[1]
Koh JL, Stewart C. Patellar instability. The Orthopedic clinics of North America. 2015 Jan:46(1):147-57. doi: 10.1016/j.ocl.2014.09.011. Epub
[PubMed PMID: 25435044]
[2]
Hawkins RJ, Bell RH, Anisette G. Acute patellar dislocations. The natural history. The American journal of sports medicine. 1986 Mar-Apr:14(2):117-20
[PubMed PMID: 3717480]
[3]
Atkin DM, Fithian DC, Marangi KS, Stone ML, Dobson BE, Mendelsohn C. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. The American journal of sports medicine. 2000 Jul-Aug:28(4):472-9
[PubMed PMID: 10921637]
[4]
Arnbjörnsson A, Egund N, Rydling O, Stockerup R, Ryd L. The natural history of recurrent dislocation of the patella. Long-term results of conservative and operative treatment. The Journal of bone and joint surgery. British volume. 1992 Jan:74(1):140-2
[PubMed PMID: 1732244]
[5]
Fithian DC, Paxton EW, Stone ML, Silva P, Davis DK, Elias DA, White LM. Epidemiology and natural history of acute patellar dislocation. The American journal of sports medicine. 2004 Jul-Aug:32(5):1114-21
[PubMed PMID: 15262631]
[6]
Hsiao M, Owens BD, Burks R, Sturdivant RX, Cameron KL. Incidence of acute traumatic patellar dislocation among active-duty United States military service members. The American journal of sports medicine. 2010 Oct:38(10):1997-2004. doi: 10.1177/0363546510371423. Epub 2010 Jul 8
[PubMed PMID: 20616375]
[7]
Sillanpää PJ, Peltola E, Mattila VM, Kiuru M, Visuri T, Pihlajamäki H. Femoral avulsion of the medial patellofemoral ligament after primary traumatic patellar dislocation predicts subsequent instability in men: a mean 7-year nonoperative follow-up study. The American journal of sports medicine. 2009 Aug:37(8):1513-21. doi: 10.1177/0363546509333010. Epub 2009 Apr 17
[PubMed PMID: 19376939]
[8]
Parikh SN, Lykissas MG. Classification of Lateral Patellar Instability in Children and Adolescents. The Orthopedic clinics of North America. 2016 Jan:47(1):145-52. doi: 10.1016/j.ocl.2015.08.016. Epub
[PubMed PMID: 26614929]
[9]
Redler LH, Wright ML. Surgical Management of Patellofemoral Instability in the Skeletally Immature Patient. The Journal of the American Academy of Orthopaedic Surgeons. 2018 Oct 1:26(19):e405-e415. doi: 10.5435/JAAOS-D-17-00255. Epub
[PubMed PMID: 30134308]
[10]
Colvin AC, West RV. Patellar instability. The Journal of bone and joint surgery. American volume. 2008 Dec:90(12):2751-62. doi: 10.2106/JBJS.H.00211. Epub
[PubMed PMID: 19047722]
[11]
Rhee SJ, Pavlou G, Oakley J, Barlow D, Haddad F. Modern management of patellar instability. International orthopaedics. 2012 Dec:36(12):2447-56. doi: 10.1007/s00264-012-1669-4. Epub 2012 Oct 7
[PubMed PMID: 23052278]
Level 3 (low-level) evidence
[12]
Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 1994:2(1):19-26
[PubMed PMID: 7584171]
[13]
Putney SA, Smith CS, Neal KM. The location of medial patellofemoral ligament injury in adolescents and children. Journal of pediatric orthopedics. 2012 Apr-May:32(3):241-4. doi: 10.1097/BPO.0b013e3182471d72. Epub
[PubMed PMID: 22411327]
[14]
Mäenpää H, Lehto MU. Patellar dislocation. The long-term results of nonoperative management in 100 patients. The American journal of sports medicine. 1997 Mar-Apr:25(2):213-7
[PubMed PMID: 9079176]
[15]
McConnell J. Rehabilitation and nonoperative treatment of patellar instability. Sports medicine and arthroscopy review. 2007 Jun:15(2):95-104
[PubMed PMID: 17505325]
[16]
He W, Yang YM, Liu M, Wang AY, Liu YJ. Reconstruction of the medial patellofemoral ligament using hamstring tendon graft with different methods: a biomechanical study. Chinese medical sciences journal = Chung-kuo i hsueh k'o hsueh tsa chih. 2013 Dec:28(4):201-5
[PubMed PMID: 24382220]
[17]
Donell ST, Joseph G, Hing CB, Marshall TJ. Modified Dejour trochleoplasty for severe dysplasia: operative technique and early clinical results. The Knee. 2006 Aug:13(4):266-73
[PubMed PMID: 16635572]
[18]
Schöttle PB, Fucentese SF, Pfirrmann C, Bereiter H, Romero J. Trochleaplasty for patellar instability due to trochlear dysplasia: A minimum 2-year clinical and radiological follow-up of 19 knees. Acta orthopaedica. 2005 Oct:76(5):693-8
[PubMed PMID: 16263617]
[19]
Fulkerson JP, Becker GJ, Meaney JA, Miranda M, Folcik MA. Anteromedial tibial tubercle transfer without bone graft. The American journal of sports medicine. 1990 Sep-Oct:18(5):490-6; discussion 496-7
[PubMed PMID: 2252090]
