Introduction
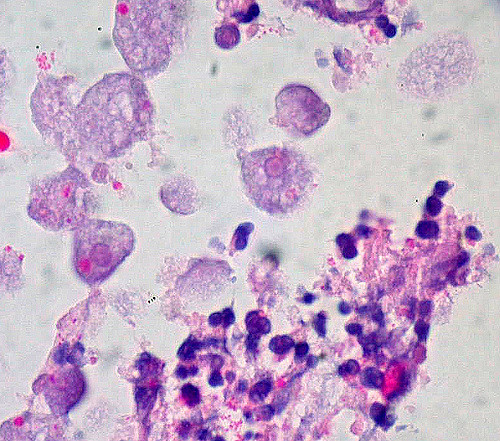
Amebic colitis results from an invasive infection of the colonic mucosa by Entamoeba histolytica (E histolytica).[1] Losch first reported disease due to E histolytica in 1875; he found amoebas in colonic ulcers at autopsy and showed that the disease could be experimentally induced in vivo by rectal inoculation with human feces (see Image. Amebic Colitis). Other scientists have shown that amoeba is the cause of the disease. E histolytica has a worldwide distribution but is uncommon in the United States. However, it occurs with increased frequencies in patients with AIDS and men who engage in sex with other men. Symptoms vary widely and include the following:
- Dysentery with diarrhea and rectal bleeding mimicking irritable bowel disease (IBD)
- Liver abscesses
- Colonic granulomatous masses that can mimic carcinoma
- Complications include colonic perforation and fistulas or liver abscesses [2]
E histolytica can spread by the ingestion of the amoeba cyst. The infective cysts can occur in contaminated food and water. Transmission by fecal-oral self-inoculation can also happen in oral-anal sexual contact.[3]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
E histolytica, the protozoan parasite causing amebiasis, colonizes the intestinal tract in 90% of susceptible individuals and presents asymptomatically. In 10%, the parasite overcomes the mucosal barrier of the colon and invades the lamina propria[4]. Untreated invasive amebiasis can lead to severe colitis and fulminant infection, which is associated with high mortality.[5] The host acquires parasite cysts through ingesting contaminated food or water, mostly in areas or countries with poor sanitation.[6]
Epidemiology
E histolytica affects approximately 10% of the global population, with over 100,000 deaths per year from amebic dysentery and liver abscesses.[5] It is most prevalent in developing countries but is known to occur in Western countries, especially among recent immigrants, travelers returning from endemic areas, men who have sex with men, and immunocompromised individuals. Entamoeba histolytica parasite cysts' infection occurs through food or water intake and is contaminated by human feces due to poor environmental sanitation or personal hygiene.[7]
Pathophysiology
The gastric acid and the mucus barrier of the intestine serve as a protective mechanism that prevents the E histolytica cysts from coming in contact with the intestinal epithelium. Encystation occurs in the terminal ileum or colon, which results in the trophozoites getting released into the lumen of the gut. Some individuals develop invasive amebic infection among those exposed, which is thought to be due to the interplay between the host's defensive factors and the virulence factor of the parasite. The 3 major virulence factors known to influence pathogenicity are:
- N-acetylgalactosamine-inhibitable lectin: Responsible for binding colonic mucin and host cell adhesion.
- Amebapore: A small peptide that facilitates the killing of host cells.
- Cystine proteases: Enzymes that facilitate the lysis of the host extracellular matrix.
As the pathology progresses, the colonic mucosa becomes diffusely inflamed and edematous, with associated necrosis and sometimes intestinal wall perforation.[8]
Histopathology
The classic endoscopic appearance is that of discrete areas of ulceration covered by exudate, with normal intervening mucosa; however, many cases depart from this description. Amebiasis may involve any part of the bowel but has a predilection for the cecum and ascending colon. The entire large bowel is involved in some cases, and there may even be an extension into the terminal ileum.[9] Perforation occurs in 5% to 10% of the cases. The microscopic appearance of a rectal biopsy is rather nonspecific. However, the relative paucity of inflammatory cells beneath the ulcer and the flask shape of the ulcer itself should alert the pathologist to consider this diagnosis. Confirmation rests on identifying trophozoites of E histolytica, which is visible in hematoxylin and eosin (H&E) slides.
