Introduction
Pediatric foot alignment deformities include a wide range of entities that can be simple or complex. The deformities can present at birth or later in life and, in some cases, are diagnosed in utero. The parents seek medical care for their children with these conditions. The most common deformities are clubfoot, planovalgus foot, cavovarus foot, congenital vertical talus, congenital oblique talus, metatarsus adductus, and skew foot deformity.[1][2][3]
Clubfoot: Clubfoot (talipes equinovarus) is a congenital idiopathic foot deformity. Clubfoot is one of the most common congenital foot deformities and can lead to severe disability if left untreated. The malformation consists of 4 components outlined with the mnemonic CAVE (Cavus, Adductus, Varus, Equinus). Clubfoot demonstrates excellent outcomes if treated early; the most commonly used management is the Ponseti method of serial casting.
Planovalgus: Pes planovalgus deformity (flatfoot deformity) is a relatively common orthopedic condition that usually presents in adolescence. This deformity is characterized by midfoot planus and hindfoot valgus deformity. The diagnosis is usually made clinically, although imaging can be pursued to exclude other coexisting conditions.
Cavovarus: Pes cavovarus is a common orthopedic condition affecting children and adults. Cavovarus and cavus deformity are usually used interchangeably as the cavus foot, most commonly, is presented with varus hindfoot deformity. This condition is generally associated with neurological disorders and can occur after trauma. On physical exam, midfoot cavus (ie, foot arch higher than normal) and hindfoot varus are described. Diagnosis is mainly clinical; treatment options range from foot orthotics to surgical intervention.
Congenital vertical talus: Congenital vertical talus (CVT) is a rare congenital condition characterized by rigid dorsal talonavicular dislocation. Chromosomal or neuromuscular abnormalities are usually the cause. Patients with CVT present with rigid flatfoot deformity. If not treated early, CVT may lead to significant disability.
Congenital oblique talus: Congenital oblique talus (COT) is an uncommon pediatric foot deformity and should be distinguished from congenital vertical talus, as they have the same clinical picture. COT may be considered a normal anatomic variant.
Metatarsus adductus: Metatarsus adductus (MA) is the most common congenital deformity of the foot in newborns and is present in 1 to 2 babies per 1000 births.[4] This deformity is isolated to the forefoot, with a medial deviation of the metatarsals at the Lisfranc joint. The exact etiology remains unknown; up to 90% of fully flexible metatarsus adductus cases resolve spontaneously by one year of age.[5][6]
Skew foot: Skewfoot is a rare pediatric foot deformity characterized by forefoot adduction, midfoot abduction, and hindfoot valgus deformity, forming a characteristic “z” appearance of the foot. The etiology varies; congenital and acquired have been identified. Treatment is usually surgical.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The etiology ranges and includes genetic and environmental factors.
Clubfoot: Although the etiology of the clubfoot is largely unknown, genetic and environmental factors have been involved. A positive family history is noted in 24.4% of newly diagnosed neonates.[7] Furthermore, few genes have been implicated in the cause of clubfoot. HOX gene, which plays a role in apoptosis and muscle contraction, and the PITX1-TBX4 pathway, critical for limb development, have been identified.[8][9][10]
Although in 80% of cases, clubfoot is an isolated deformity. Clubfoot can present as part of various genetic syndromes and medical conditions in 20% of cases. More specifically, clubfoot has been linked with arthrogryposis, myelodysplasia, amniotic band syndrome, myelomeningocele, trisomy 18, Larsen syndrome, Pierre-Robin syndrome, and prune belly syndrome.[11]
Environmental factors such as maternal smoking, maternal diabetes, and oligohydramnios have also been linked with clubfoot.[12][13] A recent systematic review and meta-analysis have reported that paternal smoking, maternal obesity, selective serotonin reuptake inhibitor (SSRI) exposure, and nulliparity have been linked to increased incidence of clubfoot.[14] Alcohol and solvent exposure have also been implicated in clubfoot.[15][16]
Planovalgus: Pes planovalgus can be congenital or acquired. Flexible flatfoot is common in childhood and can persist up to age 5.[17][18] Flexible flatfoot, due to ligamentous laxity, is corrected when children walk on their toes. Obesity may also play a role in flatfoot development.[19] Acquired flatfoot may occur after trauma or secondary to genetic syndromes, such as Down syndrome, Marfan, or Ehlers-Danlos syndromes.[20][21][22][23] This is mainly due to posterior tibialis dysfunction and laxity.[24][25]
Cavovarus: Pes cavovarus is usually associated with neurologic or traumatic conditions but can present as idiopathic; almost two-thirds of the cases are due to a neurologic condition. Other conditions present with cavovarus foot deformity are cerebral palsy, amniotic band syndrome, and Friedreich’s ataxia.[26][27][28] Charcot-Marie-Tooth should be considered the most common cause when patients present with bilateral deformity. In unilateral cases, conditions such as brain tumors or tethered spinal cord should be excluded.[26][29]
Congenital vertical talus: The exact etiology of CVT is unknown. However, over half of the cases are associated with chromosomal, musculoskeletal, or neurologic conditions. Commonly associated conditions are arthrogryposis, myelomeningocele, and cerebral palsy.[30][31][32] A positive family history may be present, and mutation in the HOXD10 gene, important for limb development, has also been reported.[33][34]
Congenital oblique talus: The etiology of COT is unknown; however, some cases are associated with neuromuscular conditions such as cerebral palsy or Down syndrome.[35]
Metatarsus adductus: The exact etiology of metatarsus adductus remains unknown.[4] However, 3 hypotheses have been described: (1) increased intrauterine pressure, supported by the high incidence of deformity in twins, (2) osseous abnormality, and (3) abnormal muscle attachments.[4][5][36] The last 2 have been debated in the literature as to if they are causative factors or simply an adaptation following the existent metatarsus adductus.[5]
Skew foot: Etiology can either be congenital or acquired, and occurrence after metatarsus adductus has been described. However, the exact etiology is unknown and can be attributed to muscle imbalances.[37][38][39][40] Napiontek et al proposed a classification of 4 types of the skew foot: (1) idiopathic congenital skew foot; (2) congenital skew foot associated with syndromes, such as osteogenesis imperfect; (3) skew foot secondary to neurological conditions, such as cerebral palsy or myelodysplasia; and (4) iatrogenic skew foot (after clubfoot or metatarsus adductus).[37][38][39][40][41]
Epidemiology
Epidemiology differs for each foot deformity.
Clubfoot: Clubfoot is the most commonly reported congenital defect of the limbs, with a reported incidence rate of approximately 1 case per 1000 live births.[16][42] However, the incidence is higher in certain populations such as Hawaiians and Maori.[43] Men are twice as likely to be affected.[7] Half of the cases occur bilaterally, while in unilateral cases, the right foot is the most commonly involved.[44]
Planovalgus: The epidemiology in children is unknown; in adults the incidence ranges from 13.6% to 37%.[45][46][47]
Cavovarus: The incidence of the deformity is largely unknown. Japas et al reported a 10% prevalence in the general population.[48] However, pes planovalgus is associated with neurologic conditions. Nagai et al reviewed cases of 148 children with bilateral cavovarus foot deformity and found that 78% were associated with Charcot-Marie-Tooth syndrome. The prevalence rose to 91% for those with a positive family history of Charcot-Marie-Tooth syndrome.[49] Another study reviewed 1047 diabetic cases and found a 25% prevalence of cavus foot deformities.[50]
Congenital vertical talus: CVT is rare, occurring in almost 1 in 10,000 live births. [51]
Congenital oblique talus: The epidemiology of COT is unknown.
Metatarsus adductus: 1 to 2 cases in 1,000 births. There is an increased rate in women, and bilateral involvement is present in about 50% of cases.[36]
Skew foot: The epidemiology is largely unknown. However, the prevalence is calculated at around 0.5% in the general pediatric population.[40]
Pathophysiology
The pathophysiology may include osseous or soft tissue imbalance.
Clubfoot: Multiple muscle contractures that work simultaneously contribute to the characteristic appearance of the clubfoot. This results in medial deviation of the forefoot and midfoot compared to the hindfoot. More specifically, the bony deformities consist mainly of medial deviation and rigid plantar flexion of the talus, which acts as a pivot point for the calcaneus (hindfoot) and the tarsal bones (midfoot).