Level 3 (low-level) evidence
[20]
Kuroda R, Kambic H, Valdevit A, Andrish JT. Articular cartilage contact pressure after tibial tuberosity transfer. A cadaveric study. The American journal of sports medicine. 2001 Jul-Aug:29(4):403-9
[PubMed PMID: 11476376]
[21]
Goyal D. Medial patellofemoral ligament reconstruction: the superficial quad technique. The American journal of sports medicine. 2013 May:41(5):1022-9. doi: 10.1177/0363546513477828. Epub 2013 Mar 4
[PubMed PMID: 23460327]
[22]
Amis AA, Oguz C, Bull AM, Senavongse W, Dejour D. The effect of trochleoplasty on patellar stability and kinematics: a biomechanical study in vitro. The Journal of bone and joint surgery. British volume. 2008 Jul:90(7):864-9. doi: 10.1302/0301-620X.90B7.20447. Epub
[PubMed PMID: 18591593]
[23]
Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. The American journal of sports medicine. 1998 Jan-Feb:26(1):59-65
[PubMed PMID: 9474403]
[24]
Chahla J, Smigielski R, LaPrade RF, Fulkerson JP. An Updated Overview of the Anatomy and Function of the Proximal Medial Patellar Restraints (Medial Patellofemoral Ligament and the Medial Quadriceps Tendon Femoral Ligament). Sports medicine and arthroscopy review. 2019 Dec:27(4):136-142. doi: 10.1097/JSA.0000000000000252. Epub
[PubMed PMID: 31688531]
[25]
Baldwin JL. The anatomy of the medial patellofemoral ligament. The American journal of sports medicine. 2009 Dec:37(12):2355-61. doi: 10.1177/0363546509339909. Epub 2009 Sep 2
[PubMed PMID: 19729366]
[26]
LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L. The anatomy of the medial part of the knee. The Journal of bone and joint surgery. American volume. 2007 Sep:89(9):2000-10
[PubMed PMID: 17768198]
[27]
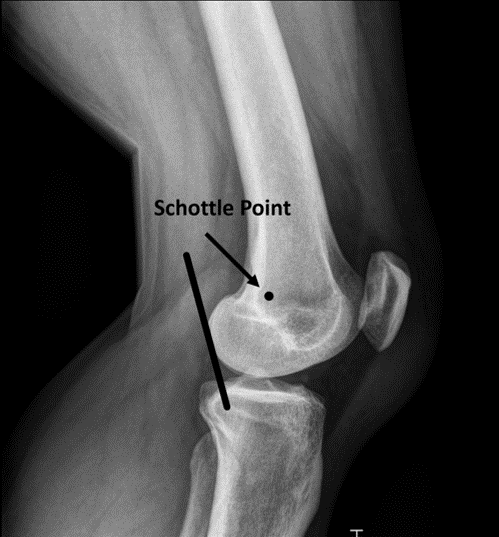
Schöttle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. The American journal of sports medicine. 2007 May:35(5):801-4
[PubMed PMID: 17267773]
[28]
Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP. Anatomy and biomechanics of the medial patellofemoral ligament. The Knee. 2003 Sep:10(3):215-20
[PubMed PMID: 12893142]
[29]
Geenen E, Molenaers G, Martens M. Patella alta in patellofemoral instability. Acta orthopaedica Belgica. 1989:55(3):387-93
[PubMed PMID: 2603680]
[30]
Wilson PL, Black SR, Ellis HB, Podeszwa DA. Distal Femoral Valgus and Recurrent Traumatic Patellar Instability: Is an Isolated Varus Producing Distal Femoral Osteotomy a Treatment Option? Journal of pediatric orthopedics. 2018 Mar:38(3):e162-e167. doi: 10.1097/BPO.0000000000001128. Epub
[PubMed PMID: 29324527]
[31]
Lee TQ, Anzel SH, Bennett KA, Pang D, Kim WC. The influence of fixed rotational deformities of the femur on the patellofemoral contact pressures in human cadaver knees. Clinical orthopaedics and related research. 1994 May:(302):69-74
[PubMed PMID: 8168325]
[32]
Weber AE, Nathani A, Dines JS, Allen AA, Shubin-Stein BE, Arendt EA, Bedi A. An Algorithmic Approach to the Management of Recurrent Lateral Patellar Dislocation. The Journal of bone and joint surgery. American volume. 2016 Mar 2:98(5):417-27. doi: 10.2106/JBJS.O.00354. Epub
[PubMed PMID: 26935465]
[33]
Staheli LT. Torsion--treatment indications. Clinical orthopaedics and related research. 1989 Oct:(247):61-6
[PubMed PMID: 2676305]
[34]
Rattey T, Hyndman J. Rotational osteotomies of the leg: tibia alone versus both tibia and fibula. Journal of pediatric orthopedics. 1994 Sep-Oct:14(5):615-8
[PubMed PMID: 7962504]
[35]
Hughston JC. Subluxation of the patella. The Journal of bone and joint surgery. American volume. 1968 Jul:50(5):1003-26
[PubMed PMID: 5676827]
[37]
Vermeulen D, van der Valk MR, Kaas L. Plaster, splint, brace, tape or functional mobilization after first-time patellar dislocation: what's the evidence? EFORT open reviews. 2019 Mar:4(3):110-114. doi: 10.1302/2058-5241.4.180016. Epub 2019 Mar 27
[PubMed PMID: 30993012]
[38]
Purohit N, Hancock N, Saifuddin A. Surgical management of patellofemoral instability. I. Imaging considerations. Skeletal radiology. 2019 Jun:48(6):859-869. doi: 10.1007/s00256-018-3123-1. Epub 2018 Dec 12
[PubMed PMID: 30542758]
[39]
Arendt EA, Askenberger M, Agel J, Tompkins MA. Risk of Redislocation After Primary Patellar Dislocation: A Clinical Prediction Model Based on Magnetic Resonance Imaging Variables. The American journal of sports medicine. 2018 Dec:46(14):3385-3390. doi: 10.1177/0363546518803936. Epub 2018 Nov 6
[PubMed PMID: 30398902]