Typically, the parasites measure 6 to 40 nm, are round or ovoid, and may demonstrate a surrounding halo; they contain an abundant and vacuolated cytoplasm with small nuclei and a prominent nuclear membrane. The organism's cytoplasm appears clean and free of ingested bacteria and vacuoles in a trichrome stain. Finely granular nuclear chromatin, demonstrating even distribution on the nuclear membrane, and the small central karyosome, stain a dark purple-red. Ingested RBCs are diagnostic for E histolytica trophozoites but usually are not present. The organisms are also detectable with periodic acid–Schiff (PAS) and immunoperoxidase stains.[10]
Toxicokinetics
E histolytica is cytotoxic to some cell types, including neutrophils, T lymphocytes, and macrophages. The organism adheres to the intestinal mucosa, invades and disrupts the mucosal barrier, produces contact-dependent killing, and stimulates apoptosis of the intestinal cells. The organism lyses and phagocytizes the cell. Cysteine proteases that destroy collagen and fibronectin mediate the invasion of the deeper layers of the intestinal wall. The host secretes proinflammatory cytokines, leading to an acute inflammatory response and migration of neutrophils and macrophages into the tissue. The organism can also secrete chemoattractants for neutrophils. It kills these cells by contact-dependent lysis, and the subsequent release of lysozymes, superoxides, and collagenases from the neutrophil granules produces additional damage to the intestinal mucosa.[6][11]
History and Physical
Almost 90% of infections are asymptomatic. Individuals who are colonized but remain asymptomatic raise a significant risk to others because they are cyst passers and, therefore, infective. Symptomatic clinical infection may appear as an acute infection in the colon called amebic colitis. Amebic colitis typically presents with symptoms of diarrhea with blood in the stools, although the symptoms can be nonspecific. Amebic colitis has a more gradual onset than bacterial colitis. Amebic colitis can closely simulate ulcerative colitis or Crohn disease on clinical grounds.[12]
The patient may have localized or diffused tenderness upon palpation during physical examination. Rarely, a palpable mass may be present. If undiagnosed and untreated, a patient may present with a toxic megacolon, which presents as an acute dilatation of the colon. This complication carries a high mortality due to associated necrosis and perforation. Fewer than 1% of patients with amebic colitis have associated extraintestinal infection, the commonest being a liver abscess. Patients with liver abscesses may have symptoms such as fever, chills, and pain in the upper right quadrant or can be asymptomatic. Weight loss, increased white blood cell counts, or elevated liver enzyme levels may occur. Jaundice is usually absent.[13] Lung abscesses may develop due to penetration of the diaphragm by amebae from hepatic abscesses or hematogenous spread. Invasion of the lung can cause symptoms such as chest pain, dyspnea, and a productive cough.[14]
Evaluation
The gold standard for diagnosing amebic colitis is the detection of trophozoites of E. histolytica with ulcers in the microscopic examination of colonoscopic biopsies or, more infrequently, in fresh stool examination. Patients with diarrhea are most likely to have trophozoites in the stool, which may be visible in direct wet mounts or trichrome-stained smears. Classically, the cecum and ascending colon are affected, and multiple punctate ulcers are observed with intervening normal tissue. The ulcers on histological examination typically appear as flask-shaped. In severe cases of amebic colitis, the ulcers may coalesce to look similar to ulcerative colitis.[7]
Amebic liver abscesses often are detected by ultrasonographic or radiographic tests.[15] Subsequent aspiration of the abscess may reveal motile trophozoites and necrotic material composed of lysed cells. Serologic methods of detecting antibodies to E. histolytica are available; the results are positive in more than 90% of patients with the extraintestinal disease. These antibody levels rise after tissue invasion but are not protective. However, antibody tests are not particularly useful in distinguishing between past and current infections because antibodies can persist for years after an infection has resolved. Also, these tests provide limited information on patients from endemic areas. Tests that detect E histolytica antigen in stool provide evidence of current infection. Point-of-care testing using immunochromatographic techniques is being developed to assist with the rapid diagnosis of E histolytica infection.[16] Some are designed to detect the antigen in the stool, and others to detect antibodies in the serum. One disadvantage of these tests is that fresh, unpreserved stool is necessary for testing.
