Introduction
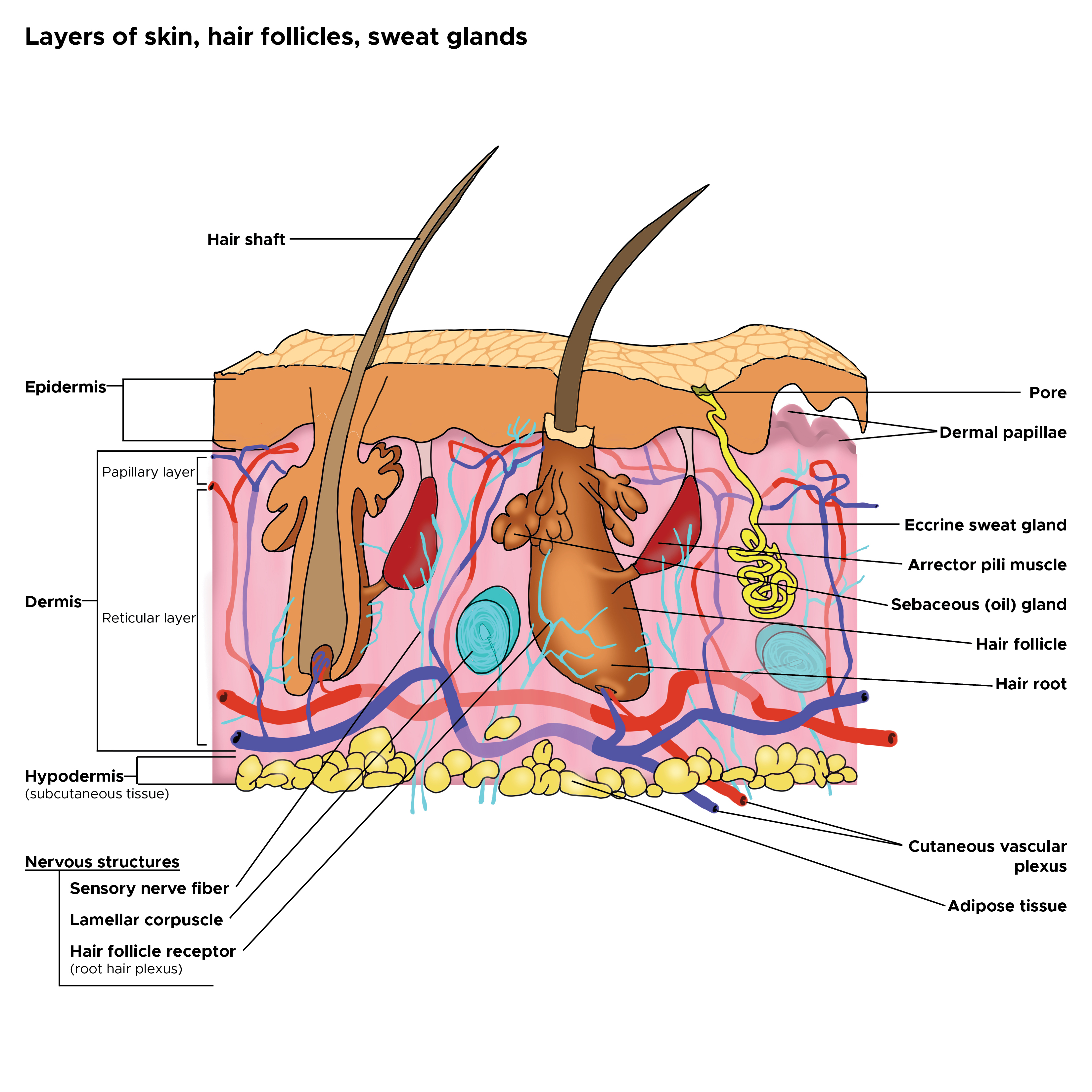
Skin is the largest organ in the body and covers the body's entire external surface. It is made up of three layers, the epidermis, dermis, and the hypodermis, all three of which vary significantly in their anatomy and function. The skin's structure is made up of an intricate network which serves as the body’s initial barrier against pathogens, UV light, and chemicals, and mechanical injury. It also regulates temperature and the amount of water released into the environment. This article discusses the relevant anatomical structures of the skin’s epidermal layer, its structure, function, embryology, vascular supply, innervation, surgical considerations, and clinical relevance.
