Continuing Education Activity
Head and neck cancer is the sixth most common cancer worldwide. The single most important factor affecting prognosis for squamous cell carcinoma is the status of the cervical lymph nodes. Metastasis to the regional lymph nodes reduces the 5-year survival rate by 50% compared with that of patients with early-stage disease. The American Cancer Society reports that 40% of patients with squamous carcinoma of the oral cavity and pharynx present with regional metastases to the cervical lymph nodes. This activity presents the causes, pathophysiology, indications, contraindications of head and neck cancer.
Objectives:
- Identify the anatomical structures in head and neck cancer dissection.
- Describe the indications for head and neck cancer surgery.
- Review the complications of head and neck surgery.
- Summarize the importance of care coordination among interprofessional team members to improve outcomes for patients undergoing head and neck surgery.
Introduction
Head and neck cancer is the sixth most common cancer worldwide.[1] The single most important factor affecting prognosis for squamous cell carcinoma is the status of the cervical lymph nodes. Metastasis to the regional lymph nodes reduces the 5-year survival rate by 50% compared with that of patients with early-stage disease. The American Cancer Society reports that 40% of patients with squamous carcinoma of the oral cavity and pharynx present with regional metastases to the cervical lymph nodes.[2] Therefore, the management of cervical lymph nodes is a vital component in the overall treatment plan for patients with squamous cell carcinoma of the head and neck. Head and neck surgery for cancer is a major undertaking with potentially enormous morbidity. Not every patient is a candidate for surgery and to avoid poor outcomes, it is important to select patients appropriately via a preoperative cardiac and pulmonary workup, in addition to their cancer staging. While surgery has demonstrated superior local control rates, overall survival remains similar with surgical versus non-surgical therapy for many head and neck cancers; the astute clinician must therefore tailor treatment to the individual patient to maximize the quality of life and post-treatment functionality. Removal of the cervical lymph nodes for oncologic reasons is termed a "neck dissection," and the surgery is tailored to address the lymph node basins at risk for metastatic spread depending on the site of the primary tumor.
Anatomy and Physiology
The classification of cervical lymph nodes is according to the system developed at Memorial Sloan-Kettering Cancer Center in the 1930s.[3][4] This system divides the lymph nodes in the lateral aspect of the neck into five nodal levels, I through V, as described below. The lymph nodes in the central compartment are in category level VI, and those in the superior anterior mediastinum are level VII. The clinical and surgical landmarks for neck node levels are:
1. Level I (submental triangle is level Ia and submandibular triangles are level Ib) borders are:
- Superior - the lower border of the body of the mandible;
- Posterior - posterior belly of digastric
- Inferior - hyoid bone
2. Level II (upper jugular lymph nodes - level IIa begins at the posterior border of the submandibular gland and extends to the accessory nerve, level IIb is the node-bearing tissue bordered anteriorly by the accessory nerve and posteriorly by the trapezius and suboccipital muscles) borders are:
- Superior - the base of the skull
- Posterior - posterior border of the sternocleidomastoid
- Anterior - lateral limit of sternohyoid
- Inferior-hyoid bone
3. Level III (middle jugular lymph nodes) borders are:
- Superior - hyoid bone
- Posterior - posterior border of the sternocleidomastoid
- Anterior - lateral limit of sternohyoid;
- Inferior - cricothyroid membrane
4. Level IV (lower jugular lymph nodes) borders are:
- Superior - cricothyroid membrane
- Posterior - posterior border of the sternocleidomastoid
- Anterior - lateral limit of sternohyoid
- Inferior - clavicle
5. Level V (posterior triangle of the neck, level Va is the tissue above the posterior belly of the omohyoid, and level Vb is the node-bearing tissue between the posterior belly of the omohyoid and the clavicle/thoracic inlet) borders are:
- Posterior - the anterior border of the trapezius
- Anterior - the posterior border of the sternocleidomastoid
- Inferior - clavicle
6. Level VI: (central compartment of the neck) borders are:
- Superior - hyoid bone;
- Inferior - suprasternal notch
- Lateral - medial border of the carotid sheath on either side
7. Level VII: (superior mediastinal lymph nodes) borders are:
- Superior - suprasternal notch
- Inferior - innominate artery
Indications
