Continuing Education Activity
Unstable angina is a form of chest pain caused by insufficient blood flow and oxygen supply to the heart. This condition is part of the acute coronary syndrome spectrum, which can lead to more severe heart conditions such as myocardial infarction (heart attack). Unstable angina is often characterized by chest discomfort that occurs unpredictably or at rest, making it more concerning than stable angina. This condition represents a medical emergency requiring immediate evaluation and management to prevent further cardiac damage. Given its prevalence and the potential for life-threatening complications, accurately diagnosing and distinguishing unstable angina from other causes of chest pain, such as stable angina or non-cardiac conditions, is critical for effective treatment.
In this course, participants learn the essentials of evaluating and managing unstable angina, emphasizing distinguishing it from other types of chest pain. The course underscores the role of timely diagnosis, appropriate diagnostic tools, and evidence-based treatment strategies to improve patient care. Collaboration within an interprofessional team—including cardiologists, emergency clinicians, nurses, and other healthcare professionals—ensures comprehensive care, enhances clinical decision-making, and leads to better patient outcomes. By working together, clinicians can promptly identify and treat unstable angina, reducing the risk of complications and improving survival rates.
Objectives:
Differentiate unstable angina from other causes of chest pain, such as stable angina and non-cardiac conditions.
Screen patients effectively using appropriate diagnostic tools to detect unstable angina.
Assess the risk factors and clinical indicators that may lead to the progression of unstable angina to myocardial infarction.
Collaborate care coordination among the interprofessional team to improve outcomes for patients affected by unstable angina.
Introduction
Unstable angina falls under the umbrella term "acute coronary syndrome." This public health issue affects a large portion of the population and remains the leading cause of death worldwide. Distinguishing between this condition and other causes of chest pain that include stable angina is important regarding the treatment and disposition of the patient. Clinicians should be aware of the signs and symptoms of acute coronary syndrome as patients rely on healthcare professionals to make the distinction from other causes of chest pain. Patients will often present to the emergency room; however, acute coronary syndrome can be seen in the outpatient setting as well. Over the years, a significant amount of research has been conducted to determine the appropriate and most effective treatment modalities and the diagnostic tools necessary for successfully managing unstable angina and other variants of acute coronary syndrome.[1][2][3]
Etiology