Skin Thickness
The thickness of each layer of the skin varies depending on body region and categorized based on the thickness of the epidermal and dermal layers (see Illustration. Cross Section, Layers of the Skin). Hairless skin found in the palms of the hands and soles of the feet is thickest because the epidermis contains an extra layer, the stratum lucidum. The upper back is considered thickest based on the thickness of the dermis, but it is considered “thin skin” histologically because the epidermal thickness lacks the stratum lucidum layer and is thinner than hairless skin.
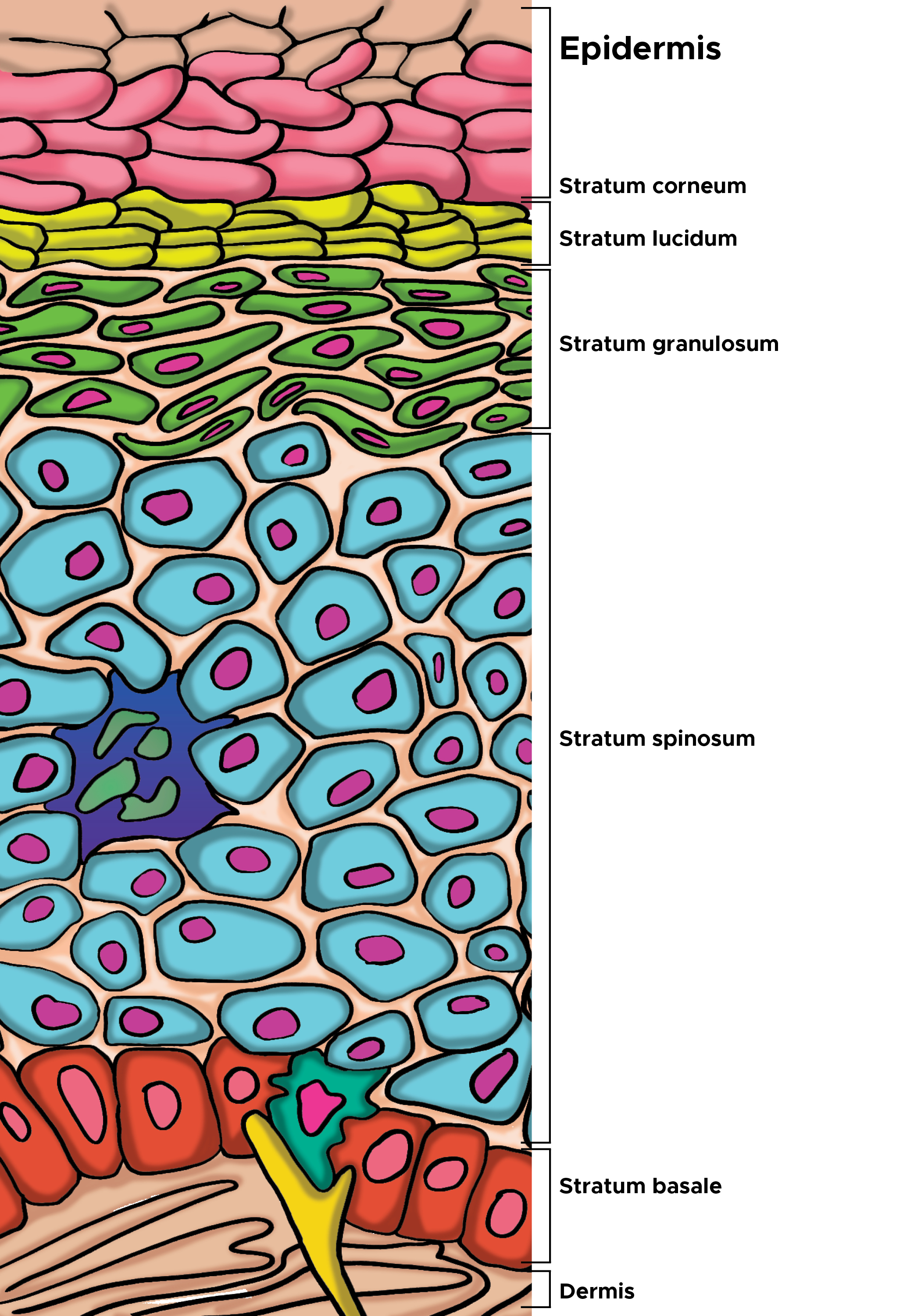
Layers of Epidermis
The layers of the epidermis include the stratum basale (the deepest portion of the epidermis), stratum spinosum, stratum granulosum, stratum lucidum, and stratum corneum (the most superficial portion of the epidermis).
Stratum basale, also known as stratum germinativum, is the deepest layer, separated from the dermis by the basement membrane (basal lamina) and attached to the basement membrane by hemidesmosomes. The cells found in this layer are cuboidal to columnar mitotically active stem cells that are constantly producing keratinocytes. This layer also contains melanocytes.
