Introduction
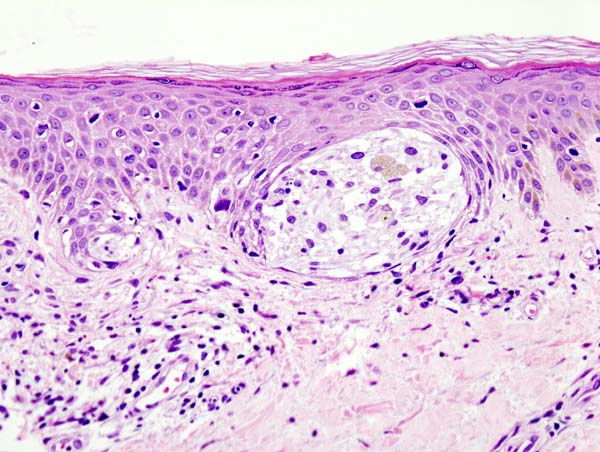
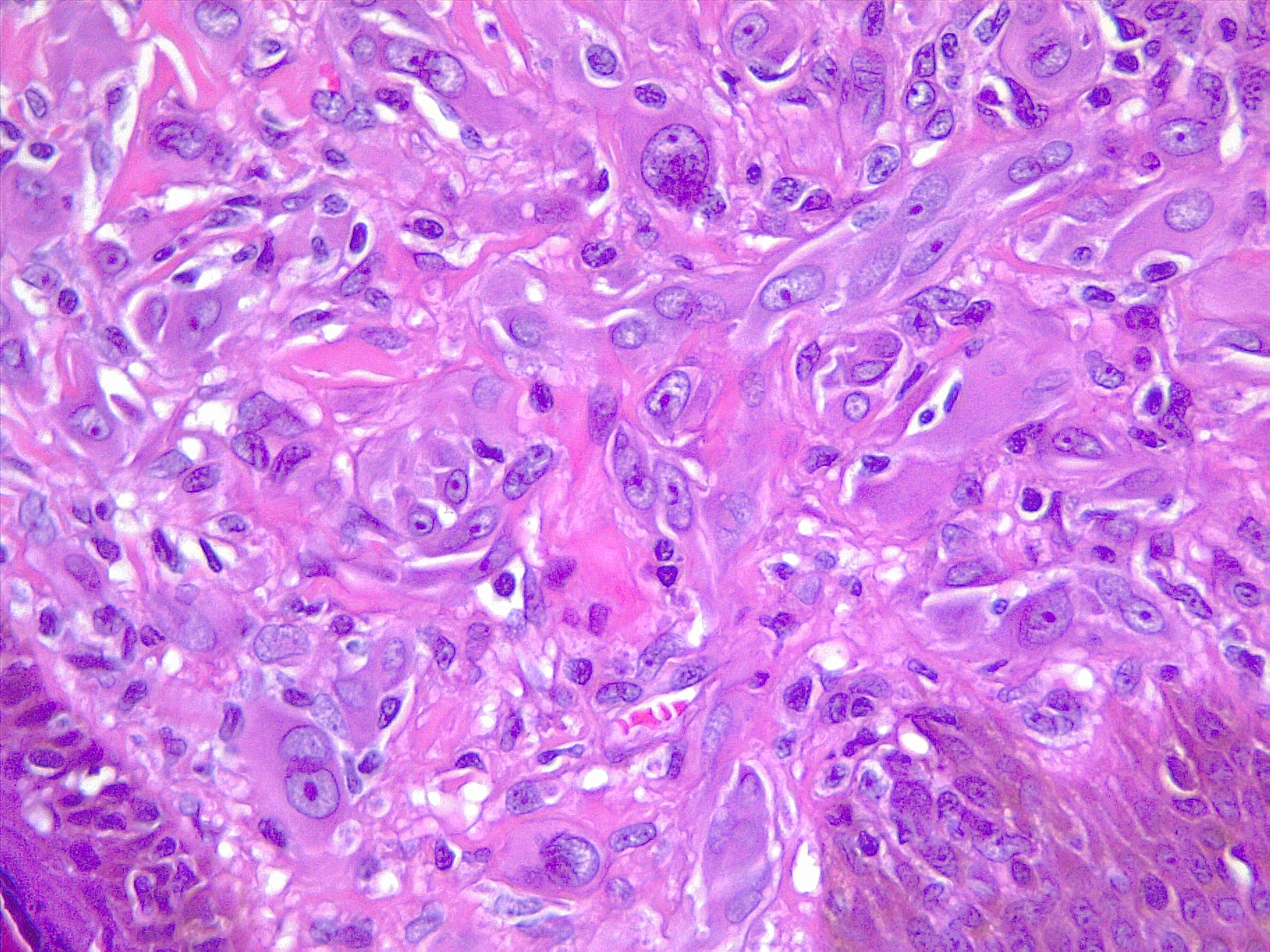
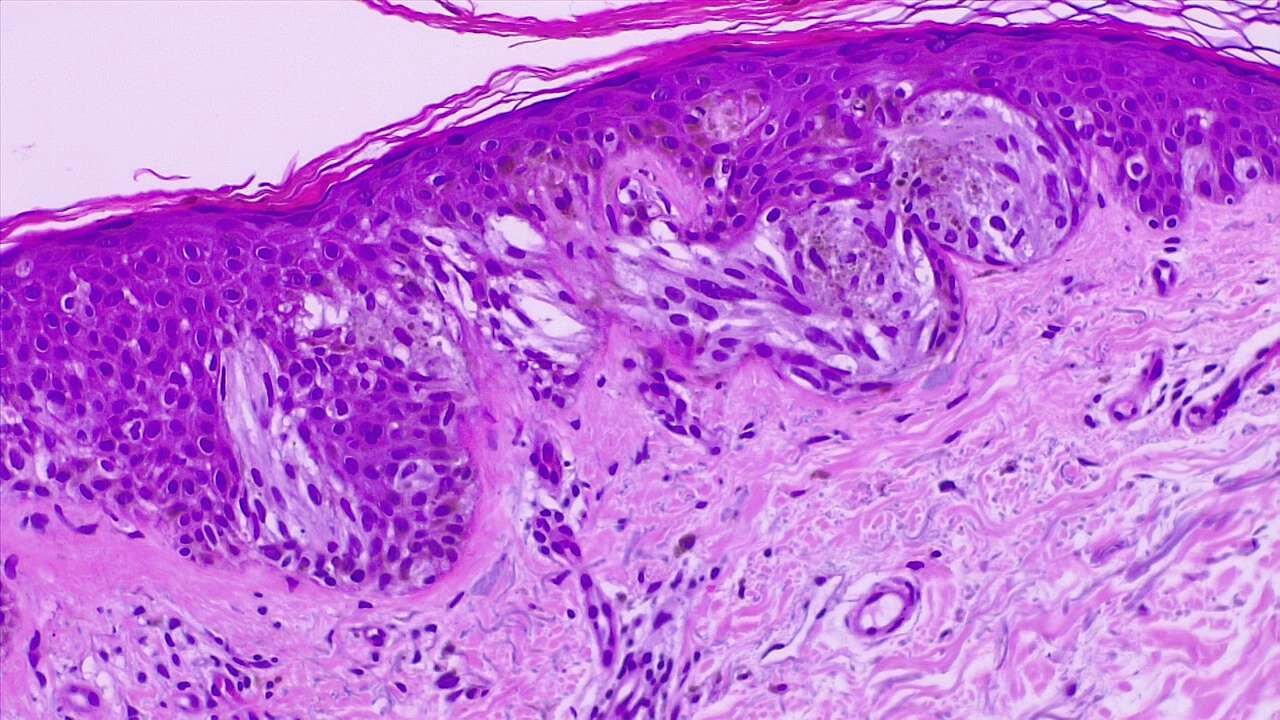
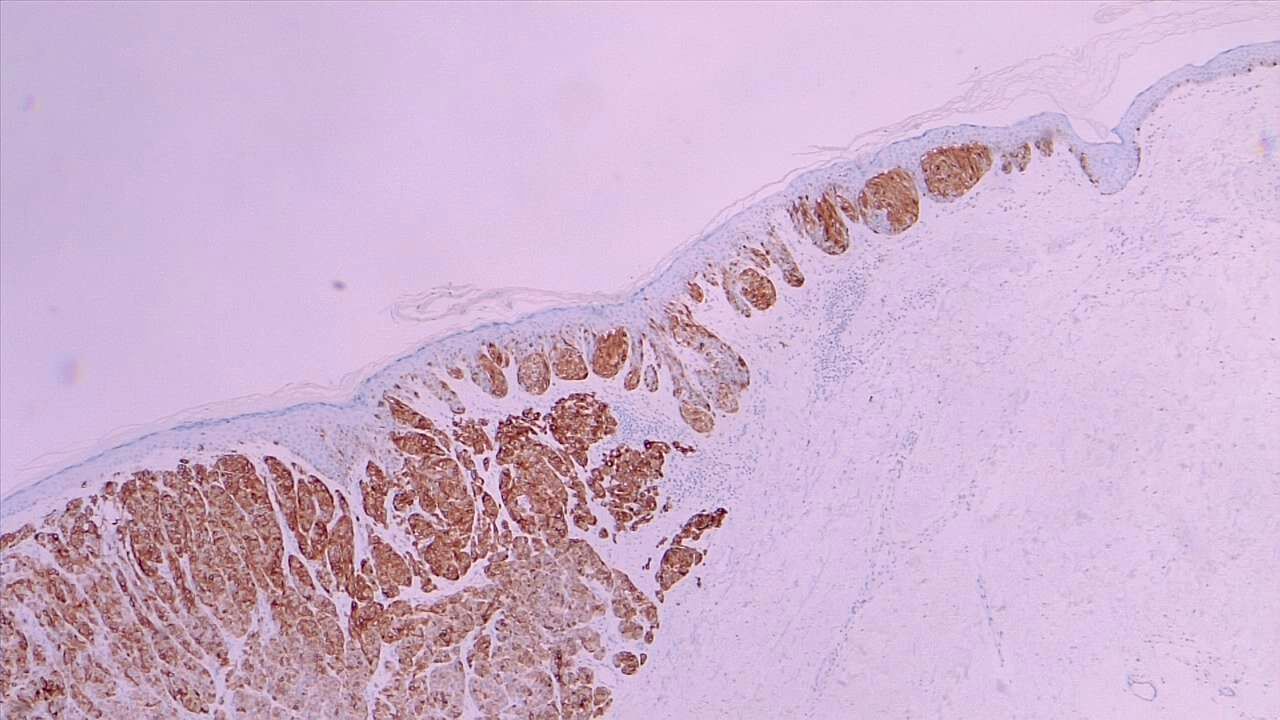
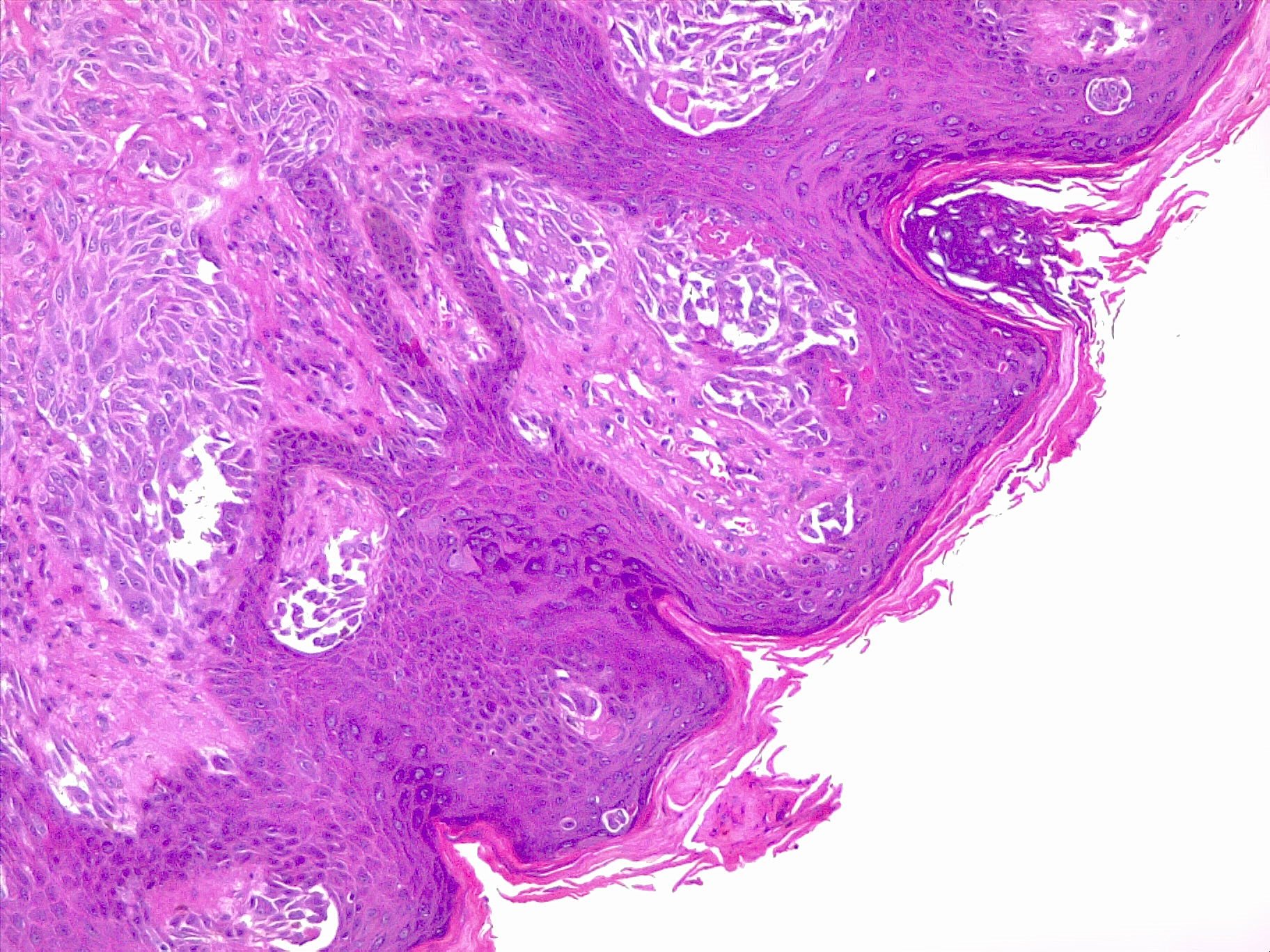
Melanoma is a skin cancer of the melanocytes that occurs after DNA mutation, most often secondary to excess sun exposure (see Image. Spitz Melanoma of the Skin). Fair-skinned and light-haired persons living in high sun-exposure environments are at greatest risk. Clinically, melanoma exhibits shape irregularity, irregular color, and asymmetry. Sometimes, melanoma exhibits ulceration and bleeding, which is associated with a poorer prognosis. A punch biopsy often reveals atypical nests of melanocytes that accumulate and coalesce