Before discussing the indications for neck dissection and the operative technique, it is essential to review the brief background, history, and types of neck dissection. The credit for neck dissection as a curative procedure for cervical metastases belongs to George Washington Crile from the Cleveland Clinic.[5] In 1900, he performed different types of neck dissections and subsequently described the classic operation of the radical neck dissection (RND) in his seminal article of 1905 published in the Transactions of the Southern Surgical and Gynecological Association. This operation is the basis of all neck dissections, with subsequent surgeries framed as modifications of this initial operation. Hayes Martin from Memorial Sloan-Kettering Cancer Center, who described the stepwise procedure of RND in his classic article in 1951, popularized this operation. However, this operative procedure is not without significant morbidity, as it results in a cosmetic deformity and dysfunction of shoulder movement due to en bloc resection of the accessory nerve, sternocleidomastoid muscle, internal jugular vein, and the tail of the parotid gland. Argentinian surgeon Oswaldo Suarez was the first to describe functional neck dissection in 1963, now called modified radical neck dissection (MRND). He described the removal of all five lymph node levels in the neck while preserving the spinal accessory nerve, sternocleidomastoid muscle, and internal jugular vein to limit any functional disability in the shoulder.[6] The types and indications of various types of neck dissection are as follows:
1. Radical neck dissection (RND): Lymph nodes from level I-V, ipsilateral sternocleidomastoid muscle (SCM), internal jugular vein (IJV), and spinal accessory nerve (SAN) undergo removal (the parotid tail is rarely included in modern RND). RND is indicated when there is bulky nodal disease in the neck with extensive soft tissue involvement due to extra-capsular spread.[7]
2. Modified radical neck dissection type I (MRND-I): Lymph nodes from level I-V, ipsilateral sternocleidomastoid muscle, and internal jugular vein are removed, with preservation of the spinal accessory nerve. Indications for MRND-I is in bulky nodal disease with extracapsular spread involving the SCM and IJ, where the accessory nerve is free of disease.
3. Modified radical neck dissection type II (MRND-II): Removal of lymph nodes from level I-V and ipsilateral sternocleidomastoid muscle, with preservation of IJV and accessory nerve. Indications for MRND-II include bulky nodal disease with SCM involvement but sparing the IJ or accessory nerve.
4. Modified radical neck dissection type III (MRND-III): Lymph nodes from level I-V undergo removal, with preservation of SCM, IJV, and SCM. MRND-III is indicated in metastatic disease with limited extracapsular spread and the IJ, SCM, and accessory nerve can all be dissected free.[8][9]
Indications:
1. Supraomohyoid neck dissection (SOHD): Lymph nodes removed are Levels I–II, with sparing of IJV, SCM, and accessory nerve. SOHD is indicated in the N0 neck for primary SCC or malignant melanoma where the primary site is anterior to the ear or is located in the lower eyelid (but should include parotidectomy for face and forehead/anterior scalp).
2. Selective neck dissection (SND): Removal of lymph nodes in levels Ib–IV, with sparing of IJV, SCM, and SAN. The procedure is indicated in N0 neck for SCC of the lateral tongue, oral cavity, anterior floor of mouth, or for N1 disease in these primary sites.[10]
3. Lateral neck dissection (also technically a selective neck dissection): Removal of lymph nodes from levels II-IV with sparing of IJV, SCM, and accessory nerve. Indications for this procedure are any N-stage neck without significant extracapsular spread for SCC of larynx and hypopharynx, for differentiated thyroid carcinoma, or for melanoma with a positive sentinel lymph node that drains to these nodal basins. Certain primary parotid malignancies also warrant this operation.
4. Postero-lateral neck dissection: Removal of levels II–V, suboccipital, retro-auricular nodes with sparing of IJV, SCM, and SAN. Indications for this procedure are any N-stage neck cutaneous melanoma with high-risk features or melanoma with a positive sentinel node where the primary site is posterior to the ear.
5. Modified radical neck dissection: As described above. This procedure has an indication for thyroid cancer and upper aerodigestive carcinomas with positive lateral neck nodes but limited extracapsular spread.[11]
Contraindications
There are no absolute contraindications to neck dissection beyond those that make a patient unfit for general anesthesia and resection, with one exception: unresectable disease. Relative contraindications include: [12][13]
- Severe cardiopulmonary disease, COPD with poor functional status
- Preoperative imaging showing deep infiltration of the tumor in the prevertebral space, scalene muscles, levator scapula muscle, phrenic nerve, and brachial plexus are not suitable candidates
- The primary tumor that is uncontrollable.
- Distant metastatic disease
- Tumor encasement of the carotid artery (NOTE: many authors view this as 'unresectable disease,' as resection and grafting does not confer a survival or local control advantage, even if it is technically possible)[14]
Absolute contraindication:
- Fixed neck mass in the deep neck muscles, prevertebral fascia, and/or skull base involvement (unresectable disease)
Equipment
A standard head and neck surgical pan should include all necessary instruments. Additional, specialized, instruments are at the surgeon's preference and can include McCabe nerve dissectors, nerve hooks, harmonic scalpels, 0.9mm forceps, Munion right-angle clamps, and many others.
