Introduction
Oncocytic carcinoma, previously known as Hürthle cell carcinoma, is a rare type of thyroid cancer originating from oncocytic cells, a specialized type of follicular thyroid cell. These cells are identified by their eosinophilic cytoplasm and an abundance of granular cytoplasm. Until 2022, oncocytic carcinoma was considered a variant of follicular thyroid carcinoma, but it has since been reclassified as a separate subtype by the World Health Organization (WHO). Oncocytic thyroid carcinoma's distinct histopathological features and molecular differences, particularly mutations in the mitochondrial genome and gene expression profiles, set it apart from follicular thyroid carcinoma.[1]
Similar to other types of thyroid cancer, oncocytic carcinoma often occurs in middle-aged women as a thyroid nodule, which may not cause symptoms. Diagnosis is typically made through thyroid ultrasonography and fine-needle aspiration or core needle biopsy of the nodule. Staging oncocytic carcinoma through imaging studies may be necessary due to its increased tendency for metastatic disease. The treatment for localized oncocytic carcinoma is thyroidectomy. Unlike other types of thyroid cancer, oncocytic carcinoma has a lower tendency for radioactive iodine uptake, so this is often not a treatment option. However, newer treatments, such as tyrosine kinase inhibitors, may be considered.
Treatment options continue to evolve as our knowledge of molecular markers grows, and more targeted agents become available. Due to the rarity and unique characteristics of oncocytic thyroid carcinoma, an extensive understanding of its pathophysiology, epidemiology, and optimal management strategies is essential to improving patient outcomes and guiding effective therapeutic interventions.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Various genetic, environmental, and biological factors influence the development of oncocytic thyroid cancer. This type of cancer originates from specialized follicular thyroid cells called oncocytes, characterized by their abundant eosinophilic cytoplasm and high mitochondrial content. The pathogenesis of oncocytic cancer is associated with specific genetic mutations, particularly in mitochondrial DNA, and changes in nuclear genes. Mutations in oncogenes like BRAF and HRAS and inactivation of tumor suppressor genes (eg, PTEN) have been identified, indicating a disruption of normal cellular signaling pathways that control cell growth and survival.[2]
Environmental factors also play a significant role in the development of oncocytic thyroid carcinoma. Exposure to ionizing radiation, especially during childhood, has been established as a risk factor for various thyroid malignancies, including oncocytic carcinoma. Individuals with preexisting thyroid conditions, such as adenomas or goiter, may have an elevated risk of developing oncocytic cancer. Additionally, genetic syndromes, including multiple endocrine neoplasia type 1 (MEN 1) and familial nonmedullary thyroid cancer, have been associated with an increased incidence of oncocytic carcinoma.[3]
Epidemiology
The incidence and prevalence of oncocytic carcinoma are less extensively documented in comparison to more prevalent thyroid cancers such as papillary or follicular thyroid carcinoma. This is in part due to its recent identification as a distinct entity. Oncocytic thyroid cancer accounts for approximately 3% to 4% of all thyroid malignancies.[4]
Oncocytic carcinoma is more commonly diagnosed in women, with a ratio of approximately 1.6 to 4.8:1 compared to men, and typically affects middle-aged adults, particularly those aged between 50 and 60 years. Specific populations, particularly those in areas with endemic goiter or iodine deficiency, may exhibit higher rates of oncocytic carcinoma.[4]
Despite its lower incidence compared to other forms of thyroid cancer, the aggressive nature and tendency of oncocytic carcinoma to metastasize contribute to its clinical significance. The 5-year relative survival rates for oncocytic carcinoma can vary widely, influenced by factors including tumor stage, histological characteristics, and the presence of metastases at diagnosis. The overall 5-year relative survival rate is high, with a weighted average of all stages of the disease at 98.5%. Approximately 2100 thyroid cancer deaths occur per year in the United States.[5] Understanding the epidemiological patterns of oncocytic carcinoma is crucial for identifying at-risk populations and informing screening and management strategies.