Stratum spinosum, 8-10 cell layers, also known as the prickle cell layer contains irregular, polyhedral cells with cytoplasmic processes, sometimes called “spines”, that extend outward and contact neighboring cells by desmosomes. Dendritic cells can be found in this layer.
Stratum granulosum, 3-5 cell layers, contains diamond shaped cells with keratohyalin granules and lamellar granules. Keratohyalin granules contain keratin precursors that eventually aggregate, crosslink, and form bundles. The lamellar granules contain the glycolipids that get secreted to the surface of the cells and function as a glue, keeping the cells stuck together.
Stratum lucidum, 2-3 cell layers, present in thicker skin found in the palms and soles, is a thin clear layer consisting of eleidin which is a transformation product of keratohyalin.
Stratum corneum, 20-30 cell layers, is the uppermost layer, made up of keratin and horny scales made up of dead keratinocytes, known as anucleate squamous cells. This is the layer which varies most in thickness, especially in callused skin. Within this layer, the dead keratinocytes secrete defensins which are part of our first immune defense.
Cells of the Epidermis
- Keratinocytes
- Melanocytes
- Langerhans’ cells
- Merkel’s cell (see Illustration. Illustration of the Cells of the Epidermis)
Keratinocytes
Keratinocytes are the predominant cell type of epidermis and originate in the basal layer, produce keratin, and are responsible for the formation of the epidermal water barrier by making and secreting lipids. Keratinocytes also regulate calcium absorption by the activation of cholesterol precursors by UVB light to form vitamin D.
Melanocytes
Melanocytes are derived from neural crest cells and primarily produce melanin, which is responsible for the pigment of the skin. They are found between cells of stratum basale and produce melanin. UVB light stimulates melanin secretion which is protective against UV radiation, acting as a built-in sunscreen. Melanin is produced during the conversion of tyrosine to DOPA by the enzyme tyrosinase. Melanin then travels from cell to cell by a process that relies on the long processes extending from the melanocytes to the neighboring epidermal cells. Melanin granules from melanocytes are transferred via the long processes to the cytoplasm of basal keratinocyte. Melanin transferred to neighboring keratinocytes by “pigment donation”; involves phagocytosis of tips of melanocyte processes by keratinocytes.
Langerhans’ Cells
Langerhans cells, dendritic cells, are the skins first line defenders and play a significant role in antigen presentation. These cells need special stains to visualize, primarily found in the stratum spinosum. These cells are the mesenchymal origin, derived from CD34 positive stem cells of bone marrow and are part of the mononuclear phagocytic system. They contain Birbeck granules, tennis racket shaped cytoplasmic organelles. These cells express both MHC I and MHC II molecules, uptake antigens in skin and transport to the lymph node.
Merkel Cells
Merkel cells are oval-shaped modified epidermal cells found in stratum basale, directly above the basement membrane. These cells serve a sensory function as mechanoreceptors for light touch, and are most populous in fingertips, though also found in the palms, soles, oral, and genital mucosa. They are bound to adjoining keratinocytes by desmosomes and contain intermediate keratin filaments and their membranes interact with free nerve endings in the skin.
Dermis
The dermis is connected to the epidermis at the level of the basement membrane and consists of two layers, of connective tissue, the papillary and reticular layers which merge together without clear demarcation. The papillary layer is the upper layer, thinner, composed of loose connective tissue and contacts epidermis. The reticular layer is the deeper layer, thicker, less cellular, and consists of dense connective tissue/ bundles of collagen fibers. The dermis houses the sweat glands, hair, hair follicles, muscles, sensory neurons, and blood vessels.
