Continuing Education Activity
Nummular headache is a chronic primary headache disorder recognized by the international headache society. Although it is a benign disorder, in some instances it can be very resistant to treatment and can cause significant morbidity. The purpose of this activity is to highlight the common presenting features, possible differential diagnosis and the role of interprofessional teams in identifying and managing this disorder.
Objectives:
- Describe the etiology and epidemiology of nummular headache.
- Review the pathophysiology of nummular headache.
- Outline the differential diagnosis and international classification of headache disorders and discuss various treatment modalities.
- Summarize the role of interprofessional collaboration for neurology, neurosurgery, hematology, pain medicine and other interprofessional teams for timely identification and management of these patients.
Introduction
The International Classification of Headache Disorders has broadly classified headache disorders into primary and secondary based on their origin. Primary headache disorders include migraine, trigeminal autonomic cephalgia, tension-type headache, and other primary headache disorders. Nummular headache categorizes under other primary headache disorders. It may be continuous or with intermittent exacerbations. The involved area is sharply contoured, fixed in size and shape, round or elliptical and about 1 to 6 cm in diameter, which has led to the name “coin-shaped headache.” Unlike migraine headache, nummular headache is not accompanied by nausea, vomiting, rhinorrhea, lacrimation, conjunctival injection, light or sound sensitivity or focal neurologic symptoms.[1][2]
Etiology
Secondary headache disorders occur secondary to a structural or metabolic abnormality such as tumor, abscess, meningitis, sinusitis and, temporomandibular joint dysfunction. The absence of an underlying etiology is mandatory for the diagnosis of nummular headache. However, nummular headache is a primary headache disorder without an identifiable underlying etiology.[1]
Epidemiology
Epidemiologically, a nummular headache is considered very rare. It was first described in 2002, and since then a few hundred cases have been described in the literature. According to one center estimate, there were 0.25% consultations made for a nummular headache out of all the headache consultations. The female to male prevalence ratio for this disorder is 1.5 to 1.
Pathophysiology
Clinical and experimental data have shown that nummular headache originates peripherally. Hence, stimulation of scalp structures reproduces this pain. Decreased pressure pain threshold areas (PPT’s) remain confined to the symptomatic area in these patients, and topographic pressure pain sensitivity maps are similar to healthy subjects except for decreased PPT’s in the areas involved.
Transdiploic and intradiploic nerves are thought to be involved in the pathophysiology of nummular headaches. These nerves connect the structures of the scalp to dura mater. Recent evidence suggests that a lesion or dysfunction of these nerves produces a sharply circumscribed area of pain similar to a nummular headache. Although there are hypotheses regarding the involvement of pericranial nerves, the lack of response to peripheral nerve blocks and the occasional presence of a sagittal PPT’s divided by the midline negate this hypothesis.
Finally, nummular headache is not associated with any psychiatric disorders, anxiety, and depression. Migraine and tension headaches may be concurrently present with a nummular headache but are not related. This evidence proves once again that the central origin of nummular headache is unlikely. Because of the above evidence, nummular headaches have a provisional classification as epicrania. Epicrania include headaches that arise from epicranial tissue such as internal and external layers of the skull, all the layers of the scalp including epicranial nerves and arteries.[1]
History and Physical
International headache society proposes the following diagnostic criteria:
- Mild to moderate head pain fulfilling the criteria B and C
- Pain is felt only in a rounded and elliptical area of 1-6 cm in diameter.
- Pain is chronic and either continuous or interrupted by spontaneous remissions lasting weeks and months.
- Not attributable to another disorder.
Two updates proposed in 2012 include[1][2]:
- Pain lasting minutes, hours or days with a remitting or unremitting course
- The symptomatic area does not change in size and shape over time.
Evaluation
An initial diagnostic workup includes a complete neurologic examination of the scalp, pericranial muscles, nerves and arteries. Laboratory tests may include a complete blood count, basic metabolic panel, liver function tests, thyroid function tests, erythrocyte sedimentation rate, alkaline phosphatase, antinuclear antibody, and rheumatoid factor. If there is clinical suspicion, CT and MRI scans can be considerations to check for underlying central nervous system pathology.[3]
