[1]
Leclaire R, Fortin L, Lambert R, Bergeron YM, Rossignol M. Radiofrequency facet joint denervation in the treatment of low back pain: a placebo-controlled clinical trial to assess efficacy. Spine. 2001 Jul 1:26(13):1411-6; discussion 1417
[PubMed PMID: 11458140]
Level 1 (high-level) evidence
[2]
Cohen SP, Hurley RW, Buckenmaier CC 3rd, Kurihara C, Morlando B, Dragovich A. Randomized placebo-controlled study evaluating lateral branch radiofrequency denervation for sacroiliac joint pain. Anesthesiology. 2008 Aug:109(2):279-88. doi: 10.1097/ALN.0b013e31817f4c7c. Epub
[PubMed PMID: 18648237]
Level 1 (high-level) evidence
[3]
van Wijk RM, Geurts JW, Wynne HJ, Hammink E, Buskens E, Lousberg R, Knape JT, Groen GJ. Radiofrequency denervation of lumbar facet joints in the treatment of chronic low back pain: a randomized, double-blind, sham lesion-controlled trial. The Clinical journal of pain. 2005 Jul-Aug:21(4):335-44
[PubMed PMID: 15951652]
Level 1 (high-level) evidence
[4]
Maas ET, Ostelo RW, Niemisto L, Jousimaa J, Hurri H, Malmivaara A, van Tulder MW. Radiofrequency denervation for chronic low back pain. The Cochrane database of systematic reviews. 2015 Oct 23:2015(10):CD008572. doi: 10.1002/14651858.CD008572.pub2. Epub 2015 Oct 23
[PubMed PMID: 26495910]
Level 3 (low-level) evidence
[5]
Manchikanti L, Kaye AD, Soin A, Albers SL, Beall D, Latchaw R, Sanapati MR, Shah S, Atluri S, Abd-Elsayed A, Abdi S, Aydin S, Bakshi S, Boswell MV, Buenaventura R, Cabaret J, Calodney AK, Candido KD, Christo PJ, Cintron L, Diwan S, Gharibo C, Grider J, Gupta M, Haney B, Harned ME, Helm Ii S, Jameson J, Jha S, Kaye AM, Knezevic NN, Kosanovic R, Manchikanti MV, Navani A, Racz G, Pampati V, Pasupuleti R, Philip C, Rajput K, Sehgal N, Sudarshan G, Vanaparthy R, Wargo BW, Hirsch JA. Comprehensive Evidence-Based Guidelines for Facet Joint Interventions in the Management of Chronic Spinal Pain: American Society of Interventional Pain Physicians (ASIPP) Guidelines Facet Joint Interventions 2020 Guidelines. Pain physician. 2020 May:23(3S):S1-S127