The calcaneus is rotated medially around the talus (hindfoot varus), and the navicular and cuboid tarsal bones are also displaced medially, resulting in forefoot adduction. Overall, the bony deformities can be summarized by the CAVE mnemonic, which consists of the Cavus of the midfoot, Adductus of the forefoot, Varus, and Equinus of the hindfoot.[52][53][54][55]
Planovalgus: Ligamentous laxity or muscle imbalance is considered the cause of pes planovalgus deformity. The posterior tibialis tendon is important for maintaining the foot arch, and when it is weak, flatfoot will ensue. Pes planovalgus has also been associated with excessive tension in the soleus, triceps surae, and gastrocnemius muscles.[56][57]
Cavovarus: The deformity results from muscle imbalances; the stronger peroneus longus and posterior tibialis muscles overpull against the weaker anterior tibialis and peroneus brevis muscles, respectively, causing plantarflexion of the first ray of the foot with forefoot pronation and compensatory varus deformity of the hindfoot.[58][59][60]
Congenital vertical talus: The main characteristic is a vertically oriented plantarflexed talus in relation to the navicular bone and a resultant fixed talonavicular dislocation. The navicular bone deviates dorsolaterally. This leads to a hypoplastic navicular bone and abnormally shaped talus. The hindfoot resumes an equinus and valgus position, resulting from the Achilles tendon and subtalar capsule contracture, and may also lead to calcaneocuboid dislocation.[61][62][63]
Metatarsus adductus: Even though the exact etiology is unknown, the most accepted theory is increased intrauterine pressure, also known as the intrauterine packaging phenomenon.[36] With fetal development and growth, there is less room to accommodate the fetus, and compression of the forefoot as legs are crossed over the body contributes to the development of the metatarsus adductus.[5][36]
Skew foot: The etiology of the skew foot is unknown; however, muscle imbalances have been speculated to play a role. More specifically, a misplaced anterior tibialis tendon insertion in combination with Achilles tendon contracture could lead to skew foot deformity.[37][38][39][40][41]
History and Physical
History and physical examination are essential for the diagnosis. Antenatal, birth, and patient history, as well as family history, should be obtained. Few deformities are associated with neurological or genetic disorders, so a neurological exam or genetic testing may also be needed.
Clubfoot: Family, antenatal, and birth history should be obtained, including positive family history for clubfoot and the presence of environmental factors such as smoking, medication, alcohol intake, and solvent exposure. However, in some countries, the presence of deformities would be diagnosed during newborn screening. On physical exam, the foot or feet assume the characteristic clubfoot position; the mnemonic CAVE will help recall the order of deformities (cavus of the midfoot, adductus of the forefoot, varus, and equinus of the hindfoot).[52][53][54][55]
Variations in the degree of severity and rigidity may exist. Limb length and girdle discrepancy could also be noted, with a smaller foot and calf and shortened tibia on the affected side.[64][65] A thorough full-body clinical exam should ensue; in almost 20% of cases, clubfoot is part of the syndromes and medical conditions.[11]
Planovalgus: Medical history should be obtained to distinguish between congenital and acquired flatfoot deformity and the presence of other risk factors. Pes planovalgus is usually asymptomatic. However, some patients may experience plantar foot pain and ankle instability. During the physical exam, midfoot planus and hindfoot valgus, on standing, will be noted. Range of motion, gait pattern, and stability need to be assessed. Flatfoot will characteristically reconstitute to normal foot arch with toe walking and foot hanging out of bed.[66]
Cavovarus: History and physical are important in reaching the diagnosis. Conditions such as CMT, cerebral palsy, spinal cord lesions, Friedreich ataxia, amniotic band syndrome, and others should be evaluated as the potential cause of the cavovarus deformity. A neurological exam should always be performed. This is important as it may alter the course of the deformity and the treatment approach. A family history should also be obtained.[29][67]
The patients usually present with chronic foot pain, ankle instability, or painful calluses.[28] In the physical exam, the medial forefoot is plantarflexed and pronated, the midfoot is in cavus, and the hindfoot is in varus position. A convenient test to assess hindfoot flexibility is the Coleman block test. This test is performed with a 1-inch block placed under the lateral foot. If the hindfoot assumes a neutral or slightly valgus position while standing on the block, it reveals hindfoot flexibility and forefoot fixed deformity. In contrast, if the hindfoot remains in a varus position while standing on the block, it reveals a fixed hindfoot deformity.[68][69]
Another pathognomonic sign is the 'peek-a-boo sign,' where the examiner can see the foot arches with the patient standing while standing in front of the patient.[70] Examination of the spine and the gait pattern should be included to assess for spinal deformities and gait abnormalities.
Congenital vertical talus: A comprehensive medical and family history is essential to identify conditions associated with the congenital vertical talus. The examiner should evaluate the patient for distinguishing facial characteristics or other clues of underlying conditions. Clinically the CVT will appear as a 'rocker-bottom' deformity with a convex midfoot appearance. Forefoot dorsiflexion and hindfoot equinus and valgus should be present to qualify for the diagnosis of CVT. The gait pattern will reveal patients walking on their heels with limited foot contact. A thorough neurologic exam is also essential.[32][63][71][72]
Congenital oblique talus: Thorough history and physical exam are required to identify other conditions that may lead to COT, such as cerebral palsy, Down syndrome, and other neuromuscular syndromes. In the physical exam, the foot will be in pronation. In more severe cases, however, possible forefoot dorsiflexion, hindfoot valgus, and equinus position are assumed. A complete neurological examination should also be performed as COT is rarely associated with cerebral palsy. [35][73]
Metatarsus adductus: A detailed history is essential as some concomitant conditions are caused by the same intrauterine packaging phenomenon that causes metatarsus adductus. These conditions include developmental hip dysplasia, acetabular dysplasia, hip dislocation, and congenital torticollis.[36] On physical exam, the 'V finger test,' Bleck heel bisector method, and even the office photocopier have all been utilized to evaluate the metatarsus adductus. Radiographs are the least reliable in the pediatric population.[5]
Skew foot: Thorough past medical and family history is essential to identify secondary causes of skew foot deformity, such as neurological conditions or syndromes. On physical exam, foot deformity should be examined while standing and assessing both the foot's plantar and dorsal aspects. Physical exams may be challenging due to the plantar fat pad in children younger than one year. The patient will more likely present with in-toeing. Unlike simple or complex metatarsus adductus, where correction to the midline is achieved either actively or passively, in a skew foot, the deformity is rigid and will likely reveal adduction of the forefoot, abduction of the midfoot, and valgus of the hindfoot. Physical exam also includes work-up for other causes of in-toeing, such as increased hip anteversion and tibia internal rotation. Through neurological exam is also essential to identify causes of skew foot deformity.[37][38][40][41]
Evaluation
In most pediatric foot deformities, the diagnosis is clinical; however, radiographic imaging is performed to confirm the diagnosis and assist with preoperative planning. The standard method of radiologic evaluation of the foot involves weight-bearing or simulated weight-bearing anteroposterior (dorsoventral) and lateral views. Diagnosing foot alignment abnormalities should be approached cautiously when non-weight-bearing radiographs are obtained. In some cases, more specific views may be required. In complex cases, CT or MRI may be performed when more imaging detail is required or when multiple structures are involved.[1][2][3][74]
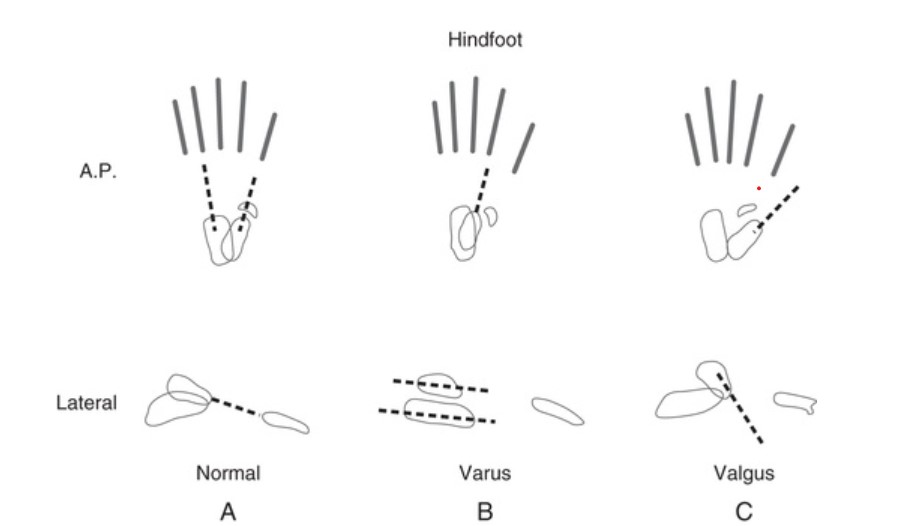
The proximally-located talus is considered fixed at the ankle because it has no direct musculotendinous attachments. The calcaneus is linked to the midfoot and forefoot and moves as a unit with these structures relative to the talus. In a normal foot, on the anteroposterior view, the axis of the talus extends through the base of the first metatarsal (Media item 1). With hindfoot varus, the more distal calcaneus is angulated inward, and the axis of the talus passes lateral to the base of the first metatarsal. With hindfoot valgus, the more distal calcaneus is angulated outward, and the axis of the talus passes medial to the base of the first metatarsal.[75]
The normal lateral talocalcaneal angle is approximately 45 degrees at birth, decreasing to 30 degrees in older children and adults. With hindfoot varus, the lateral talocalcaneal angle is decreased (more parallel), whereas, with hindfoot valgus, the angle is increased.
Normal elevation of the middle metatarsals relative to the fifth metatarsal reflects the foot's transverse arch. The anterior calcaneus is slightly inclined upward. Accentuating this upward inclination is called the calcaneus position of the os calcis. The equinus position is the downward inclination of the distal calcaneus. Normal calcaneal tilt and normal slight downward tilt of the distal metatarsals create a slight longitudinal concavity in the osseous contour of the bottom of the foot.