Treatment / Management
Amebic colitis requires treatment with combination therapy, and treatment options include luminal agents combined with tissue amebicides. The luminal amebicides include iodoquinol, diloxanide furoate, and paromomycin. The tissue amebicides include nitroimidazole (metronidazole), nitazoxanide, erythromycin, and chloroquine. Surgery is required when there is an associated liver abscess that needs drainage, or the patient presents as an emergency with a toxic megacolon with impending or free perforation.[17]
Differential Diagnosis
Differential diagnoses include appendicitis, IBD, pseudomembranous colitis, and tuberculosis. Rarely, E histolytica can affect the appendix, representing an extension of an infection of the right colon. Typical IBD does not show fibrinous materials containing organisms. Ulcerative colitis characteristically shows more diffuse colonic involvement with mucosal distortion and lamina propria basal plasma cell infiltration. Crohn's disease may show patchy mucosal ulceration but is distinguishable by fissure-like ulcers rather than flask-shaped ulceration; ulcers from Crohn's disease are mostly horizontal, whereas the amebic ulcers grow perpendicular to the long axis of the bowel.[18][19] In colon tuberculosis, grossly, ulceration with diffuse fibrosis extends through the wall, causing stenosis and obstruction. Coexistent tuberculous peritonitis presents in rare cases. Microscopically, typical granulomas are usually present.[20]
Treatment Planning
Invasive colitis is treated with metronidazole (or alternative medications including tinidazole and nitazoxanide), followed by a luminal agent (such as paromomycin or diiodohydroxyquin) to kill intraluminal cysts. A 10-day course of metronidazole eliminates the intraluminal infection in most cases, but a second agent is still required. The recommended regimen of metronidazole for amebic colitis treatment is 500 to 750 mg 3 times per day in adults and 30 to 50 mg/kg per day for 5 to 10 days in children. The alternative regimen could be 2 g oral tinidazole, a single dose daily in adults for 3 days, and 50 mg/kg per day oral in a single dose in children for 3 days.[21]
With metronidazole alone, the parasites may persist in the intestine in as many as 40% to 60% of patients.[9] Thus, the recommendation is that patients with invasive amebiasis should receive a luminal agent as the second line to eliminate surviving cysts in the bowel lumen. Luminal medications include paromomycin, diiodohydroxyquin, and diloxanide. Current guidelines recommend either iodoquinol 650 mg orally 3 times a day in adults for 20 days, and 30 to 40 mg/kg per day PO in 3 doses in children for 20 days, or paromomycin 25 to 35 mg/kg per day by mouth in 3 doses for 7 days in all ages.[22]
Toxicity and Adverse Effect Management
Broad-spectrum antibacterial therapy is necessary in patients who have known or suspected peritonitis. Surgical intervention is required in the setting of significant bowel perforation or abscesses that fail to respond to antibiotic therapy. Toxic megacolon often requires colectomy.
Prognosis
Drug treatment cures amebiasis in a few weeks. Intestinal amebiasis can be fatal in developing countries among children, especially those younger than 5 of age. Worldwide, amebiasis is the third most common cause of death due to parasitic infection after malaria and schistosomiasis, with at least 5 deaths per year in the United States.[23]
Complications
Complications of amebic colitis include fulminant or necrotizing colitis, toxic megacolon, bowel perforation, peritonitis, hemorrhage, stricture formation, or obstruction.[24] Fulminant colitis occurs in 0.5% of cases, and patients present with copious dysentery, fever, leukocytosis, and vague abdominal pain; the bowel mucosa may undergo necrosis, leading to transmural perforation and subsequent peritonitis. Treatment with nitroimidazole and early surgical management is required; in the cases of intestinal perforation, broad-spectrum antibiotics are the therapy of choice. Toxic megacolon, seen in approximately 0.5% of cases and associated with high mortality, usually requires surgical intervention. It appears as total or segmental non-obstructive colonic dilatation plus systemic toxicity. The amebic liver abscess has been reported to vary between 3% and 9 % of amebiasis cases.[25] Pleuropulmonary amebiasis can also occur, which is the second most frequent extra-intestinal manifestation of amebiasis after amebic liver abscess.
Deterrence and Patient Education
For travelers to endemic areas, preventing amebic infection involves avoiding untreated water and uncooked food, such as fruit and vegetables, that may have been washed in local water. Amebic cysts are resistant to chlorine at the levels used in water supplies, but disinfection with iodine may be effective.[26] Treatment for amebiasis should include informing patients of the medications' side effects and the need to adhere to the follow-up course of a luminal agent to eliminate the protozoa colonization and the symptoms and signs of its complications.
Pearls and Other Issues
All E. histolytica infections, even asymptomatic, should receive treatment, given the high risk of leading to invasive infection and the risk of passing the infection to the other household members.
Enhancing Healthcare Team Outcomes
It is crucial to understand amebiasis pathogenesis to have enhanced treatment and prevention. The clinical team, including nurses and pharmacists, should educate the patients on the significance of handwashing and hand hygiene after defecation and before feeding. Explanations to travelers about the risks of eating raw vegetables and fruits and drinking contaminated water are recommended. Clinicians, including doctors, nurse practitioners, and physician assistants, should be aware of how to treat asymptomatic carriers to minimize the spread of infection and diminish the risk of developing invasive disease. The pharmacist should evaluate the medication choice, check for drug-drug interactions, and ensure patient compliance. The clinical team and nursing staff should work together to ensure that patients are well-educated regarding the risks of the disease and prevention techniques.