Pathophysiology
The pathophysiology of oncocytic thyroid cancer entails a complex interplay of genetic, molecular, and cellular mechanisms contributing to its distinct behavior and clinical presentation. Oncocytic thyroid cancer originates from oncocytic cells, variants of follicular thyroid cells distinguished by abundant eosinophilic cytoplasm, high mitochondrial content, and atypical morphology. Consequently, oncocytic thyroid cancer is associated with significant genetic alterations.[2]
The cancer is linked to changes in the mitochondria, driven by mutations in mitochondrial DNA (mtDNA), including small mutations and larger deletions, leading to compromised energy production and subsequent compensatory mitochondrial proliferation within the cell.[6] Furthermore, oncocytic tumors exhibit specific alterations in nuclear DNA, although these are less prevalent compared to other thyroid tumors. For instance, mutations in oncogenes like HRAS and BRAF, commonly observed in other types of thyroid cancer, are rare in oncocytic tumors.[7]
Histopathologically, oncocytic carcinoma is distinguished by a high density of oncocytic cells, often accompanied by vascular invasion and a tendency for extra-thyroidal extension. Thyroid tumors are classified as oncocytic neoplasms when more than 75% of the tumor comprises oncocytic cells.[8] This aggressive behavior stems partly from the tumor's capacity to invade surrounding tissues and metastasize to distant sites such as the lungs and bones.[9] The vascularization of the tumor microenvironment is also crucial, as increased angiogenesis supports the tumor's growth and survival.
Histopathology
Oncocytic carcinoma is histologically characterized by at least 75% oncocytes, distinguished by their large size and well-defined cell borders.[2] The tumor cells display deeply eosinophilic and granular cytoplasm, large nuclei with prominent nucleoli, and a complete loss of cell polarity (see Image. Oncocytic Thyroid Carcinoma). Growth patterns may vary, presenting as follicular, trabecular, solid, or papillary formations. Occasional nuclear grooves or pseudo-inclusions can be observed. Additionally, psammomatous-like calcifications may be present in the lumen of follicles. However, unlike in papillary carcinoma, these calcifications lack the laminated structure typically seen in psammoma bodies within the stroma. Malignant oncocytic carcinoma typically exhibits a thicker capsule than adenomas, a solid or trabecular growth pattern, smaller cells with a high nuclear-to-cytoplasmic ratio, and increased mitotic figures. Poorly differentiated tumors are characterized by a size >4 cm, tumor necrosis, numerous mitoses, and foci of small tumor cells.[1]
History and Physical
Oncocytic thyroid cancers present similarly to other differentiated thyroid cancers. Patients often present with an asymptomatic thyroid nodule that is incidentally detected during imaging. Symptoms, when present, may include a palpable nodule that has grown over time, dysphagia, voice changes, or signs of recurrent laryngeal nerve injury such as hoarseness. Given the higher likelihood of distant metastases, particularly to the lungs and bones, clinicians should assess for bone pain and new respiratory symptoms.
A comprehensive physical examination should focus on the thyroid gland and cervical lymph nodes. Clinicians should inquire about any previous exposure to radiation, particularly to the head and neck, during childhood, as this is a known risk factor for thyroid malignancies. Family history, including multiple endocrine neoplasia (MEN) and other thyroid cancers, should be discussed, as this may predispose individuals to oncocytic carcinoma.
Evaluation
Patients presenting with thyroid nodules should have thyroid function tests performed at baseline, even though cancers are not hormonally active. A thyroid ultrasound is the initial imaging test of choice. Image-guided fine or core needle biopsies can identify oncocytic thyroid lesions, typically reported as Bethesda 4 lesions. However, needle biopsies cannot make this distinction because the demonstration of capsular and vascular invasion is the most reliable means of distinguishing between adenomas and invasive oncocytic carcinomas.
Molecular testing with commercially available genetic testing kits (eg, Afirma® or ThyroSeq® Genetic Classifier) may be helpful in further evaluating Bethesda 3 and 4 lesions. However, the data on their efficacy in oncocytic carcinoma are limited, and thus far, they have been associated with high false-positive rates (38% to 41%), which limits their utility.[10][11] Ultimately, most patients with oncocytic lesions undergo a diagnostic thyroid lobectomy. On final pathology, the diagnosis of oncocytic thyroid carcinoma can be made.
Patients with clinical features suspicious of high-risk or locally advanced disease, including ultrasound imaging indicating extrathyroidal extension or local invasion, clinical lymphadenopathy, or symptoms of local invasion, including hoarseness, dysphagia, or stridor, should undergo further evaluation. Cervical ultrasonography, computed tomography (CT), and magnetic resonance imaging (MRI) may be used to stage the disease. If distant metastatic disease is suspected, whole-body positron emission tomography (PET)/CT and bone scans are valuable modalities. Thyroid uptake studies are generally less helpful for oncocytic tumors, as they do not reliably absorb radioactive iodine.[12]
Treatment / Management
Surgical Treatment
The primary treatment for oncocytic thyroid cancer is thyroidectomy, with the specific approach contingent upon the tumor's size, location, and potential metastasis. Total thyroidectomy, involving the complete removal of the thyroid gland, is the most frequently performed procedure. This procedure is recommended for patients with tumors exceeding 4 cm, those displaying invasive characteristics, or in cases where lymph node metastasis is suspected.[4] Total thyroidectomy diminishes the risk of recurrence and enables the postoperative monitoring of thyroglobulin levels, a critical marker for oncocytic carcinoma recurrence.