Clubfoot: The diagnosis of clubfoot is clinical; therefore, a radiograph examination is not always performed. Moreover, on some occasions, clubfoot may be diagnosed antenatally. If x-rays are performed, the dorsiflexion lateral (Turco) and anteroposterior (AP) views are ordered (Media item 2). In the Turco view, there is more hindfoot (between the calcaneus and the talus) parallelism, with a talocalcaneal angle of less than 25. The AP radiograph also reveals hindfoot parallelism, with a talocalcaneal angle (Kite angle) of less than 20 (normal angle is 20-40 degrees).[76] Ultrasound is also helpful when diagnosing clubfoot antenatally.[76]
Planovalgus: Although the diagnosis is clinical, further evaluation is warranted in some cases. Radiographic imaging may be performed in symptomatic pes cavovarus cases to exclude simultaneous concomitant pathologies of the foot (Media item 3). Imaging may also be performed in rigid flatfoot deformity. Anteroposterior, lateral, and oblique weight-bearing x-rays may be ordered. If Meary’s angle (angle between the talus and first metatarsal) in the lateral radiograph is more than 4 plantarflexed (normal is 0), then pes planovalgus is likely.[66]
Cavovarus: The diagnosis is mostly clinical. Anteroposterior (AP) and lateral radiographs are often performed (Media item 4). In AR radiograph, a talocalcaneal angle below 20 degrees (normal 20-45 degrees) indicates hindfoot varus deformity, and metatarsal overlap indicates forefoot pronation. In the lateral foot radiograph, the talo-first ray angle (Meary’s angle) of above 4 with dorsal apex indicates midfoot cavus (normal close to 0). An inclination angle above 30 degrees and a 'double talar dome' sign indicates midfoot cavus deformity.[28][77]
Further imaging can be performed as needed, such as CT or MRI. As almost two-thirds of the cases are associated with a neurological condition, most commonly Charcot-Marie-Tooth, further studies may be required, such as genetic testing and electrodiagnostic studies (EMG and nerve conduction studies) to establish the cause of the deformity.[77]
Congenital vertical talus: CVT is usually diagnosed in the first months of life; therefore, the relationship of the talus, calcaneus, and metatarsals becomes essential. Anteroposterior (AP) and lateral imaging of the foot are required (Media item 5). A forced plantarflexion lateral radiograph is required to establish the diagnosis of CVT. In the AP radiograph, the talocalcaneal angle is greater than 40 (normal 20 to 40 degrees). In the lateral radiograph, the longitudinal axis of the talus is not parallel to (passes below from) the longitudinal axis of the first metatarsal, and dorsal talonavicular dislocation is noted. With forced plantarflexion of the foot, the longitudinal axes of the talus and first metatarsal remain not parallel, which is pathognomonic of the CVT. Forced dorsiflexion lateral radiograph may reveal the hindfoot equinus.[32][63][71][72]
As CVT is commonly associated with neurological or genetic conditions, further work-up, such as MRI, nerve conduction studies, or genetic testing, may be warranted in case of characteristic findings from the physical exam.[32][63][71][72]
Congenital oblique talus: Anteroposterior (AP) and lateral radiograph of the foot are required (Media item 6). In the AP radiograph, the talocalcaneal angle will be increased (normal 20-40 degrees). In the lateral radiograph, the talus's longitudinal axis passes below the first metatarsal axis with dorsal subluxation of the talonavicular joint. With forced lateral flexion, however, the talonavicular joint is reduced, and the axes of the talus and first metatarsal become parallel because of its flexible deformity. Further evaluation (MRI, nerve conduction studies, genetic testing) may be required to exclude neuromuscular or genetic causes of COT.[35][73]
Metatarsus adductus: In the pediatric population, the diagnosis is clinical. The lack of tarsal bone ossification does not allow radiographic angles to be properly assessed, and therefore radiographs provide low reliability in this population. Clinically, many tests have been proposed in the literature. The Bleck’s heel bisector is the most used today, or 'heel bisector method.'[78][4][6]
The test is performed with the patient prone and the knees flexed at 90 degrees. An imaginary line is then observed from the bisection of the heel to the forefoot. The severity of the metatarsus adductus is determined to be mild if the line falls on the third toe, moderate if it is between the third and fourth toes, and severe if it is between the fourth and fifth toes.[6] Flexibility is also commonly tested and categorized as flexible (forefoot can abduct past the midline of the foot), semi-flexible (forefoot can be corrected up to the midline of the foot), or rigid (unable to reach the midline of the foot).[5]
Skew foot: Anteroposterior (AP) and lateral foot radiographs need to confirm the diagnosis (Media item 7). In the AP radiograph, the talocalcaneal angle will be increased (normal 20 to 40 degrees). The 1 metatarsal angle described by Barriolhet is increased (normal 50 to 70 degrees) and reveals forefoot adduction. The medial cuneiform medially deviates, while the navicular may be laterally deviated in the AP radiograph. In the lateral foot radiograph, the navicular bone may be dorsiflexed and medial cuneiform plantarflexed.[40][41][79] MRI or CT may also be useful in preoperative planning. Their disadvantage, however, is that they can not be performed with the patient standing, so weight-bearing angles cannot be measured.[39]
Treatment / Management
Management of foot deformities varies and ranges from conservative management with observation and reassurance to foot orthotics and casting to complex surgical procedures.[1][2][3]
Clubfoot: The gold-standard treatment option for clubfoot is the Ponseti method of serial casting, which should be applied as early as possible after birth.[55][80][81] The Pirani system applies before treatment initiation and involves six parameters for the foot. A higher Pirani initial score correlates with the possible need for increased numbers of casts and Achilles tenotomy.[82][83] (B3)
Plaster of Paris cast appliance should commence ideally within the first two weeks after birth, with weekly serial casting application and exchange. The order of correction is the midfoot cavus, forefoot adductus, hindfoot varus, and equinus; the CAVE mnemonic can help recall the order. Tendoachilles lengthening (TAL) at week 8 after implementation of serial casting is required in 80-90% of the patients.[84] After TAL, foot abduction orthosis (FAO) should be used until the age of 4 years, 23 hours per day for 3 months after TAL, followed by application only during nighttime until age 4. A possible tibialis anterior transfer may be required in almost 20% of the patients.[85](B2)
The French method of daily manipulation and physical therapy has also been reported as an alternative method of clubfoot correction. However, it is not used in the United States as it requires strict adherence to daily manipulation and provides relatively good outcomes only in skilled hands.[54]
In residual clubfoot deformities, various surgical options exist, such as PMR, tendon transfers, osteotomies, and arthrodesis.[84]
Planovalgus: Management is conservative in most cases, as it is usually temporary, especially in children. In adults, management is based on the etiology of the deformity. Stretching, shoewear modification, and heel support with orthotics have been tried and are usually applied to asymptomatic or slightly symptomatic patients.[86][87][88] The orthotics use, however, does not change the course of the deformity. Surgical management can be implemented in symptomatic patients, where conservative management failed, in fixed deformity cases, and in cases with underlying risk factors. Although rarely indicated, the Evans calcaneal lengthening osteotomy is the most commonly performed.[87][89][90](A1)
Cavovarus: Management varies and ranges from foot orthotics to surgery. Although foot orthotics have been used, there are often reserved for mild cases or as adjuvants before or after surgical procedures.[91] Different types of foot orthosis have been described, such as ankle foot orthosis (AFO), supramalleolar orthosis, and insole orthotic with lateral wedge and fixed plantarflexion of the first ray.
However, the optimal management of pes cavovarus is surgical, as foot orthosis alone is insufficient for most cases. The surgical approaches vary and depend on whether a fixed forefoot or hindfoot component causes the deformity.[58][92]
In the case of flexible hindfoot deformity, where the cavus is produced by fixed forefoot deformity, the patient may benefit from dorsiflexion osteotomy of the first metatarsal and plantar fascia release. In the case of fixed hindfoot deformity (hindfoot remains varus during Coleman's block test), the patient may benefit from lateral valgus-producing calcaneal osteotomy and peroneus longus to brevis transfer and with procedures for the forefoot.[29][69][93] (B2)
Other soft tissue release approaches include posterior tibia tendon transfer, Achilles tenotomy, Broström ligament reconstruction (performed for ankle instability), and Jones tendon transfers (transfer of the extensor hallucis longus and extensor of the digit tendons to the dorsum of the metatarsals).[28][58][94] Triple arthrodesis has also been described but is reserved for failure of the other approaches as it produces inferior results.[95]
Congenital vertical talus: The goal of the treatment is to avoid complications and render the patients able to walk. Conservative treatment alone is rarely sufficient for CVT. The most commonly used management strategy is an initial application of long-leg serial casts, followed by soft tissue releases and talonavicular joint fixation. The treatment yields better results when performed before the age of 2.