A high prevalence of autoimmune disorders has been reported in patients with nummular headache(69%). Most commonly antinuclear antibodies(ANA) were detected in the blood of these patients. In this study, sjogren's syndrome was most commonly identified but most patients had no signs and symtoms of Autoimmune disease at the time of presentation. [4]
Treatment / Management
Nerve block, radiofrequency ablation, and decompression surgery have all been used successfully for the treatment of epicrania, but they seldom work for nummular headaches. For mild to moderate pain, NSAIDs and analgesics may be all that is needed. However, in resistant cases, preventative therapy with chemical neuromodulators such as gabapentin, pregabalin and tricyclic antidepressants TCAs have been successfully used. Peripheral nerve stimulation for intractable supraorbital pain has been used as well with favorable outcomes.[5] Transcutaneous nerve stimulation has been used successfully as well.[6][7]
Therapy with botulinum toxin deserves a special mention. For refractory cases of nummular headache, two case series, and several case reports showed that 10 to 25 units of botulinum toxin A injected in the affected and surrounding area resulted in substantial relief of symptoms. Its onset of action is 6 to 10 days, and the effect lasts up to 14 weeks at which point the procedure is repeated.[8]
Differential Diagnosis
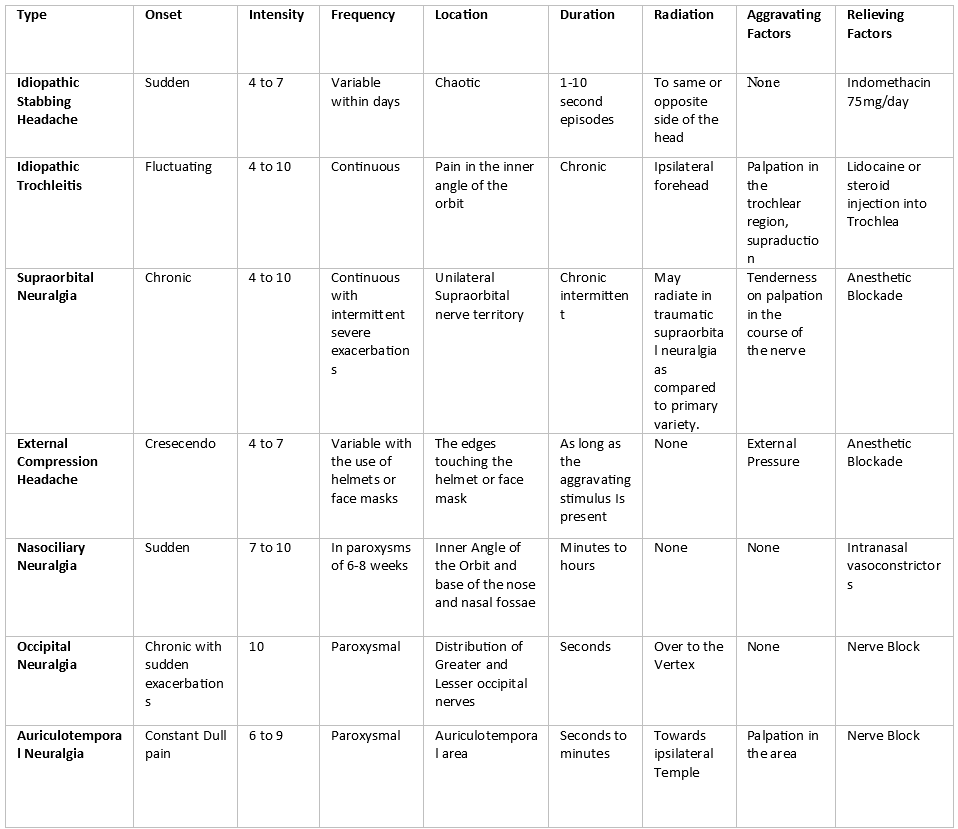
Broadly, nummular headache classifies under epicrania. The differential diagnosis includes migraine headaches and tension-type headache as well. Concurrent presence of other headaches disorders is not uncommon as well, making nummular headache a diagnosis of exclusion. Following differential diagnosis are a broad list of headache disorders as put forth in The International Classification of Headache Disorders 3rd edition issued by International headache society. Disorders in italics are considered epicrania.
Primary headache disorders:
Migraine headache
Tension-type headache
Trigeminal autonomic cephalalgias
Other primary headache disorder
- Primary cough headache
- Primary exercise headache
- Primary headache associated with sexual activity
- Primary thunderclap headache
- Cold-stimulus headache
- Hypnic headache
- New daily persistent headache (NDPH)
- Nummular headache
- Primary stabbing headache
- Idiopathic trochleitis
- Supraorbital neuralgia
- External compression headache
- Nasociliary neuralgia
- Occipital neuralgia
- Auriculotemporal neuralgia
Secondary Headache disorders:
Trauma and Injury headache
Vascular headache
Headache secondary to intracranial disorders
Chemical or substance abuse-related headache
Headache related to infectious causes in the head and neck regions
Headache related to disorders of homeostasis
- Headache related to hypoxia and hypercapnia
- High altitude
- Airplane travel
- Diving
- Sleep apnea
- Dialysis headache
- Hypertension headache
- Autonomic dysreflexia
- Preeclampsia and eclampsia
- Pheochromocytoma
- Hypertensive crisis and encephalopathy
- Fasting headache
- Cardiac cephalgia
- Hypothyroidism headache
- Other disorders of homeostasis
Prognosis
So far it is assumed that it is a benign disorder with a chronic course.
Complications
Nummular headache is a relatively new diagnosis, and there is limited evidence of any complications that may arise in longstanding cases. However, treatment with neuromodulators can cause excessive drowsiness; hence patients should be cautioned about operating heavy machinery and driving.
Consultations
Since nummular headache is a diagnosis of exclusion, investigations are carried out to rule out any brain and spinal cord pathology. Depending on the diagnosis, consultations with respective services including neurosurgery, orthopedic surgery, are in order.
Deterrence and Patient Education
The patient should receive education about the benign nature of this headache. However, they should be strongly encouraged to seek help if any focal neurologic signs appear, such as blurry or loss of vision, focal weakness, numbness, facial droop, slurring speech and loss of consciousness.
Enhancing Healthcare Team Outcomes
Although nummular headache is a primary headache disorder, the possibility of a secondary cause mimicking the symptoms require rigorous exclusion through neurologic exams, laboratory tests, and neuroimaging. The nurse practitioner, primary care provider, emergency department physician, neurologist, and an internist should inform the patient about the benign nature of this disorder. However, any focal neurologic symptoms, new-onset headache, persistent or morning headaches apart from the nummular headache, should prompt a physician consultation.[9]
Nummular headaches, along with all headaches disorders, are best addressed in a collaborative, interprofessional team approach regarding both diagnosis and treatment. This healthcare team includes physicians and specialists, neuroscience specialty trained nursing staff, and pharmacists, working collaboratively to bring about optimal patient care and results. Often the pharmacist will need to assist in medication management and assist in educating the patient regarding compliance. A coordinated interprofessional approach will result in the best outcomes. [Level V]