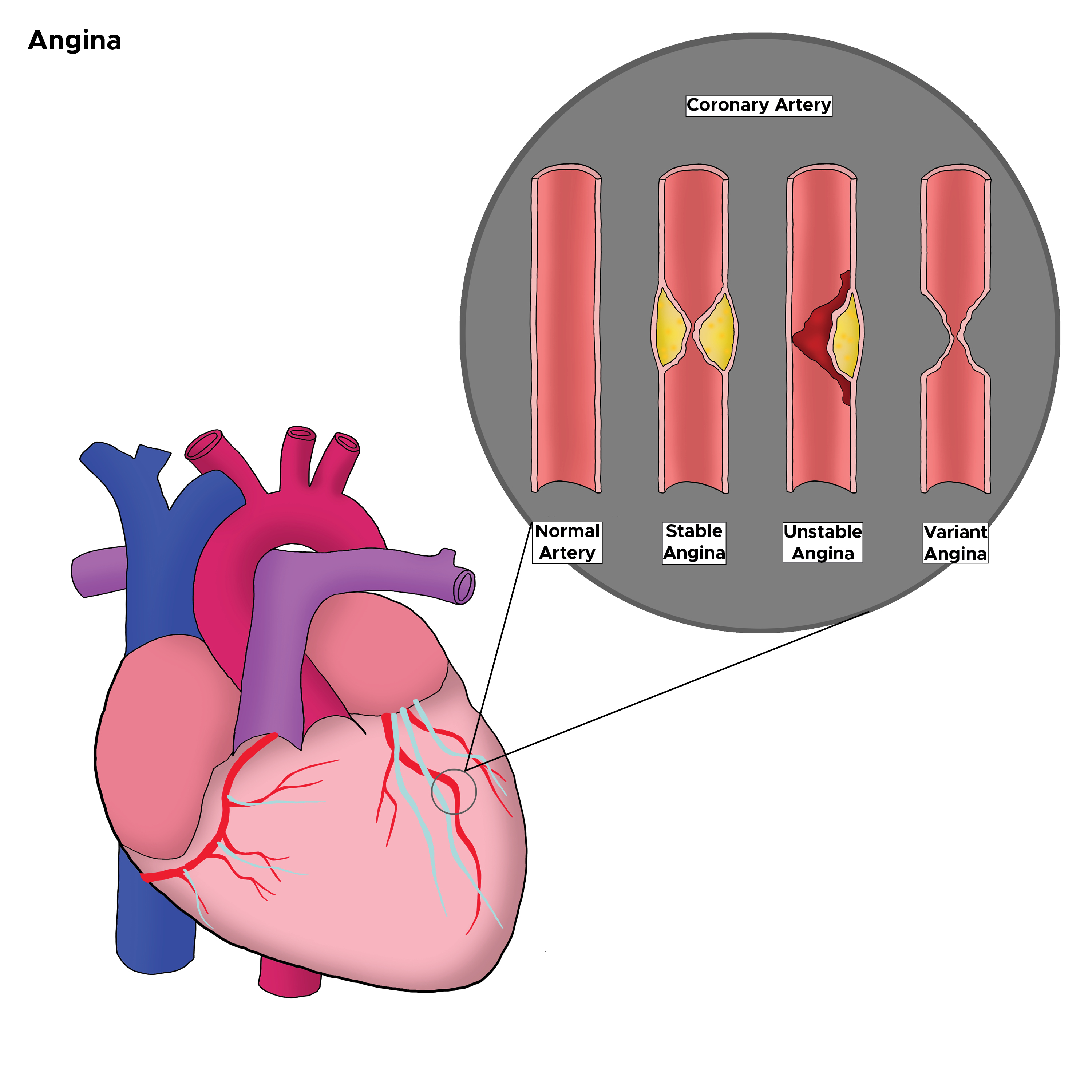
Coronary atherosclerotic disease is the underlying cause of unstable angina in nearly all patients with acute myocardial ischemia. The most common cause of unstable angina is due to coronary artery narrowing from a nonocclusive thrombus that develops on a disrupted atherosclerotic plaque. A less common cause is vasospasm of a coronary artery (eg, variant Prinzmetal angina). Endothelial or vascular smooth dysfunction causes this vasospasm (see Image. Types of Angina in the Coronary Artery).[4]
Epidemiology
Coronary artery disease affects a large portion of the population. There is an estimation that coronary artery disease causes more than a third of deaths in people aged 35 and older; this condition is the leading cause of death in this particular age group. Roughly 18 million individuals in the United States alone are believed to be affected by this disease. The incidence is higher in men, but as individuals surpass 75, the incidence of men and women becomes similar. Other risk factors include:
- Obesity
- Diabetes
- Hypertension
- High cholesterol
- Smoking history
- Cocaine or amphetamine abuse
- Family history
- Chronic kidney disease
- Human immunodeficiency syndrome
- Autoimmune disorders
- Anemia [5]
The mean age of presentation is 62, and women tend to be older than men at the time of presentation, while Black individuals tend to present at a younger age.
Pathophysiology
Unstable angina occurs when blood flow to the myocardium is obstructed, leading to inadequate perfusion. Blood supply to the heart begins in the aorta and flows into the coronary arteries, which branch into smaller vessels to nourish specific areas of the heart. The left coronary artery divides into the circumflex and left anterior descending arteries, while the right coronary artery splits into smaller branches. Unstable angina commonly results from intraluminal plaque formation, thrombosis, vasospasm, or elevated blood pressure. Frequently, a combination of these factors contributes to reduced blood flow, triggering symptoms of unstable angina. Factors that increase myocardial oxygen demand include:
- Arrhythmias
- Fever
- Hypertension
- Cocaine use
- Aortic stenosis
- Arteriovenous shunts
- Anemia
- Thyrotoxicosis
- Pheochromocytoma
- Congestive heart failure
History and Physical
Patients will often present with chest pain and shortness of breath. The chest pain will usually be described as pressure-like, although not necessarily limited to this description. Tightness, burning, and sharp types of pain can be defined. Often, patients will report discomfort as opposed to actual pain. The pain often radiates to the jaw or arms, affecting both the left and right sides. Constitutional symptoms such as nausea, vomiting, diaphoresis, dizziness, and palpitations may also be present. Exertion may worsen pain, and rest can ease the pain; nitroglycerin and aspirin administration may also improve the pain.