Hypodermis
The hypodermis is deep to the dermis and is also called subcutaneous fascia. It is the deepest layer of skin and contains adipose lobules along with some skin appendages like the hair follicles, sensory neurons, and blood vessels.[1][2][3][4][5][6]
Structure and Function
The skin has many functions. It serves as a barrier to water, invasion by microorganisms, mechanical and chemical trauma, and damage from UV light. The epidermal water barrier established by the cell envelop, a layer of insoluble proteins on the inner surface of the plasma membrane. It is formed by cross-linking of small proline-rich proteins and larger proteins like cystatin, desmoplakin, filaggrin and contributes to strong mechanics of barrier. And the lipid envelope, a lipid/hydrophobic layer attached to the outer surface of the plasma membrane. As keratinocytes in stratum spinosum produce keratohyalin granules, they also produce lamellar bodies (containing a mixture of glycosphingolipids, phospholipids, and ceramides) assembled within Golgi. Lamellar bodies’ contents are then secreted by exocytosis into extracellular spaces between the stratum granulosum and corneum. Skin is the first site of immunological defense by the action of the Langerhans cells in the epidermis which are dendritic epidermal T lymphocytes and part of the adaptive immune system. The skin preserves the bodies homeostasis by regulating temperature and water loss, while also serving both endocrine and exocrine functions. The endocrine functions include the production of vitamin D in the keratinocytes which are responsible for converting 7-dehydrocholesterol in the epidermis to vitamin D, with the assistance of UV light from the sun. The keratinocytes express the vitamin D receptor (VDR) and also contain the enzymes needed to convert vitamin D to its active form of 1, 25 dihydroxy vitamin D. The significance of the VDR is that stimulation of it plays a role in the proliferation of the stratum basale and differentiation of keratinocytes as they move upwards in the epidermis. The exocrine functions of the skin are by way of the sweat and sebaceous glands. Another important role of the skin is a sensation to touch, heat, cold, and pain by the actions of the nociceptors. The general appearance, turgor, and other qualities also give insight into the general health of the body. [7][8][9][10]
Embryology
The epidermis is derived from ectodermal tissue. The dermis and hypodermis are derived from mesodermal tissue from somites. The mesoderm is also responsible for the formation of Langerhans cells. Neural crest cells, responsible for specialized sensory nerve endings and melanocyte formation migrate into the epidermis during epidermal development.[11][12]
Blood Supply and Lymphatics
Blood vessels and lymphatic vessels are found in the dermal layer of the skin. Blood supply to the skin is an arrangement of two plexuses, the first lies between the papillary and reticular layers of the dermis and the second lie between the dermis and subcutaneous tissues. Supply to the epidermis is by way of the superficial arteriovenous plexus (subepidermal/papillary plexus). These vessels are important for temperature regulation. The mechanism by which the body regulates temperature through the skin is very effective and works by increased blood flow to the skin, transferring heat from the body to the environment. The changes in blood flow are controlled by the autonomic nervous system, sympathetic stimulation resulting in vasoconstriction (heat retention) and while vasodilation results in heat loss. Vasodilation of the blood vessels is the response to increased body temperature and is the result of inhibition of the sympathetic centers in the posterior hypothalamus whereas decreased body temperature will cause vasoconstriction of skin blood vessels.[13][14]
Nerves
Nerves of the skin include both somatic and autonomic nerves. The somatic sensory system is responsible for pain (nociceptors), temperature, light touch, discriminative touch, vibration, pressure, and proprioception medicated primarily by specialized cutaneous receptors/end organs including Merkel disks, Pacinian corpuscles, Meissner’s corpuscles, and Ruffini corpuscles. The autonomic innervation is responsible for the control of the tone of the vasculature, pilomotor stimulation at the hair root, and sweating. The free nerve endings extend into the epidermis and sense pain, heat, and cold. They are most numerous in the stratum granulosum layer and surround most hair follicles. Merkel disks sense light touch and reach the stratum basale layer. The other nerve endings are found in the deeper portions of the skin and include the Pacinian corpuscle which senses deep pressure, Meissner’s corpuscle which senses low-frequency stimulation at the level of the dermal papillae, and Ruffini corpuscles which sense pressure.[15][16][17]
Muscles
The arrector pili muscles are bundles of smooth muscle fibers that attach to the connective tissue sheath of hair follicles. When the muscles contract, they pull the hair follicle outward resulting in the hair erecting up but also compresses the sebaceous glands, resulting in the secretion of their contents. Hair does not exit perpendicularly, but instead at an angle. This erection of hair also produces goosebumps, the bumpy appearance of the skin. [18]
Physiologic Variants
Skin is continuously shedding and desquamating and varies slightly depending on the body region. There are more layers of cells in thicker hairless skin with an additional layer, known as the stratum lucidum. Overall, the process of cell division, desquamation, and shedding go as follows:
- Cell division occurs in stratum basale/germinativum. One cell remains, another cell is pushed toward the surface. Basal cells begin synthesis of tonofilaments (composed of keratin) which are grouped into bundles (tonofibrils).
- Cells are pushed into stratum spinosum. In the upper part of the spinous layer, cells begin to produce keratohyalin granules having intermediate-associated proteins, filaggrin, and trichohyalin; helps aggregate keratin filaments and conversion of granular cells to cornified cells, i.e. keratinization. Cells also produce lamellar bodies.
- Cells are pushed into stratum granulosum and become flattened and diamond shaped. The cells accumulate keratohyalin granules mixed between tonofibrils.