at the dermo-epidermal junction (see Image. Malignant Melanoma of the Skin). The depth of melanoma is the most important prognostic factor. Two staging systems are available to assess depth: Breslow and Clark levels. In the past, physicians used the Clark level. However, Breslow level is now the standard of care because it is more specific. Depending on the depth of the lesion, the 10-year survival rate varies tremendously. Also, a melanoma lesion's depth determines the margins that a surgeon is to take when resecting the lesion.[1][2][3]
Issues of Concern
The physical exam should consist of checking the entire body of the patient for any suspicious lesions. Specifically, the ABCDEs should be assessed: asymmetry, border irregularity, color (variation), diameter (more than 5 mm), and/or erythema. Any positivity in the exam should raise suspicion for malignant melanoma, and then the practitioner should obtain a biopsy of the lesion (see Image. Malignant Melanoma). It is important not to perform a shave biopsy on lesions suspected to have malignant melanoma but rather perform a punch biopsy or an excisional biopsy if the lesion is less than 7 mm. Shave biopsy does not allow to assess the entire depth and may ruin any chance of proper staging.
Causes
Mutations in DNA cause melanoma. The risk factors for skin melanoma is excessive exposure to the sun, especially in people with lighter skin.
Anatomical Pathology
There are various types of melanoma: superficial spreading melanoma (most common), nodular (worst prognosis), lentigo malignant (best prognosis), and acral lentiginous (occurs on palms of hand and soles of feet, common in African Americans). See Images. Malignant Melanoma, Superficial Spread and Melanoma In Situ).
Melanoma most commonly metastasizes to the skin and lungs, but sometimes metastasizes to the small bowel (most common site of metastases). When diffusely metastatic, there are chemotherapy options available, namely intralesional Bacillus Calmette-Guerin therapy (BCG) or immunotherapy with vaccines aimed to raise the levels of anti-melanoma tumor antibodies.
Biochemical and Genetic Pathology
Ultraviolet radiation is strongly associated with DNA mutations and the development of melanoma.