Thyroid lobectomy is recommended in cases where the cytology suggests a Bethesda 3 or 4 lesion.[12] This procedure also serves a diagnostic purpose, and if the lobectomy specimen indicates oncocytic thyroid carcinoma, a completion thyroidectomy is advised. In certain instances where the tumor is small and confined to 1 lobe of the thyroid, a lobectomy (removal of 1 lobe) may be considered. Nevertheless, due to the aggressive nature of oncocytic carcinoma and the potential for multifocality, total thyroidectomy is often the preferred option.(A1)
Additionally, therapeutic neck dissection of the central and lateral compartments should be performed for clinically positive lymph nodes.[12] (A1)
Medical Treatment
After total thyroidectomy, patients require thyroid hormone replacement, usually with levothyroxine. Levothyroxine is dosed to suppress thyroid-stimulating hormone (TSH) production, potentially reducing the risk of residual cancer growth. The degree of TSH suppression is based on the risk of tumor recurrence.
Currently, guidelines regarding the postoperative use of radioactive iodine (RAI) are inconsistent. The largest study to date found no improvement in disease-specific or overall survival with the addition of RAI to surgery, even in patients at high risk for recurrence. Occasionally, patients have tumors that concentrate iodine. RAI may be applicable in these patients, and a sodium iodide I 123 or I 131 uptake study can help identify patients who are candidates for ablation.
For patients with metastatic oncocytic carcinoma who are asymptomatic and have well-differentiated tumors with slow-growing disease, observation is an acceptable option as long as they do not have brain metastases. However, for patients with symptoms or rapidly growing metastatic tumors that respond to iodine treatment, RAI is a preferable option. If the patient's tumor is not suitable for RAI, systemic therapy with tyrosine kinase inhibitors (eg, lenvatinib or sorafenib) is considered.[13][14] Lenvatinib is preferred over sorafenib due to its better adverse effect profile. However, because oncocytic cell tumors are rare, most of the data for using tyrosine kinase inhibitors in metastatic disease is extrapolated from other thyroid carcinomas.[12](A1)
The molecular analysis of these cancers can be beneficial. Larotrectinib or entrectinib can be used for cancers with neurotrophic tyrosine receptor kinase (NTRK) fusion, and pembrolizumab can be used for patients with a high tumor mutation burden, regardless of the cancer type.[15][16] Selpercatinib and pralsetinib are helpful for patients with non-small cell lung cancers and thyroid carcinomas with RET fusions and can be used as a first-line treatment for patients with this mutation.[17][18][19] Most patients with RET fusions have medullary thyroid carcinoma, but the findings can be applied to oncocytic thyroid carcinomas with RET fusions. While cytotoxic chemotherapy has been used in small studies, it has not been shown to benefit patients with oncocytic carcinoma significantly and is typically used as a last resort.[20]
Radiation Treatment
If surgical resection is not possible or contraindicated, particularly if the cancer has spread beyond the thyroid and threatens vital structures, then external beam radiation therapy or intensity-modulated radiation therapy can be considered.[21][22][23][2](B2)
Monitoring and Follow-Up
Regular follow-up care is crucial for patients treated for oncocytic carcinoma. This typically includes physical examinations, neck ultrasounds, and monitoring of serum thyroglobulin levels. Patients should be educated about the signs of recurrence, eg, new lumps in the neck or voice changes. The frequency and type of follow-up imaging and laboratory testing will depend on individual risk factors and the initial treatment approach.
Differential Diagnosis
Differential diagnoses that should be considered when evaluating oncocytic thyroid cancer include:
- Benign oncocytic adenoma
- Follicular thyroid cell carcinoma
- Papillary thyroid carcinoma
- Thyroid lymphoma
- Medullary thyroid carcinoma
- Parathyroid neoplasms
- Anaplastic thyroid carcinoma
- Thyroiditis
- Metastatic disease
- Goiter
Staging
Staging of oncocytic thyroid cancer utilizes the tumor, node, metastasis (TNM) system from the American Joint Committee on Cancer (AJCC), with specific criteria tailored for this subtype. T staging categorizes tumors based on size and local extension: T1 indicates tumors ≤2 cm, T2 for those >2 cm but ≤4 cm, T3 for tumors >4 cm or with extrathyroidal extension, and T4 for any tumor with significant invasion into adjacent structures. N staging assesses regional lymph node involvement, where N0 indicates no nodal involvement, N1a involves level VI (ie, pretracheal and paratracheal) nodes, and N1b includes lateral neck nodes. M staging denotes distant metastasis, with M0 indicating no distant spread and M1 for distant metastasis.