Personnel
The surgical team comprises:
An operating surgeon, an assistant surgeon (resident/registrar, another surgeon, or a certified first-assistant), scrub nurse, circulating nurse, and the anesthetist.
Preparation
There are no specific preoperative preparatory requirements for patients undergoing neck dissection other than planning of the incisions for neck dissection, particularly if the primary tumor is undergoing resection simultaneously. Also, preparation of the neck dissection incisions must take into consideration any reconstructive effort required to repair the surgical defect created after the excision of the primary tumor. General endotracheal anesthesia is essential for performing a neck dissection, and the use of paralytic agents should be discussed between the surgeon and anesthetist. The patient placement is in the supine position with the head elevated to 30 degrees. The neck is hyper-extended with the use of a shoulder roll, and rotated to the opposite side.[15]
Technique or Treatment
Incision: There are many historical incisions including the Latyshevsky and Freund, Mac Fee, Crile, Kocher, Schobinger, and Hockey stick, but in modern head & neck surgery, the operation is performed via a single incision placed in an existing neck skin crease midway down the neck. Trifurcate incisions were popular in the past, and can still be used in the case of bulky posterior neck disease, but care should be taken to not place the trifurcation over the carotid artery.[16][17]
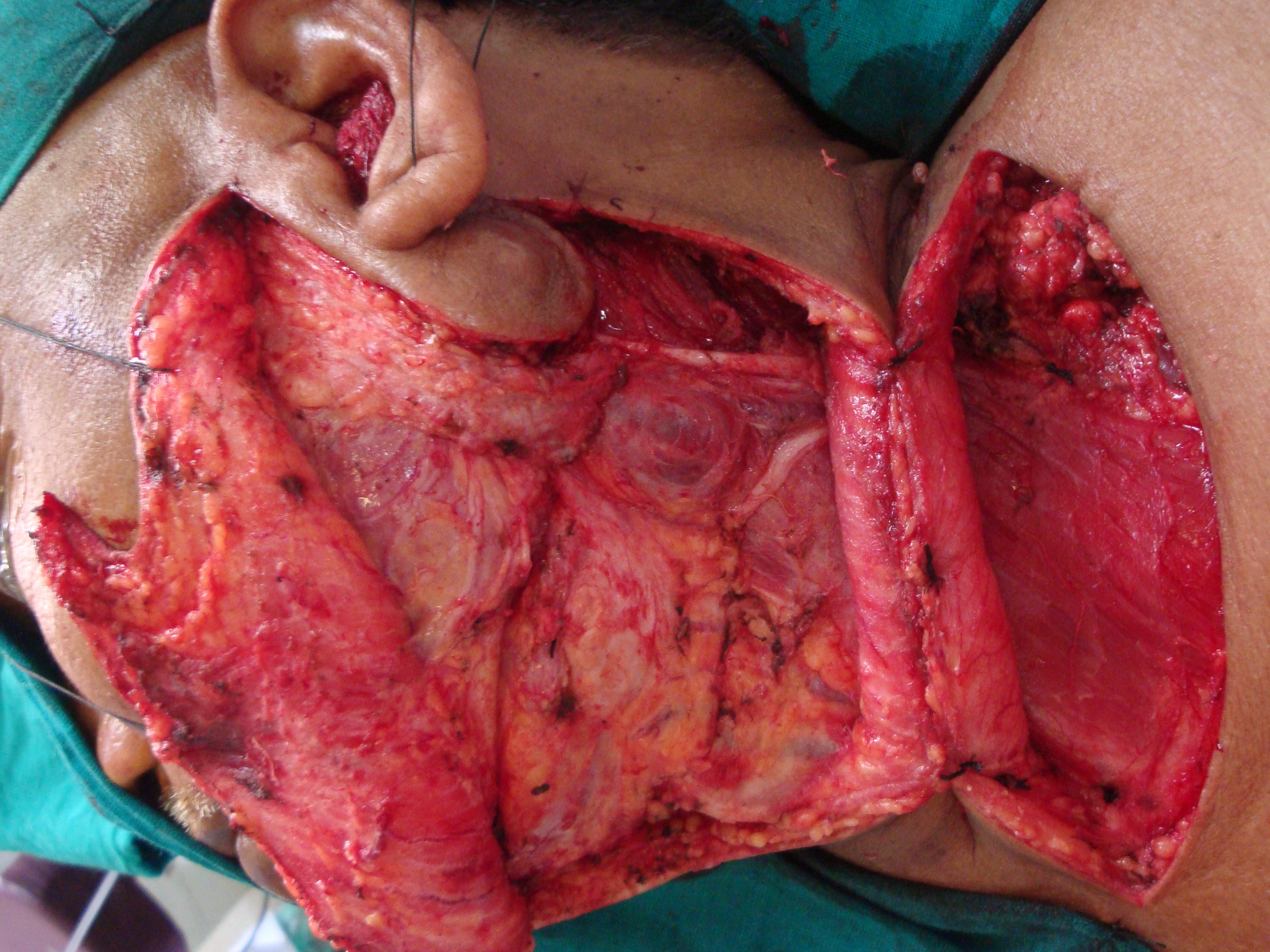
Raising skin flaps: The skin incision is deepened through the subcutaneous tissue and then through the platysma muscle. The posterior flap is then raised in the subplatysmal plane by applying traction to the flap with skin hooks and counter-traction of the deeper soft tissues. The flap is elevated up to the anterior border of the trapezius muscle. (Figure I).
