Introduction
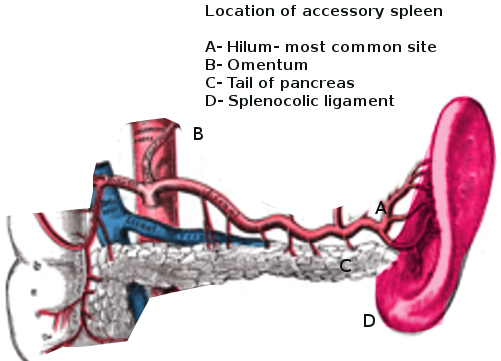
An accessory spleen, also called a supernumerary spleen, a splenule, or a splenunculus, is a benign and asymptomatic condition in which splenic tissue is found outside the normal spleen. Accessory spleens are a relatively common phenomenon with an estimated 10% to 30% of the population having one. Typically, an individual can have anywhere from one to six accessory splenic buds. Furthermore, the size of an accessory spleen can also vary. Most accessory spleens are approximately 1 centimeter, but it is not uncommon to find accessory spleens larger than a few centimeters. [1] Accessory spleens typically form due to developmental anomalies and are often confused with splenosis which is another form of ectopic splenic tissue. Splenosis arises from trauma which results in a portion of the spleen breaking off and embedding itself somewhere else in the peritoneal cavity. The newly embedded ectopic splenic tissue recruits local blood supply and becomes functional splenic tissue. An accessory spleen can be distinguished from splenosis since an accessory spleen is functionally and histologically similar to normal splenic tissue, but splenosis is missing key splenic characteristics such as a thick capsule, smooth muscle elements, and a blood supply arising from the splenic artery. [2]