Age also influences the stage of oncocytic thyroid malignancies. Patients 55 or older are classified under a different prognostic category, often leading to a higher stage classification due to their increased risk of aggressive disease. Accurate staging is essential for guiding treatment decisions and predicting outcomes in oncocytic thyroid cancer.[12]
Prognosis
The prognosis of oncocytic carcinoma is influenced by various clinical, pathological, and socioeconomic factors, reflecting its relatively aggressive nature compared to other differentiated thyroid cancers. The 10-year survival rate for patients with oncocytic carcinoma can exceed 90%, especially when detected early and managed effectively.[24] However, prognosis declines significantly for those with advanced disease or unfavorable characteristics.
A key prognostic indicator is tumor size. Tumors larger than 4 cm (classified as T3 or T4) are associated with a higher risk of metastasis and recurrence. Additionally, extrathyroidal extension correlates with poorer outcomes, particularly when involving adjacent structures. Age is also a crucial prognostic factor. Patients diagnosed at age 55 or older face a higher risk of aggressive disease progression, often exacerbated by comorbidities and the effects of biological aging.
Lymph node involvement is another critical consideration. Patients with regional lymph node metastases (ie, N1a or N1b) have increased recurrence risks and lower survival rates. Additionally, vascular invasion—where cancer cells invade blood vessels—significantly predicts poor prognosis and higher rates of distant metastasis.[7] Long-term follow-up is essential due to the potential for late recurrence. The American Thyroid Association (ATA) risk stratification system is commonly used by clinicians postsurgery to predict disease recurrence and guide surveillance.[25][5]
Regular monitoring through ultrasound and serum thyroglobulin levels is vital for early detection of recurrence, which can improve management outcomes. While oncocytic carcinoma presents significant prognostic challenges, timely and personalized treatment approaches can improve outcomes.
Complications
Complications associated with oncocytic thyroid cancer can arise from both the disease and its treatment. A significant concern is local invasion, which may compress surrounding structures such as the trachea, esophagus, or recurrent laryngeal nerve. This compression can lead to symptoms, including difficulty swallowing, breathing problems, or hoarseness. Oncocytic carcinoma also tends to spread through the lymphatic system, resulting in swollen lymph nodes and potential surgical complications if lymph node dissection is necessary. Additionally, the disease can spread to distant sites, such as the lungs and bones, making management and prognosis more challenging.
While often necessary, surgical intervention carries a risk for complications, including bleeding, infection, and damage to adjacent tissues or nerves. Patients may also experience long-term issues related to thyroid hormone management postthyroidectomy, including hypothyroidism and the need for lifelong hormone replacement therapy. The potential for the cancer to come back adds a psychological burden, requiring ongoing monitoring and follow-up, which can contribute to anxiety and uncertainty. Therefore, a comprehensive approach to management is essential to address these multifaceted complications associated with oncocytic thyroid carcinoma.
Deterrence and Patient Education
Oncocytic carcinomas can be more aggressive than other differentiated types of thyroid carcinomas. The United States Preventive Services Task Force does not recommend routine screening methods for diagnosing thyroid neoplasms in the general asymptomatic population. However, patients with a family history of medullary thyroid carcinomas, multiple endocrine neoplasia, a personal history of thyroid cancer, familial adenomatous polyposis syndrome, or radiation exposure are at a higher risk of developing thyroid cancer. They should be educated about the importance of being vigilant for suspicious signs or symptoms. Timely evaluation of any such symptoms is critical to early diagnosis and treatment.
Enhancing Healthcare Team Outcomes
Providing patient-centered care for individuals with oncocytic cell carcinoma requires a highly collaborative, interprofessional approach involving physicians, advanced practitioners, nurses, pharmacists, and other health professionals. Each team member plays a critical role in enhancing care coordination, patient safety, and team performance. Clinicians, such as endocrinologists, oncologists, and surgeons, must develop specialized skills in diagnosing and evaluating this rare thyroid cancer, including proficiency in interpreting imaging studies and understanding its distinct histopathological features. Given the complexity of oncocytic carcinoma, referrals to surgical specialists or oncologists are often necessary, particularly for patients with aggressive disease or high-risk characteristics. Advanced practitioners and nurses also play key roles in patient education, follow-up care, and monitoring for complications or recurrence.