[PubMed PMID: 32503359]
Level 1 (high-level) evidence
[6]
Oh WS, Shim JC. A randomized controlled trial of radiofrequency denervation of the ramus communicans nerve for chronic discogenic low back pain. The Clinical journal of pain. 2004 Jan-Feb:20(1):55-60
[PubMed PMID: 14668658]
[7]
Choi EJ, Choi YM, Jang EJ, Kim JY, Kim TK, Kim KH. Neural Ablation and Regeneration in Pain Practice. The Korean journal of pain. 2016 Jan:29(1):3-11. doi: 10.3344/kjp.2016.29.1.3. Epub 2016 Jan 4
[PubMed PMID: 26839664]
[8]
Hao D, Yong RJ, Cohen SP, Stojanovic MP. Medial Branch Blocks and Radiofrequency Ablation for Low Back Pain from Facet Joints. The New England journal of medicine. 2023 Dec 21:389(25):e53. doi: 10.1056/NEJMvcm2211108. Epub
[PubMed PMID: 38118025]
[10]
Sowder T, Sayed D, Concannon T, Pew SH, Strand NH, Abd-Elsayed A, Wie CS, Gomez Ramos DE, Raslan AM, Deer TR. The American Society of Pain and Neuroscience (ASPN) Guidelines for Radiofrequency Ablative Procedures in Patients with Implanted Devices. Journal of pain research. 2023:16():3693-3706. doi: 10.2147/JPR.S419594. Epub 2023 Nov 3
[PubMed PMID: 37942223]
[11]
Chen B, Yang Y, Wang H, Guo X, Wu Z, Lan Z. Is radiofrequency ablation effective in treating patients with chronic knee osteoarthritis? A meta-analysis of randomized controlled trials. Annals of medicine and surgery (2012). 2024 Jan:86(1):412-420. doi: 10.1097/MS9.0000000000001509. Epub 2023 Nov 17
[PubMed PMID: 38222705]
Level 1 (high-level) evidence
[12]
Zakrzewska JM, Akram H. Neurosurgical interventions for the treatment of classical trigeminal neuralgia. The Cochrane database of systematic reviews. 2011 Sep 7:2011(9):CD007312. doi: 10.1002/14651858.CD007312.pub2. Epub 2011 Sep 7
[PubMed PMID: 21901707]
Level 1 (high-level) evidence
[13]
Saedi N, Hamilton HK, Arndt KA, Dover JS. How to prepare patients for ablative laser procedures. Journal of the American Academy of Dermatology. 2013 Aug:69(2):e49. doi: 10.1016/j.jaad.2013.04.019. Epub