Identifying Marginal mandibular nerve: Careful identification of the marginal mandibular branch of the facial nerve is crucial. Avoidance of paralytics is advocated at this point in the operation by some surgeons. Posteriorly, the greater auricular nerve and the external jugular vein overlying the sternocleidomastoid muscle come into view as the elevation of the flap continues. The greater auricular nerve and the external jugular vein should be identified carefully and preserved. We advise the use of the scalpel or scissors to dissect around the mandibular branch rather than electrocautery as it may cause temporary damage to the nerve. This nerve lies just anterior to the submandibular fascia and superficial to the posterior facial vein. The vein is ligated, and its upper stump retracted cephalad, protecting the marginal branch of the facial nerve (the Hayes Martin maneuver). Alternately, the facial vein and marginal mandibular nerves can be skeletonized and preserved individually. This can greatly increase vessel length available for microvascular reconstruction and should be discussed between the ablative and reconstructive surgeons preoperatively if it is oncologically sound to perform this dissection. The peri-facial nodes can be dissected out at this point if indicated.
Superior Dissection: The fibrous fatty tissue of the submental triangle is dissected off the anterior bellies of the digastric muscles and the mylohyoid. The fascia is then dissected off the anterior belly of the digastric muscle, and the specimen is retracted posteriorly, removing the fibrous fatty tissue containing lymph nodes lateral to the mylohyoid muscle. When the dissection reaches the posterior border of the mylohyoid, this is retracted anteriorly, exposing the lingual nerve and the submandibular gland duct are divided. Finally, the facial artery is ligated as it crosses forward, under the posterior belly of the digastric muscle. Alternately, the facial artery and vein can be dissected through the substance of the submandibular gland to increase the length of these vessels available for microvascular anastomosis, or if a submental flap is planned. The tail of the parotid gland is elevated off of the SCM and deep structures, and the sternocleidomastoid muscle is then incised close to its insertion in the mastoid process. The fibro-fatty tissue medial to the muscle is incised, exposing the splenius capitis and the levator scapulae muscles. Otherwise, incising the fascia below the digastric muscle and gentle inferior traction of the specimen allows identification of the hypoglossal nerve, the upper end of the internal jugular vein, and the spinal accessory nerve. At this point in the dissection, the internal jugular vein and the spinal accessory nerve are identified and preserved, reflecting the lymph node-bearing tissue inferiorly with the surgical specimen.
Inferior dissection: The dissection is continued posteriorly and inferiorly along the anterior border of the trapezius muscle. The spinal accessory nerve and the transverse cervical vessels are divided as they cross the anterior the border of the trapezius muscle. During this step of the operation, it is important to preserve the branches of the cervical plexus that innervate the levator scapulae muscle, unless the extent of the disease in the neck precludes it. The sternocleidomastoid muscle and the superficial layer of the deep cervical fascia are incised above the superior border of the clavicle. The omohyoid muscle is divided, and the external jugular vein can either be preserved or divided, depending upon the vascular needs of the reconstructive surgeon. The fibro-fatty tissue in this region is then gently pushed in an upward direction, exposing the brachial plexus, the scalenus anterior muscle, and the phrenic nerve (Fig. 1-6). Posteriorly, the dissection is continued to join the previous dissection along the anterior border of the trapezius.