Ethical considerations and patient autonomy must guide all discussions about treatment options, ensuring that patients are fully informed about the risks and benefits of various approaches, including active surveillance or more aggressive interventions. Effective interprofessional communication is essential, with each team member clearly understanding their responsibilities in contributing specialized knowledge to optimize patient care. Pharmacists may be involved in managing medications and exploring new targeted therapies, while pathologists are critical in accurate diagnosis.
Care coordination ensures seamless transitions from initial diagnosis through treatment and ongoing follow-up. Regular interprofessional meetings allow for shared decision-making and improved communication, minimizing errors and delays and enhancing patient safety and outcomes. Through this collaborative, patient-centered approach, healthcare professionals can address the unique challenges of oncocytic thyroid carcinoma, improving overall care quality and ensuring the best possible patient outcomes.
Media
(Click Image to Enlarge)
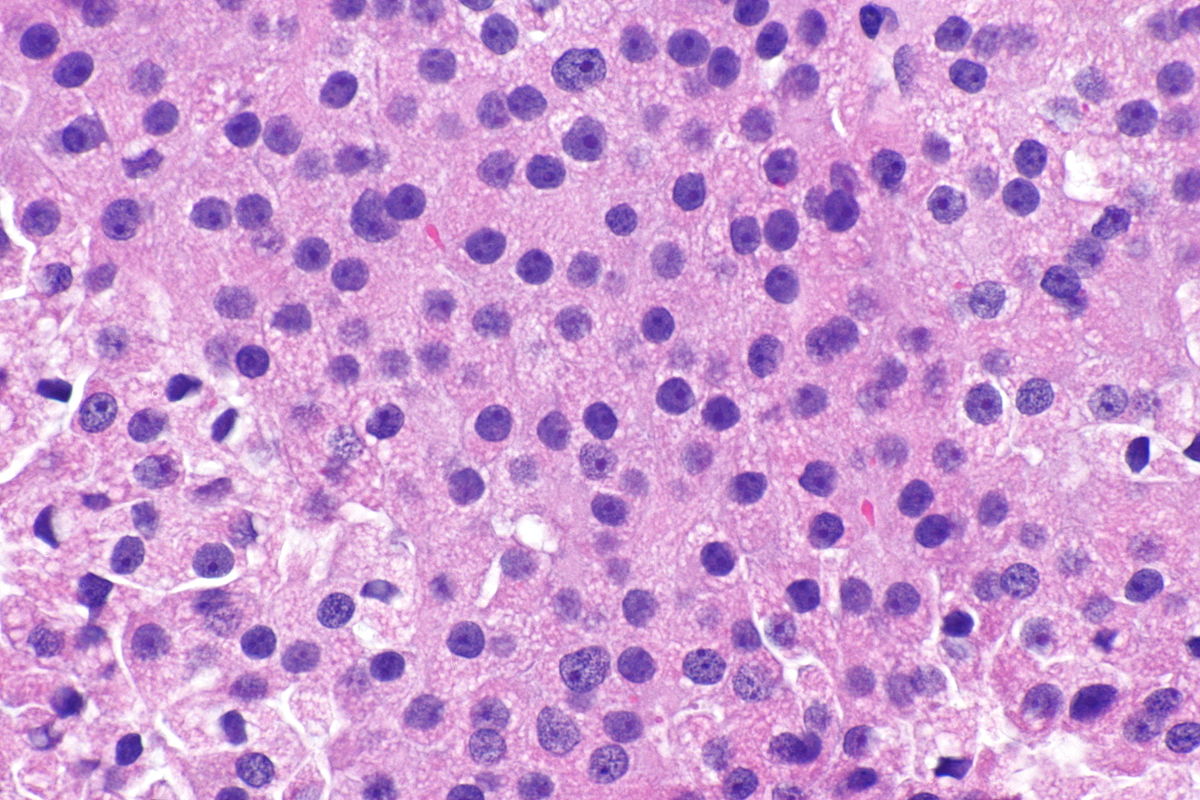
Thyroid Carcinoma. High Power Magnification demonstrates tumor cells with deeply eosinophilic and granular cytoplasm, large nuclei with prominent nucleoli, and a complete loss of cell polarity.