Serial casting and manipulation are initially performed to stretch the soft tissues for the surgery. Once reduction is achieved with casts, open reduction of the talonavicular joint with pin fixation is performed. Achilles tenotomy is also usually required to correct the equinus contracture, along with possible lengthening of the peroneals and toe extensors. The surgical approach can be performed in one or two stages. Triple arthrodesis is reserved for cases that failed prior surgical treatment or when the diagnosis of CVT is made at a later age, and no other surgical option is available.[32][96][97][98](B2)
Congenital oblique talus: Treatment ranges from observation to using shoe inserts or casting and surgical approach for more severe cases. Most cases of COT are successfully treated with shoe inserts or even need just observation. However, in cases that failed conservative management, with more fixed equinus, and when talonavicular joint subluxation persists, serial casting with talonavicular fixation and soft tissue release are warranted. Talonavicular fixation is achieved with open reduction and talonavicular pinning to reduce fixed talonavicular subluxation and requires adjuvant Achilles tenotomy to correct fixed equinus deformity.[35][73]
Metatarsus adductus: Most deformities reach a spontaneous complete resolution before age one year. However, 4 to 14% of all metatarsus adductus deformities progress to rigid deformities in adulthood.[99] The severity of the deformity and the patient's age will define the treatment plan.[6] Flexible mild metatarsus adductus does not require treatment.[6] Parents should be advised to adjust sitting/ sleeping positions, manually abduct the forefoot while maintaining the hindfoot in neutral, and change footwear. Severe and rigid deformities require intervention. Once a decision is made to start treatment, for best results, the literature suggests starting treatment before 8 or 9 months of age.[100]
Historically, serial casting has been the gold standard treatment for metatarsus adductus. However, they are usually not well tolerated by the pediatric population, with side effects such as skin bruises, circulatory problems, deep wounds, and nerve injury being described. In the past 30 years, many research papers tried to find a solution for these side effects by reporting the use of new orthoses as an alternative to casting. Some of these include Bebax, a below-the-ankle orthosis shown to be as successful as casting, and Universal Neonatal Foot Orthotics (UNFO), a practical foot orthotic that a caregiver instead of the physician can adjust.[100]
If conservative treatment fails in symptomatic severe and rigid cases, surgery is an option. Different procedures have been described without a consensus on the best option. Options include tarsometatarsal capsulotomies for patients aged 2 to 4 years, a combination of dome shape or close wedge osteotomies on all lesser metatarsals, and usually an opening wedge osteotomy on the medial column in patients older than 4 years.[101][102][103] Nevertheless, surgery for the metatarsus adductus is notorious for showing variable outcomes, with a high rate of failure or recurrence. In addition, the deformity is usually asymptomatic in adulthood, and surgery is rarely indicated.
Skew foot: There is no clear consensus regarding the treatment approach. It usually depends on the severity of the deformities and the age at diagnosis. Conservative management, such as serial long-leg casting with hindfoot valgus molding, can be used initially. Surgery is usually reserved for more severe cases and deferred after the age of 6 years as all three components of the foot (forefoot, midfoot, and hindfoot) need correction. If surgery is needed, multiple forefoot, midfoot, and hindfoot osteotomies are performed. In the forefoot, shortening of the lateral column and opening of the medial column osteotomies are needed to correct forefoot adduction. This is performed in combination with calcaneal opening wedge osteotomy.[37][38][40][41][79]
Differential Diagnosis
Pediatric foot deformities may share similar characteristics, and their clinical pictures may resemble other foot entities. Therefore, it is essential to distinguish among different pediatric foot deformities.
Clubfoot: Clubfoot has a characteristic appearance and is difficult to be confused with other foot deformities. However, other congenital foot deformities, such as congenital vertical talus or calcaneovalgus, should be excluded. It is essential to differentiate clubfoot from other correctable conditions or deformities.
Planovalgus: Differential diagnosis is limited. Pes planovalgus should be differentiated from the prominent arch fat pad and tarsal coalition.
Cavovarus: Cavovarus foot should be differentiated from equinovarus foot.[104]
Congenital vertical talus: CVT should be differentiated from congenital oblique talus. The lateral radiograph will depict no parallel longitudinal axes of the talus and first metatarsal in both conditions. In congenital oblique talus, however, with forced plantarflexion, the talonavicular joint is reduced, so the parallel longitudinal axes of the talus and first metatarsal become parallel, meaning that it is a flexible deformity. Other differentials include tarsal coalition and pes planovalgus.[32][63]
Congenital oblique talus: Differential diagnoses include congenital vertical talus (forced plantarflexion does not cause reduction of the talonavicular joint) and pes planovalgus.[35]
Metatarsus adductus: Due to the distinct in-toeing gait, the metatarsus adductus can be confused with internal tibial torsion and increased femoral anteversion.[105]
Skew foot: Skewfoot may be differentiated from simple or complex metatarsus adductus, equinovarus, and pes planus.[40][79]
Prognosis
The prognosis depends on the deformity's cause and complexity and whether it is primary or associated with other medical conditions.
Clubfoot: The Ponseti method has a reported success rate of around 90% in reducing the need for posteromedial surgical release (PMR), with children expected to be able to walk independently and even run and be active after the end of the treatment.[106][107]
Planovalgus: Prognosis varies depending on age and the underlying risk factors. However, the deformity resolves spontaneously in most cases, especially in children.[89]
Cavovarus: Prognosis is associated with the underlying condition leading to cavovarus deformities.[108]
Congenital vertical talus: The prognosis depends on the age at which the patient is diagnosed and the staging of the CVT.
Congenital oblique talus: COT may be considered a physiologic, anatomic variant. Prognosis, therefore, varies and depends on the degree of the deformity.[35]
Metatarsus adductus: Excellent prognosis, with 90% of flexible metatarsus adductus resolving spontaneously without intervention.[5][6]
Skew foot: Prognosis varies and, in severe cases, may lead to foot pain or dysfunction.
Complications
Complications include consequences from the progression of the deformity where inadequate treatment is obtained and consequences from treatment failure.
Clubfoot: The most commonly reported complication is deformity relapse, primarily due to non-compliance.[109] FAO application is crucial for recurrence avoidance.[53] Repeating Ponseti method casting may be sufficient in children under two years old, while TAL and tendon transfers are usually required in older children.[110] Rocker bottom deformity may also occur if correction of hindfoot equinus is attempted before correction of hindfoot varus.[111] After treatment with the Ponseti method, residual dynamic supination can be managed with anterior tibialis transfer with good results.[112]
Complications with surgical management include under-correction, dorsal bunion, residual cavus, in-toeing gait, and pes planus, among others.[113]
Planovalgus: Complications are associated with long-term conditions such as persistent pain or arthritis. Postoperative complications may include surgical site infection, hardware failure, malunion, or non-union.[89]
Cavovarus: A delay in the diagnosis may lead to a rigid deformity. Complications include ankle instability, stress fractures of the 4 and 5 metatarsals, peroneal tendon pathology, and plantar fasciitis. Chronic ankle instability may lead to arthritis.[114][115][116]
Congenital vertical talus: If left untreated, CVT will cause a fixed “rocker-bottom” deformity and, if diagnosed much later than two years of age, may require triple arthrodesis.
Congenital oblique talus: Complications are rare if COT is a physiologic, anatomic variant. In more severe cases or if COT is associated with neurological conditions, COT may lead to fixed foot deformity and difficulty with walking.
Metatarsus adductus: Conservative treatment provides minimal to no complications. However, surgical intervention has a history of high complication rates, including stress risers, osseous bridging between the metatarsals, loss of purchase of the distal cortex, inability to hold correction, and unequal bone removal when surgery is performed on all metatarsals.[101][99][6]
Skew foot: Skefoot deformity may lead to problems with walking and foot development if left untreated.
Deterrence and Patient Education
Patient and parents’ education and counseling should be provided for all causes of pediatric foot deformity. In addition, parents should be aware that pediatric foot deformity prognosis depends on the severity and complexity of the deformities. Therefore treatment approaches could vary and range from observation to casting to surgery. In most cases, deformities are congenital. However, they may be secondary to neurological, endocrine, or genetic conditions.