[PubMed PMID: 23866890]
[14]
McCormick ZL, Reddy R, Korn M, Dayanim D, Syed RH, Bhave M, Zhukalin M, Choxi S, Ebrahimi A, Kendall MC, McCarthy RJ, Khan D, Nagpal G, Bouffard K, Walega DR. A Prospective Randomized Trial of Prognostic Genicular Nerve Blocks to Determine the Predictive Value for the Outcome of Cooled Radiofrequency Ablation for Chronic Knee Pain Due to Osteoarthritis. Pain medicine (Malden, Mass.). 2018 Aug 1:19(8):1628-1638. doi: 10.1093/pm/pnx286. Epub
[PubMed PMID: 29300971]
[15]
Manchikanti L, Pampati V, Fellows B, Baha AG. The inability of the clinical picture to characterize pain from facet joints. Pain physician. 2000 Apr:3(2):158-66
[PubMed PMID: 16906195]
[16]
Cohen SP, Bhaskar A, Bhatia A, Buvanendran A, Deer T, Garg S, Hooten WM, Hurley RW, Kennedy DJ, McLean BC, Moon JY, Narouze S, Pangarkar S, Provenzano DA, Rauck R, Sitzman BT, Smuck M, van Zundert J, Vorenkamp K, Wallace MS, Zhao Z. Consensus practice guidelines on interventions for lumbar facet joint pain from a multispecialty, international working group. Regional anesthesia and pain medicine. 2020 Jun:45(6):424-467. doi: 10.1136/rapm-2019-101243. Epub 2020 Apr 3
[PubMed PMID: 32245841]
Level 1 (high-level) evidence
[17]
Conger A, Burnham T, Salazar F, Tate Q, Golish M, Petersen R, Cunningham S, Teramoto M, Kendall R, McCormick ZL. The Effectiveness of Radiofrequency Ablation of Medial Branch Nerves for Chronic Lumbar Facet Joint Syndrome in Patients Selected by Guideline-Concordant Dual Comparative Medial Branch Blocks. Pain medicine (Malden, Mass.). 2020 May 1:21(5):902-909. doi: 10.1093/pm/pnz248. Epub
[PubMed PMID: 31609391]
Level 2 (mid-level) evidence
[18]
Djebbar S, Rossi IM, Adler RS. Ultrasound-Guided Cryoanalgesia of Peripheral Nerve Lesions. Seminars in musculoskeletal radiology. 2016 Nov:20(5):461-471. doi: 10.1055/s-0036-1596063. Epub 2016 Dec 21
[PubMed PMID: 28002868]
[19]