Librepath, Public Domain, via Wikimedia Commons
References
Jung CK, Bychkov A, Kakudo K. Update from the 2022 World Health Organization Classification of Thyroid Tumors: A Standardized Diagnostic Approach. Endocrinology and metabolism (Seoul, Korea). 2022 Oct:37(5):703-718. doi: 10.3803/EnM.2022.1553. Epub 2022 Oct 4 [PubMed PMID: 36193717]
McFadden DG, Sadow PM. Genetics, Diagnosis, and Management of Hürthle Cell Thyroid Neoplasms. Frontiers in endocrinology. 2021:12():696386. doi: 10.3389/fendo.2021.696386. Epub 2021 Jun 10 [PubMed PMID: 34177816]
Doerfler WR, Nikitski AV, Morariu EM, Ohori NP, Chiosea SI, Landau MS, Nikiforova MN, Nikiforov YE, Yip L, Manroa P. Molecular alterations in Hürthle cell nodules and preoperative cancer risk. Endocrine-related cancer. 2021 Apr 27:28(5):301-309. doi: 10.1530/ERC-20-0435. Epub 2021 Apr 27 [PubMed PMID: 33792557]
Kure S, Ohashi R. Thyroid Hürthle Cell Carcinoma: Clinical, Pathological, and Molecular Features. Cancers. 2020 Dec 23:13(1):. doi: 10.3390/cancers13010026. Epub 2020 Dec 23 [PubMed PMID: 33374707]
Boucai L, Zafereo M, Cabanillas ME. Thyroid Cancer: A Review. JAMA. 2024 Feb 6:331(5):425-435. doi: 10.1001/jama.2023.26348. Epub [PubMed PMID: 38319329]
Ganly I, Makarov V, Deraje S, Dong Y, Reznik E, Seshan V, Nanjangud G, Eng S, Bose P, Kuo F, Morris LGT, Landa I, Carrillo Albornoz PB, Riaz N, Nikiforov YE, Patel K, Umbricht C, Zeiger M, Kebebew E, Sherman E, Ghossein R, Fagin JA, Chan TA. Integrated Genomic Analysis of Hürthle Cell Cancer Reveals Oncogenic Drivers, Recurrent Mitochondrial Mutations, and Unique Chromosomal Landscapes. Cancer cell. 2018 Aug 13:34(2):256-270.e5. doi: 10.1016/j.ccell.2018.07.002. Epub [PubMed PMID: 30107176]
Wong KS, Angell TE, Barletta JA, Krane JF. Hürthle cell lesions of the thyroid: Progress made and challenges remaining. Cancer cytopathology. 2021 May:129(5):347-362. doi: 10.1002/cncy.22375. Epub 2020 Oct 27 [PubMed PMID: 33108684]
Fariduddin MM, Sherman S, Menon G, Syed W. Oncocytic (Hürthle Cell) Thyroid Carcinoma. StatPearls. 2024 Jan:(): [PubMed PMID: 33760495]
Sabra MM, Ghossein R, Tuttle RM. Time Course and Predictors of Structural Disease Progression in Pulmonary Metastases Arising from Follicular Cell-Derived Thyroid Cancer. Thyroid : official journal of the American Thyroid Association. 2016 Apr:26(4):518-24. doi: 10.1089/thy.2015.0395. Epub 2016 Feb 12 [PubMed PMID: 26872102]
Patel KN, Angell TE, Babiarz J, Barth NM, Blevins T, Duh QY, Ghossein RA, Harrell RM, Huang J, Kennedy GC, Kim SY, Kloos RT, LiVolsi VA, Randolph GW, Sadow PM, Shanik MH, Sosa JA, Traweek ST, Walsh PS, Whitney D, Yeh MW, Ladenson PW. Performance of a Genomic Sequencing Classifier for the Preoperative Diagnosis of Cytologically Indeterminate Thyroid Nodules. JAMA surgery. 2018 Sep 1:153(9):817-824. doi: 10.1001/jamasurg.2018.1153. Epub [PubMed PMID: 29799911]
Steward DL, Carty SE, Sippel RS, Yang SP, Sosa JA, Sipos JA, Figge JJ, Mandel S, Haugen BR, Burman KD, Baloch ZW, Lloyd RV, Seethala RR, Gooding WE, Chiosea SI, Gomes-Lima C, Ferris RL, Folek JM, Khawaja RA, Kundra P, Loh KS, Marshall CB, Mayson S, McCoy KL, Nga ME, Ngiam KY, Nikiforova MN, Poehls JL, Ringel MD, Yang H, Yip L, Nikiforov YE. Performance of a Multigene Genomic Classifier in Thyroid Nodules With Indeterminate Cytology: A Prospective Blinded Multicenter Study. JAMA oncology. 2019 Feb 1:5(2):204-212. doi: 10.1001/jamaoncol.2018.4616. Epub [PubMed PMID: 30419129]