Enhancing Healthcare Team Outcomes
An interprofessional approach is crucial for the patients' proper diagnosis, management, and follow-up. The team should include the primary care clinician or pediatrician, the specialized orthopedic team (pediatric orthopedic specialist, pediatric orthopedic nurse, cast technician, pediatric anesthesiologist, pediatric orthopedic scrub nurse), pediatric psychologist, play therapists, physiotherapists, and orthotic providers. The patients may need weekly changes and application of casts and may also need individualized postoperative care. Precise and careful collaboration between all involved members of the interprofessional team is essential for the optimal outcome of every pediatric patient. [Level 5]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
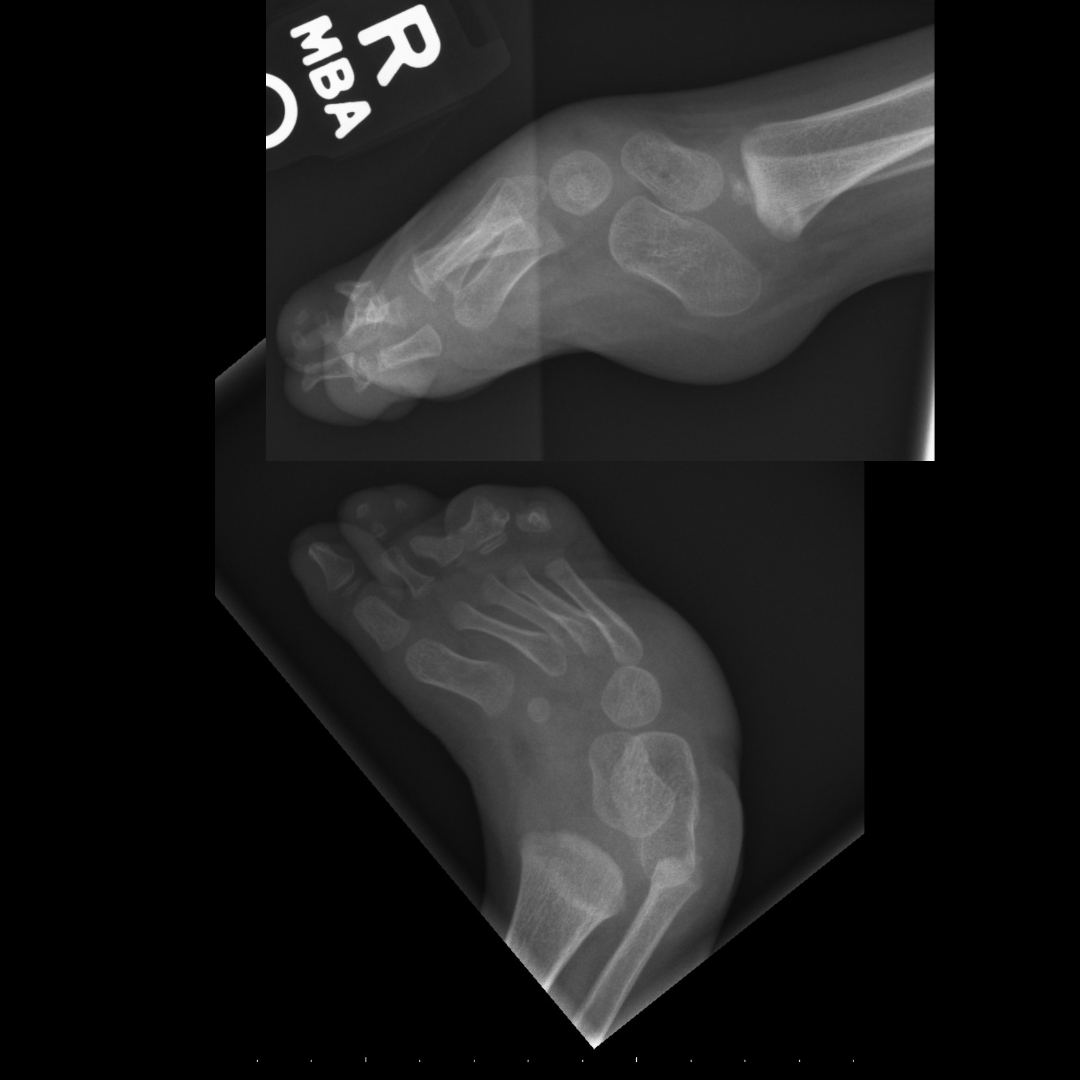
Clubfoot. Right foot radiographs demonstrating severe hindfoot varus on frontal view with talus and calcaneus in parallel orientation on the lateral view, metatarsals adducted and supinated on frontal with ladder-like arrangement on lateral and the calcaneus in equinus. Contributed by Aby Thomas, MD
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Churgay CA. Diagnosis and treatment of pediatric foot deformities. American family physician. 1993 Mar:47(4):883-9 [PubMed PMID: 8438686]
Hoffinger SA. Evaluation and management of pediatric foot deformities. Pediatric clinics of North America. 1996 Oct:43(5):1091-111 [PubMed PMID: 8858075]
Winfeld MJ, Winfeld BE. Management of pediatric foot deformities: an imaging review. Pediatric radiology. 2019 Nov:49(12):1678-1690. doi: 10.1007/s00247-019-04503-4. Epub 2019 Nov 4 [PubMed PMID: 31686173]
Marshall N, Ward E, Williams CM. The identification and appraisal of assessment tools used to evaluate metatarsus adductus: a systematic review of their measurement properties. Journal of foot and ankle research. 2018:11():25. doi: 10.1186/s13047-018-0268-z. Epub 2018 Jun 1 [PubMed PMID: 29881466]
Level 1 (high-level) evidenceWilliams CM, James AM, Tran T. Metatarsus adductus: development of a non-surgical treatment pathway. Journal of paediatrics and child health. 2013 Sep:49(9):E428-33. doi: 10.1111/jpc.12219. Epub 2013 May 6 [PubMed PMID: 23647850]
Level 1 (high-level) evidenceRerucha CM, Dickison C, Baird DC. Lower Extremity Abnormalities in Children. American family physician. 2017 Aug 15:96(4):226-233 [PubMed PMID: 28925669]
Lochmiller C, Johnston D, Scott A, Risman M, Hecht JT. Genetic epidemiology study of idiopathic talipes equinovarus. American journal of medical genetics. 1998 Sep 1:79(2):90-6 [PubMed PMID: 9741465]
Weymouth KS, Blanton SH, Powell T, Patel CV, Savill SA, Hecht JT. Functional Assessment of Clubfoot Associated HOXA9, TPM1, and TPM2 Variants Suggests a Potential Gene Regulation Mechanism. Clinical orthopaedics and related research. 2016 Jul:474(7):1726-35. doi: 10.1007/s11999-016-4788-1. Epub 2016 Mar 28 [PubMed PMID: 27020427]
Basit S, Khoshhal KI. Genetics of clubfoot; recent progress and future perspectives. European journal of medical genetics. 2018 Feb:61(2):107-113. doi: 10.1016/j.ejmg.2017.09.006. Epub 2017 Sep 14 [PubMed PMID: 28919208]
Level 3 (low-level) evidenceDobbs MB, Gurnett CA. Genetics of clubfoot. Journal of pediatric orthopedics. Part B. 2012 Jan:21(1):7-9. doi: 10.1097/BPB.0b013e328349927c. Epub [PubMed PMID: 21817922]
Level 3 (low-level) evidenceGurnett CA, Boehm S, Connolly A, Reimschisel T, Dobbs MB. Impact of congenital talipes equinovarus etiology on treatment outcomes. Developmental medicine and child neurology. 2008 Jul:50(7):498-502. doi: 10.1111/j.1469-8749.2008.03016.x. Epub [PubMed PMID: 18611198]
Level 2 (mid-level) evidenceParker SE, Mai CT, Strickland MJ, Olney RS, Rickard R, Marengo L, Wang Y, Hashmi SS, Meyer RE, National Birth Defects Prevention Network. Multistate study of the epidemiology of clubfoot. Birth defects research. Part A, Clinical and molecular teratology. 2009 Nov:85(11):897-904. doi: 10.1002/bdra.20625. Epub [PubMed PMID: 19697433]
Honein MA, Paulozzi LJ, Moore CA. Family history, maternal smoking, and clubfoot: an indication of a gene-environment interaction. American journal of epidemiology. 2000 Oct 1:152(7):658-65 [PubMed PMID: 11032161]
Level 2 (mid-level) evidenceChen C, Kaushal N, Scher DM, Doyle SM, Blanco JS, Dodwell ER. Clubfoot Etiology: A Meta-Analysis and Systematic Review of Observational and Randomized Trials. Journal of pediatric orthopedics. 2018 Sep:38(8):e462-e469. doi: 10.1097/BPO.0000000000001191. Epub [PubMed PMID: 29917009]
Level 1 (high-level) evidenceHalmesmäki E, Raivio K, Ylikorkala O. A possible association between maternal drinking and fetal clubfoot. The New England journal of medicine. 1985 Mar 21:312(12):790 [PubMed PMID: 3974658]
Level 3 (low-level) evidenceDodwell E, Risoe P, Wright J. Factors Associated With Increased Risk of Clubfoot: A Norwegian National Cohort Analysis. Journal of pediatric orthopedics. 2015 Dec:35(8):e104-9. doi: 10.1097/BPO.0000000000000449. Epub [PubMed PMID: 26539903]
Nemeth B. The diagnosis and management of common childhood orthopedic disorders. Current problems in pediatric and adolescent health care. 2011 Jan:41(1):2-28. doi: 10.1016/j.cppeds.2010.10.004. Epub [PubMed PMID: 21195338]
Halabchi F, Mazaheri R, Mirshahi M, Abbasian L. Pediatric flexible flatfoot; clinical aspects and algorithmic approach. Iranian journal of pediatrics. 2013 Jun:23(3):247-60 [PubMed PMID: 23795246]
Mickle KJ, Steele JR, Munro BJ. The feet of overweight and obese young children: are they flat or fat? Obesity (Silver Spring, Md.). 2006 Nov:14(11):1949-53 [PubMed PMID: 17135610]
Level 2 (mid-level) evidenceGajendran VK, Yoo BJ, Hunter JC. Unusual Variant of the Nutcracker Fracture of the Calcaneus and Tarsal Navicular. Radiology case reports. 2008:3(3):208. doi: 10.2484/rcr.v3i3.208. Epub 2015 Nov 6 [PubMed PMID: 27303549]
Level 3 (low-level) evidenceLindsey JM, Michelson JD, MacWilliams BA, Sponseller PD, Miller NH. The foot in Marfan syndrome: clinical findings and weight-distribution patterns. Journal of pediatric orthopedics. 1998 Nov-Dec:18(6):755-9 [PubMed PMID: 9821131]
Perotti LR, Abousamra O, Del Pilar Duque Orozco M, Rogers KJ, Sees JP, Miller F. Foot and ankle deformities in children with Down syndrome. Journal of children's orthopaedics. 2018 Jun 1:12(3):218-226. doi: 10.1302/1863-2548.12.170197. Epub [PubMed PMID: 29951120]
Shirley ED, Demaio M, Bodurtha J. Ehlers-danlos syndrome in orthopaedics: etiology, diagnosis, and treatment implications. Sports health. 2012 Sep:4(5):394-403 [PubMed PMID: 23016112]
Bubra PS, Keighley G, Rateesh S, Carmody D. Posterior tibial tendon dysfunction: an overlooked cause of foot deformity. Journal of family medicine and primary care. 2015 Jan-Mar:4(1):26-9. doi: 10.4103/2249-4863.152245. Epub [PubMed PMID: 25810985]