- Cells continue to stratum corneum where they flatten and lose organelles and nuclei. The keratohyalin granules turn tonofibrils into a homogenous keratin matrix.
- Finally, cornified cells reach the surface and are desquamated via a break-down of desmosomes. Proteinase activity of KLK (kallikrein-related serine peptidase) is triggered by lowered pH near the surface.[19][20]
Surgical Considerations
Langer’s Lines, also known as cleavage lines, are topological lines used to define the tension of the skin, corresponding to the alignment of collagen and elastic fibers in the reticular dermis. Surgical incisions made along these lines, less scarring will occur. [21]
Clinical Significance
There are numerous clinically significant aspects of the skin, including the dermatomes of the skin, skin segments divided based on the afferent nerves they are supplied by which are numbered according to the level of spinal vertebral from which they arise. There are seven cervical, twelve thoracic, five lumbar, and five sacral. Certain diseases like shingles, caused by varicella-zoster infection, have pain sensation and eruptive rashes that involve a dermatomal distribution. Dermatomes are useful in the diagnosis of vertebral spinal injury levels. Aside from the dermatomes, the cells of the epidermis are susceptible to neoplastic changes resulting in various cancer types. Some autoimmune and immunological diseases target the desmosomes and hemidesmosomes founds in the epidermis. Certain infections can also disrupt the integrity of the epidermis along with drug reactions that present variably as well.
Squamous cell carcinoma is cancer that arises from mutated keratinocytes, usually due to UV damage in individuals with Type I or II skin types (light skin, blue or green eyes, red or blonde hair, burn and never tan) and often appear as scaly, flaky, thick red patches that may bleed or even appear wart-like. This type of skin cancer can metastasize. Squamous cell carcinoma may arise from actinic keratosis, which is also caused by sun damage to the epidermal layer of skin and may have cutaneous horns. Basal cell carcinoma is a cancer of the basal layers of the epidermis and is much less likely to metastasize. This type of skin cancer is more common in sun-exposed areas and often appear are pearly papules on the face, with telangiectasias and ulcerate easily. Melanomas are cancers of the melanocytes and have a high metastatic potential, significantly mediated by the depth of the lesion. Melanomas can be found anywhere on the body, are usually irregularly pigmented but can be amelanotic. Langerhans Cell Histiocytosis is a type of cancer where Langerhans cells accumulate in the body and result in the formation of granulomas, often in the bones, resulting in bone pain. These granulomas can also appear in the skin like rashes, erythematous papules or blisters (see Image. Histology, Trichodysplasia spinulosa). An interesting association with this condition is the effect of the pituitary gland, which can be affected and individuals may present with diabetes insipidus, infertility, or other endocrine diseases due to insufficient hormones. Other serious and deadly complications are due to pancytopenia (anemia, thrombocytopenia, leukocytopenia) as a direct response to overcrowding by the Langerhans cells. Merkel cell carcinoma is an uncommon cancer of the Merkel cells and is categorized as neuroendocrine small cell carcinoma
Pemphigus vulgaris is an autoimmune disease that targets the intercellular proteins, desmosomes, that connect the keratinocytes to each other. Blisters form within the epidermis and are easily ruptured, resulting in acantholysis histologically. This disease is associated with a positive nikolsky sign, peeling away from the epidermis with rubbing of that area. Bullous Pemphigoid is another blistering disease that results in tense subepidermal blisters in older populations, that are due to antibodies that target the hemidesmosomes that connect the epidermis at the level of the basement membrane to the extracellular matrix of the dermis. This condition is not acantholytic and is not associated with a positive nikolsky sign.
Infections that affect the integrity of the skin include scalded skin syndrome caused by the exfoliative toxin released by staphylococcal aureus bacteria infection. This infection results in peeling away of the skin, positive nikolsky, an appearance of a severe burn (very red), and fever. Drug reactions like DRESS syndrome, erythema multiforme, Stevens-Johnsons syndrome, and Toxic Epidermal Necrolysis syndrome are often associated with certain medications that include sulfa-containing drugs, NSAIDs, and anti-seizure medications. [22][23][24][25][26][27][28][29]
Other Issues
The epidermal layer of skin contains much of our normal flora and the microbiome of the epidermis varies based on the body region. The microorganisms that inhabit our skin surface is nonpathogenic and can be commensal or mutualistic in nature. The bacteria that tend to predominate are staphylococci epidermidis, aureus, cutibacterium acnes, Corynebacterium, Streptococcus, candida and clostridium perfringens. When the protective skin barrier is altered, an infection can occur. [30]