Medial dissection: The dissection is continued medially to expose the vagus nerve, the common carotid artery, and the internal jugular vein. Inferiorly, the phrenic nerve is identified and protected by not violating the deep fascia of the floor of the neck overlying the brachial plexus and muscles. The surgeon must remain very vigilant on the left side to be able to identify thoracic duct, which arches downward and forward from behind the common carotid to open into the internal jugular vein, the subclavian vein, or the angle formed by the junction of these two vessels. The duct is located anterior or superficial to the anterior scalene muscle and the phrenic nerve. To prevent a chyle leak, the surgeon must also remember that the thoracic duct may have multiple connections at its upper end and that at the base of the neck it usually receives a jugular, a subclavian, and perhaps other minor lymphatic trunks, which must be individually ligated or clipped.
The internal jugular vein can almost always be spared with meticulous technique, but if resection is necessary, it is important to obtain circumferential control of the vessel proximally and distally with vessel loops before cross-clamping and dividing it. If the tumor mass is located low in the jugulodigastric region or the mid-jugular region, the internal jugular vein is first ligated and divided superiorly. The dissection then continues in an inferior direction, separating the specimen from the vagus nerve, the carotid artery, and the superior thyroid vessels. If instead, the disease is located high in the jugulodigastric region, the internal jugular vein is divided inferiorly, and the dissection continues in a superior direction along the common carotid artery; this is especially useful when the tumor is extensive and may require removal of the external carotid artery or the hypoglossal nerve. Mobilization of the surgical specimen from below allows easier dissection from the internal carotid artery and, if possible, the external carotid and the hypoglossal nerve.
Closure: Incision closure is in three layers: the first layer approximates the platysma anteriorly and the subcutaneous tissue laterally, and the second layer approximates the subcuticular layer. The skin can then be closed with sutures, staples, or dermal glue. One or two suction drains should remain in place, placed in the most dependent areas (the lateral gutter and inferior aspect near the thoracic inlet). The drain(s) should not rest immediately over the carotid artery or in the area of the thoracic duct, or atop any named nerve.
Complications
1. Infection.
2. Air leak.
3. Postoperative bleeding.
4. Chylous fistula. The reported incidence varies between 1% and 2.5%. Management depends on the time of onset of the fistula, on the amount of chyle drainage in 24 hours, and the presence or absence of accumulation of chyle under the skin flaps. When the daily output of chyle exceeds 600 mL in a day or 200 to 300 mL per day for 3 days, especially when the chyle fistula becomes apparent immediately after surgery, conservative closed wound management is unlikely to succeed; these are indications for surgical exploration.
5. Synchronous bilateral radical neck dissections, in which both internal jugular veins undergo ligation, can result in the development of facial edema, cerebral edema, or both; blindness; and hypoxia.
6. Carotid artery rupture. The most feared and often lethal complication after neck surgery is exposure and rupture of the carotid artery. Therefore, every effort must be made to prevent it. If the skin incisions have the proper design, the carotid seldom becomes exposed in the absence of a salivary fistula. If the carotid becomes exposed, it should be covered promptly with well-vascularized tissue.
7. The most notable sequelae observed in patients who have undergone a radical neck dissection are related to the removal of the spinal accessory nerve. The resulting denervation of the trapezius muscle causes destabilization of the scapula with progressive flaring at the vertebral border, drooping, and lateral and anterior rotation. The loss of trapezius function decreases the patient’s ability to abduct the shoulder above 90 degrees at the shoulder. These physical changes result in a syndrome of pain, weakness, and deformity of the shoulder girdle commonly associated with the radical neck dissection. Careful performing of a modified radical neck dissection greatly reduces the severity, likelihood, and duration of these complications.[18][19]
Clinical Significance
Currently, head and neck surgeons throughout the world use a variety of different cervical lymph node dissections for the surgical treatment of the neck in patients with cancer of the head and neck region. In contrast to the measured pace of refinements to the technique of neck dissection, the role of neck dissection in the management of regional disease across the entire gamut of histologies, from squamous cell carcinoma to cutaneous melanoma, to papillary thyroid carcinoma, is evolving rapidly.[20]
Enhancing Healthcare Team Outcomes
Strategies to improve the quality of head and neck cancer care do exist.[21][22]
The most important aspects of success involve interprofessional care of the patient. Nurses provide coordination of care, managing documentation, and follow-ups and reporting when untoward complications occur to the clinical team. The clinical team, assisted by the nursing staff, must make sure protocols are followed to avoid infections, hydration issues, and calorie intake. Interprofessional cooperation will assist in making sure patients obtain the best outcomes. Modern care of the cancer patient is by definition, multi-disciplinary. Tumor Boards, where all subspecialties and allied health practitioners meet to discuss and plan treatment for new cancer diagnoses are now the norm and the expectation.