Kohls-Gatzoulis J, Woods B, Angel JC, Singh D. The prevalence of symptomatic posterior tibialis tendon dysfunction in women over the age of 40 in England. Foot and ankle surgery : official journal of the European Society of Foot and Ankle Surgeons. 2009:15(2):75-81. doi: 10.1016/j.fas.2008.08.003. Epub 2008 Oct 1 [PubMed PMID: 19410173]
Nogueira MP, Farcetta F, Zuccon A. Cavus Foot. Foot and ankle clinics. 2015 Dec:20(4):645-56. doi: 10.1016/j.fcl.2015.07.007. Epub 2015 Oct 23 [PubMed PMID: 26589083]
Krähenbühl N, Weinberg MW. Anatomy and Biomechanics of Cavovarus Deformity. Foot and ankle clinics. 2019 Jun:24(2):173-181. doi: 10.1016/j.fcl.2019.02.001. Epub 2019 Apr 2 [PubMed PMID: 31036262]
Rosenbaum AJ, Lisella J, Patel N, Phillips N. The cavus foot. The Medical clinics of North America. 2014 Mar:98(2):301-12. doi: 10.1016/j.mcna.2013.10.008. Epub 2014 Jan 8 [PubMed PMID: 24559876]
Younger AS, Hansen ST Jr. Adult cavovarus foot. The Journal of the American Academy of Orthopaedic Surgeons. 2005 Sep:13(5):302-15 [PubMed PMID: 16148356]
Aroojis AJ, King MM, Donohoe M, Riddle EC, Kumar SJ. Congenital vertical talus in arthrogryposis and other contractural syndromes. Clinical orthopaedics and related research. 2005 May:(434):26-32 [PubMed PMID: 15864028]
Level 2 (mid-level) evidenceRubio EI, Mehta N, Blask AR, Bulas DI. Prenatal congenital vertical talus (rocker bottom foot): a marker for multisystem anomalies. Pediatric radiology. 2017 Dec:47(13):1793-1799. doi: 10.1007/s00247-017-3957-z. Epub 2017 Sep 6 [PubMed PMID: 28879597]
Miller M, Dobbs MB. Congenital Vertical Talus: Etiology and Management. The Journal of the American Academy of Orthopaedic Surgeons. 2015 Oct:23(10):604-11. doi: 10.5435/JAAOS-D-14-00034. Epub 2015 Sep 3 [PubMed PMID: 26337950]
Dobbs MB, Gurnett CA, Robarge J, Gordon JE, Morcuende JA, Bowcock AM. Variable hand and foot abnormalities in family with congenital vertical talus and CDMP-1 gene mutation. Journal of orthopaedic research : official publication of the Orthopaedic Research Society. 2005 Nov:23(6):1490-4 [PubMed PMID: 16005596]
Dobbs MB, Gurnett CA, Pierce B, Exner GU, Robarge J, Morcuende JA, Cole WG, Templeton PA, Foster B, Bowcock AM. HOXD10 M319K mutation in a family with isolated congenital vertical talus. Journal of orthopaedic research : official publication of the Orthopaedic Research Society. 2006 Mar:24(3):448-53 [PubMed PMID: 16450407]
Harris EJ. The oblique talus deformity. What is it, and what is its clinical significance in the scheme of pronatory deformities? Clinics in podiatric medicine and surgery. 2000 Jul:17(3):419-42 [PubMed PMID: 10943497]
Varacallo M, Aiyer A. Metatarsalgia in Metatarsus Adductus Patients: A Rational Approach. Foot and ankle clinics. 2019 Dec:24(4):657-667. doi: 10.1016/j.fcl.2019.08.002. Epub 2019 Sep 25 [PubMed PMID: 31653370]
Napiontek M. Skewfoot. Journal of pediatric orthopedics. 2002 Jan-Feb:22(1):130-3 [PubMed PMID: 11744869]
Mosca VS. Flexible flatfoot and skewfoot. Instructional course lectures. 1996:45():347-54 [PubMed PMID: 8727755]
Hubbard AM, Davidson RS, Meyer JS, Mahboubi S. Magnetic resonance imaging of skewfoot. The Journal of bone and joint surgery. American volume. 1996 Mar:78(3):389-97 [PubMed PMID: 8613446]
Hagmann S, Dreher T, Wenz W. Skewfoot. Foot and ankle clinics. 2009 Sep:14(3):409-34. doi: 10.1016/j.fcl.2009.06.003. Epub [PubMed PMID: 19712883]
Hutchinson B. Pediatric metatarsus adductus and skewfoot deformity. Clinics in podiatric medicine and surgery. 2010 Jan:27(1):93-104. doi: 10.1016/j.cpm.2009.09.005. Epub [PubMed PMID: 19963172]
Smythe T, Kuper H, Macleod D, Foster A, Lavy C. Birth prevalence of congenital talipes equinovarus in low- and middle-income countries: a systematic review and meta-analysis. Tropical medicine & international health : TM & IH. 2017 Mar:22(3):269-285. doi: 10.1111/tmi.12833. Epub 2017 Jan 22 [PubMed PMID: 28000394]
Level 1 (high-level) evidenceChing GH, Chung CS, Nemechek RW. Genetic and epidemiological studies of clubfoot in Hawaii: ascertainment and incidence. American journal of human genetics. 1969 Nov:21(6):566-80 [PubMed PMID: 5365759]
Level 2 (mid-level) evidenceWallander H, Hovelius L, Michaelsson K. Incidence of congenital clubfoot in Sweden. Acta orthopaedica. 2006 Dec:77(6):847-52 [PubMed PMID: 17260191]
Pita-Fernandez S, Gonzalez-Martin C, Alonso-Tajes F, Seoane-Pillado T, Pertega-Diaz S, Perez-Garcia S, Seijo-Bestilleiro R, Balboa-Barreiro V. Flat Foot in a Random Population and its Impact on Quality of Life and Functionality. Journal of clinical and diagnostic research : JCDR. 2017 Apr:11(4):LC22-LC27. doi: 10.7860/JCDR/2017/24362.9697. Epub 2017 Apr 1 [PubMed PMID: 28571173]
Level 2 (mid-level) evidenceLauterbach S, Kostev K, Becker R. Characteristics of diabetic patients visiting a podiatry practice in Germany. Journal of wound care. 2010 Apr:19(4):140, 142, 144 passim [PubMed PMID: 20379125]
Aenumulapalli A, Kulkarni MM, Gandotra AR. Prevalence of Flexible Flat Foot in Adults: A Cross-sectional Study. Journal of clinical and diagnostic research : JCDR. 2017 Jun:11(6):AC17-AC20. doi: 10.7860/JCDR/2017/26566.10059. Epub 2017 Jun 1 [PubMed PMID: 28764143]
Level 2 (mid-level) evidenceJapas LM. Surgical treatment of pes cavus by tarsal V-osteotomy. Preliminary report. The Journal of bone and joint surgery. American volume. 1968 Jul:50(5):927-44 [PubMed PMID: 5676832]
Nagai MK, Chan G, Guille JT, Kumar SJ, Scavina M, Mackenzie WG. Prevalence of Charcot-Marie-Tooth disease in patients who have bilateral cavovarus feet. Journal of pediatric orthopedics. 2006 Jul-Aug:26(4):438-43 [PubMed PMID: 16791058]
Level 2 (mid-level) evidenceLedoux WR, Shofer JB, Ahroni JH, Smith DG, Sangeorzan BJ, Boyko EJ. Biomechanical differences among pes cavus, neutrally aligned, and pes planus feet in subjects with diabetes. Foot & ankle international. 2003 Nov:24(11):845-50 [PubMed PMID: 14655889]
Jacobsen ST, Crawford AH. Congenital vertical talus. Journal of pediatric orthopedics. 1983 Jul:3(3):306-10 [PubMed PMID: 6874927]
Cummings RJ, Davidson RS, Armstrong PF, Lehman WB. Congenital clubfoot. Instructional course lectures. 2002:51():385-400 [PubMed PMID: 12064128]
Herzenberg JE, Radler C, Bor N. Ponseti versus traditional methods of casting for idiopathic clubfoot. Journal of pediatric orthopedics. 2002 Jul-Aug:22(4):517-21 [PubMed PMID: 12131451]
Level 2 (mid-level) evidenceNoonan KJ, Richards BS. Nonsurgical management of idiopathic clubfoot. The Journal of the American Academy of Orthopaedic Surgeons. 2003 Nov-Dec:11(6):392-402 [PubMed PMID: 14686824]