In summary, amebic colitis requires an interprofessional team approach, including physicians, infectious disease specialists, specialty-trained infection control and gastrointestinal nurses, and pharmacists, collaborating across disciplines to achieve optimal patient results.
With drug treatment, a cure is possible in most patients. However, without drug therapy, failure to thrive and even death are common. The recovery with drug treatment may take a few weeks or months.
Media
(Click Image to Enlarge)
References
Espinosa-Cantellano M, Martínez-Palomo A. Pathogenesis of intestinal amebiasis: from molecules to disease. Clinical microbiology reviews. 2000 Apr:13(2):318-31 [PubMed PMID: 10756002]
Level 3 (low-level) evidenceCooper CJ, Fleming R, Boman DA, Zuckerman MJ. Varied Clinical Manifestations of Amebic Colitis. Southern medical journal. 2015 Nov:108(11):676-81. doi: 10.14423/SMJ.0000000000000370. Epub [PubMed PMID: 26539949]
Roure S, Valerio L, Soldevila L, Salvador F, Fernández-Rivas G, Sulleiro E, Mañosa M, Sopena N, Mate JL, Clotet B. Approach to amoebic colitis: Epidemiological, clinical and diagnostic considerations in a non-endemic context (Barcelona, 2007-2017). PloS one. 2019:14(2):e0212791. doi: 10.1371/journal.pone.0212791. Epub 2019 Feb 21 [PubMed PMID: 30789955]
Level 2 (mid-level) evidenceBegum S, Quach J, Chadee K. Immune Evasion Mechanisms of Entamoeba histolytica: Progression to Disease. Frontiers in microbiology. 2015:6():1394. doi: 10.3389/fmicb.2015.01394. Epub 2015 Dec 15 [PubMed PMID: 26696997]
Stanley SL Jr. Amoebiasis. Lancet (London, England). 2003 Mar 22:361(9362):1025-34 [PubMed PMID: 12660071]
Level 3 (low-level) evidenceRalston KS, Petri WA Jr. Tissue destruction and invasion by Entamoeba histolytica. Trends in parasitology. 2011 Jun:27(6):254-63. doi: 10.1016/j.pt.2011.02.006. Epub 2011 Mar 26 [PubMed PMID: 21440507]
Domazetovska A, Lee R, Adhikari C, Watts M, Gilroy N, Stark D, Sivagnanam S. A 12-Year Retrospective Study of Invasive Amoebiasis in Western Sydney: Evidence of Local Acquisition. Tropical medicine and infectious disease. 2018 Jun 26:3(3):. doi: 10.3390/tropicalmed3030073. Epub 2018 Jun 26 [PubMed PMID: 30274469]
Level 2 (mid-level) evidenceMoonah SN, Jiang NM, Petri WA Jr. Host immune response to intestinal amebiasis. PLoS pathogens. 2013:9(8):e1003489. doi: 10.1371/journal.ppat.1003489. Epub 2013 Aug 22 [PubMed PMID: 23990778]
Level 3 (low-level) evidenceHaque R, Huston CD, Hughes M, Houpt E, Petri WA Jr. Amebiasis. The New England journal of medicine. 2003 Apr 17:348(16):1565-73 [PubMed PMID: 12700377]
Level 3 (low-level) evidenceKobayashi TK, Koretoh O, Kamachi M, Watanabe S, Ishigooka S, Matsushita I, Sawaragi I. Cytologic demonstration of Entamoeba histolytica using immunoperoxidase techniques. Report of two cases. Acta cytologica. 1985 May-Jun:29(3):414-8 [PubMed PMID: 2860765]
Level 3 (low-level) evidenceRavdin JI, Croft BY, Guerrant RL. Cytopathogenic mechanisms of Entamoeba histolytica. The Journal of experimental medicine. 1980 Aug 1:152(2):377-90 [PubMed PMID: 6249882]
Level 3 (low-level) evidencePittman FE, el-Hashimi WK, Pittman JC. Studies of human amebiasis. I. Clinical and laboratory findings in eight cases of acute amebic colitis. Gastroenterology. 1973 Oct:65(4):581-7 [PubMed PMID: 4355733]
Level 3 (low-level) evidencePérez-Tamayo R, Montfort I, García AO, Ramos E, Ostria CB. Pathogenesis of acute experimental liver amebiasis. Archives of medical research. 2006 Feb:37(2):203-9 [PubMed PMID: 16380320]