Level 2 (mid-level) evidenceHaddad RI, Bischoff L, Ball D, Bernet V, Blomain E, Busaidy NL, Campbell M, Dickson P, Duh QY, Ehya H, Goldner WS, Guo T, Haymart M, Holt S, Hunt JP, Iagaru A, Kandeel F, Lamonica DM, Mandel S, Markovina S, McIver B, Raeburn CD, Rezaee R, Ridge JA, Roth MY, Scheri RP, Shah JP, Sipos JA, Sippel R, Sturgeon C, Wang TN, Wirth LJ, Wong RJ, Yeh M, Cassara CJ, Darlow S. Thyroid Carcinoma, Version 2.2022, NCCN Clinical Practice Guidelines in Oncology. Journal of the National Comprehensive Cancer Network : JNCCN. 2022 Aug:20(8):925-951. doi: 10.6004/jnccn.2022.0040. Epub [PubMed PMID: 35948029]
Level 1 (high-level) evidenceSchlumberger M, Tahara M, Wirth LJ, Robinson B, Brose MS, Elisei R, Habra MA, Newbold K, Shah MH, Hoff AO, Gianoukakis AG, Kiyota N, Taylor MH, Kim SB, Krzyzanowska MK, Dutcus CE, de las Heras B, Zhu J, Sherman SI. Lenvatinib versus placebo in radioiodine-refractory thyroid cancer. The New England journal of medicine. 2015 Feb 12:372(7):621-30. doi: 10.1056/NEJMoa1406470. Epub [PubMed PMID: 25671254]
Level 1 (high-level) evidenceBrose MS, Nutting CM, Jarzab B, Elisei R, Siena S, Bastholt L, de la Fouchardiere C, Pacini F, Paschke R, Shong YK, Sherman SI, Smit JW, Chung J, Kappeler C, Peña C, Molnár I, Schlumberger MJ, DECISION investigators. Sorafenib in radioactive iodine-refractory, locally advanced or metastatic differentiated thyroid cancer: a randomised, double-blind, phase 3 trial. Lancet (London, England). 2014 Jul 26:384(9940):319-28. doi: 10.1016/S0140-6736(14)60421-9. Epub 2014 Apr 24 [PubMed PMID: 24768112]
Level 1 (high-level) evidenceDrilon A, Laetsch TW, Kummar S, DuBois SG, Lassen UN, Demetri GD, Nathenson M, Doebele RC, Farago AF, Pappo AS, Turpin B, Dowlati A, Brose MS, Mascarenhas L, Federman N, Berlin J, El-Deiry WS, Baik C, Deeken J, Boni V, Nagasubramanian R, Taylor M, Rudzinski ER, Meric-Bernstam F, Sohal DPS, Ma PC, Raez LE, Hechtman JF, Benayed R, Ladanyi M, Tuch BB, Ebata K, Cruickshank S, Ku NC, Cox MC, Hawkins DS, Hong DS, Hyman DM. Efficacy of Larotrectinib in TRK Fusion-Positive Cancers in Adults and Children. The New England journal of medicine. 2018 Feb 22:378(8):731-739. doi: 10.1056/NEJMoa1714448. Epub [PubMed PMID: 29466156]
Drilon A, Siena S, Dziadziuszko R, Barlesi F, Krebs MG, Shaw AT, de Braud F, Rolfo C, Ahn MJ, Wolf J, Seto T, Cho BC, Patel MR, Chiu CH, John T, Goto K, Karapetis CS, Arkenau HT, Kim SW, Ohe Y, Li YC, Chae YK, Chung CH, Otterson GA, Murakami H, Lin CC, Tan DSW, Prenen H, Riehl T, Chow-Maneval E, Simmons B, Cui N, Johnson A, Eng S, Wilson TR, Doebele RC, trial investigators. Entrectinib in ROS1 fusion-positive non-small-cell lung cancer: integrated analysis of three phase 1-2 trials. The Lancet. Oncology. 2020 Feb:21(2):261-270. doi: 10.1016/S1470-2045(19)30690-4. Epub 2019 Dec 11 [PubMed PMID: 31838015]
Wirth LJ, Sherman E, Robinson B, Solomon B, Kang H, Lorch J, Worden F, Brose M, Patel J, Leboulleux S, Godbert Y, Barlesi F, Morris JC, Owonikoko TK, Tan DSW, Gautschi O, Weiss J, de la Fouchardière C, Burkard ME, Laskin J, Taylor MH, Kroiss M, Medioni J, Goldman JW, Bauer TM, Levy B, Zhu VW, Lakhani N, Moreno V, Ebata K, Nguyen M, Heirich D, Zhu EY, Huang X, Yang L, Kherani J, Rothenberg SM, Drilon A, Subbiah V, Shah MH, Cabanillas ME. Efficacy of Selpercatinib in RET-Altered Thyroid Cancers. The New England journal of medicine. 2020 Aug 27:383(9):825-835. doi: 10.1056/NEJMoa2005651. Epub [PubMed PMID: 32846061]