Ponseti IV. The ponseti technique for correction of congenital clubfoot. The Journal of bone and joint surgery. American volume. 2002 Oct:84(10):1889-90; author reply 1890-1 [PubMed PMID: 12377924]
Level 3 (low-level) evidenceVan Boerum DH, Sangeorzan BJ. Biomechanics and pathophysiology of flat foot. Foot and ankle clinics. 2003 Sep:8(3):419-30 [PubMed PMID: 14560896]
Kido M, Ikoma K, Imai K, Tokunaga D, Inoue N, Kubo T. Load response of the medial longitudinal arch in patients with flatfoot deformity: in vivo 3D study. Clinical biomechanics (Bristol, Avon). 2013 Jun:28(5):568-73. doi: 10.1016/j.clinbiomech.2013.04.004. Epub 2013 May 2 [PubMed PMID: 23643289]
Level 1 (high-level) evidenceKaplan JRM, Aiyer A, Cerrato RA, Jeng CL, Campbell JT. Operative Treatment of the Cavovarus Foot. Foot & ankle international. 2018 Nov:39(11):1370-1382. doi: 10.1177/1071100718798817. Epub 2018 Oct 4 [PubMed PMID: 30284471]
Manoli A 2nd, Graham B. The subtle cavus foot, "the underpronator". Foot & ankle international. 2005 Mar:26(3):256-63 [PubMed PMID: 15766431]
Mann DC, Hsu JD. Triple arthrodesis in the treatment of fixed cavovarus deformity in adolescent patients with Charcot-Marie-Tooth disease. Foot & ankle. 1992 Jan:13(1):1-6 [PubMed PMID: 1577335]
Drennan JC. Congenital vertical talus. Instructional course lectures. 1996:45():315-22 [PubMed PMID: 8727751]
Seimon LP. Surgical correction of congenital vertical talus under the age of 2 years. Journal of pediatric orthopedics. 1987 Jul-Aug:7(4):405-11 [PubMed PMID: 3611335]
McKie J, Radomisli T. Congenital vertical talus: a review. Clinics in podiatric medicine and surgery. 2010 Jan:27(1):145-56. doi: 10.1016/j.cpm.2009.08.008. Epub [PubMed PMID: 19963176]
Shimode K, Miyagi N, Majima T, Yasuda K, Minami A. Limb length and girth discrepancy of unilateral congenital clubfeet. Journal of pediatric orthopedics. Part B. 2005 Jul:14(4):280-4 [PubMed PMID: 15931033]
Spiegel DA, Loder RT. Leg-length discrepancy and bone age in unilateral idiopathic talipes equinovarus. Journal of pediatric orthopedics. 2003 Mar-Apr:23(2):246-50 [PubMed PMID: 12604959]
Level 2 (mid-level) evidenceAlazzawi S, Sukeik M, King D, Vemulapalli K. Foot and ankle history and clinical examination: A guide to everyday practice. World journal of orthopedics. 2017 Jan 18:8(1):21-29. doi: 10.5312/wjo.v8.i1.21. Epub 2017 Jan 18 [PubMed PMID: 28144575]
Eleswarapu AS, Yamini B, Bielski RJ. Evaluating the Cavus Foot. Pediatric annals. 2016 Jun 1:45(6):e218-22. doi: 10.3928/00904481-20160426-01. Epub [PubMed PMID: 27294497]
Coleman SS, Chesnut WJ. A simple test for hindfoot flexibility in the cavovarus foot. Clinical orthopaedics and related research. 1977 Mar-Apr:(123):60-2 [PubMed PMID: 852192]
Paulos L, Coleman SS, Samuelson KM. Pes cavovarus. Review of a surgical approach using selective soft-tissue procedures. The Journal of bone and joint surgery. American volume. 1980 Sep:62(6):942-53 [PubMed PMID: 7430182]
Manoli A 2nd, Smith DG, Hansen ST Jr. Scarred muscle excision for the treatment of established ischemic contracture of the lower extremity. Clinical orthopaedics and related research. 1993 Jul:(292):309-14 [PubMed PMID: 8519125]
OUTLAND T, SHERK HH. Congenital vertical talus. Clinical orthopaedics. 1960:16():214-8 [PubMed PMID: 14429483]
Hamanishi C. Congenital vertical talus: classification with 69 cases and new measurement system. Journal of pediatric orthopedics. 1984 May:4(3):318-26 [PubMed PMID: 6736236]
Level 3 (low-level) evidenceHart ES, Grottkau BE, Rebello GN, Albright MB. The newborn foot: diagnosis and management of common conditions. Orthopedic nursing. 2005 Sep-Oct:24(5):313-21; quiz 322-3 [PubMed PMID: 16272908]
Reginelli A, Russo A, Turrizziani F, Picascia R, Micheletti E, Galeazzi V, Russo U, Sica A, Cioce F, Aliprandi A, Giovagnoni A, Cappabianca S. Imaging of pediatric foot disorders. Acta bio-medica : Atenei Parmensis. 2018 Jan 19:89(1-S):34-47. doi: 10.23750/abm.v89i1-S.7009. Epub 2018 Jan 19 [PubMed PMID: 29350636]
Thapa MM, Pruthi S, Chew FS. Radiographic assessment of pediatric foot alignment: review. AJR. American journal of roentgenology. 2010 Jun:194(6 Suppl):S51-8. doi: 10.2214/AJR.07.7143. Epub [PubMed PMID: 20489117]
Level 3 (low-level) evidenceRoye DP Jr, Roye BD. Idiopathic congenital talipes equinovarus. The Journal of the American Academy of Orthopaedic Surgeons. 2002 Jul-Aug:10(4):239-48 [PubMed PMID: 15089073]
Akoh CC, Phisitkul P. Clinical Examination and Radiographic Assessment of the Cavus Foot. Foot and ankle clinics. 2019 Jun:24(2):183-193. doi: 10.1016/j.fcl.2019.02.002. Epub 2019 Apr 2 [PubMed PMID: 31036263]
Bleck EE. Metatarsus adductus: classification and relationship to outcomes of treatment. Journal of pediatric orthopedics. 1983 Feb:3(1):2-9 [PubMed PMID: 6841597]
Greene WB. Metatarsus adductus and skewfoot. Instructional course lectures. 1994:43():161-77 [PubMed PMID: 9097146]
Ponseti IV. Treatment of congenital club foot. The Journal of bone and joint surgery. American volume. 1992 Mar:74(3):448-54 [PubMed PMID: 1548277]
Radler C. The Ponseti method for the treatment of congenital club foot: review of the current literature and treatment recommendations. International orthopaedics. 2013 Sep:37(9):1747-53. doi: 10.1007/s00264-013-2031-1. Epub 2013 Aug 9 [PubMed PMID: 23928728]
Dyer PJ, Davis N. The role of the Pirani scoring system in the management of club foot by the Ponseti method. The Journal of bone and joint surgery. British volume. 2006 Aug:88(8):1082-4 [PubMed PMID: 16877610]
Flynn JM, Donohoe M, Mackenzie WG. An independent assessment of two clubfoot-classification systems. Journal of pediatric orthopedics. 1998 May-Jun:18(3):323-7 [PubMed PMID: 9600557]
Hosseinzadeh P, Kelly DM, Zionts LE. Management of the Relapsed Clubfoot Following Treatment Using the Ponseti Method. The Journal of the American Academy of Orthopaedic Surgeons. 2017 Mar:25(3):195-203. doi: 10.5435/JAAOS-D-15-00624. Epub [PubMed PMID: 28195983]
Bor N, Coplan JA, Herzenberg JE. Ponseti treatment for idiopathic clubfoot: minimum 5-year followup. Clinical orthopaedics and related research. 2009 May:467(5):1263-70. doi: 10.1007/s11999-008-0683-8. Epub 2009 Jan 7 [PubMed PMID: 19130158]
Level 2 (mid-level) evidenceJane MacKenzie A, Rome K, Evans AM. The efficacy of nonsurgical interventions for pediatric flexible flat foot: a critical review. Journal of pediatric orthopedics. 2012 Dec:32(8):830-4. doi: 10.1097/BPO.0b013e3182648c95. Epub [PubMed PMID: 23147627]
Mosca VS. Flexible flatfoot in children and adolescents. Journal of children's orthopaedics. 2010 Apr:4(2):107-21. doi: 10.1007/s11832-010-0239-9. Epub 2010 Feb 18 [PubMed PMID: 21455468]
Wenger DR, Mauldin D, Speck G, Morgan D, Lieber RL. Corrective shoes and inserts as treatment for flexible flatfoot in infants and children. The Journal of bone and joint surgery. American volume. 1989 Jul:71(6):800-10 [PubMed PMID: 2663868]
