lyons GD, Fazekas-May MA, Rigby PL, Nuss DW, David L, Williams K. Utility of helical computed tomography in the study of arytenoid dislocation and arytenoid subluxation. The Annals of otology, rhinology, and laryngology. 1997 Dec:106(12):1020-3 [PubMed PMID: 9415597]
Schroeder U, Motzko M, Wittekindt C, Eckel HE. Hoarseness after laryngeal blunt trauma: a differential diagnosis between an injury to the external branch of the superior laryngeal nerve and an arytenoid subluxation. A case report and literature review. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 2003 Jul:260(6):304-7 [PubMed PMID: 12883952]
Level 3 (low-level) evidenceClose LG, Merkel M, Watson B, Schaefer SD. Cricoarytenoid subluxation, computed tomography, and electromyography findings. Head & neck surgery. 1987 Jul-Aug:9(6):341-8 [PubMed PMID: 3623957]
Level 3 (low-level) evidenceCao L, Wu X, Mao W, Hayes C, Wei C. Closed reduction for arytenoid dislocation under local anesthesia. Acta oto-laryngologica. 2016 Aug:136(8):812-8. doi: 10.3109/00016489.2016.1157267. Epub 2016 Mar 22 [PubMed PMID: 27002978]
Lee SW, Park KN, Welham NV. Clinical features and surgical outcomes following closed reduction of arytenoid dislocation. JAMA otolaryngology-- head & neck surgery. 2014 Nov:140(11):1045-50. doi: 10.1001/jamaoto.2014.2060. Epub [PubMed PMID: 25257336]
Level 2 (mid-level) evidenceRyu IS, Nam SY, Han MW, Choi SH, Kim SY, Roh JL. Long-term voice outcomes after thyroplasty for unilateral vocal fold paralysis. Archives of otolaryngology--head & neck surgery. 2012 Apr:138(4):347-51. doi: 10.1001/archoto.2012.42. Epub 2012 Mar 19 [PubMed PMID: 22431862]
Level 2 (mid-level) evidenceCura O, Uluoz U, Kirazli T, Karci B. [Arytenoidopexy in bilateral abductor paralysis of the glottis]. Revue de laryngologie - otologie - rhinologie. 1991:112(1):59-62 [PubMed PMID: 2052789]
Zimmermann TM, Orbelo DM, Pittelko RL, Youssef SJ, Lohse CM, Ekbom DC. Voice outcomes following medialization laryngoplasty with and without arytenoid adduction. The Laryngoscope. 2019 Aug:129(8):1876-1881. doi: 10.1002/lary.27684. Epub 2018 Dec 24 [PubMed PMID: 30582612]
Rontal E, Rontal M. Botulinum toxin as an adjunct for the treatment of acute anteromedial arytenoid dislocation. The Laryngoscope. 1999 Jan:109(1):164-6 [PubMed PMID: 9917060]
Tigges M, Hess M. [Glottis injection to improve voice function : Review of more than 500 operations]. HNO. 2015 Jul:63(7):489-96. doi: 10.1007/s00106-015-0029-2. Epub [PubMed PMID: 26104911]
Mallur PS, Rosen CA. Vocal fold injection: review of indications, techniques, and materials for augmentation. Clinical and experimental otorhinolaryngology. 2010 Dec:3(4):177-82. doi: 10.3342/ceo.2010.3.4.177. Epub 2010 Dec 22 [PubMed PMID: 21217957]
Sulica L, Rosen CA, Postma GN, Simpson B, Amin M, Courey M, Merati A. Current practice in injection augmentation of the vocal folds: indications, treatment principles, techniques, and complications. The Laryngoscope. 2010 Feb:120(2):319-25. doi: 10.1002/lary.20737. Epub [PubMed PMID: 19998419]
Reiter R, Hoffmann TK, Rotter N, Pickhard A, Scheithauer MO, Brosch S. [Etiology, diagnosis, differential diagnosis and therapy of vocal fold paralysis]. Laryngo- rhino- otologie. 2014 Mar:93(3):161-73. doi: 10.1055/s-0033-1355373. Epub 2013 Oct 17 [PubMed PMID: 24135826]
Kato T, Wada K, Morioka N, Onuki E, Ozaki M, Ishida T. [Arytenoid cartilage dislocation caused by endotracheal intubation which resolved spontaneously]. Masui. The Japanese journal of anesthesiology. 2010 Jun:59(6):724-6 [PubMed PMID: 20560374]
Level 3 (low-level) evidenceAbe K, Nishino H, Makino N, Ishikawa K, Ishikawa K, Imai K, Ichimura K. [Fiberscopic reduction under local anesthesia for anterior arytenoid cartilage dislocation]. Nihon Jibiinkoka Gakkai kaiho. 2007 Jan:110(1):13-9 [PubMed PMID: 17302296]