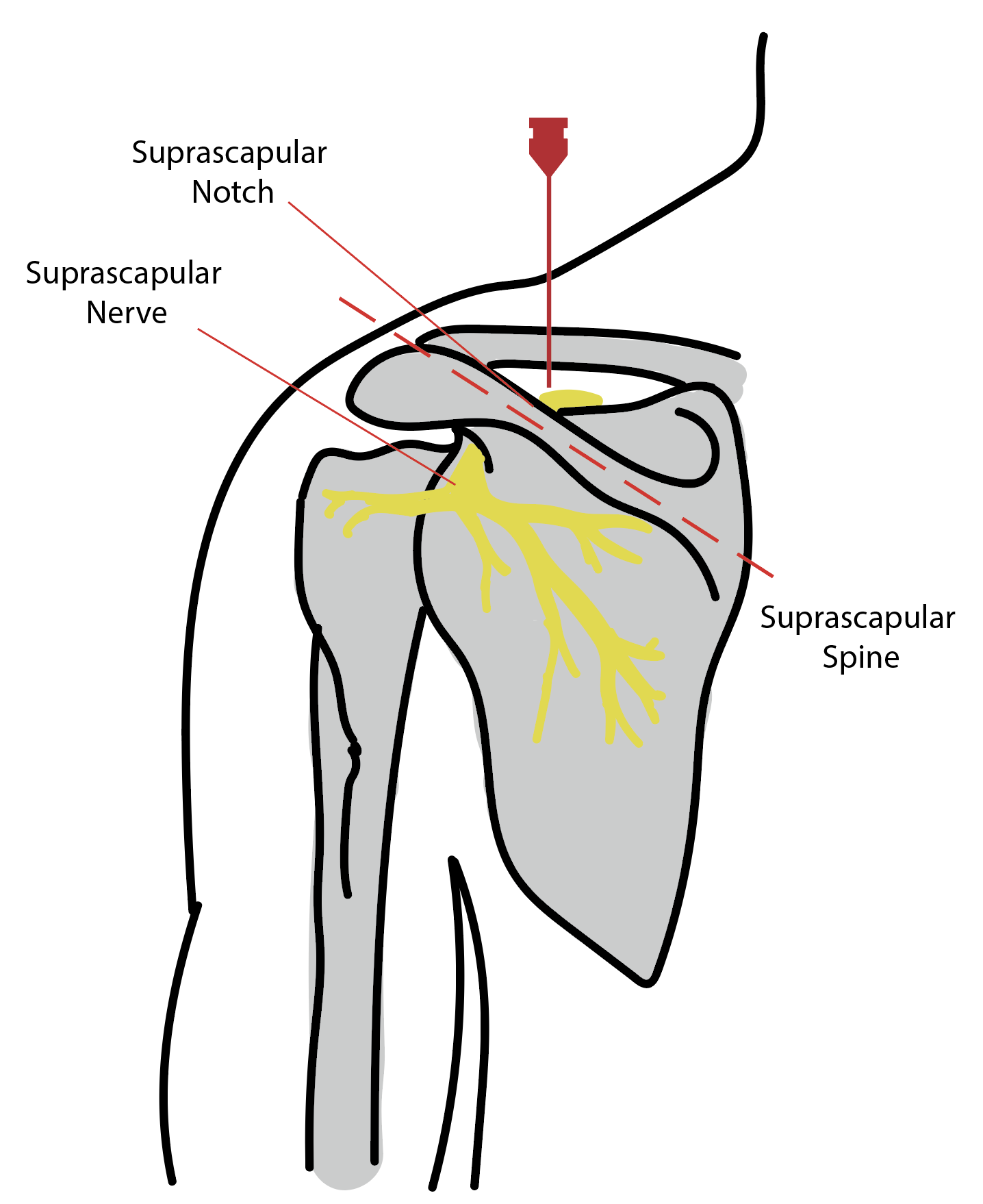
Chang KV, Hung CY, Wang TG, Yang RS, Sun WZ, Lin CP. Ultrasound-Guided Proximal Suprascapular Nerve Block With Radiofrequency Lesioning for Patients With Malignancy-Associated Recalcitrant Shoulder Pain. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2015 Nov:34(11):2099-105. doi: 10.7863/ultra.14.12042. Epub 2015 Oct 9
[PubMed PMID: 26453125]
[20]
Tekin I, Mirzai H, Ok G, Erbuyun K, Vatansever D. A comparison of conventional and pulsed radiofrequency denervation in the treatment of chronic facet joint pain. The Clinical journal of pain. 2007 Jul-Aug:23(6):524-9
[PubMed PMID: 17575493]
[21]
Toukhy ME, Campkin NT. Severe diarrhea following neurolytic coeliac plexus block: case report and literature review. The American journal of hospice & palliative care. 2011 Nov:28(7):511-4. doi: 10.1177/1049909111402185. Epub 2011 Mar 21
[PubMed PMID: 21422068]
Level 3 (low-level) evidence
[22]
Dobrogowski J, Wrzosek A, Wordliczek J. Radiofrequency denervation with or without addition of pentoxifylline or methylprednisolone for chronic lumbar zygapophysial joint pain. Pharmacological reports : PR. 2005 Jul-Aug:57(4):475-80
[PubMed PMID: 16129914]
[23]
McCormick ZL, Conger A, Kendall R, Wagner G, Henrie AM, Littell M, Sperry BP, Petersen R, Cooper AN, Teramoto M, Burnham TR. A pragmatic randomized prospective trial of cooled radiofrequency ablation of the medial branch nerves versus facet joint injection of corticosteroid for the treatment of lumbar facet syndrome: 12 month outcomes. Pain medicine (Malden, Mass.). 2023 Dec 1:24(12):1318-1331. doi: 10.1093/pm/pnad107. Epub
[PubMed PMID: 37578437]
Level 1 (high-level) evidence
[24]
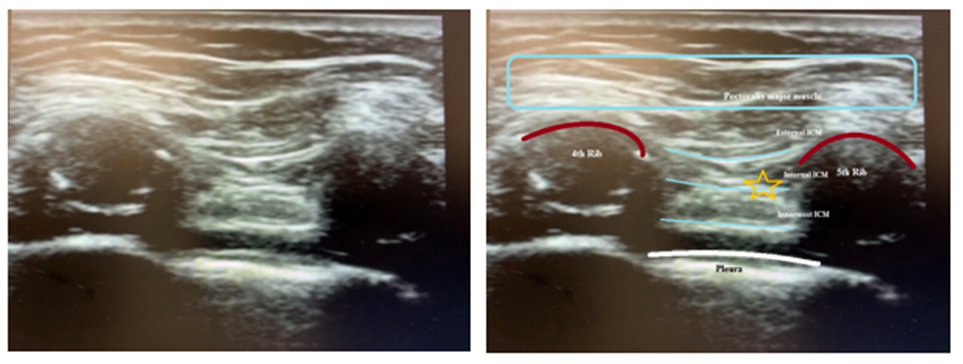
Abd-Elsayed A, Lee S, Jackson M. Radiofrequency Ablation for Treating Resistant Intercostal Neuralgia. Ochsner journal. 2018 Spring:18(1):91-93
[PubMed PMID: 29559878]
[25]