Level 3 (low-level) evidenceNasrullah A, Haq S, Ghazanfar H, Sheikh AB, Akhtar A, Zafar R, Nasir A, Shaukat F, Abbas AH. A Unique Case of Empyema Secondary to Amoebic Liver Abscess. Cureus. 2017 Jun 21:9(6):e1377. doi: 10.7759/cureus.1377. Epub 2017 Jun 21 [PubMed PMID: 28775917]
Level 3 (low-level) evidenceKoizumi K, Masuda S, Uojima H, Ichita C, Tokoro S, Sasaki A, Egashira H, Kimbara T, Kako M. Endoscopic ultrasound-guided drainage of an amoebic liver abscess extending into the hepatic subcapsular space. Clinical journal of gastroenterology. 2015 Aug:8(4):232-5. doi: 10.1007/s12328-015-0585-8. Epub 2015 Jul 24 [PubMed PMID: 26204883]
Tachibana H, Kakino A, Kazama M, Feng M, Asai S, Umezawa K, Nozaki T, Makiuchi T, Kamada T, Watanabe H, Horiki N, Cheng X, Masuda G. Development of a sensitive immunochromatographic kit using fluorescent silica nanoparticles for rapid serodiagnosis of amebiasis. Parasitology. 2018 Dec:145(14):1890-1895. doi: 10.1017/S0031182018000690. Epub 2018 May 9 [PubMed PMID: 29739480]
Jackson-Akers JY, Prakash V, Oliver TI. Amebic Liver Abscess. StatPearls. 2024 Jan:(): [PubMed PMID: 28613582]
Gajendran M, Loganathan P, Jimenez G, Catinella AP, Ng N, Umapathy C, Ziade N, Hashash JG. A comprehensive review and update on ulcerative colitis(). Disease-a-month : DM. 2019 Dec:65(12):100851. doi: 10.1016/j.disamonth.2019.02.004. Epub 2019 Mar 2 [PubMed PMID: 30837080]
Langner C, Aust D, Ensari A, Villanacci V, Becheanu G, Miehlke S, Geboes K, Münch A, Working Group of Digestive Diseases of the European Society of Pathology (ESP) and the European Microscopic Colitis Group (EMCG). Histology of microscopic colitis-review with a practical approach for pathologists. Histopathology. 2015 Apr:66(5):613-26. doi: 10.1111/his.12592. Epub 2015 Jan 12 [PubMed PMID: 25381724]
Rathi P, Gambhire P. Abdominal Tuberculosis. The Journal of the Association of Physicians of India. 2016 Feb:64(2):38-47 [PubMed PMID: 27730779]
Gonzales MLM, Dans LF, Sio-Aguilar J. Antiamoebic drugs for treating amoebic colitis. The Cochrane database of systematic reviews. 2019 Jan 9:1(1):CD006085. doi: 10.1002/14651858.CD006085.pub3. Epub 2019 Jan 9 [PubMed PMID: 30624763]
Level 1 (high-level) evidenceEscobedo AA, Almirall P, Alfonso M, Cimerman S, Rey S, Terry SL. Treatment of intestinal protozoan infections in children. Archives of disease in childhood. 2009 Jun:94(6):478-82. doi: 10.1136/adc.2008.151852. Epub 2009 Mar 26 [PubMed PMID: 19329448]
Level 3 (low-level) evidenceGunther J, Shafir S, Bristow B, Sorvillo F. Short report: Amebiasis-related mortality among United States residents, 1990-2007. The American journal of tropical medicine and hygiene. 2011 Dec:85(6):1038-40. doi: 10.4269/ajtmh.2011.11-0288. Epub [PubMed PMID: 22144440]
Fleming R, Cooper CJ, Ramirez-Vega R, Huerta-Alardin A, Boman D, Zuckerman MJ. Clinical manifestations and endoscopic findings of amebic colitis in a United States-Mexico border city: a case series. BMC research notes. 2015 Dec 14:8():781. doi: 10.1186/s13104-015-1787-3. Epub 2015 Dec 14 [PubMed PMID: 26666636]
Level 2 (mid-level) evidenceMisra SP, Misra V, Dwivedi M, Singh PA, Barthwal R. Factors influencing colonic involvement in patients with amebic liver abscess. Gastrointestinal endoscopy. 2004 Apr:59(4):512-6 [PubMed PMID: 15044887]
Lotter H, Tannich E. The current status of an amebiasis vaccine. Archives of medical research. 2006 Feb:37(2):292-6 [PubMed PMID: 16380335]