Li AY, McCusker MG, Russo A, Scilla KA, Gittens A, Arensmeyer K, Mehra R, Adamo V, Rolfo C. RET fusions in solid tumors. Cancer treatment reviews. 2019 Dec:81():101911. doi: 10.1016/j.ctrv.2019.101911. Epub 2019 Oct 30 [PubMed PMID: 31715421]
Drilon A, Oxnard GR, Tan DSW, Loong HHF, Johnson M, Gainor J, McCoach CE, Gautschi O, Besse B, Cho BC, Peled N, Weiss J, Kim YJ, Ohe Y, Nishio M, Park K, Patel J, Seto T, Sakamoto T, Rosen E, Shah MH, Barlesi F, Cassier PA, Bazhenova L, De Braud F, Garralda E, Velcheti V, Satouchi M, Ohashi K, Pennell NA, Reckamp KL, Dy GK, Wolf J, Solomon B, Falchook G, Ebata K, Nguyen M, Nair B, Zhu EY, Yang L, Huang X, Olek E, Rothenberg SM, Goto K, Subbiah V. Efficacy of Selpercatinib in RET Fusion-Positive Non-Small-Cell Lung Cancer. The New England journal of medicine. 2020 Aug 27:383(9):813-824. doi: 10.1056/NEJMoa2005653. Epub [PubMed PMID: 32846060]
Marabelle A, Le DT, Ascierto PA, Di Giacomo AM, De Jesus-Acosta A, Delord JP, Geva R, Gottfried M, Penel N, Hansen AR, Piha-Paul SA, Doi T, Gao B, Chung HC, Lopez-Martin J, Bang YJ, Frommer RS, Shah M, Ghori R, Joe AK, Pruitt SK, Diaz LA Jr. Efficacy of Pembrolizumab in Patients With Noncolorectal High Microsatellite Instability/Mismatch Repair-Deficient Cancer: Results From the Phase II KEYNOTE-158 Study. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2020 Jan 1:38(1):1-10. doi: 10.1200/JCO.19.02105. Epub 2019 Nov 4 [PubMed PMID: 31682550]
Tuttle RM, Rondeau G, Lee NY. A risk-adapted approach to the use of radioactive iodine and external beam radiation in the treatment of well-differentiated thyroid cancer. Cancer control : journal of the Moffitt Cancer Center. 2011 Apr:18(2):89-95 [PubMed PMID: 21451451]
Romesser PB, Sherman EJ, Shaha AR, Lian M, Wong RJ, Sabra M, Rao SS, Fagin JA, Tuttle RM, Lee NY. External beam radiotherapy with or without concurrent chemotherapy in advanced or recurrent non-anaplastic non-medullary thyroid cancer. Journal of surgical oncology. 2014 Sep:110(4):375-82. doi: 10.1002/jso.23656. Epub 2014 Jun 24 [PubMed PMID: 24961938]
Servagi Vernat S, Khalifa J, Sun XS, Kammerer E, Blais E, Faivre JC, Sio TT, Pan J, Qiu H, Bar-Sela G, Simon JM, Salleron J, Thariat J. 10-Year Locoregional Control with Postoperative External Beam Radiotherapy in Patients with Locally Advanced High-Risk Non-Anaplastic Thyroid Carcinoma De Novo or at Relapse, a Propensity Score Analysis. Cancers. 2019 Jun 19:11(6):. doi: 10.3390/cancers11060849. Epub 2019 Jun 19 [PubMed PMID: 31248183]
Level 2 (mid-level) evidenceHumphreys BM, Memeh KO, Funkhouser A, Vaghaiwalla TM. Prognostic factors and survival analysis of Hurthle cell carcinoma: A population-based study. Surgery. 2022 Nov:172(5):1379-1384. doi: 10.1016/j.surg.2022.07.007. Epub 2022 Aug 26 [PubMed PMID: 36038373]
Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, Pacini F, Randolph GW, Sawka AM, Schlumberger M, Schuff KG, Sherman SI, Sosa JA, Steward DL, Tuttle RM, Wartofsky L. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid : official journal of the American Thyroid Association. 2016 Jan:26(1):1-133. doi: 10.1089/thy.2015.0020. Epub [PubMed PMID: 26462967]