Jamison DE, Cohen SP. Radiofrequency techniques to treat chronic knee pain: a comprehensive review of anatomy, effectiveness, treatment parameters, and patient selection. Journal of pain research. 2018:11():1879-1888. doi: 10.2147/JPR.S144633. Epub 2018 Sep 18
[PubMed PMID: 30271194]
[26]
Iannaccone F, Dixon S, Kaufman A. A Review of Long-Term Pain Relief after Genicular Nerve Radiofrequency Ablation in Chronic Knee Osteoarthritis. Pain physician. 2017 Mar:20(3):E437-E444
[PubMed PMID: 28339444]
[27]
Amr SA, Reyad RM, Othman AH, Mohamad MF, Mostafa MM, Alieldin NH, Hamed FA. Comparison between radiofrequency ablation and chemical neurolysis of thoracic splanchnic nerves for the management of abdominal cancer pain, randomized trial. European journal of pain (London, England). 2018 Nov:22(10):1782-1790. doi: 10.1002/ejp.1274. Epub 2018 Jul 11
[PubMed PMID: 29975804]
[28]
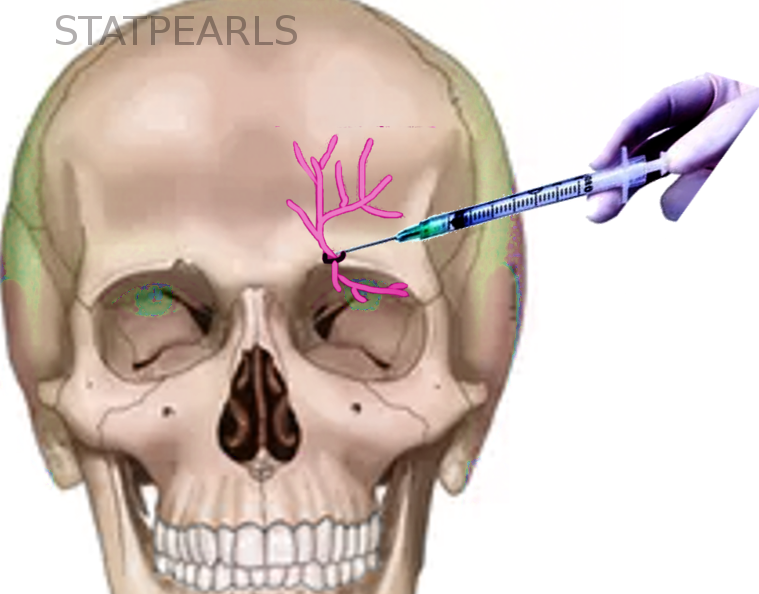
Abd-Elsayed A, Kreuger L, Wheeler S, Robillard J, Seeger S, Dulli D. Radiofrequency Ablation of Pericranial Nerves for Treating Headache Conditions: A Promising Option for Patients. Ochsner journal. 2018 Spring:18(1):59-62
[PubMed PMID: 29559871]
[29]
Solberg J, Copenhaver D, Fishman SM. Medial branch nerve block and ablation as a novel approach to pain related to vertebral compression fracture. Current opinion in anaesthesiology. 2016 Oct:29(5):596-9. doi: 10.1097/ACO.0000000000000375. Epub
[PubMed PMID: 27548307]
[30]
Cohen SP, Doshi TL, Constantinescu OC, Zhao Z, Kurihara C, Larkin TM, Griffith SR, Jacobs MB, Kroski WJ, Dawson TC, Fowler IM, White RL, Verdun AJ, Jamison DE, Anderson-White M, Shank SE, Pasquina PF. Effectiveness of Lumbar Facet Joint Blocks and Predictive Value before Radiofrequency Denervation: The Facet Treatment Study (FACTS), a Randomized, Controlled Clinical Trial. Anesthesiology. 2018 Sep:129(3):517-535. doi: 10.1097/ALN.0000000000002274. Epub
[PubMed PMID: 29847426]
[31]
Huang P, Liu H, Huang L, Jin X. The long-term outcome of CT-guided radiofrequency ablation of the peripheral branches of the trigeminal nerve in trigeminal neuralgia. Neurosurgical review. 2024 Jan 6:47(1):33. doi: 10.1007/s10143-023-02269-w. Epub 2024 Jan 6