BRAF is an oncogene often altered in melanomas. The most common BRAF mutation in this setting leads to the p.V600E protein substitution, especially in the low-CSD (cumulative ssun damage) group.
NF1, NRAS, BRAF (non-V600E mutations), KIT are commonly altered in the high-CSD group.
TERT is commonly altered in the promotor region and is related to both groups.
CDKN2A is the gene encoding for p16 protein and is frequently altered in melanomas. p16 is an oncosoppressor and is inhibited during melanoma carcinogenesis either directly or indirectly.
Clinicopathologic Correlations
Surgical Excision
- Main Lesion
- Less than 0.76 mm excised with 1 cm margin.
- 0.76 to 1.0 mm excised with 2 cm margin
- More than 1 mm excised with 2cm to 3 cm margin
- Excision should be down to the fascia
Because melanoma of the skin carries a high mortality rate, prevention should be emphasized in all patients, especially fair-skinned patients. Wearing sunscreen, avoiding the sun, and checking skin annually with a dermatologist is highly recommended.
Staging
Once the biopsy is obtained, one moves on to assess the depth of the melanoma. Based on the Breslow Depth, the surgeon decides on surgical excision margins.
Surgery
Preoperatively, it is important to discuss the patient's overall plan, including the risks of the procedure, aesthetic results, and the likelihood of cure. It is important to have detailed and realistic communication with the patient about the scar that may be left after surgery, the need for regular skin cancer screening after surgery, and tobacco cessation if the patient is a current smoker. Because cancer is a systemic disease, the patient with malignant melanoma may be predisposed to more skin cancer and even other cancer types. This is why such screening is an important detail to discuss.
Once surgery plans are made, the surgeon has to decide whether a sentinel lymph node biopsy needs to be performed. Sentinel lymph node biopsy should be performed on patients with greater than 10 mm depth or less than 10 mm depth and ulcerations or high-grade pathology. A technetium colloid is injected around the lesion site, and a lymphoscintigraphy scan will determine which lymphatic drainage tract is draining the lymph node. This will decide where the sentinel lymph node biopsy will be performed. Usually, a lymphoscintigraphy scan is performed on the day of surgery.
The treatment for malignant melanoma is wide, local excision with margins noted above. Surgeons should never attempt Mohs surgery for malignant melanoma. On extremities, usually, an elliptical incision is made in a 3:1 spacing (length: width) to allow for cosmetic closure results. The incision should be carried down to superficial muscle fascia but not deep muscle fascia. Flap creation is sometimes needed to allow for tension-free closure. The incision should be made along the length of the extremity. Sometimes skin grafting is required to cover the excised region if not enough skin is available for primary closure. However, this should be a last resort, as it can be quite cosmetically unappealing.
There is a role in adjuvant interferon therapy in high-risk melanoma patients, such as ones with high-grade lesions or ulcerated melanomas. Genetic testing is available to determine who is at high risk of recurrence or in patients with a family history of melanoma or pancreatic cancer.
The most common site of metastasis to small bowel is malignant melanoma. Metastatic melanoma should be treated with surgery for palliation only and adjuvant chemotherapy and interferon therapy.
Interferon therapy works by creating antibodies in the lab that have been pre-exposed to cancer cells. Those antibodies are then injected into the patient and are ready to fight cancer cells.
After the procedure, the pathology should be candidly reviewed with the patient, including the need for further treatment (such as when sentinel lymph node comes back positive, warrants full lymph node dissection of the region) and the prognosis of the lesion based on excision and margins.
Education and prevention are the most important tools to prevent malignant melanoma. All patients should be counseled on skin cancer preventative tactics such as staying out of the sun and wearing high sun protection factor (SPF) on exposed areas even with the cloudy weather. Preventative education should start in school-aged children. Community-based programs designed to screen individuals at risk aid in early diagnosis and may ultimately improve mortality associated with malignant skin neoplasia.[4][5]
Clinical Significance
In the United States, malignant melanoma is now the fifth most common cancer in men and seventh in women, with about 50,000 new cases diagnosed annually. About 15% of these lead to death. At the time of diagnosis, about 80% present with localized disease, 15% with regional disease, and 5% with distant metastasis. When a physician refers a patient with malignant melanoma to a surgeon, and a shave biopsy is used to confirm the diagnosis, it is imperative that the surgeon tactfully educate that physician about appropriate diagnostic measures of the melanoma.[6]