A key distinguishing feature of unstable angina is that the pain may not fully resolve with typical relieving factors. Many patients with unstable angina have pre-existing coronary artery disease, either previously diagnosed or with symptoms they have experienced for some time. These patients may report a noticeable increase in the frequency, duration, or severity of chest pain episodes. Such changes point to unstable angina as the likely diagnosis rather than stable angina or other causes of chest pain. Recognizing these symptoms is critical, as they may indicate an impending myocardial infarction or ST-elevation myocardial infarction (STEMI), requiring urgent evaluation due to the higher risk of morbidity and mortality compared to stable angina.The exam will likely be standard, although the patient may be clutching at their chest, sweating, or have
labored breathing; their heart sounds may be tachycardic, and rales may be heard due to pulmonary edema. Findings suggestive of a high-risk situation include:
- Dyskinetic apex
- Elevated jugular venous pressure
- Presence of third or fourth heart sounds (S3 or S4)
- New apical systolic murmur
- The presence of rales and crackles
- Hypotension
Evaluation
When a patient presents, they should be evaluated quickly with an electrocardiogram (ECG) to assess for ischemic signs or possible STEMI. The ECG in unstable angina may show hyperacute T-wave, flattening of the T-waves, inverted T-waves, and ST depression. ST elevations indicate STEMI, and these patients should be treated with percutaneous coronary intervention or thrombolytics while they wait for the availability of a catheterization lab. Any arrhythmias may be present in acute coronary syndrome, including junctional rhythms, sinus tachycardia, ventricular tachycardia, ventricular fibrillation, and left bundle branch block. However, most commonly, the patient will be in sinus rhythm, especially in unstable angina, as opposed to infarcted tissue.
The patient’s lab work should include a complete blood count to evaluate for anemia and platelet count and a basic metabolic profile to check for electrolyte abnormalities. A troponin test is essential to assess for myocardial infarction. A pro-brain natriuretic peptide test may also be performed, as elevated levels are linked to higher mortality. Coagulation studies are recommended if anticoagulation is planned or anticipated. A chest x-ray is often helpful to assess heart size and the mediastinum, allowing the clinician to screen for aortic dissection or other potential causes of chest pain.The history should be screened for other emergent causes of chest pain, shortness of breath, pulmonary embolism, aortic dissection, esophageal rupture, pneumonia, and pneumothorax. The patient should be kept on a cardiac monitor to evaluate for any rhythm changes. Further testing may include any number of cardiac stress tests (eg, walking treadmill stress test, stress echocardiogram, myocardial perfusion imaging, cardiac computed tomography/magnetic resonance imaging, or the gold standard—cardiac catheterization). These tests are typically ordered and performed by inpatient and primary care clinicians, but with the growth of observation medicine, emergency medicine clinicians may order these.[6][7]
Acute coronary syndrome risk assessment:
- Prior myocardial infarction or known history of coronary artery disease
- Transient ECG or hemodynamic changes during chest pain
- Chest, neck, or left arm with documented angina
- ST depression or elevation of more than 1 mm
- Marked symmetrical T-wave inversion
Treatment / Management
The mainstay of treatment focuses on improving perfusion of the coronary arteries, which can be performed in several ways.
Aspirin
Patients are often treated with aspirin for its antiplatelet therapies (162-325 mg orally or 300 mg rectally if the patient cannot swallow). The aspirin should be administered within 30 minutes.
Nitroglycerin
Nitroglycerin comes in several forms (intravenous, sublingual, transdermal, orally) and improves perfusion by vasodilating the coronaries, allowing improved blood flow and blood pressure. This decreases the amount of work the heart has to perform, which reduces its energy demand.
Clopidogrel
Clopidogrel is an option for patients who cannot tolerate aspirin. Prasugrel is more effective than clopidogrel but is associated with a higher risk of bleeding. Recently, ticagrelor and aspirin have been approved to reduce the rate of thrombotic cardiac events.
Supplemental Oxygen
Supplemental oxygen should also be given via nasal cannula to maintain appropriate oxygen saturation. These 3 actions are the quickest and most important functions to evaluate and treat unstable angina. The patient's response should be assessed in patients with continued pain or longer recovery time because they are at much higher risk for myocardial infarction.