[PubMed PMID: 38182916]
[32]
Wang Z, Wang Z, Li K, Su X, Du C, Tian Y. Radiofrequency thermocoagulation for the treatment of trigeminal neuralgia. Experimental and therapeutic medicine. 2022 Jan:23(1):17. doi: 10.3892/etm.2021.10939. Epub 2021 Oct 30
[PubMed PMID: 34815769]
[33]
Karm MH, Kwon HJ, Kim CS, Kim DH, Shin JW, Choi SS. Cooled radiofrequency ablation of genicular nerves for knee osteoarthritis. The Korean journal of pain. 2024 Jan 1:37(1):13-25. doi: 10.3344/kjp.23344. Epub
[PubMed PMID: 38155108]
[34]
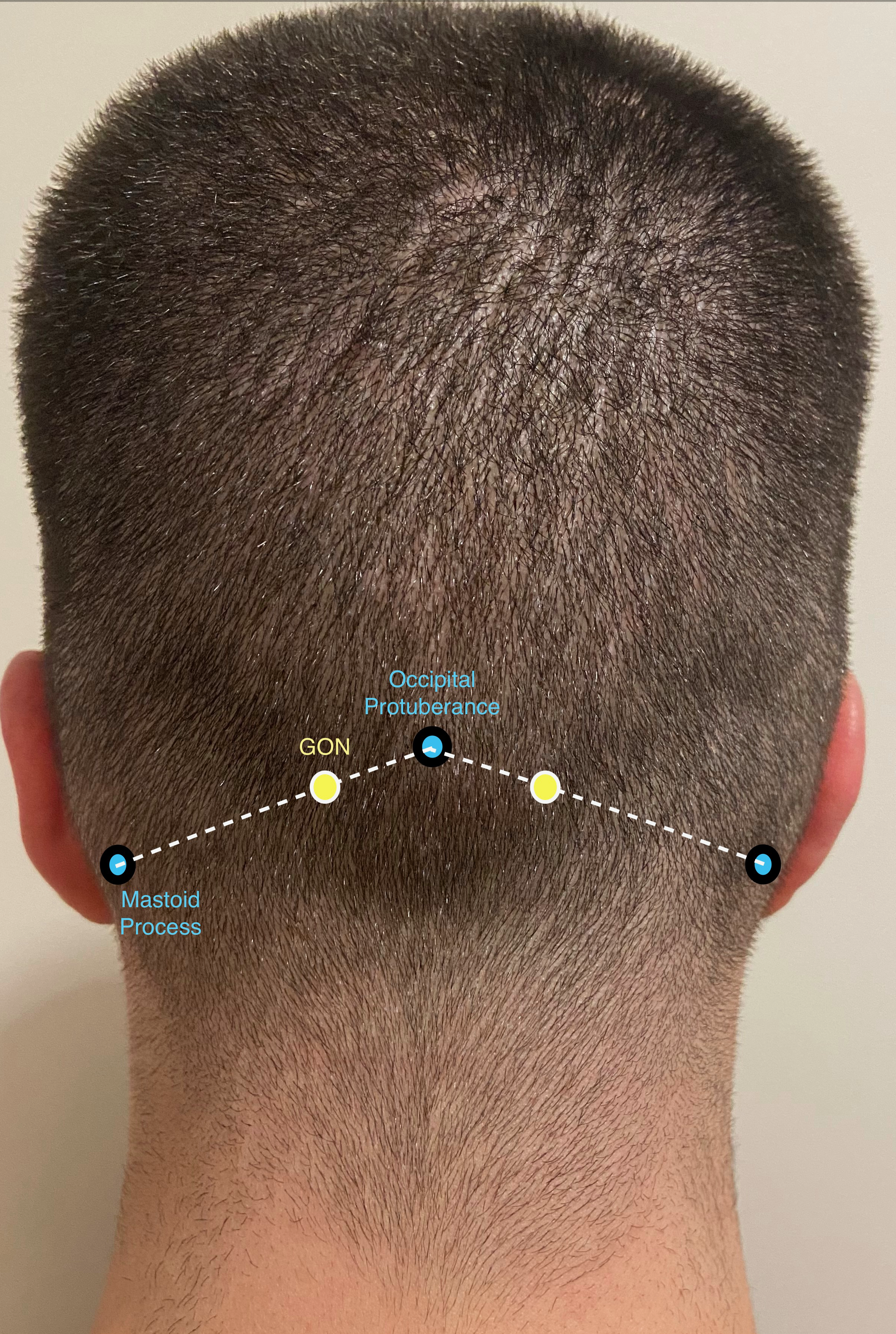
Fabry A, Nedunchelian M, Stacoffe N, Guinebert S, Zipfel J, Krainik A, Maindet C, Kastler B, Grand S, Kastler A. Review of craniofacial pain syndromes involving the greater occipital nerve: relevant anatomy, clinical findings, and interventional management. Neuroradiology. 2024 Feb:66(2):161-178. doi: 10.1007/s00234-023-03273-z. Epub 2023 Dec 30
[PubMed PMID: 38159141]
[35]
Odonkor CA, Tang T, Taftian D, Chhatre A. Bilateral Intra-Articular Radiofrequency Ablation for Cervicogenic Headache. Case reports in anesthesiology. 2017:2017():1483279. doi: 10.1155/2017/1483279. Epub 2017 Jan 9
[PubMed PMID: 28149652]
Level 3 (low-level) evidence
[36]
Fiala KJ, Martens JM, Keith MK, Ghouse A, Abd-Elsayed A. Cooled Radiofrequency Ablation for Intercostal Neuralgia. Ochsner journal. 2023 Summer:23(2):159-163. doi: 10.31486/toj.22.0087. Epub
[PubMed PMID: 37323517]
[37]
Reyad RM, Ghobrial HZ, Shaker EH, Reyad EM, Shaaban MH, Hashem RH, Darwish WM. Modified technique for thermal radiofrequency ablation of Thoracic dorsal root ganglia under combined fluoroscopy and CT guidance: a randomized clinical trial. BMC anesthesiology. 2019 Dec 18:19(1):234. doi: 10.1186/s12871-019-0906-4. Epub 2019 Dec 18
[PubMed PMID: 31852438]
Level 1 (high-level) evidence
[38]
