Introduction
The long thoracic nerve, also referred to as the external respiratory nerve of Bell or posterior thoracic nerve, arises from the upper portion of the superior trunk of the brachial plexus and typically receives contributions from cervical nerve roots C5, C6, and C7. It is responsible for the innervation of the serratus anterior muscle; the long thoracic nerve descends posteriorly to the roots of the brachial plexus and anteriorly to the scalenus posterior muscle, and courses along the chest wall in the mid-axillary line to lie on the superficial surface of the serratus anterior muscle. Due to its long, relatively superficial course, the long thoracic nerve is susceptible to damage during certain surgical procedures or through direct trauma or stretch. When the long thoracic nerve is injured, a phenomenon known as winging of the scapula results.[1]
Structure and Function
The long thoracic nerve is the motor nerve to the serratus anterior muscle, which functions to pull the scapula forward around the thorax, allowing for anteversion of the arm, and to lift the ribs, assisting in respiration. Also, the serratus anterior inferior is responsible for the anterolateral motion of the scapula, which allows for arm elevation.
The long thoracic nerve runs downward and passes anterior to the scalenus posterior muscle, courses distal and laterally deep to the clavicle and superficial to the first and second rib, and travels inferiorly on the chest wall along the mid-axillary line on the outer surface of the serratus anterior muscle for a distance of approximately 22 to 24 centimeters.[2] The nerve lies posterior to the first part of the axillary artery and from where it emerges to the posterior angle of the second rib, the nerve travels at an estimated 30-degree angle posteriorly, relative to the anterior axillary line. From this junction, the nerve courses between the posterior and middle axillary lines.[3]
The long thoracic nerve forms as an upper portion originating from the C5 and C6 nerve roots and a lower portion coming from the C7 nerve root. The fusion of these two portions occurs in the axilla. Within the supraclavicular region, the upper division of the long thoracic nerve travels parallel to the brachial plexus near the suprascapular nerve.[3]
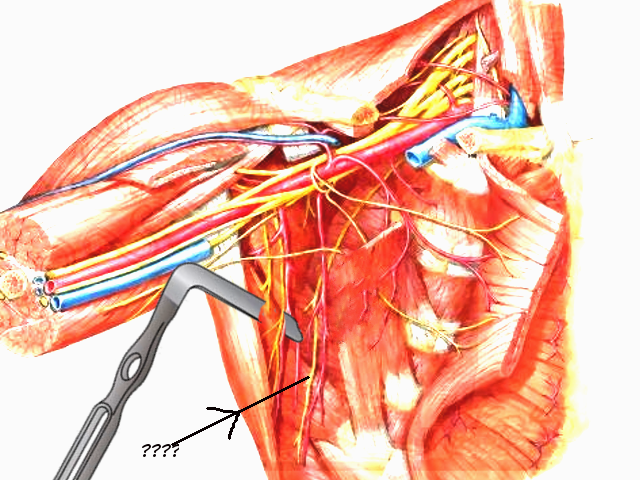
A distinct characteristic of the long thoracic nerve is its superficial course along the entire length of the serratus anterior muscle it supplies. The nerve further divides into smaller branches that are parallel to the main trunk before turning at right angles and providing innervation to the individual slips by entering via the superior aspect of the slips. A collateral branch of the thoracodorsal artery, specifically the serratus anterior branch, joins the long thoracic nerve at the proximal edge of the distal serratus anterior head, and eventually travels over the nerve and divides into the terminal muscle branches. This juncture is known as Crow’s feet and is significant in serving as a landmark in flap transfer surgeries.
Blood Supply and Lymphatics
The long thoracic nerve and its blood supply are vulnerable to both compression and stretching anterior to the lower segment of the scapula. The subscapular artery via the inferior angle of the scapula is responsible for the blood supply to the lowest four to six digitations of the serratus anterior muscle as well as the peripheral portion of the long thoracic nerve. As such, nerve damage may result after poor epineural blood flow as a consequence of compression or traction of the subscapular artery. Both the long thoracic nerve and its blood supply are anchored to the serratus anterior muscle by the fascia, thus moving with the muscle as it contracts. With arm adduction, the scapula moves anteriorly, while simultaneously bringing the nerve and blood vessels anteriorly as well, out of the way of the scapula. During arm extension, the serratus anterior muscle prevents winging of the scapula, thereby preventing stretching of the nerve and vasculature.[4]
Muscles
The serratus anterior muscle, known as the “boxer’s muscle,” receives its innervation solely from the long thoracic nerve, which when damaged results in paralysis of the muscle, a phenomenon known as a winged scapula. The serratus anterior is primarily responsible for protraction of the scapula, a movement occurring when throwing a punch. The serratus anterior works in conjunction with the trapezius muscle to allow for sustained upward rotation of the scapula, which is essential for overhead lifting.