Other Therapies
Other potential therapies include:
- Heparin: Either low- or high-molecular-weight heparin for anticoagulation
- Beta-blockers: Can decrease the energy demand by reducing blood pressure and heart rate [1][8][9]
- Ranolazine: Studied in patients with unstable angina; significant reduction in the endpoint of recurrent ischemia in the ranolazine group [10]
- Statins: Used in patients with unstable angina, validated by many trials
Cardiac angiography is indicated in unstable angina if the patient has:
- Cardiogenic shock
- Depressed ejection fraction
- Angina refractory to pharmacological therapy
- New mitral regurgitation
- Unstable arrhythmias
Early percutaneous coronary intervention in non-STEMI (eg, within 6 hours) has been shown to have lower mortality than those who undergo delayed percutaneous coronary intervention.
Differential Diagnosis
The differential diagnoses for instable angina include the following:
- Aortic dissection
- Pericarditis
- Pneumothorax
- Pulmonary embolism
- Peptic ulcer disease
Prognosis
The critical complications of unstable angina include:
- Myocardial infarction
- Stroke
- Death
Study results show that patients with new-onset ST-segment elevation (>1 mm) have a 12-month rate of myocardial infarction or death of about 11%, compared with only 7% for patients who only have isolated inversion of the T-wave.
Adverse prognostic factors include:
- Low ejection fraction
- Ongoing congestive heart failure
- New or worsening mitral regurgitation
- Hemodynamic instability
- Sustained ventricular tachycardia
- Recurrent episodes of angina despite maximal therapy
Consultations
Once a patient has been diagnosed with unstable angina, a cardiologist and a cardiac surgeon should be consulted. The cardiologist will need to stratify the risk and help decide on management.
Deterrence and Patient Education
Prevention
The prevention goals are to enable the patient to resume all daily activities, preserve myocardial function, and prevent future cardiac events. Today, most cardiac centers have specialized teams like cardiac rehab that offer intensive and more effective counseling.
Lifestyle
Smoking cessation is mandatory to prevent recurrent cardiac events. This applies to everyone in the household. Lipid-lowering should try to obtain a target low-density cholesterol level of 70 mg/dL or lower, a high-density cholesterol level of at least 35 mg/dL, and a triglyceride level of less than 200 mg/dL. The patient should also exercise and eat a low-fat diet.
Control of Hypertension
The target blood pressure should be below 140/90 mm Hg. At the same time, the patient should decrease their intake of sodium and alcohol.
Diabetes Mellitus Management
Blood sugar levels may be decreased with diet, exercise, or pharmacotherapy.
Weight Management and Nutritional Counseling
The patient should be encouraged to lose weight and achieve a body mass index of 25 kg/m
Activity Management
Patients at risk for unstable angina should avoid intense physical activity, especially in cold weather.
Pearls and Other Issues
Legally, unstable angina and other variants of acute coronary syndrome constitute a large portion of cases brought against clinicians. Aggressive evaluations of chest pain, in general, have led to over-testing, high admission rates, and often false positives, resulting in inappropriate testing. Several rules have been developed over the past several years to limit inappropriate admissions and testing. Many of these have variable sensitivity and specificity. Even with the number of ongoing legal cases, clinicians are often somewhat aggressive in the management and treatment of chest pain involving potential acute coronary syndrome.
Enhancing Healthcare Team Outcomes
Unstable angina is a pervasive disorder that is seen in the emergency room. There are many recommendations for the management of this severe cardiac condition. Current recommendations are that this disorder should be managed by an interprofessional team that includes primary healthcare professionals, nurse practitioners, physician assistants, pharmacists, cardiologists, and emergency room physicians, functioning together as an interprofessional team. In addition, a consult from a cardiac surgeon is highly recommended. The American College of Cardiology and the American Heart Foundation have issued guidelines on managing unstable angina.[11]
Once the patient has been stabilized, prevention is critical. Clinicians should urge the patient to quit smoking, eat a healthy diet, resume regular exercise, maintain a healthy body weight, and remain compliant with medications. Close follow-up is necessary to ensure that patients meet cardiac rehab goals. Further, lipid-lowering is vital to reduce the risk of recurrent unstable angina. The pharmacist should provide input and check dosing and potential drug-drug interactions; clinicians and pharmacists should emphasize the importance of blood pressure control and management of diabetes. Nurses will perform most ongoing monitoring, evaluate treatment effectiveness, and alert the clinician to potential issues. This type of interprofessional teamwork yields the best outcomes. Today, most hospitals have healthcare teams that specialize in managing unstable angina. These teams need to be familiar with the latest guidelines and educate patients on reducing risk factors and the benefits of medication compliance.
Outcomes
Evidence exists that quality improvement programs have the lowest morbidity and best outcomes.[12]