Level 1 (high-level) evidenceVulcano E, Deland JT, Ellis SJ. Approach and treatment of the adult acquired flatfoot deformity. Current reviews in musculoskeletal medicine. 2013 Dec:6(4):294-303. doi: 10.1007/s12178-013-9173-z. Epub [PubMed PMID: 23765382]
Rodriguez N, Choung DJ, Dobbs MB. Rigid pediatric pes planovalgus: conservative and surgical treatment options. Clinics in podiatric medicine and surgery. 2010 Jan:27(1):79-92. doi: 10.1016/j.cpm.2009.08.004. Epub [PubMed PMID: 19963171]
Janisse DJ, Janisse E. Shoe modification and the use of orthoses in the treatment of foot and ankle pathology. The Journal of the American Academy of Orthopaedic Surgeons. 2008 Mar:16(3):152-8 [PubMed PMID: 18316713]
Krause FG, Wing KJ, Younger AS. Neuromuscular issues in cavovarus foot. Foot and ankle clinics. 2008 Jun:13(2):243-58, vi. doi: 10.1016/j.fcl.2008.02.003. Epub [PubMed PMID: 18457772]
Mubarak SJ, Van Valin SE. Osteotomies of the foot for cavus deformities in children. Journal of pediatric orthopedics. 2009 Apr-May:29(3):294-9. doi: 10.1097/BPO.0b013e31819aad20. Epub [PubMed PMID: 19305283]
Level 2 (mid-level) evidenceElias FN, Yuen TJ, Olson SL, Sangeorzan BJ, Ledoux WR. Correction of clawed hallux deformity: comparison of the Jones procedure and FHL transfer in a cadaver model. Foot & ankle international. 2007 Mar:28(3):369-76 [PubMed PMID: 17371661]
Wetmore RS, Drennan JC. Long-term results of triple arthrodesis in Charcot-Marie-Tooth disease. The Journal of bone and joint surgery. American volume. 1989 Mar:71(3):417-22 [PubMed PMID: 2925716]
Stricker SJ, Rosen E. Early one-stage reconstruction of congenital vertical talus. Foot & ankle international. 1997 Sep:18(9):535-43 [PubMed PMID: 9310763]
Duncan RD, Fixsen JA. Congenital convex pes valgus. The Journal of bone and joint surgery. British volume. 1999 Mar:81(2):250-4 [PubMed PMID: 10204930]
Kodros SA, Dias LS. Single-stage surgical correction of congenital vertical talus. Journal of pediatric orthopedics. 1999 Jan-Feb:19(1):42-8 [PubMed PMID: 9890285]
Level 2 (mid-level) evidenceKnörr J, Soldado F, Pham TT, Torres A, Cahuzac JP, de Gauzy JS. Percutaneous correction of persistent severe metatarsus adductus in children. Journal of pediatric orthopedics. 2014 Jun:34(4):447-52. doi: 10.1097/BPO.0000000000000122. Epub [PubMed PMID: 24276227]
Panski A, Goldman V, Simanovsky N, Lamdan M, Lamdan R. Universal neonatal foot orthotics-a novel treatment of infantile metatarsus adductus. European journal of pediatrics. 2021 Sep:180(9):2943-2949. doi: 10.1007/s00431-021-04048-5. Epub 2021 Apr 9 [PubMed PMID: 33835248]
Siegel SJ. The Modified Lepird Procedure for Correction of Metatarsus Adductus. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 2019 Sep:58(5):1045-1050. doi: 10.1053/j.jfas.2018.12.033. Epub 2019 Jul 23 [PubMed PMID: 31345764]
Leucht AK, Younger A, Veljkovic A, Perera A. The Windswept Foot: Dealing with Metatarsus Adductus and Toe Valgus. Foot and ankle clinics. 2020 Sep:25(3):413-424. doi: 10.1016/j.fcl.2020.05.005. Epub 2020 Jul 11 [PubMed PMID: 32736739]
Feng L, Sussman M. Combined Medial Cuneiform Osteotomy and Multiple Metatarsal Osteotomies For Correction of Persistent Metatarsus Adductus in Children. Journal of pediatric orthopedics. 2016 Oct-Nov:36(7):730-5. doi: 10.1097/BPO.0000000000000559. Epub [PubMed PMID: 26057072]
Matuszak SA, Baker EA, Fortin PT. The adult paralytic foot. The Journal of the American Academy of Orthopaedic Surgeons. 2013 May:21(5):276-85. doi: 10.5435/JAAOS-21-05-276. Epub [PubMed PMID: 23637146]
Faulks S, Brown K, Birch JG. Spectrum of Diagnosis and Disposition of Patients Referred to a Pediatric Orthopaedic Center for a Diagnosis of Intoeing. Journal of pediatric orthopedics. 2017 Oct/Nov:37(7):e432-e435. doi: 10.1097/BPO.0000000000001007. Epub [PubMed PMID: 28471818]
Kenmoku T, Kamegaya M, Saisu T, Ochiai N, Iwakura N, Iwase D, Takahashi K, Takaso M. Athletic ability of school-age children after satisfactory treatment of congenital clubfoot. Journal of pediatric orthopedics. 2013 Apr-May:33(3):321-5. doi: 10.1097/BPO.0b013e31827d0c88. Epub [PubMed PMID: 23482271]
Lohle-Akkersdijk JJ, Rameckers EA, Andriesse H, de Reus I, van Erve RH. Walking capacity of children with clubfeet in primary school: something to worry about? Journal of pediatric orthopedics. Part B. 2015 Jan:24(1):18-23. doi: 10.1097/BPB.0000000000000112. Epub [PubMed PMID: 25350905]
Level 2 (mid-level) evidenceSchwend RM, Drennan JC. Cavus foot deformity in children. The Journal of the American Academy of Orthopaedic Surgeons. 2003 May-Jun:11(3):201-11 [PubMed PMID: 12828450]
Morcuende JA, Dolan LA, Dietz FR, Ponseti IV. Radical reduction in the rate of extensive corrective surgery for clubfoot using the Ponseti method. Pediatrics. 2004 Feb:113(2):376-80 [PubMed PMID: 14754952]
Level 2 (mid-level) evidenceGöksan SB, Bilgili F, Eren İ, Bursalı A, Koç E. Factors affecting adherence with foot abduction orthosis following Ponseti method. Acta orthopaedica et traumatologica turcica. 2015:49(6):620-6. doi: 10.3944/AOTT.2015.14.0348. Epub [PubMed PMID: 26511688]
Ponseti IV, Smoley EN. The classic: congenital club foot: the results of treatment. 1963. Clinical orthopaedics and related research. 2009 May:467(5):1133-45. doi: 10.1007/s11999-009-0720-2. Epub 2009 Feb 14 [PubMed PMID: 19219519]
Ezra E, Hayek S, Gilai AN, Khermosh O, Wientroub S. Tibialis anterior tendon transfer for residual dynamic supination deformity in treated club feet. Journal of pediatric orthopedics. Part B. 2000 Jun:9(3):207-11 [PubMed PMID: 10904909]
Level 2 (mid-level) evidenceMerrill LJ, Gurnett CA, Connolly AM, Pestronk A, Dobbs MB. Skeletal muscle abnormalities and genetic factors related to vertical talus. Clinical orthopaedics and related research. 2011 Apr:469(4):1167-74. doi: 10.1007/s11999-010-1475-5. Epub 2010 Jul 20 [PubMed PMID: 20645034]
Level 2 (mid-level) evidenceBosman HA, Robinson AH. Treatment of ankle instability with an associated cavus deformity. Foot and ankle clinics. 2013 Dec:18(4):643-57. doi: 10.1016/j.fcl.2013.08.005. Epub 2013 Oct 6 [PubMed PMID: 24215830]
Ward CM, Dolan LA, Bennett DL, Morcuende JA, Cooper RR. Long-term results of reconstruction for treatment of a flexible cavovarus foot in Charcot-Marie-Tooth disease. The Journal of bone and joint surgery. American volume. 2008 Dec:90(12):2631-42. doi: 10.2106/JBJS.G.01356. Epub [PubMed PMID: 19047708]
Saltzman CL, Fehrle MJ, Cooper RR, Spencer EC, Ponseti IV. Triple arthrodesis: twenty-five and forty-four-year average follow-up of the same patients. The Journal of bone and joint surgery. American volume. 1999 Oct:81(10):1391-402 [PubMed PMID: 10535589]