[3]
Luigetti M, Ranieri F, Profice P, Pilato F, Capone F, Di Lazzaro V. Benedictine hand of 'central' origin. Emergency medicine journal : EMJ. 2013 Feb:30(2):173. doi: 10.1136/emermed-2012-201490. Epub 2012 May 28
[PubMed PMID: 22641767]
[4]
Futterman B. Analysis of the Papal Benediction Sign: The ulnar neuropathy of St. Peter. Clinical anatomy (New York, N.Y.). 2015 Sep:28(6):696-701. doi: 10.1002/ca.22584. Epub 2015 Jun 28
[PubMed PMID: 26118346]
[5]
Zdilla MJ. The Hand of Sabazios: Evidence of Dupuytren's Disease in Antiquity and the Origin of the Hand of Benediction. The journal of hand surgery Asian-Pacific volume. 2017 Sep:22(3):403-410. doi: 10.1142/S0218810417970012. Epub
[PubMed PMID: 28774258]
[6]
Soubeyrand M, Melhem R, Protais M, Artuso M, Crézé M. Anatomy of the median nerve and its clinical applications. Hand surgery & rehabilitation. 2020 Feb:39(1):2-18. doi: 10.1016/j.hansur.2019.10.197. Epub 2019 Dec 6
[PubMed PMID: 31816428]
[7]
Ko JW, Mirarchi AJ. Late reconstruction of median nerve palsy. The Orthopedic clinics of North America. 2012 Oct:43(4):449-57. doi: 10.1016/j.ocl.2012.07.014. Epub
[PubMed PMID: 23026460]
[8]
Soldado F, Ghizoni MF, Bertelli JA. The ulnar nerve consistently drives flexion of the middle finger. The Journal of hand surgery, European volume. 2014 Feb:39(2):211-2. doi: 10.1177/1753193413505581. Epub 2013 Sep 13
[PubMed PMID: 24038536]
[9]
Bertelli JA, Soldado F, Lehn VL, Ghizoni MF. Reappraisal of Clinical Deficits Following High Median Nerve Injuries. The Journal of hand surgery. 2016 Jan:41(1):13-9. doi: 10.1016/j.jhsa.2015.10.022. Epub
[PubMed PMID: 26710729]
[10]
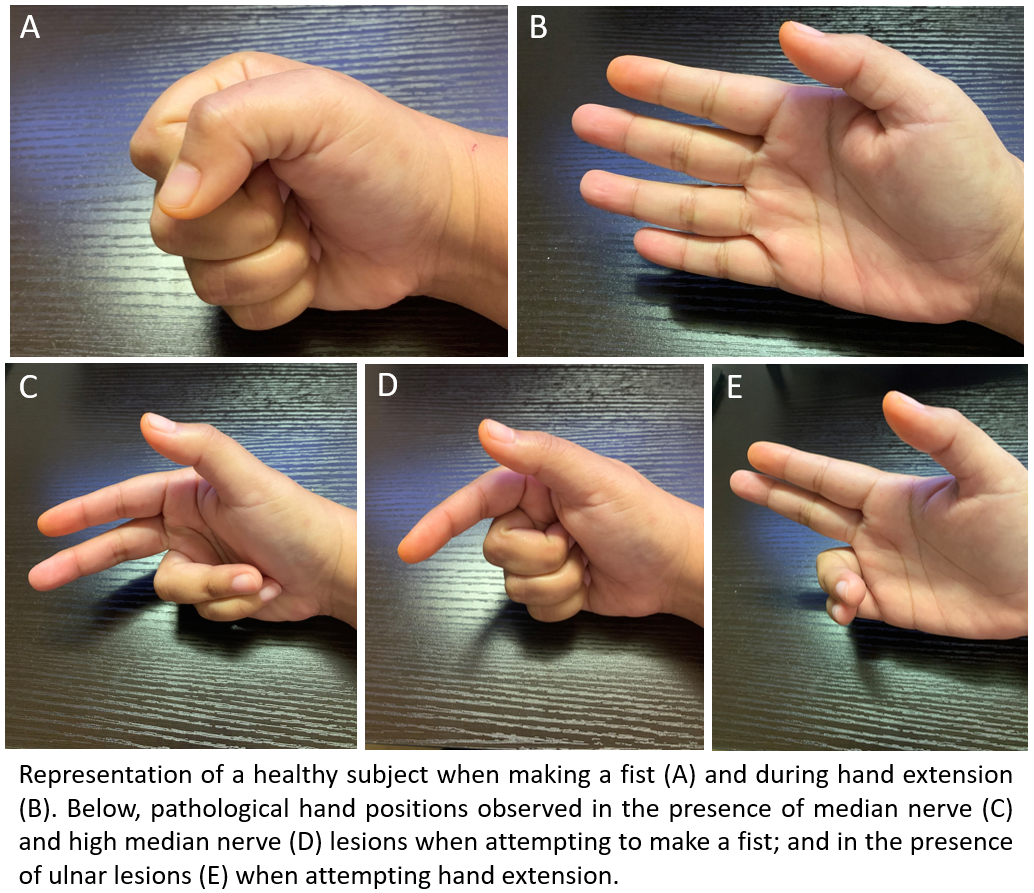
Duraku LS, Schreuders TAR, Power DM, Rajaratnam V, Chaudhry T, Hundepool CA, Zuidam JM. High Median Nerve Paralysis: Is the Hand of Benediction or Preacher's Hand A Correct Sign? Plastic and reconstructive surgery. Global open. 2022 Oct:10(10):e4598. doi: 10.1097/GOX.0000000000004598. Epub 2022 Oct 28
[PubMed PMID: 36320624]
[14]
Adler JA, Wolf JM. Proximal Median Nerve Compression: Pronator Syndrome. The Journal of hand surgery. 2020 Dec:45(12):1157-1165. doi: 10.1016/j.jhsa.2020.07.006. Epub 2020 Sep 4
[PubMed PMID: 32893044]
[15]
Küçükakkaş O, Yurdakul OV. The diagnostic value of clinical examinations when diagnosing carpal tunnel syndrome assisted by nerve conduction studies. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2019 Mar:61():136-141. doi: 10.1016/j.jocn.2018.10.106. Epub 2018 Nov 3
[PubMed PMID: 30396816]
[16]
Campbell WW, Pridgeon RM, Riaz G, Astruc J, Sahni KS. Variations in anatomy of the ulnar nerve at the cubital tunnel: pitfalls in the diagnosis of ulnar neuropathy at the elbow. Muscle & nerve. 1991 Aug:14(8):733-8
[PubMed PMID: 1653898]
[17]
Schuppe V. Ulnar claw: A kinder, gentler solution. Journal of hand therapy : official journal of the American Society of Hand Therapists. 2020 Jan-Mar:33(1):140-145. doi: 10.1016/j.jht.2018.08.002. Epub 2019 Mar 8
[PubMed PMID: 30857894]
[19]
Aswani Y, Saifi S. Atraumatic Main-En-Griffe due to Ulnar Nerve Leprosy. Polish journal of radiology. 2016:81():1-4. doi: 10.12659/PJR.894850. Epub 2016 Jan 1
[PubMed PMID: 26788223]
[20]
Wu WT, Chang KV, Hsu YC, Tsai YY, Mezian K, Ricci V, Özçakar L. Ultrasound Imaging and Guidance for Distal Peripheral Nerve Pathologies at the Wrist/Hand. Diagnostics (Basel, Switzerland). 2023 May 31:13(11):. doi: 10.3390/diagnostics13111928. Epub 2023 May 31
[PubMed PMID: 37296780]