Located deep to the subscapularis, the serratus anterior muscle is subdivided into three components depending upon their origins and points of insertion: serratus anterior superior, serratus anterior intermediate, and serratus anterior inferior. Consequently, the innervation of the serratus anterior varies according to the part of the muscle. The superior segment is innervated by both an independent branch unrelated to the main trunk of the long thoracic nerve as well as by the actual long thoracic nerve. Interestingly, the course of the independent branch mirrors that of the nerves charged with innervation of the levator scapulae muscle, thereby suggesting a relation between the serratus anterior superior and the levator scapulae muscle. The serratus anterior intermediate is innervated by the long thoracic nerve, while the inferior segment receives innervation from two sources, namely the long thoracic nerve and a branch of the intercostal nerve.[5]
Physiologic Variants
While the long thoracic nerve typically arises from the anterior rami of the C5, C6, and C7 roots of the brachial plexus, the nerve also receives supply from C8 in approximately 10% of the population. Documentation exists for an aberrant connection between the long thoracic nerve and dorsal scapular nerve. It has also known that the long thoracic nerve, which is typically formed by the three ventral rami of C5, C6, and C7 cervical nerves, was comprised mainly by C6 and C7. There are documented instances where the C5 component of the long thoracic nerve was absent, but a communicating branch from C6 was assumed to carry fibers from C5.[6]
Moreover, typically the long thoracic nerve is formed by the joining of C5, C6, and C7 components in the axillary region. However, there has been documentation of the union of these components of the long thoracic nerve occurring above the axillary region posterior to the clavicle. This physiological variant increases susceptibility to nerve injury during clavicular fractures and in the treatment of thoracic outlet syndrome.[6]
Surgical Considerations
Cases of damage to the long thoracic nerve result in a phenomenon known as winged scapula, which is due to paralysis of the serratus anterior or trapezius muscles. Procedures in the thoracic region, including radical mastectomy, transthoracic sympathectomy, transaxillary thoracotomy, misplaced intercostal drains, video thoracoscopy port insertion, axillary lymph node dissections, chest tube placements, and resection of the first rib, increase the risk for proximal injury of the long thoracic nerve. Moreover, young children undergoing a posterolateral thoracotomy incision for closed heart procedures, or any other procedures requiring separation of the serratus anterior muscles from the latissimus dorsi, are susceptible to long thoracic nerve injury and subsequent winging of the scapula. Hence, understanding the anatomical course of the long thoracic nerve is essential in increasing the surgical success rate and decreasing the risk of unintentional nerve damage. Physiological variants in the course of the long thoracic nerve positionally to the middle scalene muscle may lead to iatrogenic nerve injury and subsequent scapular winging as it has been documented that the nerve roots may be found anterior, posterior, or through the middle scalene muscle.
Further, with a winged scapula, the serratus anterior muscle is not functioning synchronously with the other muscles of the shoulder girdle. This condition predisposes to abnormal movements of the scapula relative to the long thoracic nerve. For instance, when a patient is under general anesthesia, there is reduced control of the shoulder girdle muscles, and passive adduction of the arm (such as when a patient’s arm is raised and crossed over his or her chest) may cause the scapula to shift anteriorly. This could cause creasing the of the muscle and compression of the long thoracic nerve and its blood supply.[4]
Clinical Significance
Denervation of the long thoracic nerve results in weakness of the serratus anterior and winging of the scapula. Any dysfunction/weakness affecting any muscle that stabilizes the scapula may lead to scapula winging. A weakness of the serratus anterior muscle is the most prevalent cause of winging due to the weak protraction of the scapula and unopposed medial scapula retraction by the rhomboid muscles and elevation by the trapezius, resulting in medial winging of the scapula. This condition is easily differentiated from the much less common lateral winging due to weakness of the trapezius muscle which is supplied by the spinal accessory nerve.
Compared to other nerves of the brachial plexus, the long thoracic nerve has a comparatively smaller diameter which, when coupled with its minimal connective tissue and superficial course along the surface of the serratus anterior muscle, increases its susceptibility to damage both operatively or non-operatively with subsequent development of scapular winging. The long thoracic nerve travels to the level of the eighth or ninth rib and is relatively unprotected from the axilla down. As such, the nerve may suffer exposure to external injury, including compression from a cast, use of crutches, anesthesia, or Saturday night palsy.[4] Other non-surgical causes of nerve damage include heavy load bearing; compression from the middle scalene muscle, fascial sheath, or second rib; entrapment within the middle or posterior scalene muscles; and nerve traction caused by athletics, overuse as in unaccustomed household or gardening activities such as digging, compression by shoulder straps of heavy backpacks, and rarely from chiropractic manipulation.[7][2][8][2]
Passive extension of the arm and uncoordinated scapular movements during sports, such as sudden jerking of the shoulder, may stretch the long thoracic nerve and its blood vessels, resulting in scapular winging. It has been noted that with increasing proximity of the long thoracic nerve to the lower angle of the scapula, the less scapular motion is required to compress or stretch the nerve. Individual differences in the distance between the nerve and the scapula may account for the variable incidence of serratus anterior paralysis.[4]
Other Issues
The management and prognosis of long thoracic neuropathy are dependent upon the mechanism of nerve injury. For instance, recovery from neuralgic amyotrophy is typically a gradual process occurring throughout one to three years. Contrastingly, injury as a result of a repetitive activity or carrying of heavy loads are incomplete and generally resolve spontaneously in 6 to 24 months. In these cases, physical therapy and exercise are crucial in the maintenance of the range of motion and strengthening of surrounding muscles, such as the trapezius and rhomboid muscles. Trauma to the long thoracic nerve, either from a direct insult to the shoulder or lateral chest wall, is generally more severe and recovery is limited. Patients may be surgical candidates if they do not experience functional recovery. There have been recent case reports documenting successful treatment with nerve transfer utilizing the thoracodorsal or medial pectoral nerves.[9]
Inasmuch as the long thoracic nerve innervates the serratus anterior muscle, clinical examination of neural integrity is assessed by observing the power and symmetry of bilateral scapulae and serratus anterior muscles. Any asymmetry, muscular atrophy, or fasciculation noted is suggestive of long thoracic nerve injury, and the serratus muscle wall test can be performed to examine and compare the strength of the serratus anterior. The serratus wall test entails the patient facing approximately 2 feet away from a wall and pushing against the wall with palms flat at waist level. Damage to the long thoracic nerve would manifest as winging (medial winging) of the scapula secondary to paralysis of the serratus anterior muscle.