Alanbay E, Aras B, Kesikburun S, Kizilirmak S, Yasar E, Tan AK. Effectiveness of Suprascapular Nerve Pulsed Radiofrequency Treatment for Hemiplegic Shoulder Pain: A Randomized-Controlled Trial. Pain physician. 2020 Jun:23(3):245-252
[PubMed PMID: 32517390]
Level 1 (high-level) evidence
[39]
Misra S, Ward S, Coker C. Pulsed radiofrequency for chronic testicular pain-a preliminary report. Pain medicine (Malden, Mass.). 2009 May-Jun:10(4):673-8. doi: 10.1111/j.1526-4637.2009.00581.x. Epub 2009 Mar 19
[PubMed PMID: 19302438]
[40]
Vallejo R, Benyamin RM, Kramer J, Stanton G, Joseph NJ. Pulsed radiofrequency denervation for the treatment of sacroiliac joint syndrome. Pain medicine (Malden, Mass.). 2006 Sep-Oct:7(5):429-34
[PubMed PMID: 17014602]
[41]
Rozen D, Parvez U. Pulsed radiofrequency of lumbar nerve roots for treatment of chronic inguinal herniorraphy pain. Pain physician. 2006 Apr:9(2):153-6
[PubMed PMID: 16703977]
[42]
Teixeira A, Sluijter ME. Intradiscal high-voltage, long-duration pulsed radiofrequency for discogenic pain: a preliminary report. Pain medicine (Malden, Mass.). 2006 Sep-Oct:7(5):424-8
[PubMed PMID: 17014601]
[43]
Caicedo Gutiérrez L, Moreno Martínez D. Case report: Baxter's nerve radiofrequency in patient with plantar fasciitis nonresponsive to conventional treatment. Revista espanola de anestesiologia y reanimacion. 2022 May:69(5):306-309. doi: 10.1016/j.redare.2022.05.001. Epub 2022 May 13
[PubMed PMID: 35577703]
Level 3 (low-level) evidence
[44]
Kallas ON, Nezami N, Singer AD, Wong P, Kokabi N, Bercu ZL, Umpierrez M, Tran A, Reimer NB, Oskouei SV, Gonzalez FM. Cooled Radiofrequency Ablation for Chronic Joint Pain Secondary to Hip and Shoulder Osteoarthritis. Radiographics : a review publication of the Radiological Society of North America, Inc. 2022 Mar-Apr:42(2):594-608. doi: 10.1148/rg.210074. Epub 2022 Feb 11
[PubMed PMID: 35148246]
[45]
Zakrzewska JM, Linskey ME. Trigeminal neuralgia. BMJ clinical evidence. 2009 Mar 12:2009():. pii: 1207. Epub 2009 Mar 12
[PubMed PMID: 19445753]